People with schizophrenia die early, especially from cardiovascular disease (Reference Mortensen and JuelMortensen & Juel, 1993), which is associated with a low intake of fruit and vegetables (Reference GillmanGillman, 1996). We have previously shown that people with schizophrenia make poor dietary choices (Reference McCreadie, Macdonald and BlacklockMcCreadie et al, 1998), and we concluded that assertive programmes to improve their eating habits were necessary. Advice to the general population to improve fruit and vegetable intake has been shown to be successful, at least in the short term (Reference Zino, Skeaff and WilliamsZino et al, 1997). However, we believe that improvements in patients’ eating habits might be achieved if the intervention focused on the environment, rather than relying on the patient to make changes. We therefore decided that the principal intervention in our randomised controlled trial would be the provision of free fruit and vegetables. Provision of free food can influence the diet of the general population (Reference Pietinen, Dougherty and MutanenPietinen et al, 1984), and also that of people who are homeless (Reference Gelberg, Stein and NeumannGelberg et al, 1995) or obese (Reference Wing, Jeffery and BurtonWing et al, 1996). Associated instruction in the preparation of food may be necessary, and we incorporated this in one arm of our intervention programme.
METHOD
Participants
Patients with a DSM–IV diagnosis of schizophrenia (American Psychiatric Association, 1994) were recruited from those living in the community in two areas of Scotland: Nithsdale, in Dumfries and Galloway (n=55), and Partick, in west Glasgow (n=47). Patients lived on their own or in supported accommodation, 2–11 to a house. Patients were encouraged to be responsible for their own domestic chores, including shopping and cooking. Support was provided by regular input from care workers. The patients in supported accommodation were no longer living with their families for various reasons but their position in the community had been assessed by social services as sufficiently precarious for them to need additional support. A generation ago it is likely these patients would have been in long-stay psychiatric wards.
All patients gave written, informed consent and the project was approved by the relevant local research ethics committees.
Randomisation
Randomisation of patients was clearly impractical where there was more than one resident in a house. Therefore houses, not patients, were randomly allocated to receive free fruit and vegetables for a period of 6 months, and associated instruction; free fruit and vegetables alone; or to continue as before. Randomisation was stratified by urban (Partick) and rural (Nithsdale) areas.
Where a house was allocated free fruit and vegetables, care workers responsible for that house ensured that each week sufficient fruit and vegetables were purchased to provide at least five portions per resident per day. The residents were encouraged to take part in the shopping expeditions and make appropriate purchases. Care workers kept the till receipts from supermarkets and shops as a record of what was purchased. Those who received free fruit and vegetables and associated instruction received in addition to the free food basic instruction in food preparation from an occupational therapist or senior care worker. Such instruction included meal planning and the purchase, storage and preparation of food, with particular reference to fruit and vegetables. The occupational therapist worked with the patient during the first month and gave additional help in the third and sixth months.
Assessment
Patients’ diets were assessed in three ways. First, a nurse, masked as to whether the patient received free food, assessed the usual eating habits of the patient by means of the eating habits section of the Scottish Health Survey Questionnaire (Scottish Executive Health Department, 1998), which assesses food intake retrospectively. Second, within this questionnaire there is a specific assessment of fruit and vegetable intake. Third, a blood sample was taken to measure plasma folate, glucose, vitamins C and E and carotenoids, and serum total cholesterol and high-density lipoprotein (HDL) cholesterol (see below). Plasma and serum were stored at –70 °C. Measurements were made masked to intervention status.
Dietary assessments were made, and blood samples taken as close as possible to the dietary assessment, at baseline (before randomisation), at the end of the intervention (6 months) and at 6 months and 12 months after the intervention. At the same time intervals, each patient's mental state was assessed by a psychiatrist masked to intervention status, using the Positive and Negative Syndrome Scale (PANSS) for schizophrenia (Reference Kay, Fiszbein and OplerKay et al, 1987); also recorded were body mass index and level of physical activity (Reference Lowther and MutrieLowther & Mutrie, 1996). At baseline and 18 months later, cardiovascular risk factors (age, gender, smoking status, blood pressure, left ventricular hypertrophy, plasma glucose concentration and serum total cholesterol and HDL cholesterol levels) were measured by the Framingham assessment and associated computer program (Reference Hingorami and VallanceHingorami & Vallance, 1999).
Outcome measures
The primary outcome measure was the number of portions of fruit and vegetables eaten per week, with a comparison of change from baseline to 12 months after the provision of free fruit and vegetables was withdrawn. This was measured by the fruit and vegetables section of the Scottish Health Survey questionnaire (Reference Lean, Anderson and MorrisonLean et al, 2003). Secondary measures included global assessment of diet; plasma folate, vitamins C and E and carotenoids; cardiovascular risk factors and body mass index.
Analysis
Analyses were done on an intent-to-treat basis. All patients with baseline data and at least one post-baseline measurement were included in the analyses. The differences among the three groups in the primary outcome measure (the number of portions of fruit and vegetables consumed per week) were measured by analysis of variance, including baseline intake as a covariate in the model. Clusters (the houses) were the unit rather than individual patients (Reference Kerry and BlandKerry & Bland, 1998). Two-tailed tests were used.
Power calculation
Based on the assumption of 90 houses, 1 with seven patients, 1 with six, 5 with three, 13 with two and 70 with one patient, there would therefore be 90 clusters with an average of 1.4 patients per cluster. If we assume the mean intake of fruit and vegetables in the intervention group (free fruit and vegetables plus instruction) rises from 16 to 23 portions per week (an increase of one portion per day), and there is no change in the two other groups, then these are adequate numbers to detect a significant among-group difference, with 90% power and 5% significance level.
RESULTS
We approached 186 patients with an invitation to participate in the study; 102 patients (55%) living in 85 houses consented. Those who consented did not differ from those who refused in gender distribution or age. The progress of participants through the trial is shown in Fig. 1.

Fig. 1 Progress of participants through the trial.
Baseline findings
Baseline findings have been reported elsewhere (Reference McCreadieMcCreadie, 2003); they are summarised in Table 1 (socio-demographic data) and Table 2, a comparison of our patients’ dietary choices with the Scottish Health Survey data (Scottish Executive Health Department, 1998) which most closely reflect the aspirational targets of the Diet Action Plan for Scotland (Scottish Office Department of Health, 1996, 1999). Fewer men with schizophrenia than men in the general population reached target levels of consumption of fresh fruit and vegetables, skimmed or semi-skimmed milk, potatoes, pasta or rice and pulses. More men with schizophrenia than men in the general population frequently consumed breakfast cereal. Fewer women with schizophrenia than women in the general population reached acceptable levels of consumption of skimmed or semi-skimmed milk and potatoes, pasta or rice.
Table 1 Socio-demographic data
| Gender, n (%) | |
| Male | 72 (71) |
| Female | 30 (29) |
| Age, years: mean (s.d.) | 45 (13) |
| Length of illness, years: mean (s.d.) | 21 (13) |
| Marital status, n (%) | |
| Single | 82 (80) |
| Married | 3 (3) |
| Divorced/separated | 14 (14) |
| Widowed | 3 (3) |
| Domiciliary status, n (%) | |
| Lives alone | 56 (55) |
| Lives with other patients | 41 (40) |
| Other | 5 (5) |
Table 2 Baseline findings: dietary choices of patients and of the general population of Scotland

| Dietary choice1 | Men | Women | ||||
|---|---|---|---|---|---|---|
| Patients (n=72) % | General population2 (n=3941) % | P 3 | Patients (n=30) % | General population2 (n=5106) % | P 3 | |
| Fresh fruit once a day or more | 33 | 46 | 0.04 | 43 | 59 | 0.12 |
| Fruit juice once a day or more | 17 | 26 | 0.09 | 20 | 32 | 0.23 |
| Cooked green vegetables five times a week or more | 10 | 39 | <0.0001 | 27 | 44 | 0.08 |
| Cooked root vegetables five times a week or more | 1 | 22 | <0.001 | 10 | 27 | 0.06 |
| Raw vegetables or salad twice a week or more | 25 | 45 | 0.001 | 40 | 59 | 0.05 |
| Use skimmed or semi-skimmed milk | 50 | 63 | 0.03 | 50 | 69 | 0.04 |
| Oil-rich fish less than once a month | 43 | 33 | 0.09 | 27 | 33 | 0.59 |
| Potatoes, pasta or rice five or more times a week | 25 | 64 | <0.0001 | 30 | 69 | <0.0001 |
| Pulses two or more times a week | 32 | 67 | <0.0001 | 30 | 58 | 0.004 |
| Breakfast cereal once a day or more | 58 | 38 | 0.0007 | 50 | 38 | 0.25 |
| Usually eat wholemeal bread | 6 | 10 | 0.29 | 20 | 16 | 0.73 |
The mean number of fruit and vegetable portions consumed each week was 16 (s.d.=14). This was made up of fruit (excluding fruit juice): mean number of portions 7 (s.d.=10); vegetables: mean 6 (s.d.=6); and fruit juice: mean 3 (s.d.=7).
Intervention
Thirty-two patients received free fruit and vegetables plus instruction, 37 received fruit and vegetables alone and 33 received treatment as usual (Table 3). One patient in the free fruit and vegetable group refused further free food at 3 months. All patients in the first two groups were reassessed at the end of the intervention and 27 of 33 in the treatment as usual group.
Table 3 Participants’ consumption of fruit, vegetables and fruit juice
| Portions per week, n: mean (s.d.) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Free fruit and vegetables with instruction group | Free fruit and vegetables group | Treatment as usual group | ||||||||||
| Baseline (n=32) | 6 months (n=32) | 12 months (n=31) | 18 months (n=31) | Baseline (n=37) | 6 months (n=37) | 12 months (n=37) | 18 months (n=36) | Baseline (n=33) | 6 months (n=27) | 12 months (n=27) | 18 months (n=24) | |
| All fruit and vegetables | 16 (14) | 30 (19) | 23 (21) | 21 (19) | 14 (12) | 31 (24) | 16 (11) | 20 (19) | 19 (17) | 18 (15) | 20 (25) | 19 (14) |
| Fruit (excluding fruit juice) | 7 (6) | 12 (11) | 9 (11) | 10 (11) | 5 (7) | 13 (12) | 8 (8) | 9 (10) | 9 (15) | 9 (10) | 7 (12) | 10 (16) |
| Vegetables | 6 (4) | 7 (5) | 8 (7) | 6 (5) | 5 (6) | 8 (6) | 5 (4) | 6 (4) | 8 (6) | 5 (5) | 6 (7) | 6 (5) |
| Fruit juice | 4 (8) | 10 (10) | 7 (8) | 5 (8) | 3 (5) | 10 (14) | 3 (4) | 5 (8) | 2 (6) | 4 (7) | 7 (6) | 4 (7) |
Figure 2 shows in the three groups the mean weekly total number of fruit and vegetable portions at different stages in the study. Using the last observation carried forward method, there was no significant between-group difference in the primary outcome measure, namely change from baseline to 12 months after the intervention finished in the number of portions of fruit and vegetables consumed. Further analysis of the different periods showed that, when change from baseline to the end of the intervention was examined, there was a significant between-group difference; fruit and vegetable intake increased in both the free fruit and vegetables alone and the free fruit and vegetables plus instruction groups, but not in the treatment as usual group. Figure 2 suggests that the fall in consumption after the intervention stopped was more gradual in the fruit and vegetable plus intervention group, but the difference between the groups 6 months after the intervention stopped was not statistically significant. Table 4 shows the results separately for fruit (excluding fruit juice), vegetables and fruit juice. Inspection of the data suggests that at the end of the intervention, in the two free fruit and vegetables groups it was the consumption of fruit and fruit juice that rose most. However, the most significant result, statistically speaking, was in the consumption of vegetables; this was because consumption fell in the treatment as usual group.
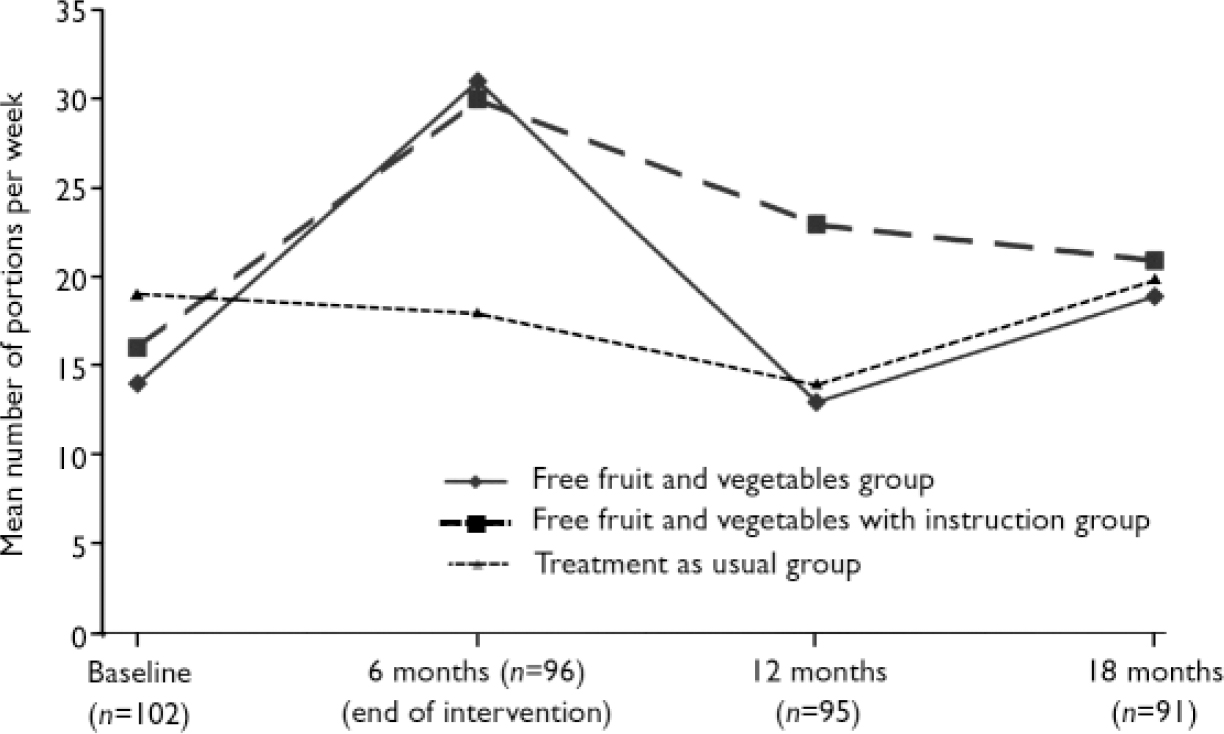
Fig. 2 Total fruit and vegetable intake in the three study groups.
Table 4 Analysis of variance
| All fruit and vegetables | Fruit (excluding fruit juice) | Vegetables | Fruit juice | |||||
|---|---|---|---|---|---|---|---|---|
| F | P | F | P | F | P | F | P | |
| 0-6 months | 8.82 | 0.003 | 2.85 | 0.06 | 8.32 | 0.0005 | 4.01 | 0.02 |
| 0-12 months | 0.27 | 0.76 | 0.68 | 0.50 | 4.16 | 0.02 | 0.79 | 0.46 |
| 0-18 months | 0.46 | 0.63 | 0.03 | 0.97 | 3.82 | 0.03 | 0.30 | 0.74 |
There was no significant between-group difference at any time point in measures of change from baseline in blood indices of nutrition, mental state as measured by the PANSS, body mass index, level of physical activity and risk of coronary heart disease, as measured by the Framingham assessment (further details available from the author upon request). Also, there was no significant change from baseline at any time point in other aspects of the patients’ diet, such as consumption of skimmed or semi-skimmed milk, oil-rich fish, potatoes, pasta or rice, pulses, breakfast cereal or wholemeal bread.
DISCUSSION
Methodological issues
We have discussed some of the methodological issues in a previous paper (Reference McCreadieMcCreadie, 2003). First, although almost half the patients we approached refused to participate in the study, those who refused did not differ from those who did participate in gender distribution, age or living arrangements. Second, the dietary questionnaire that we used assesses food intake retrospectively, with the possibility of recall errors. However, it is by no means certain that a prospective weighed intake of food would have provided a more accurate assessment. Third, there was no independent way to confirm that the free fruit and vegetables provided were actually eaten.
The power calculation suggested that about 120 patients should enter the study. Only 102 did so. However, the calculation was based on an increase in consumption of only one portion of fruit and vegetables per day. The actual increase achieved by the end of the intervention was substantially greater than this.
Consumption of fruit and vegetables
We found that people with schizophrenia who habitually eat little fruit or vegetables are able and willing to consume more if the food is provided free of charge. Only one patient withdrew from the free fruit and vegetable groups before the intervention stopped. The mean consumption of fruit and vegetables doubled in those who were given either free fruit and vegetables or free fruit and vegetables and associated instruction. Inspection of the data suggested it was easier to increase the intake of fruit and fruit juice than that of vegetables. Fruit and fruit juice can be readily consumed, whereas most vegetables need preparation.
The change in consumption of fruit and vegetables by the end of the intervention was not accompanied by changes in any of the other dietary targets identified in the Scottish Health Survey (Scottish Office Department of Health, 1996), such as an increase in the consumption of oil-rich fish, potatoes, pasta or rice, or wholemeal bread. Thus fruit and vegetables were simply ‘added on’ to their existing diet. The change in fruit and vegetable consumption was also not accompanied by any change in mental state, as assessed by PANSS total and sub-scale scores. This longitudinal finding complements that in the cross-sectional survey (Reference McCreadieMcCreadie, 2003), which identified no difference in PANSS scores between those taking the most and the fewest portions of fruit and vegetables per week.
Persistence of improvement
With regard to the primary outcome measure – that is, the difference in consumption of fruit and vegetables between baseline and 12 months after the intervention stopped – there was no difference between the three groups. In this sense the intervention was unsuccessful.
In three of the studies quoted in the opening paragraph there was either no follow-up or only a very brief one (8 weeks) (Reference Pietinen, Dougherty and MutanenPietinen et al, 1984; Reference Gelberg, Stein and NeumannGelberg et al, 1995; Reference Zino, Skeaff and WilliamsZino et al, 1997). In the fourth (Reference Wing, Jeffery and BurtonWing et al, 1996), improvement in the intervention groups was sustained 1 year later.
There are no doubt a number of reasons why change did not persist. First, perhaps the intervention did not last long enough. Second, after the intervention stopped, patients had to buy their own food; fruit and vegetables are not cheap and are not always easily available. Almost all our patients were unemployed and lived on state benefits. Two-thirds of our patients smoke; approximately a third of their benefits is spent on tobacco (Reference McCreadie and KellyMcCreadie & Kelly, 2000). Third, we found that fruit and vegetable consumption increased among both those who received free fruit and vegetables alone and those who received free fruit and vegetables together with associated instruction. Our hypothesis was that not only was the provision of free fruit and vegetables necessary to improve patients’ diet but also that dietary education and help with food purchase and preparation would be essential. However, the results show little value from the additional support, so although the lessons were ‘taught’ they were not ‘learned’. Perhaps the occupational therapists’ help was not sufficient or aspects of the patients’ illness contributed to an unwillingness or inability to change. It may also be that, although patients consented to enter the study, they lacked the will to change. Perhaps a form of motivational interviewing might have been more effective.
The positive results at 6 months raise the possibility that if patients had continued to receive free fruit and vegetables weekly, their consumption might have remained at a higher level. Continuing long-term provision of free food has been advocated for the homeless (Reference Gelberg, Stein and NeumannGelberg et al, 1995) and now, under the National School Fruit and Vegetable Scheme (Department of Health, 2005), all children aged 4–6 years in state schools in England are entitled to a free piece of fruit or vegetable each school day. For population subgroups who are not fully able to make wise, informed choices about dietary health, a case can be made for providing foods that will fulfil dietary targets for health. Many patients with schizophrenia come into this category.
The wider context of treatment
The failure of an intervention to produce a sustained change in people with schizophrenia must be placed in the wider context of their treatment. Other interventions in people with schizophrenia, unless sustained, do not produce lasting benefits. For example, it has long been known that withdrawal of antipsychotic medication can cause relapse (Reference Leff and WingLeff & Wing, 1971). Medication is provided free to most people with schizophrenia.
Although there was an increase in fruit and vegetable consumption by the end of 6 months, this was not accompanied by changes in plasma micronutrients, which at baseline were at abnormal levels in substantial numbers of patients: for example, 42% had low b-carotene levels, 49% had low vitamin C levels and 53% had a high cholesterol:HDL ratio (Reference McCreadieMcCreadie, 2003). There are at least three possible reasons for this. First, the plasma half-life of some water-soluble micronutrients is short; if blood samples were taken even a few days after fruit and vegetable consumption fell, plasma micronutrient levels might also have fallen. Second, within the groups there was a great variability in plasma levels; differences between groups would therefore be harder to detect. Third, as stated before, there was no independent way to confirm that the fruit and vegetables had actually been eaten.
There was no change in body mass index or risk of coronary heart disease. This reinforces the view that the consumption of free fruit and vegetables was an ‘add-on’ and the extra consumption was not enough to displace other foods.
We have found that the lifestyle of people with schizophrenia as measured by diet, weight and exercise must give cause for concern, especially in relation to coronary heart disease (Reference McCreadieMcCreadie, 2003). Our intervention did not prove successful in the longer term and therefore other ways must be found to address these issues. Primary care services should be encouraged to be more involved. In addition, outreach from secondary services to such patients in the community (a vulnerable section of the population) should be concerned not only with mental but also with physical health, otherwise the risk of cardiovascular and other diseases will remain high and patients will die prematurely.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ People with schizophrenia who habitually eat little fruit or vegetables are able to consume more if the food is provided free of charge.
-
▪ After withdrawal of free fruit and vegetables the improvement in diet did not persist. Perhaps the intervention should have continued longer.
-
▪ Both primary and secondary care should probably be involved in the management of the physical health of people with schizophrenia.
LIMITATIONS
-
▪ Almost half of the patients approached refused to participate in the study.
-
▪ The dietary questionnaire assessed food intake retrospectively.
-
▪ There was no independent way to confirm that the free fruit and vegetables were actually eaten.
Acknowledgements
We thank the patients for their cooperation. The following are members of the Scottish Schizophrenia Lifestyle Group: Crichton Royal Hospital, Dumfries: Professor R. G. McCreadie, Mrs S. Williams, Ms E. Brown, Mrs S. Farrington, Mrs M. Hunter, Dr S. Macdonald, Dr J. White, Dr I. Kader, Dr S. Holmes, Dr G. Morrison, Mrs S. Wall, Mrs C. Colwell; Gartnavel Royal Hospital, Glasgow: Dr C. Kelly, Dr M. Connolly, Ms D. Fraser, Mrs C. Gray, Dr J. Ellison, Dr R. Brogan, Dr D. Brown; Dumfries & Galloway Royal Infirmary: Dr J. R. Paterson, Miss H. Barrington, Mrs G. J. Baxter; Royal Infirmary, Glasgow: Professor M. Lean, Dr C. Hankey; Rowett Research Institute, Aberdeen: Dr G. Duthie.
The study was funded by the Chief Scientist Office, Scottish Executive, Edinburgh.









eLetters
No eLetters have been published for this article.