Until recently, considerable evidence suggested that treatments which lastingly improved anxiety disorders succeeded because they included some form of systematic exposure to the feared stimulus (imaginal, live, vicarious, rapid, slow, continuous, intermittent) (Reference MarksMarks, 1973). In many randomised controlled trials (RCTs), treatments that lacked exposure were ineffective (e.g. relaxation, modelling without exposure, encouraging avoidance, reassurance), while efficacy of exposure variants was unimpaired when non-exposure elements such as relaxation were omitted.
Fear-reduction by exposure was called habituation - a decrease in response to cues that a subject is exposed to repeatedly, especially if for prolonged periods. If the response had initially been conditioned, its attenuation was called extinction. Although habituation and extinction can differ somewhat, habituation is used here to denote both processes because of their many similarities. Habituation is an evolutionarily ancient mechanism which appears in single-cell species and in immune and endocrine cells as well as neurons within multicellular species. Its strength is broadly proportional to the dose of exposure.
SHORTCOMINGS OF THE EXPOSURE PRINCIPLE
The idea that exposure is necessary to overcome fear encountered anomalies (Reference MarksMarks, 1987) that could be explained while conserving the role of exposure. When self-exposure failed to help some patients, this was ascribed to their exposure having not been ‘engaged’ or ‘functional’ due to avoidance, be it mental (e.g. dissociation, distraction), behavioural (e.g. escape, neutralising rituals), or biochemical (e.g. benzodiazepines, alcohol). Avoidance was said to prevent fear signals from reaching those parts of the brain which process emotion. Similarly, when exposure led to sensitisation, rather than habituation, during onset or relapse of anxiety disorders, this was explained by mental avoidance or insufficient exposure. Another explicable anomaly was that patients with phobias improved even after escaping from exposure whenever fear rose above a certain threshold (Reference Crowe, Marks and AgrasCrowe et al, 1972; Reference Rachman, Craske and TallmanRachman et al, 1986). However, as soon as those patients escaped they were asked to return to the frightening situation. Escape may have removed them from the feared cue too briefly for it to become a safety behaviour marking the lasting end of the fear.
Other anomalies were hard to explain. Some patients with chronic phobias reported no fear or avoidance from their very first exposure session; this improvement was too sudden to be explained by habituation. Some patients improved with medication without exposure. In a few patients fear did not decline despite prolonged and engaged exposure. Fear can decline just with hypnosis without exposure, with reassuring information, or pill placebo (Reference De Silva and RachmanDe Silva & Rachman, 1981).
As long as they were exceptional such cases were hard to study. “Fear reduction by non-exposure methods has to be made reliable before it can be examined systematically” (Reference MarksMarks, 1987). Now several studies provide converging evidence that non-exposure methods reduced fear in many cases.
EVIDENCE OF RELIABLE FEAR REDUCTION WITHOUT EXPOSURE
Muscle-tensing for blood phobia
The first RCT to report an effective non-exposure treatment for fear reduction (Reference Ost, Fellenius and SternerOst et al, 1991) involved patients with blood-injury phobias learning to tense their muscles to maintain blood pressure to stop hypotensive faints from the bradycardia evoked by seeing blood. Practising this physiological skill was even more effective than exposure at up to one-year follow-up. They did well on encountering blood at post-treatment without prior exposure (or cognitive restructuring).
Cognitive therapy
Fear also drops reliably with cognitive therapy which shares elements with thought control (Reference AlexanderAlexander, 1928), self-instructional training (Reference MeichenbaumMeichenbaum, 1977) and anxiety-management training (Reference Ramm, Marks and YukselRamm et al, 1981). Cognitive therapy usually involves: (a) identification and monitoring of negative thoughts; (b) evaluation of those thoughts by Socratic questioning, probability estimations of threat, evidence for and against threat and for positive and negative ways of thinking; and (c) encouragement of alternative positive thoughts and re-attributions. Exposure is typically added as ‘behavioural experiments’ with the patient being asked to face the feared situation in order to challenge negative expectations.
The common inclusion of exposure in ‘cognitive’ therapy raised doubts about whether the cognitive component was effective in its own right. Recently, however, cognitive therapy without systematic exposure yielded reliable and enduring fear-reduction. RCTs for various anxiety disorders, each of which teased apart the exposure from the cognitive therapy components, found similar efficacy of each approach in obsessive-compulsive disorder (OCD) (Reference Van Oppen, De Haan and Van BalkomVan Oppen et al, 1995), agoraphobia and/or panic disorder (Reference Williams and FalboWilliams & Falbo, 1996; Reference Hecker, Fink and VogeltanzHecker et al, 1998), post-traumatic stress disorder (PTSD) (Reference Marks, Lovell and NoshirvaniMarks et al, 1998; Reference Tarrier, Pilgrim and SommerfieldTarrier et al, 1999) and hypochondriasis (Reference Bouman and VisserBouman & Visser, 1998). These RCTs improved anxiety disorders with cognitive therapy even when it excluded exposure instructions or behavioural experiments. These trials on two continents point the same way. Exposure alone and cognitive therapy alone are each sufficient, but neither is necessary, to reduce fear reliably in anxiety disorders.
Problem-solving (self-examination therapy)
A non-exposure form of problem-solving (‘self-examination therapy’; Reference Bowman, Scogin and FloydBowman et al, 1997) was effective in an RCT for generalised anxiety disorder. Over four weeks, patients used a manual directing them to decide what was important and invest energy in that and think less negatively about things that did not matter. Assisted by a daily worksheet, patients selected important problems, brain-stormed possible solutions to these problems and tried them out, and learned to accept insoluble problems. Self-examination therapy, compared with a delayed-treatment group, reduced anxiety significantly to three-month follow-up.
Mindful meditation
Mindful meditation teaches people to cope with discomfort including fear (Reference Kabat-ZinnKabat-Zinn, 1996), typically in daily hour-long practice sessions over eight weeks. Mindful meditation-trained people reported no distress from their first encounter with hitherto-avoided unpleasant situations despite having had no systematic exposure or cognitive therapy. In RCTs, mindful meditation hastened the healing of psoriasis (a stress-affected condition) (Reference Basoglu, Wheeler and LightKabat-Zinn et al, 1998) and reduced recurrences of depression. Mindful meditation training includes learning to regard thoughts as ‘just’ thoughts without reacting (reminiscent of imaginal exposure and stress immunisation). Mindful meditation also trains attention to breathing, relaxation and hatha yoga. It teaches neither problem-solving nor cognitive-labelling of thoughts as positive, negative, or faulty, and does not challenge beliefs. Dismantling RCTs are needed in anxiety disorders.
Medication
In RCTs, anxiety disorders improved with antidepressant medications despite initial mood being normal and absence of exposure instructions. Improvement, however, was usually lost when medication was discontinued (Reference LiebowitzLiebowitz, 1998), whereas gains from the effective psychotherapies discussed above are typically maintained post-treatment.
ISSUES RAISED BY NON-EXPOSURE FEAR REDUCTION
The above findings challenge the idea that exposure is essential to reduce anxiety, and raise questions about how fear is reduced by such diverse methods.
Does exposure act merely by cognitive restructuring?
Across species, exposure gradually lessens avoidance, subjective fear and physiological responses to cues that a subject is exposed to. In humans, it also changes thoughts, attitudes and beliefs. Cognitive change is unlikely to be the primary path of fear reduction during exposure. First, cognitions often change only after avoidance, fear and physiological reactions have dwindled. Second, exposure reduces responses even in invertebrates and in single cells; to speak of their cognitions or expectations or sense of control would stretch the meaning of these terms. Third, in exposure therapy fear declines despite expressed negative expectations being confirmed. People with blood-phobias expect to faint, and indeed faint, on seeing blood early in exposure therapy, yet improve despite their syncope. Agoraphobics improve by deliberately inducing dreaded panic and enduring it until it subsides.
Does cognitive therapy act only by changing beliefs?
Cognitive therapy assumes that distress is maintained by negative beliefs or thoughts, and tries to change those. Beliefs at baseline and during treatment indeed predicted outcome in panic/agoraphobia (Reference HoffartHoffart, 1995). Other evidence, however, implies that cognitive therapy may also act non-cognitively. First, in an RCT of cognitive therapy for PTSD, key beliefs that were challenged changed after behaviour and symptoms had improved (Reference LivanouLivanou, 1998); some had changed marginally by the same rating point where behaviour and symptoms were much improved, but no beliefs changed before behaviour and symptoms did. Second, most panic/agoraphobia patients did not report, unprompted, the catastrophic thoughts about panic that are targeted by cognitive therapy (Reference Basoglu, Mineka and BasogluBasoglu & Mineka, 1992). Are such thoughts sometimes suggested to rather than elicited from patients? Third, catastrophic thoughts can calm rather than terrify. An agoraphobic woman endured panic by summoning up horrific images of a tiger devouring her that she had visualised during irrelevant exposure therapy (Reference Watson and MarksWatson & Marks, 1971). Patients improve with paradoxical intention by imagining terrifying scenes briefly to reduce fear - too briefly to involve habituation. What is visualised may be less vital than bracing, steeling, preparing, controlling oneself to face the worst (see below).
INTEGRATION OF FINDINGS
Potential fear-reducing components in various treatments
Table 1 displays components of four treatments that were effective for anxiety disorders in RCTs (exposure, cognitive, muscle-tensing, problem-solving) of another seeming promising in uncontrolled work (mindful meditation), and of two treatments that did poorly in RCTs (relaxation (non-applied), avoidance).
Table 1 Generic and specific treatment components
| Treatment components | Effective treatments | Uncertain effectiveness | Ineffective treatments | ||||
|---|---|---|---|---|---|---|---|
| Exposure | Cognitive therapy (without exposure) | Muscle-tensing | Problem-solving | Mindful meditation | Relaxation (non-applied) | Avoidance | |
| Generic across most treatments | |||||||
| Treatment set | + | + | + | + | + | + | + |
| Rationale | + | + | + | + | + | + | + |
| Problem-solving approach | + | + | + | + | +- | - | - |
| Regular homework assignments | + | + | + | + | + | + | + |
| Keeping diaries | + | + | - | + | + | + | + |
| Specific to certain treatments only | |||||||
| Exposure to fear cues | + | - | - | - | +- | - | - |
| Stress immunisation | - | - | - | - | +- | - | - |
| Cognitive restructuring | - | + | - | +- | - | - | - |
| Physiological coping skill | - | - | + | - | - | - | - |
| General coping skills | - | - | - | - | + | - | - |
| Relaxation (non-applied) | - | - | - | - | +- | - | - |
All four effective treatments include the four components of a treatment set, rationale, homework and (except for muscle-tensing) diary-keeping. The homework and diary content vary. They include: in exposure, staying in the feared situation; in cognitive therapy, monitoring and changing thoughts; in tension training for blood phobia, muscle-tensing; in problem-solving, listing and dealing with problems.
Both ineffective approaches (relaxation and avoidance) also contain the above four components, showing they are not therapeutic per se. In contrast, neither relaxation nor avoidance include problem-solving, which involves externalising, attending to, analysing, reframing and coping with the problem bit by bit. Those bits, however, are managed differently in the various effective treatments (e.g. by exposure, or cognitive restructuring, or muscle-tensing). Like exposure, problem-solving may suffice but not be necessary for fear reduction, as it is absent in mindful meditation.
Treatments act on the emotional response syndrome of fear
Fear, like any emotion, is a loosely linked network of responses spanning feelings, thoughts, behaviours and physiological events (Fig. 1). These are normal unpleasant reactions to threat. They constitute an emotional response syndrome. When excessive, such responses are what anxiety disorder patients want to reduce.
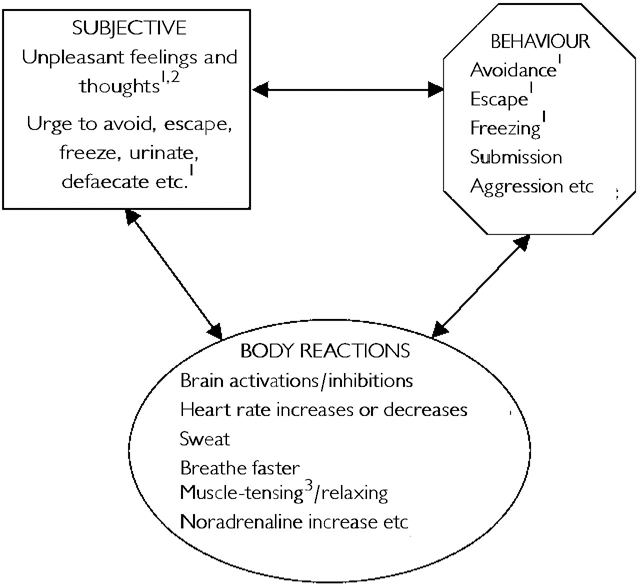
Fig. 1 Three domains of emotional response syndromes with constituent components (each has far more than shown) which connect to other components within and between domains. Some components may connect more tightly across than within domains, certain connections being one-way, others two-way. Particular fear components may be reduced first by particular treatment ingredients with knock-on effects on other fear components. 1. Exposure action. 2. Cognitive restructuring. 3. Muscle-tensing therapies.
An emotional syndrome can be curbed in various ways by weakening one or more links in its response network. Attenuating one can erode others. Treatment may reduce emotion better by weakening some links than others. Some treatments may weaken several links in the fear network simultaneously. Certain links may be unidirectional, while others may be bi-directional or form interactive feedback (Reference BarlowBarlow, 1988). How different treatments act on each link with diverse knock-on effects needs elucidation.
Examples may clarify this model. Exposure seems to improve fearful feelings, behaviour and physiological reactions simultaneously, with cognitive changes following later (Reference MarksMarks, 1987). The underlying process may involve exposure lowering fear with resultant change in beliefs which lessens fear further which facilitates more exposure which reduces fear still more and gradually transforms beliefs. Cognitive therapy appears to improve fearful feelings, behaviour and cognitions. In two RCTs, heart rate biofeedback enabled patients with phobias to reduce tachycardia during exposure but this did not enhance subjective or behavioural improvement (Reference MarksMarks, 1987). In contrast, the physiological approach of muscle-tensing enhanced subjective and behavioural improvement of patients with blood phobias (Reference Ost, Fellenius and SternerOst et al, 1991). Test is needed of whether stress-immunising or cognitive or problem-solving approaches act widely across the fear network.
How many roads to the Rome of fear-reduction?
A provisional map would show: (a) an exposure highway that habituates many fear components; (b) a cognitive road acting on cognitive and/or other fear components; (c) a physiological track of coping skills acting on particular problems; (d) a problem-solving path without exposure or cognitive restructuring that modulates emotions; and (e) an indistinct trail of attention-training or stress immunisation such as mindful meditation. Exposure, cognitive restructuring and problem-solving might converge on a common end path of problem-solving. All three might share with mindful meditation an attention-training path that disengages feelings and thoughts from automatic action. Muscle-tensing seems a separate physiological track.
Other questions are: can changing beliefs motivate exposure that lessens fear and speed fear reduction during exposure? Can exposure lessen fear by revising beliefs? Can habituation of fearful feelings and bodily reactions in turn alter beliefs? How important is it that before doing exposure patients practise problem-solving - externalise the problem, attend to, analyse, reframe and deal with aspects of it gradually, and delay action on strident feelings?
Cognitions can change via several paths. First, by directly habituating thoughts that arise during exposure or behavioural experiments in cognitive-behavioural therapy (in the ‘mere exposure’ procedure of semantic satiation, repeating words quickly many times weakens their meaning). Second, by direct reasoning as used in cognitive therapy. Third, indirectly, by problem-solving intrinsic to learning why and how to do cognitive therapy, as it is intrinsic to learning how to do exposure. Fourth, indirectly, as a secondary effect of the habituation of behaviours and bodily reactions during exposure.
Physiological roads to fear-reduction have rarely been studied in RCTs except for muscle-tensing and heart-rate biofeedback.
Each treatment might act on particular aspects of the fear response network with domino effects on other links. Exposure (both relevant and irrelevant), cognitive therapy and mindful meditation might all train attention to tolerate thoughts and feelings without reacting automatically to them and so enhance emotional control. How focusing attention improves different facets of various anxiety disorders, in what sequence, and for how long, awaits research. It might improve control over more emotions than just fear, for example, anger, jealousy and sexual arousal, making it a form of stress immunisation (toughening up). Conversely, anger-management training may also reduce anxiety.
Certain medications reduce fear directly as well as indirectly by relieving the low mood that often complicates anxiety disorders. Some may enhance exposure in the short term but hamper long-term outcome (Reference Marks, Swinson and BasogluMarks et al, 1993). The neurochemical paths of drug action are outside the present paper's remit, but need inclusion in a comprehensive fear-reduction theory.
Control: descriptive or explanatory construct?
Do effective treatments act on that domain variously called sense of control, confidence, mastery, empowerment or self-efficacy? Animals become more disturbed after uncontrollable and unpredictable aversive experiences, and less distressed after being allowed mastery experiences (Reference Basoglu, Mineka and BasogluBasoglu & Mineka, 1992). PTSD after torture is prevented by being psychologically prepared for it (involving perceived control; Reference Basoglu, Mineka and PakerBasoglu et al, 1997) and is associated with perceived loss of control during torture. In PTSD, more post-treatment sense of control and internal attribution of gains predicted continuing gains at follow-up (Reference Basoglu, Marks and KilicBasoglu et al, 1994; Reference LivanouLivanou, 1998). Occasionally, reducing anxiety by exposure boosts confidence to overcome wider problems (Reference Marks, Viswanathan and LipsedgeMarks et al, 1972; Reference Marks and Mataix-ColsMarks & Mataix-Cols, 1997). Conversely, a surge of confidence for any reason may inspire practice of exposure to overcome phobias. Confidence might reflect other mechanisms. Its rise after therapy and correlation with improvement could result from rather than cause fear reduction.
Reduction of anxiety is not always associated with a sense of control. Becoming resigned to one's fate (giving up vain attempts at control - safety behaviours) seems calming, not frightening - a key to some religious practices. During exposure, people phobic about flying try to control the plane by moving their body; learning to accept its uncontrollable movements seems important in overcoming their fear.
DIRECTIONS FOR FUTURE RESEARCH
Fear-reducing mechanisms can be clarified. Cognitive therapy components deserve dissection. Many treatment packages including teaching of a physiological skill - slow, deep breathing, to counter panic; this needs study on its own. Whether enhancing a sense of control lessens fear requires testing. Meditation components need dismantling: attention to breathing, relaxation, yoga, looking at thoughts as ‘just’ thoughts without reacting.
The identification of therapy components that reduce each facet of fear would be aided by searching for predictors of improvement at each treatment stage and at follow-up. What patients do, feel and think during and between sessions requires recording. Process measures can unravel potential fear-reduction mechanisms, such as targeted beliefs, confidence, general and specific sense of control, coping skills, problem orientation, habituation.
Caveats
The research outlined above will advance knowledge more if it tries to disconfirm rather than support hypotheses, in order to separate the sheep of one theory from the goats of another. If dropping safety behaviours enhances improvement, for example, that does not separate an exposure from a cognitive model, because it makes exposure more functional and also disconfirms dangerous expectations.
Exposure, cognitive therapy and other approaches may all be teaching patients to uncouple thoughts/feelings from immediate action. Manipulation of fear-reducing treatment ingredients and close attention to subsequent sequences could unravel which of changes in beliefs, sense of control, physiology or avoidance are primary and which secondary.
Finally, confusion from inconsistent use of terms for fear-reducing approaches could be reduced by adopting standard definitions of treatment components. Although every label is ineluctably theory-laden, it is more useful to define procedures by what is done than by the rationale for doing them.
ACKNOWLEDGEMENTS
This paper was facilitated by a Sackler Scholarship for I.M. at the Sackler Advanced Studies Institute at Tel Aviv University. Valuable comments on the manuscript were made by Drs Metin Basoglu, Ken Kirkby, Maria Livanou and Anne-Marie O'Dwyer.





eLetters
No eLetters have been published for this article.