To prosper in the long term, assertive outreach teams need to attract and retain skilled and dedicated staff. Difficulties with staff recruitment and retention threaten effective mental health service delivery in the UK (Sainsbury Centre for Mental Health, 2001). Several studies in the 1990s reported high levels of ‘burn-out’ among community mental health team (CMHT) staff, although paradoxically associated with relatively good job satisfaction (Reference Fagin, Brown and BartlettFagin et al, 1995; Reference Prosser, Johnson and KuipersProsser et al, 1996; Reference Onyett, Pillenger and MuijenOnyett et al, 1997; Reference Wykes, Stevens and EverettWykes et al, 1997). Some authors have argued that staff delivering intensive community care to severely ill client groups are very susceptible to burn-out, threatening the sustainability of this model (Reference DedmanDedman, 1993; Reference Connolly, Marks and LawrenceConnolly et al, 1996). However, assertive outreach team staff may also find the work particularly rewarding. Empirical evidence regarding the views and experiences of staff in assertive outreach teams is lacking. This part of the Pan-London Assertive Outreach Study compares satisfaction and burn-out, sources of stress and satisfaction and views about training and supervision between assertive outreach team and CMHT staff. It also explores whether there are differences between types of assertive outreach team.
METHOD
Sample
All 24 dedicated assertive outreach teams established within Greater London by the summer of 2001 were recruited to the Pan-London Assertive Outreach Study. Within each team, all clinical staff in post between 18 June and 18 September 2001 were asked to complete a confidential questionnaire. Nine CMHTs were also included in the study for comparison. One was selected at random from each of the nine mental health trusts in which assertive outreach teams were operating. Where a trust had a single catchment area in which an assertive outreach team operated, the CMHT was selected randomly within this area, but if there were multiple catchment areas with assertive outreach teams within a trust, then a catchment area was first selected at random and then a team within this area. All clinical staff in position between 1 November 2001 and 1 February 2002 in the CMHTs were also asked to complete the questionnaire. All the assertive outreach teams and CMHTs that we invited to participate agreed to do so.
Measures
Background information
Brief data were collected on socio-demographic and occupational characteristics, including age, gender, profession and length of service.
Measures of burn-out and job satisfaction
Staff burn-out was assessed using the Maslach Burnout Inventory (Reference Maslach and JacksonMaslach & Jackson, 1986), which yields scores for three components of burn-out. These components are ‘emotional exhaustion’ (depletion of emotional resources, leading to workers feeling unable to give of themselves at a psychological level), ‘depersonalisation’ (negative, cynical attitudes and feelings about patients) and ‘reduced personal accomplishment’ (evaluating oneself negatively, particularly with regard to working with patients).
Job satisfaction was measured using two instruments used previously in major UK studies of mental health staff and thus useful for comparisons with previous findings. The first was the job satisfaction section from the Job Diagnostic Survey (Reference Hackman and OldhamHackman & Oldham, 1975). All five items in this measure relate to global attitudes to the job rather than views about specific aspects of it. The second was the Minnesota Satisfaction Questionnaire, Short Form (Reference Weiss, Davis and EnglandWeiss et al, 1967), which consists of 20 items rated on a five-point scale, each measuring satisfaction with a particular aspect of work. This yields scores for intrinsic and extrinsic job satisfaction sub-scales. Intrinsic job satisfaction is scored from 12 to 60 and reflects the extent to which staff feel that their job fits their vocational abilities and needs, with ratings including satisfaction with ‘the chance to do things for other people’ and ‘the chance to do something that makes use of my abilities’. Extrinsic satisfaction is scored from 6 to 30 and is a measure of satisfaction with working conditions and rewards, with ratings including satisfaction with ‘the pay and amount of work I do’ and with ‘the way my boss handles his/her workers’.
Sources of stress and satisfaction
Staff were asked to rate the extent to which their working environment, clinical case-loads and other aspects of work were stressful or satisfying. The questionnaire used was an adapted version of that developed and reported by Prosser et al (Reference Prosser, Johnson and Kuipers1997), and included additional items with specific relevance to work in assertive outreach teams.
Description of and views about training and supervision received
Staff were asked to describe how much training and supervision they had received in their post, how satisfactory they found it and whether they felt that they had further training needs in any area.
Statistical analysis
Statistical software STATA (release 8.0; Stata Corporation, 2003) was used for data analysis. Results for staff working in the same team may not be independent, therefore all significance tests and confidence intervals were computed using robust standard errors that allow for clustering by team. The survey estimation commands in STATA allow the computation of means, confidence intervals and χ2 tests adjusted for clustering, and were used for descriptive statistics and tests of association between categorical variables. Linear regression using robust standard errors was used to test for associations between continuously distributed variables such as burn-out and satisfaction scores and other variables. The principal analyses followed three stages.
-
(a) The socio-demographic and occupational characteristics of assertive outreach team and CMHT staff were described and compared.
-
(b) Comparisons were made between scores for assertive outreach teams and CMHTs for each of the main burn-out and satisfaction indicators. To identify confounders and explore factors associated with burn-out and job satisfaction, the main socio-demographic and occupational variables were added as additional independent variables in regression analyses, with burn-out and satisfaction scores as the dependent variables.
-
(c) Burn-out and satisfaction scores were compared between the three types of assertive outreach team identified in the Pan-London Assertive Outreach Study
(see Reference Wright, Burns and JamesWright et al, 2003, this issue). Adjustment was made for socio-demographic characteristics. and occupational
RESULTS
Response rates
The response rate from the assertive outreach teams was 89% (187 of a total of 211 staff) and from the CMHT sample was 75% (114 out of 152 staff), giving a total of 301 respondents. Responses were obtained from 92% of the nurses in the teams (118 out of 128), 52% of the psychiatrists (27 out of 52), 83% of the social workers (63 out of 76), 81% of the clinical psychologists (13 out of 16), 96% of the occupational therapists (22 out of 23), all 36 community support workers and 85% of those whose occupation was classified as ‘other’ (22 out of 26). The ‘other’ category consisted mainly of staff designated as generic ‘assertive outreach’ workers, generally not qualified mental health professionals but with a variety of relevant experience. Data were not obtained regarding the occupations of six non-respondents. Among the psychiatrists, a much higher response rate was obtained in assertive outreach teams (15 out of 21, 71%) than in CMHTs (12 out of 31, 39%). Thus, psychiatrists in CMHTs are the group for whom the representativeness of our sample is most doubtful, with good response rates obtained from all other professions.
Staff socio-demographic and job details
Table 1 shows socio-demographic and job details for the assertive outreach team and CMHT staff. There was a highly significant difference in age distribution, the assertive outreach team staff being younger than the CMHT staff. The difference in ethnic group also reached statistical significance, with more staff from Black Caribbean, Black African and Black British backgrounds in the assertive outreach teams. A tendency for CMHTs to have more female workers just reached statistical significance, although account was not taken of multiple testing, and CMHT staff tended to have worked in mental health for slightly longer, reflecting their greater age. The CMHTs were made up predominantly of nurses, social workers and psychiatrists. The assertive outreach teams were more likely than the CMHTs to employ community or housing support workers and other non-professionally qualified staff. The CMHT staff worked mainly between 09.00 and 17.00 h Monday to Friday. Half of the assertive outreach team staff worked other patterns of hours or shifts. The proportion of staff with jobs split between different parts of the service was also investigated: 16% (30 out of 186) of assertive outreach team staff and 17% of the CMHT staff (18 out of 109) reported spending some sessions with another team. Their mean scores for the burn-out and satisfaction variables did not differ significantly from those whose sessions were wholly with the team involved in this study.
Table 1 Socio-demographic and job details of respondents
| Characteristic | Assertive outreach team staff (n=187) | Community mental health team staff (n=114) | Significance test |
|---|---|---|---|
| Gender (%) | |||
| Male | 94 (50.3) | 45 (39.5) | ϰ2=5.5 |
| Female | 93 (49.7) | 69 (60.5) | P=0.0261 |
| Age (%) | |||
| 18-25 years | 1 (0.5) | 4 (3.6) | ϰ2=6.3 |
| 26-35 years | 80 (42.8) | 30 (26.8) | P=0.00021 |
| 36-45 years | 74 (39.6) | 38 (33.9) | |
| 46-54 years | 30 (16.0) | 23 (20.5) | |
| 55+ years | 2 (1.1) | 17 (15.2) | |
| Ethnicity (%) | |||
| White UK, Irish or European | 116 (62.4) | 76 (66.7) | |
| Black African, Black Caribbean or Black | 42 (22.6) | 11 (9.7) | ϰ2=4.2 |
| British | P=0.00951 | ||
| Asian | 17 (9.1) | 18 (15.8) | |
| Mixed or ‘other’ | 11 (5.9) | 9 (7.9) | |
| Occupation (%) | |||
| Nursing | 65 (34.8) | 53 (46.5) | |
| Social work | 32 (17.1) | 31 (27.2) | |
| Occupational therapy | 18 (8.9) | 5 (4.4) | ϰ2=5.7 |
| Psychiatry | 15 (8.0) | 12 (10.5) | P=0.00021 |
| Clinical psychology | 5 (2.7) | 8 (7.0) | |
| Community/housing support | 32 (17.1) | 4 (3.5) | |
| Other | 21 (11.2) | 1 (0.9) | |
| Experience (mean (s.d.)) | |||
| Mean no. of years in current team | 2.0 (2.5) | 3.3 (4.6) | P=0.0332 |
| Mean no. of years in current type of team | 2.1 (2.1) | 5.4 (5.2) | P <0.00052 |
| Mean no. of years worked in a mental health service | 10.4 (7.1) | 13.6 (9.6) | P=0.0222 |
| Position in team (%) | |||
| Team leader, deputy or consultant | 36 (19.4) | 20 (17.9) | ϰ2=0.16 |
| Other mental health worker | 150 (80.7) | 92 (82.1) | P=0.691 |
| Pattern of work (%) | |||
| Within office hours (Monday-Friday, 09.00-17.00 h) only | 93 (50.3) | 93 (83) | ϰ2=41.9 |
| P=0.0061 | |||
| Shifts, including some evenings and/or weekends but no overnight work | 65 (35.1) | 13 (11.6) | |
| Shifts, including some evenings and weekends; on call overnight by telephone only | 21 (11.4) | 1 (0.9) | |
| Shifts, including evenings, weekends and overnight | 1 (0.5) | 4 (3.6) | |
| Other | 5 (2.7) | 1 (0.9) |
Satisfaction and burn-out
Mean scores
Table 2 shows the mean job satisfaction and burn-out scores for assertive outreach team and CMHT staff. For the Job Diagnostic Survey, a mean score on a seven-point scale is calculated, with 1 indicating severe dissatisfaction, 7 indicating a very high level of satisfaction and 4 indicating neither overall satisfaction nor dissatisfaction with work. In both types of team, staff appeared on average fairly, but not highly, satisfied with their work. For the Minnesota score, a neutral attitude is indicated by scores of 60 for overall satisfaction, 18 for extrinsic satisfaction and 36 for intrinsic satisfaction, so again attitudes to work were mildly positive. No clear evidence emerged of a difference between assertive outreach teams and CMHTs for satisfaction.
Table 2 Means and confidence intervals for satisfaction and burn-out: comparison between assertive outreach and community mental health teams

| Measure | Assertive outreach team staff (n=187) mean (95% CI)1 | Community mental health team staff (n=114) mean (95% CI)1 | p 2 |
|---|---|---|---|
| Job Diagnostic Survey | |||
| Global satisfaction | 5.1 (4.6-5.5) | 4.7 (4.4-5.0) | 0.14 |
| Minnesota Satisfaction Scale | |||
| General job satisfaction | 70.8 (68.0-73.6) | 70.9 (69.5-72.3) | 0.94 |
| Intrinsic satisfaction | 42.5 (40.8-44.2) | 42.2 (41.4-43.0) | 0.73 |
| Extrinsic satisfaction | 20.8 (19.9-21.7) | 21.2 (20.6-21.8) | 0.41 |
| Maslach Burnout Inventory | |||
| Emotional exhaustion | 17.4 (15.1-19.7) | 19.0 (16.3-21.7) | 0.42 |
| Depersonalisation | 4.4 (3.7-5.2) | 5.7 (4.2-7.1) | 0.12 |
| Personal accomplishment | 34.8 (33.8-35.8) | 32.7 (31.6-33.8) | 0.006 |
Maslach & Jackson (Reference Maslach and Jackson1986) categorised each dimension of burn-out into low, medium and high levels, producing standardised norms for various professions. According to their norms for mental health staff, high burn-out is characterised by a score of 21 or more on emotional exhaustion, 8 or more on depersonalisation and 28 or less on personal accomplishment. Average burn-out is indicated by 14–20 on emotional exhaustion, 5–7 on depersonalisation and 33–29 on personal accomplishment. Low burn-out is indicated by scores of 13 or less on emotional exhaustion, 4 or less on depersonalisation and 34 or more on personal accomplishment. For the emotional exhaustion component, the mean score was within the average range for both assertive outreach team and CMHT staff, with no evidence of a significant difference between them. For depersonalisation, the mean score was within the low range for assertive outreach teams and within the average range for CMHTs, but this difference did not quite reach statistical significance. For personal accomplishment, the mean for assertive outreach teams was in the low burn-out (i.e. high personal accomplishment) range, and for CMHTs it was in the average burn-out range, a difference that reached statistical significance.
Multivariate analysis
Table 3 shows the results from multiple regression analyses with burn-out and satisfaction scores as the dependent variables. It confirms a difference favouring assertive outreach staff in personal accomplishment and also suggests lower levels of depersonalisation among assertive outreach staff.
Table 3 Variables associated with satisfaction and burn-out scores in assertive outreach and community mental health teams
| Measure | Characteristics associated with measure at least at P=0.05 level | Regression coefficient (95% CI) | P | R 2 for model |
|---|---|---|---|---|
| Job Diagnostic Survey Global satisfaction | Occupational therapist (greater satisfaction) | 0.87 (0.12 to 1.62) | 0.03 | 0.13 |
| Time as mental health worker (greater satisfaction with longer career) | 0.04 (0.01 to 0.08) | 0.02 | ||
| Time in current post (less satisfaction with longer time in post) | −0.07 (−0.12 to −0.01) | 0.02 | ||
| Minnesota Satisfaction Scale General job satisfaction | Psychiatrist (greater satisfaction) | 5.2 (0.2 to 10.1) | 0.04 | 0.14 |
| Mixed or ‘other’ ethnic group (poorer satisfaction) | −6.4 (−11.3 to −1.4) | 0.01 | ||
| Intrinsic satisfaction | Psychiatrist (greater satisfaction) | 4.0 (1.0 to 6.9) | 0.01 | 0.15 |
| Mixed or ‘other’ ethnic group (poorer satisfaction) | −4.4 (−7.6 to −1.2) | 0.01 | ||
| Time as mental health worker (greater satisfaction with longer career) | 0.14 (0.0 to 0.28) | 0.05 | ||
| Extrinsic satisfaction | No independent variables significantly associated | |||
| Maslach Burnout Inventory Emotional exhaustion | Black ethnic group (less exhaustion) | −6.4 (−10.4 to −2.5) | 0.002 | 0.17 |
| Psychiatrist (less exhaustion) | −5.0 (−9.2 to −0.8) | 0.02 | ||
| ‘Other’ occupation (less exhaustion) | −4.9 (−9.7 to 0.0) | 0.05 | ||
| Time as mental health worker (less exhaustion with longer career) | −0.28 (−0.56 to 0.0) | 0.05 | ||
| Time in current post (more exhaustion with longer in post) | 0.62 (0.13 to 1.1) | 0.02 | ||
| Depersonalisation | Female (less depersonalisation) | −1.3 (−2.2 to −0.5) | 0.003 | 0.21 |
| Psychologist (less depersonalisation) | −3.2 (−5.6 to −0.9) | 0.008 | ||
| ‘Other’ occupation (less depersonalisation) | −1.7 (−3.5 to −0.06) | 0.04 | ||
| Assertive outreach team member (less depersonalisation) | −1.7 (−3.1 to −0.4) | 0.01 | ||
| Black ethnic group (less depersonalisation) | −2.0 (−3.6 to −0.3) | 0.02 | ||
| Aged over 55 years (less depersonalisation) | −8.3 (−15.7 to −1.0) | 0.03 | ||
| Time in current post (more depersonalisation with longer in post) | 0.24 (0.04 to 0.44) | 0.02 | ||
| Time as mental health worker (less depersonalisation with longer career) | −0.11 (−0.20 to −0.01) | 0.04 | ||
| Personal accomplishment | Assertive outreach team member (greater personal accomplishment) | 1.8 (0.4 to 3.2) | 0.01 | 0.08 |
| Community/housing support worker (greater personal accomplishment) | 3.1 (0.2 to 6.0) | 0.04 | ||
| ‘Other’ occupation (greater personal accomplishment) | 4.5 (1.3 to 7.8) | 0.008 |
Variation among teams
Figure 1 indicates that, although the overall means were similar for emotional exhaustion for assertive outreach teams and CMHTs, the way in which the individual team means were distributed differed. For CMHTs, seven out of nine teams had mean scores within the average burn-out category, with only two teams in the high category, whereas assertive outreach teams were more widely distributed between categories, with 7 out of 24 falling in the low burn-out category but 9 out of 24 in the high burn-out category. This pattern was not repeated for the other two components of burn-out.
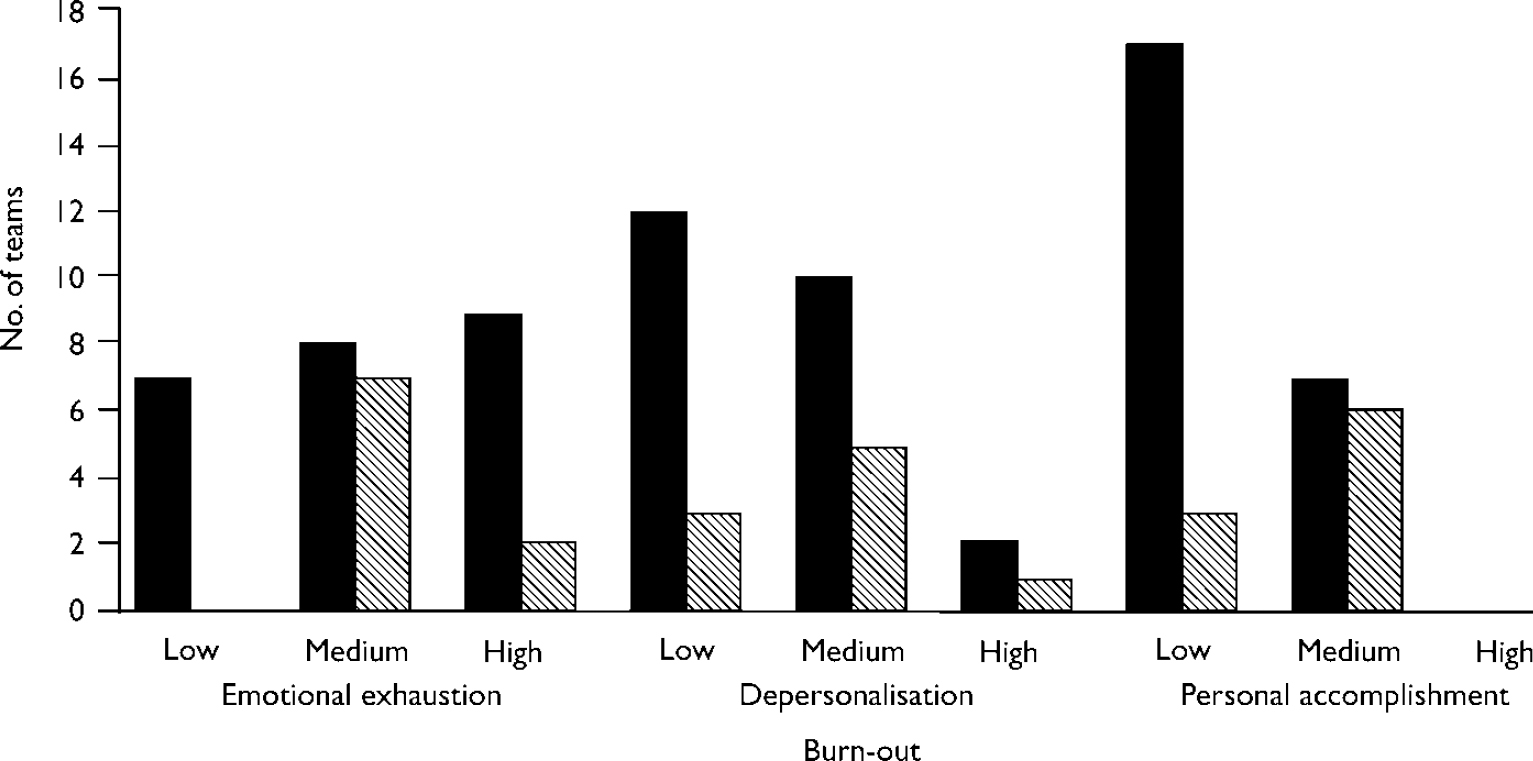
Fig. 1 Burn-out scores across the teams (▪, assertive outreach teams; ▧, community mental health teams). Staff are categorised as low burn-out for the personal accomplishment component if they have high scores on this component.
Variations among team clusters
Table 4 shows the results of comparing satisfaction and burn-out between assertive outreach teams belonging to the three clusters identified in the Pan-London Assertive Outreach Study (see Reference Wright, Burns and JamesWright et al, 2003, this issue). Teams in clusters A and B have full responsibility for patients' care and offer integrated health and social care. Cluster A teams have more psychiatric input and dedicated in-patient beds, lower case-loads per staff member and more contacts outside office hours than teams in cluster B. Cluster C teams are all non-statutory, have no dedicated beds or psychiatric input, tend to be smaller and have the highest frequency of in vivo contact. Initial comparison of burn-out and satisfaction between teams suggested that they differed significantly on all Minnesota Satisfaction Scale sub-scores and on the emotional exhaustion component of burn-out, with cluster A teams tending to be more satisfied and less burnt out. When adjustment was made for potential confounders, no cluster was significantly different from the others for the general and intrinsic Minnesota Satisfaction Scale scores. However, membership of a cluster B team appeared to be associated with greater emotional exhaustion and a lower score for extrinsic job satisfaction. This was also reflected in the distribution of team means for emotional exhaustion. Three of the fourteen cluster A teams, all four cluster B teams and two of the six cluster C teams made up the nine teams with mean emotional exhaustion scores in the high range.
Table 4 Differences between assertive outreach team types in burn-out and job satisfaction scores
| Measure | Cluster A team staff (n=125) (mean, 95% CI) | Cluster B team staff (n=31) (mean, 95% CI) | Cluster C team staff (n=31) (mean, 95% CI) | P |
|---|---|---|---|---|
| Job Diagnostic Survey | ||||
| Global satisfaction | 5.3 (4.6-5.9) | 4.9 (4.2-5.6) | 4.7 (4.1-5.2) | 0.341 |
| Minnesota Satisfaction Scale | ||||
| General job satisfaction | 72.8 (69.6-76.1) | 66.8 (62.0-71.6) | 66.7 (63.9-69.6) | 0.0191 |
| Regression coefficient and P value adjusted for | Reference category | −4.6 (−11.0 to 1.8) | −3.7 (−9.6 to 2.1) | 0.26 |
| potential confounders (CI) 2 | P=0.15 | P=0.20 | ||
| Intrinsic satisfaction | 43.7 (41.8-45.6) | 41.0 (37.6-44.4) | 39.3 (37.6-41.0) | 0.00631 |
| Regression coefficient and P value adjusted for | Reference category | −1.7 (−6.1 to 2.8) | −2.5 (−6.2 to 1.1) | 0.34 |
| potential confounders (CI) 2 | P=0.44 | P=0.16 | ||
| Extrinsic satisfaction | 21.5 (20.5-22.5) | 18.9 (17.5-20.3) | 19.8 (18.8-20.7) | 0.00951 |
| Regression coefficient and P value adjusted for | Reference category | −2.4 (−4.2 to −0.6) | −1.4 (−3.3 to 0.5) | 0.034 |
| potential confounders (CI) 2 | P=0.01 | P=0.15 | ||
| Maslach Burnout Inventory | ||||
| Emotional exhaustion | 16.0 (13.3-18.7) | 22.0 (20.6-23.3) | 18.4 (13.7-23.1) | 0.00131 |
| Regression coefficient and P value adjusted for | Reference category | 6.2 (3.2 to 9.0) | 4.1 (−1.7 to 9.9) | 0.0011 |
| potential confounders (CI) 2 | P<0.0005 | P=0.16 | ||
| Depersonalisation | 4.4 (3.3-5.4) | 4.7 (4.0-5.5) | 4.4 (3.0-5.7) | 0.791 |
| Personal accomplishment | 34.8 (33.5-36.2) | 34.3 (32.6-36.0) | 35.1 (32.8-37.5) | 0.831 |
Sources of satisfaction and stress
Figure 2 shows the profiles of sources of job satisfaction for the assertive outreach teams and CMHTs. Zero indicates that the aspect of work concerned is not a source of satisfaction at work, 1 indicates a minor source, 2 indicates a moderate source, 3 indicates an important source and 4 indicates a very important source. The profiles are strikingly similar, with the assertive outreach team staff recording slightly higher satisfaction levels in all areas. When t-tests were used to investigate whether differences were significant, the three areas rated as more important sources of satisfaction by assertive outreach teams were salary (t=2.9, P=0.004), making a contribution to the overall service provided by the team (t=4.4, P<0.00005) and working mainly with patients whose mental health and social problems were severe (t=3.0, P=0.003) (Bonferroni correction applied for multiple testing regarding sources of satisfaction; adjusted threshold for statistical significance P=0.005). The three areas of potential satisfaction that are specific to assertive outreach teams – the team approach to patients, small case-loads and working in an innovative type of team – all attracted high ratings.

Fig. 2 Mean ratings for sources of satisfaction for assertive outreach team (▪) and community mental health team (▧) staff. NHS, National Health Service; SMI, severe mental illness.
Figure 3 illustrates the profiles for sources of job stress for the assertive outreach team and CMHT staff, rated in the same way. Again, the overall pattern is very similar. Areas where the two types of team differed significantly were lack of support from senior staff in the service, rated as more important by assertive outreach team staff (t=3.3, P=0.0009), and working with people with dual diagnosis (t=3.0, P=0.003), with patients whose clinical and social problems are severe (t=2.9, P=0.004) and with difficult-to-engage patients (t=4.5, P<0.00005), all rated as more significant sources of stress by CMHT staff (Bonferroni correction applied; threshold for significance P=0.003).
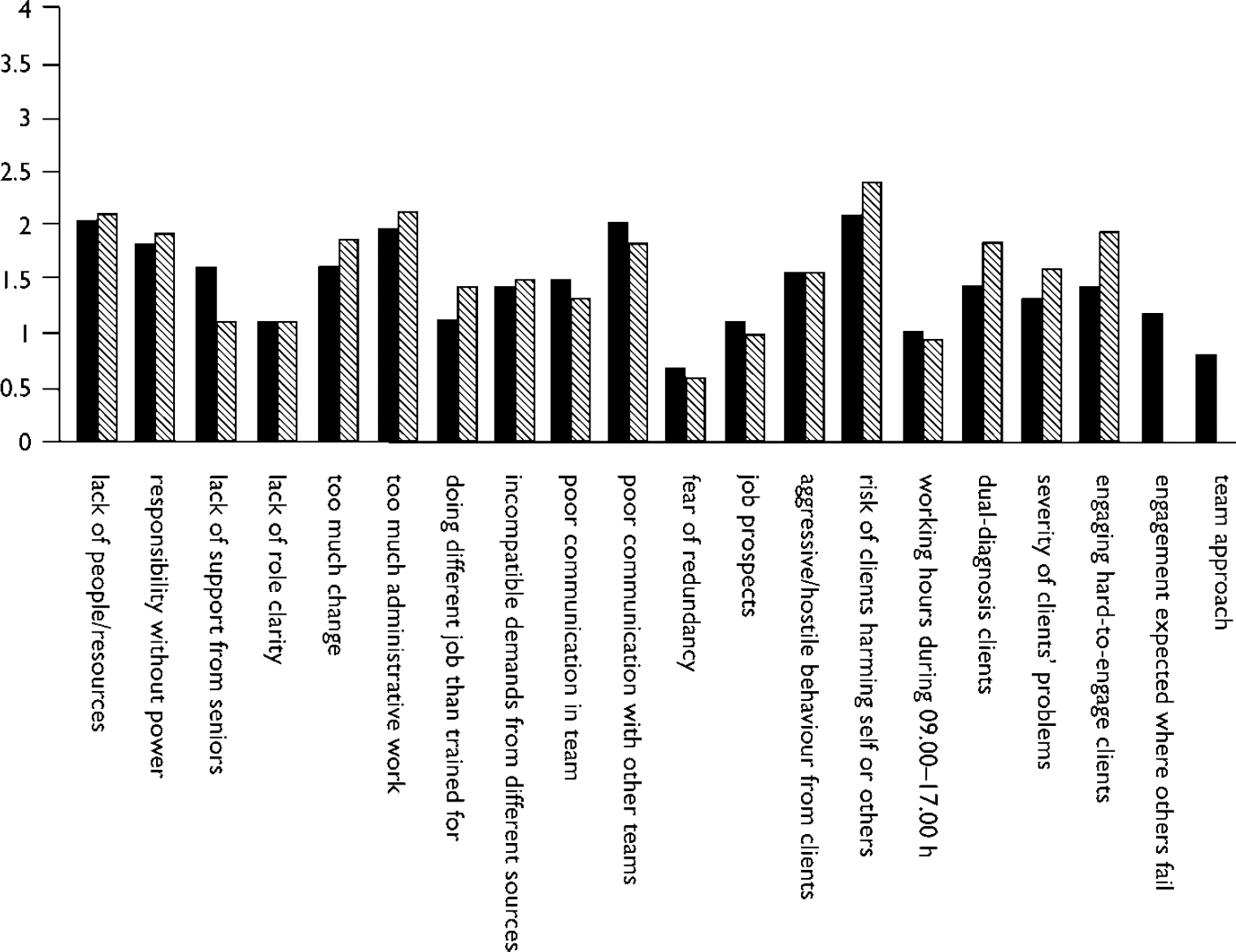
Fig. 3 Mean ratings for sources of stress for assertive outreach team (▪) and for community mental health team (▧) staff.
Training
Respondents were asked to rate how satisfactory their training had been in ten areas. Ratings were on a scale of 1–3: 1, no or very inadequate training; 2, some training, but with important gaps; and 3, a satisfactory amount of training. Staff also had the option of saying that a particular type of training was not relevant for them: these responses are not included in Table 5 but at least 90% of the sample regarded each listed aspect of training as relevant for their work, except for physical health problems, which 86% saw as relevant.
Table 5 Staff rating of training received

| Area of training | Rating: how far does training meet needs? | Assertive outreach team staff | Community mental health team staff |
|---|---|---|---|
| Techniques for outreach for difficult-to-engage patients | Satisfactory | 99 (58%) | 25 (25%) |
| Some gaps | 38 (22%) | 28 (28%) | |
| Very inadequate | 33 (19%) | 46 (47%) | |
| Assessing risk | Satisfactory | 116 (68%) | 55 (49%) |
| Some gaps | 45 (25%) | 43 (38%) | |
| Very inadequate | 17 (10%) | 14 (13%) | |
| Managing risk | Satisfactory | 102 (58%) | 49 (44%) |
| Some gaps | 55 (31%) | 52 (47%) | |
| Very inadequate | 19 (11%) | 10 (9%) | |
| Working with patients with a dual diagnosis of substance misuse and severe mental illness | Satisfactory | 53 (30%) | 27 (24%) |
| Some gaps | 71 (41%) | 46 (41%) | |
| Very inadequate | 53 (30%) | 38 (34%) | |
| Working with patients' families | Satisfactory | 72 (41%) | 40 (37%) |
| Some gaps | 50 (29%) | 30 (28%) | |
| Very inadequate | 52 (30%) | 39 (36%) | |
| Working with patients to increase willingness to take medication | Satisfactory | 83 (49%) | 44 (41%) |
| Some gaps | 50 (30%) | 35 (32%) | |
| Very inadequate | 35 (21%) | 29 (27%) | |
| Helping patients to develop ways of coping with distressing symptoms such as hallucinations and paranoid thoughts | Satisfactory | 70 (40%) | 45 (41%) |
| Some gaps | 74 (42%) | 41 (37%) | |
| Very inadequate | 32 (18%) | 25 (23%) | |
| Providing advice and help regarding benefits entitlements, housing and other social problems | Satisfactory | 64 (38%) | 28 (28%) |
| Some gaps | 59 (35%) | 25 (25%) | |
| Very inadequate | 47 (28%) | 49 (48%) | |
| Physical health care | Satisfactory | 74 (48%) | 43 (41%) |
| Some gaps | 45 (29%) | 31 (30%) | |
| Very inadequate | 36 (23%) | 30 (29%) | |
| Working with patients on a team rather than an individual basis | Satisfactory | 105 (61%) | Not applicable |
| Some gaps | 39 (23%) | ||
| Very inadequate | 28 (16%) |
Table 5 indicates that a large variety of responses was obtained for most items. In all but one of the areas, more assertive outreach team than CMHT staff felt that they had received adequate training for their job. For assertive outreach team staff, the three areas in which they were most likely to feel that their training was very inadequate were: working with patients with dual diagnosis of substance misuse and severe mental illness; working with patients' families; and giving advice regarding housing, benefits and other social problems. The CMHT staff felt that the most important gaps in their training were with regard to advice on housing and benefits, assertive outreach techniques for the difficult-to-engage patients and working with families, with dual diagnosis close behind.
Supervision
A total of 176 (95%) of the assertive outreach team staff and 112 (98%) of the CMHT staff had a named supervisor. Among the assertive outreach staff, only 14 (8%) met with their supervisor at least weekly, 54 (30%) met at least once per fortnight but less than once per week, 106 (59%) met less often than once per fortnight and 7 (4%) did not meet at all. Among the CMHT staff, 12 (11%) met with their supervisor at least weekly, 37 (33%) met at least once per fortnight but less than weekly, 61 (54%) met less than once per fortnight and 3 (3%) did not meet at all.
Staff satisfaction with six aspects of supervision was also assessed. There was little difference between the assertive outreach team and CMHT staff on any measure. The modal response in each area was that the supervisor provided as much help as needed.
DISCUSSION
Limitations
The generalisability of our findings is limited by the fact that the study was carried out exclusively in a large metropolitan area with distinctive staff characteristics, clinical populations and working conditions that are not likely to be representative of the UK as a whole, or indeed of other countries where assertive outreach teams operate. Although the staff were given strong assurances of confidentiality, they may have been reluctant to disclose their most negative thoughts about patients and their work to researchers with obvious connections with local medical schools, particularly as they were aware that patient outcomes also were being evaluated in the Pan-London Assertive Outreach Study. All London assertive outreach teams in operation at the beginning of the study period were included and their response rate was high, so findings are likely to be highly representative of these teams. However, representativeness may be less good for the CMHTs: the response rate was lower and their similarity to London CMHTs in general was not ascertained. The CMHT psychiatrists were particularly poorly represented. Although levels of satisfaction and burn-out were measured using well-established instruments with known psychometric properties, our measures in other areas had to be devised or adapted for the study.
Main findings
Overall, the findings are moderately encouraging both for assertive outreach teams and for CMHTs. In most of the teams surveyed, levels of satisfaction are fairly good and burn-out is moderate or low. A notable finding is that the high levels of emotional exhaustion reported from CMHTs in the studies of the 1990s have not, on the whole, been replicated in this study. For example, Prosser et al (Reference Prosser, Johnson and Kuipers1996) reported, from a survey of CMHT staff carried out in South London in 1994, a mean score for emotional exhaustion of 27.4, compared with 19.0 for CMHT staff in our study. It would be of interest to discover whether this lower burn-out score can be replicated in other current CMHT samples. Possible explanations for a reduction in emotional exhaustion include CMHT staff having experienced less change recently than during the extensive national and local mental health policy changes of the 1990s (Reference PeckPeck, 1999), increased resources for mental health care and newly established assertive outreach teams relieving CMHTs of some of the patients they find most difficult to manage. In the longitudinal study conducted by Prosser et al (Reference Prosser, Johnson and Kuipers1999), a trend towards diminishing emotional exhaustion as teams became established in the community was noted, and this may have persisted.
Differences in burn-out and satisfaction between assertive outreach teams and CMHTs are not strikingly large but there is evidence of differences favouring assertive outreach team members for some aspects of burn-out. Ratings regarding sources of stress and satisfaction also suggest more positive views about work among assertive outreach team members. Thus, the gloomy prognosis predicted by some authors for models of care that involve very intensive working with a case-load of difficult-to-engage patients with severe social and clinical problems does not seem to have been realised in London. There is, however, an important caveat: although the mean emotional exhaustion score for London assertive outreach team staff overall is in the average range, it falls into the ‘high’ range for just over one-third of teams, and the variation between teams seems to be very large, suggesting the sustainability of certain teams may be at risk. Emotional exhaustion and job satisfaction scores for the cluster B assertive outreach teams are of particular concern. The Pan-London Assertive Outreach Study data on the case-loads of each team type (see Reference Priebe, Fakhoury and WattsPriebe et al, 2003, this issue) indicate that patients on cluster B team case-loads resemble cluster A patients in clinical and social characteristics such as diagnosis, history of hospitalisation and compulsory admission and substance misuse. Like cluster A teams, they take full responsibility for patients' clinical and social care. However, in terms of staff case-load size, availability of a psychiatrist within the team and of dedicated beds and extent to which they work outside usual office hours, they are less well-resourced than cluster A teams. This may make the severe clinical and social problems of their patients more difficult and stressful to manage. Thus, our findings suggest that, from the point of view of staff well-being and therefore of team sustainability, setting up assertive outreach teams with such a combination of high case-load severity and limited resources and model fidelity may be inadvisable.
With regard to other socio-demographic and occupational variables associated with satisfaction and burn-out on multivariate analysis, the exploratory nature of the analysis and the relative weakness of most associations need to be emphasised. The two measures of satisfaction, one based on global ratings and the other on summed ratings for specific aspects of work, yielded different models and most associations were quite weak so that the explanatory power of these models is limited. With regard to burn-out, the lower levels among people from Black Caribbean, Black African and Black British backgrounds replicate previous work in the UK (Reference Prosser, Johnson and KuipersProsser et al, 1999) and with Black Americans (Reference Maslach and JacksonMaslach & Jackson, 1986), although the basis of this difference is unclear. A longer career in mental health services is associated with less burn-out on two components, which may reflect an earlier departure from clinical work among mental health professionals who become burnt out. The observation that length of service in current post is associated with more burn-out on two measures sounds a note of caution about the prognosis for these teams, because most assertive outreach teams are still relatively newly established (see Reference Wright, Burns and JamesWright et al, 2003, this issue).
Factors rated as the most important sources of satisfaction and stress follow very similar patterns in both team types. Some sources of stress that might be expected to be particularly salient for assertive outreach teams, such as dual diagnosis, difficult-to-engage patients and high severity of clinical and social problems, are, in fact, rated as more important by CMHT staff than by assertive outreach staff. This suggests that these problems may be less daunting when working within the assertive outreach team framework with appropriate training and a small case-load, although it may also indicate that staff who choose to work in an assertive outreach team are those who do not experience these difficulties as very stressful. The aspects of work that are peculiar to the assertive outreach team model (the team approach, working in an innovative service, small case-loads and working to engage patients who have not engaged in other parts of the system) tend to be rated as important as sources of satisfaction but not of stress, again suggesting that staff working in assertive outreach teams are relatively happy with the model.
Clinical implications
Although most assertive outreach teams are at too early a stage of development for the long-term outlook for their staff to be established with certainty, our findings indicate that this model can be introduced without effects on staff that threaten its sustainability. This may not apply, however, to teams that take full clinical responsibility for a case-load with severe clinical and social problems but have limited medical time and lack access to dedicated in-patient beds and out-of-hours service provision. The mechanisms underlying high levels of burn-out in certain teams and the ways in which these may be alleviated warrant further investigation. Many staff in CMHTs and assertive outreach teams identify multiple areas in which they feel their training does not meet their needs. Our survey suggests that training in interventions with patients with dual diagnoses and patients' families, and training regarding the benefits system and other elements in the social care system, would be valued in both CMHTs and assertive outreach teams. The high proportion of assertive outreach staff who rate their training regarding dual diagnosis as inadequate is of concern, given the high rates of comorbid substance misuse identified in the Pan-London Assertive Outreach Study of assertive outreach team clients (see Reference Priebe, Fakhoury and WattsPriebe et al, 2003, this issue). Many CMHT staff feel that they need training in the interventions for difficult-to-engage patients that are employed in assertive outreach teams.
APPENDIX
Members of the Pan-London Assertive Outreach Study Group
Tom Burns, Christine Wright, Peter James, Adele Greaves, Christine Benfell, Nan Greenwood (St George's Hospital Medical School); Paul Bebbington, Sonia Johnson, Joanne Billings (University College London and Camden and Islington Mental Health and Social Care Trust); Stefan Priebe, Walid Fakhoury, Joanna Watts (Unit for Social and Community Psychiatry, Barts' and The London School of Medicine); Matt Muijen, Iain Ryrie, Rebecca Walwyn (Sainsbury Centre for Mental Health); Ian White (Medical Research Council Biostatistics Unit).
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Staff in London's assertive outreach teams are fairly satisfied with their jobs and most are not experiencing high levels of burn-out. However, just over one-third of the teams have team means in the high range for the ‘emotional exhaustion’ component of burn-out.
-
▪ Comparing community mental health and assertive outreach teams, levels and sources of stress and satisfaction are fairly similar but evidence on certain measures suggests that well-being at work may be greater among assertive outreach team staff.
-
▪ There is a wide range of views among assertive outreach team staff on the adequacy of their training. Dual diagnosis of substance misuse and severe mental illness, working with families and giving advice on housing and benefits were the areas in which staff most often felt that they had major unmet training needs.
LIMITATIONS
-
▪ All staff surveyed were working in London, where working conditions and case-loads may be atypical in important ways.
-
▪ Most teams studied are relatively new, so evidence from the study on the longer-term effects of working in an assertive outreach team is limited.
-
▪ Staff may have been wary of disclosing their true feelings about work, especially in a study in which patient outcomes also were being evaluated.
Acknowledgements
We thank those who were involved in the development of the study: Peter Tyrer, Kevin Gournay, Graham Thornicroft, Tom Craig and Angela Greatley. This study was also developed and carried out partly under the auspices of The London Mental Health Virtual Institute for Research and Development (LoMHR&D).











eLetters
No eLetters have been published for this article.