The challenge of obesity to the health of Western society has been clearly identified by the World Health Organization (WHO)(1), which also recognises that maintenance of a healthy weight is in itself as large a challenge as obesity. In the UK, the Department of Health’s publication, Choosing Health: Making Healthy Choices Easier, aimed to improve the understanding of the increasing rise in the overweight and obese population in the UK and from this numerous strategies and networks are being developed to reduce the prevalence of an obese population(2). Guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children was published by the National Institute for Clinical Excellence (NICE) in December 2006. The first two NICE dietary guidelines for healthy weight maintenance recommend(3):
• Base meals on starchy foods such as potatoes, bread, rice and pasta, choosing whole grains wherever possible;
• Eat plenty of fibre-rich foods – such as oats, beans, peas, lentils, grains, seeds, fruit and vegetables, as well as whole-grain bread and brown rice and pasta.
The recent Dietary Guidelines for Americans(4) state that 3 or more ounce equivalents of whole-grain products should be consumed per day (with the rest of the recommended grains coming from enriched or whole-grain products) and whole-grain intake is also emphasised in advice given by WHO(5). Its guidelines include promoting healthy behaviours to encourage, motivate and enable individuals to lose weight by eating more fruit and vegetables, as well as nuts and whole grains. In summarising the totality of evidence of factors that may protect or be causative in obesity and weight management, WHO adopted an assessment of data which described evidence as being convincing, probable, possible and insufficient. It concluded that convincing evidence existed to suggest that high intake of energy-dense, micronutrient-poor foods was associated with obesity. It promoted the intake of foods low in energy density, i.e. energy-dilute foods such as fruit, vegetables and whole-grain cereals that are high in dietary fibre and water. The relationship between dietary fibre and body weight (BW) has been explored in two reviews of randomised trialsReference Pereira and Ludwig(6, Reference Howarth, Saltzman and Roberts7), which concluded that the majority of studies show that a high intake of non-starch polysaccharides (NSP dietary fibre) promotes weight loss. While this relationship between fibre and BW has been extensively studied, the relationship between whole grains and BW has not received the same degree of scientific scrutiny.
It has been argued that the beneficial role of whole grains in the diet exceeds the provision of dietary fibreReference Seal(8–Reference Anderson10), but its specific role and the mechanisms involved in weight management have been little researched. A brief review of whole-grain consumption and weight gain conducted in 2003Reference Koh-Banerjee and Rimm(11) concluded that epidemiological data were sparse. Indeed, evidence from randomised controlled trials is also limited. To this end in the UK the Food Standards Agency has commissioned two large intervention studies which aim to provide mechanistic evidence for whole grains and cardiovascular disease, but also to underpin public health strategies related to whole grainsReference Seal(8).
The awareness of the potential public health benefits from the inclusion of whole grains in the diet was raised with the publication of health claims in the USA(12), UK and SwedenReference Richardson(13) and has led to more information about whole grains being published in recently reported epidemiological studies.
The objective of the present study was to review the scientific literature relating to whole-grain intake and its effect on healthy BW and adiposity, exploring the weight and strength of the evidence that exists. Clearly important public health recommendations are already being made with regard to whole-grain consumption; its inclusion in the diet offers an attractive and food-based dietary strategy for targeting the whole population. However, it is important to better understand the scientific evidence that supports its inclusion in diets for a healthy BW and whether it can be promoted as a marker of healthy BW.
Materials and methods
Searching
Computerised scientific publication databases were searched. The search was focused on Medline (www.ncbi.nlm.nih.gov/entrez/query.fcgi) for the period 1990 to December 2006 and complemented by searches in EMBASE and hand search of key papers and publications. In addition, the reference lists in identified papers were scrutinised for further studies. Search terms were ‘wholegrain or whole grain’ and ‘obesity or body weight or BMI or body fat’ in Medline, and with the addition of ‘body measures’ in EMBASE. The search was limited to human studies and those published in English or with a summary in English. The initial search was conducted by the British Library and complemented by hand searches conducted by the authors.
Identification and selection of studies
The main objective was to systematically review observational studies published since 1990 in which BW and whole-grain intake of volunteers had been assessed by suitable methods. The aim was to compare a nil or low consumption of whole grains with a much higher intake, preferably about three servings per day. In studies reporting whole-grain intake in grams, the equivalent intake was approximately 48 g/d.
The broad criteria for study inclusion were the following.
• Original epidemiology research: cohort, cross-sectional or case studies in humans reported in full in peer-reviewed journals.
• Clear definition and measurement of whole grains.
• Use of suitable measures of BW maintenance: for example, body mass index (BMI), waist circumference (WC) or waist:hip ratio (WHR).
• Reports that measured a range of whole-grain intakes in comparable populations – preferably a group with no or very low whole-grain intake that could be compared with a population consuming about three servings per day or more – and that employed a suitable measure of BW or adiposity.
Duplicates of the same cohort or study were excluded, with the most recent report included. This review and analysis were conducted following the principles for systematic review of observational studies detailed by Stroup et al.Reference Stroup, Berlin, Morton, Olkin, Williamson, Rennie, Moher, Becker, Sipe and Thacker(14). The review was conducted by both authors and differences resolved by detailed discussion.
Data abstraction and quality assessment
The key characteristics of the studies were abstracted and the findings collated, which included: identification of the number of volunteers, gender, age, location and duration of study, measurements of BW or adiposity, macronutrient content of the diet (where available), definition of ‘whole-grain’ and method of assessment of intake. The data abstracted were subject to quality assessment in three main areas:
• recruitment and flow of subjects through the study;
• dietary assessment including definition of ‘whole-grain’;
• treatment and reporting of data.
Analysis of appropriate subgroups resulted from this assessment. Where data were not available in the published paper the authors were contacted requesting the necessary detail.
Definition of whole-grain foods
Definition of ‘whole-grain’ is problematic, with definitions varying in different countries. The US Food and Drug Administration permits health claims on foods that contain at least 51 % of whole grains (including milled products of whole grains). The most commonly used definition in research defines whole-grain intake from products containing 25 % or more of whole grainsReference Jacobs, Marquart, Slavin and Kushi(15). However, using data derived from the National Diet and Nutrition Survey (NDNS) in young people aged 4–18 years, it has been shown that defining whole-grain foods as those containing at least 51 % of whole grains underestimates whole-grain intake by 28 %Reference Thane, Jones, Stephen, Seal and Jebb(16); lowering the threshold to ≥25 % content of whole grains to define whole-grain foods reduces underestimation to 15 %, when compared with a definition based on foods containing ≥10 %.
In addition to inconsistent definition of whole-grain intake, servings frequently used as a measure in food-frequency questionnaires (FFQs) also vary in amount. Consequently, it was considered to be impossible to confine the review to a single definition; instead attention was focused on reports where a wide range of whole-grain intake was reported between high and low consumers. Some reports refer to intake of servings and others to intake in grams; where possible results are reported on the basis of servings per day. If total whole-grain servings were not reported, it was considered essential that either bread or breakfast cereal intake should be assessed as they are major sources of whole grains in both the UKReference Thane, Jones, Stephen, Seal and Jebb(16–Reference Lang and Jebb18) and the US dietReference Cleveland, Moshfegh, Albertson and Goldman(19).
Measures of weight maintenance
In the area of weight management, the usual measure to assess risk is BMI. It is defined as BW divided by the square of height and is reported in units of kg/m2. Obesity is defined as BMI ≥ 30 kg/m2, overweight as BMI ≥ 25 to <30 kg/m2 and healthy weight as BMI < 25 kg/m2 (reference 1). In earlier studies WHR was used to provide an indication of central adiposity, although a better and now more frequently used measure of adiposity is WC. Three categories each for men and women relate WC to obesity; for men these are <94 cm, ≥94 to <102 cm and ≥102 cm, and for women these are <80 cm, ≥80 to <88 cm and ≥88 cm. These equate to the healthy, overweight and obese categories of BMI. In the UK the higher two categories have been designated ‘action levels’ 1 and 2, corresponding respectively to slightly increased and substantially increased risk of chronic conditions such cardiovascular disease and diabetesReference Lean, Han and Seidell(20).
Statistical analysis
The key outcomes reported were mean values for BMI, WHR or WC from the lowest and highest whole-grain intake groups (usually about three servings per day). For computation of the pooled effect, each study was assigned a weight consisting of the reciprocal of its variance. Estimates of mean difference and 95 % confidence interval (CI) were calculated by using a random-effects model. The assumption of heterogeneity implied by the use of random-effects models is plausible because of the differences in amounts of whole-grain intake, study populations, study duration, initial BMI and the presence of other covariates. To explore the possible influence of these covariates further, pre-specified subgroup analysis was conducted based on quality assessment of studies and biological plausibility. Finally, to estimate potential publication bias, we plotted the standard error of the studies against their corresponding effect size to produce funnel plots. All statistical analyses were conducted using Comprehensive Meta Analysis statistical software package (Biostat, Englewood, NJ, USA).
A secondary outcome reported herein compares key aspects associated with a healthy lifestyle in the low and high consumption populations. The main lifestyle factors reported were smoking, activity level, macronutrient intake and alcohol intake. Mean values and standard error of the difference were calculated and subject to a Student’s t test assuming population variances not to be equal.
Results
Trial flow
Figure 1 outlines the results from the reported selection process. The search identified 115 papers; when abstracts were scanned and exclusion criteria applied, this resulted in 26 potentially relevant studies. After reading the full articles, 22 studies remained that excluded duplicate reports of the same cohort at different periods of follow-up. Exclusion of a further three reports that included inadequate detail or insufficient range of whole-grain intakes and three non-epidemiological studies resulted in 15 retained reportsReference Sahyoun, Jacques, Zhang, Juan and McKeown(21–35), two of which related to data not published in full (Good et al.(34) was a conference abstract, Thane et al.(35) was an Epublication ahead of print at the time of the search and analysis; both sets of authors provided further details as a personal communication). Details of the 15 retained papers containing cross-sectional data or reports of cohorts from which cross-sectional data were extracted are shown in Table 1.
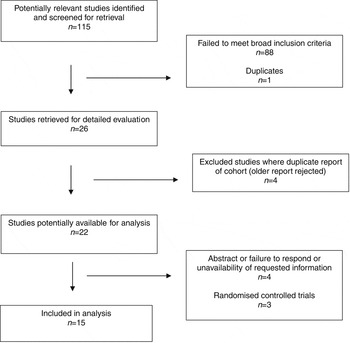
Fig. 1 Systematic review – flow of studies
Table 1 Details of the cohorts and cross-sectional data included in the present systematic review and analysis

WG, whole-grain/whole grains; BMI, body mass index; WCm, waist circumference in metres; WHR, waist:hip ratio; Wt, weight; Ht, height; M, males; F, females; NDNS, National Diet and Nutrition Survey; B, boys; G, girls; w, White; AA, African American; base, baseline; PHS, Physicians’ Health Study; TLGS, Tehran Lipid and Glucose Study; BP, blood pressure; CARDIA, Coronary Artery Risk Development in Young Adults; USDA, US Department of Agriculture; CSFII, Continuing Survey of Food Intakes by Individuals; HPFS, Health Professionals’ Follow-Up Study; NHS, Nurses’ Health Study; ARIC, Atherosclerosis Risk in Community; IWHS, Iowa Women’s Health Study; FDA, Food and Drug Administration; semi-quant, semi-quantitative; FFQ, food-frequency questionnaire.
* Method used to determine Wt and height Ht: measured independently (I), by self (S) or information not given (Ng).
† Data adjusted for following main factors: age (A), alcohol intake (AA), BMI, caffeine (C), dieting and eating behaviour (DE), dietary fibre intake (DF), disease history (DH), energy intake (E), education (Edu), specific foods (F), fat intake (Fa), gender (G), hypertension (H), hormone replacement therapy status (HRT), lipid-lowering or hypertensive medication (LipMed), marital status (MS), occupation (Occ), physical activity (PA), polyunsaturated fat intake (PF), race (R), refined grain intake at base and changes (RG), smoking (S), socio-economic status (SES), saturated fat intake (SF), multivitamin use (V), WC and Wt.
Study characteristics
Each report contained data from a single study with one exception, the study of Thane et al.(35), which included two separate sources, specifically the 1986/87 and 2000/01 NDNS. Information was presented by gender separately in three papersReference Jacobs, Meyer and Solvoll(32, 34, 35), with the result that 20 data pairs were available for analysis representing 119 829 subjects. Table 1 provides details of the main characteristics of the studies including BMI, WC and WHR.
All studies apart from twoReference Bazzano, Song, Bubes, Good, Manson and Liu(22, 34) reported energy intake. The key nutrient combinations reported were fat and/or saturated fat and dietary fibre intake, reported in nine studiesReference Esmaillzadeh, Mirmiran and Azizi(23–Reference Steffen, Jacobs, Murtaugh, Moran, Steinberger, Hong and Sinaiko29, Reference McKeown, Meigs, Liu, Wilson and Jacques31, Reference Jacobs, Meyer, Kushi and Folsom33). The main lifestyle factors reported were the proportion of subjects currently smoking and exercising regularly and alcohol consumption.
Analysis of main outcomes
The mean difference in BMI between the lowest and high intakes of whole grains for each of the 20 data pairs is shown in Fig. 2. The combined and weighted mean difference in BMI using a random-effects model resulted in a reduction of 0·630 kg/m2 when high whole-grain intake was compared with low or no whole-grain intake, P < 0·0001 (95 % CI 0·460, 0·800 kg/m2).

Fig. 2 Mean difference in body mass index (ΔBMI) in non- or low consumers of whole grains compared with high consumers of whole grains (95 % confidence interval shown by vertical bars)
Adiposity was assessed by comparison of the difference in either mean WC or WHR in the lowest and highest groups of whole-grain intake, see Fig. 3. WC (six data pairs, n = 4178) was reduced by 2·7 (95 % CI 0·2, 5·2) cm, P = 0·03, in high consumers of whole grains; WHR (four data pairs, n = 20 147) was reduced by 0·023 (95 % CI 0·016, 0·030), P < 0·0001.

Fig. 3 Mean difference (and 95 % confidence interval, CI) in waist:hip ratio (WHR) or waist circumference (WC) when low or no whole-grain intake is compared with high intake
Subgroup analysis
The introduction of more stringent exclusion criteria resulted in the exclusion of studies not reporting any dietary information (three data pairs) or where the intake of whole grains was less than about three servings per day (48 g/d). Additionally, attention was focused on gender and the effect computed for males and females separately, or study location where studies conducted in the USA were compared with those conducted in Europe. The results of subgroup analysis are shown in Table 2.
Table 2 Subgroup analysis of studies resulting from this systematic review

BMI, body mass index; CI, confidence interval.
The exclusion of studies which did not include dietary information or focusing on studies where intake was less than about three servings had little effect on the difference in BMI. There was a small gender difference; BMI reduction in women was marginally greater than in men. Geographic location had a small effect on the reduction in BMI, with BMI loss being marginally higher in the USA compared with Europe.
The mean nutrient intakes for the low and high whole-grain data sets are shown in Table 3. Higher whole-grain intake led to increased energy (1·80 MJ (431 kcal), P < 0·05) and dietary fibre intake (9 g, P < 0·01). Total and saturated fat intakes were reduced non-significantly by 10·1 g and 3·8 g respectively in the high intake group. Other aspects of healthy lifestyle that were reported in a consistent format were alcohol intake and number of smokers, which were both lower in the high whole-grain group, significantly so in the case of smokers, where there were 12·4 % fewer (P < 0·01). The proportion undertaking regular physical activity was increased by 11·4 % in the high whole-grain group, but this did not reach significance. Data relating to micronutrient intake or mineral supplementation were not reported with sufficient consistency to be collated, but where reported was generally higher or supplementation more prevalent in the higher whole-grain group.
Table 3 The associations between high or low intake of whole grains and mean energy, fat, saturated fat and fibre intake and various lifestyle factors

sed, standard error of the difference; NS, not significant.
Discussion
Epidemiological data have been used to suggest that the consumption of at least one serving of whole-grain foods each day is associated with a reduced risk of death from cardiovascular diseaseReference Jacobs, Meyer and Solvoll(32, Reference Jacobs, Meyer, Kushi and Folsom33, Reference Jensen, Koh-Banerjee, Hu, Franz, Sampson, Gronbaek and Rimm37, Reference Liu, Stampfer, Hu, Giovannucci, Rimm, Manson, Hennekens and Willett38) and reduced incidence of diabetesReference Montonen, Knekt, Jarvinen, Aromaa and Reunanen(28, Reference Pereira, Jacobs, Van Horn, Slattery, Kartashov and Ludwig39) and the metabolic syndromeReference Esmaillzadeh, Mirmiran and Azizi(23, Reference McKeown, Meigs, Liu, Saltzman, Wilson and Jacques40). Obesity is a risk factor for all of these conditions; hence it is perhaps not surprising that in this, the most complete systematic review of the epidemiological evidence reported to date, an association has been demonstrated between a higher whole-grain intake and BMI. This association is in agreement with the findings from two large cohort studies, the Nurses’ Study and Health Professionals’ Follow-Up StudyReference Koh-Banerjee, Franz, Sampson, Liu, Jacobs, Spiegelman, Willett and Rimm(26, Reference Liu, Willett, Manson, Hu, Rosner and Colditz27), both of which reported a reduction in weight gain over at least 7 years when whole-grain intake was about three servings per day. In addition there is limited evidence provided by short-term clinical trialsReference Melanson, Angelopoulos, Nguyen, Martini, Zukley, Lowndes, Dube, Fiutem, Yount and Rippe(41, Reference Saltzman, Das, Lichtenstein, Dallal, Corrales, Schaefer, Greenberg and Roberts42) that whole grains, when included in an energy-restricted diet, were at least as effective as other regimens.
The reduction reported in the subgroup analysis with about three whole-grain servings is 0·58 kg/m2 for BMI; waist circumference is about 2·7 cm less, equivalent to a reduction of approximately 3 % assuming an average waist circumference of 90 cm. While this reduction may in itself be quite modest, the healthy lifestyle factors (lower prevalence of smoking and greater participation in physical activity) associated with higher whole-grain consumption and the dietary changes (reduction in total and saturated fat, increased fibre intake and moderate alcohol consumption) add strength to public health messages encouraging its intake.
A further aspect that has previously been reported with reference to the NDNS 2000/01 is a greater micronutrient density in those consuming more whole-grain foods (Thane et al., personal communication).
Overall the findings are very much in line with anthropometric changes in adults reported when factor analysis of food patterns were used to predict BW and adiposity in the Baltimore Longitudinal Study of AgingReference Newby, Muller, Hallfrisch, Andres and Tucker(43).
The potential mechanism(s) by which whole grains result in a healthier weight is speculative. In both clinical trials and observational studies the intake of whole grains has been inversely associated with plasma biomarkers of obesity including insulin, C-peptide and leptin concentrationReference Fung, Rimm, Spiegelman, Rifai, Tofler, Willett and Hu(44). The key mechanisms involved appear to relate to the role that whole grains have on satiety and insulin sensitivity, and as a source of dietary fibre and antioxidants. It is speculatedReference Koh-Banerjee and Rimm(11) that whole grains or their components may influence hormonal factors; whether the active moiety is fibre or one of the micro-components, such as lignan or phytosterol, is not clear.
It has been suggested that there is no real mechanism of action and whole-grain consumption is simply a marker of a healthier lifestyle – that the benefits reported in epidemiological studies relate to the lower fat, higher carbohydrate and higher fibre intakes reported. However, this argument is not entirely plausible. Certainly reported intake of fruits and vegetables is generally higher and meat consumption lower in diets rich in whole grains, factors that would generally be considered beneficial to health and weight managementReference Newby, Muller, Hallfrisch, Andres and Tucker(43). However, when data from the Framingham Offspring CohortReference McKeown, Meigs, Liu, Wilson and Jacques(31) were adjusted for potential confounding variables and dietary factors associated with diets high in whole grains, the association between whole-grain intake and BMI or WHR – while attenuated – was still significant.
One of the main weaknesses of this analysis is the reliance on observational data. The unreliability of FFQs to determine food intake, in particular whole-grain foods which have been defined inconsistently over the years, does not enhance this case. In addition, half of the studies used in this analysis have relied on self-reported measures of height and weight. All studies cited have made some adjustment to the data, primarily age, gender and energy intake, but again the degree of sophistication of the models employed is highly variable.
A funnel plot (Fig. 4) was used to test for publication bias; study size (as measured by standard error) was plotted as a function of effect size. Generally, large studies appear towards the top of the plot and tend to cluster near the mean effect size. Smaller studies appear towards the bottom of the plot, and (since there is more sampling variation in effect size estimates in the smaller studies) will be dispersed across a range of values. As the studies appear to be distributed symmetrically about the combined effect size an absence of publication bias is suggested.
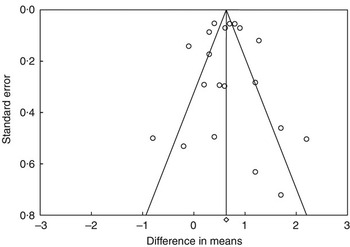
Fig. 4 Funnel plot of standard error by difference in means
Despite these various shortcomings the association between whole-grain intake and lower BW is highly significant (P < 0·0001) and is the result of the integration of a large number (20) of data pairs including about 120 000 subjects. The consumption of about three daily servings of whole grains is associated with lower BMI and central adiposity. In addition, people who consume more whole grains are likely to have a healthier lifestyle as fewer of them smoke, they exercise more frequently and they tend to have lower fat and higher fibre intake. The evidence identified supports the inclusion of whole grains in diets for the maintenance of healthy body weight and indicates it can be promoted as a marker of healthy body weight.
Acknowledgements
Provision of additional data by Drs Larsson, Liu, Jacobs, McKeown and Rimm is gratefully acknowledged, as is permission to use data from the Framingham Offspring Cohort.









