Poor oral health among older adults is among the conditions that contribute to inadequate dietary intake(Reference Hung, Colditz and Joshipura1–Reference Walls and Steele7). Functional limitations like not being able to chew properly or eat without pain discourage the consumption of foods that are crunchy, stringy or dry, such as vegetables, whole fruits, certain meats, or seeds and grains(Reference Gilbert, Duncan, Heft, Dolan and Vogel8, Reference Hildebrandt, Dominguez, Schork and Loesche9). These eating difficulties compound the effects of age-related declines in taste and nutrient absorption on the nutrient status of older adults(Reference Chernoff10). This increases the likelihood that diets will be inadequate within populations whose food choices are affected by their physical limitations, psychological decline and financial barriers(Reference Clarkston, Pantano, Morley, Horowitz, Littlefield and Burton11–Reference Sturm, MacIntosh, Parker, Wishart, Horowitz and Chapman16). When designing nutrition interventions or education programmes for older adults, key issues are to identify individuals with these limitations and to address the influence that compromised dental status has on their food choices.
Reduction in the number and functioning of teeth has been associated with poor diet quality among older adults. The number and location (anterior and posterior) of functional units (any opposing pair of natural or fixed prosthetic teeth) has been related to food avoidance and difficulties in chewing(Reference Hildebrandt, Dominguez, Schork and Loesche9). Several investigators have examined the role of missing posterior functional units (premolar and molar combined) in relation to dietary intake of specific nutrients or overall diet quality(Reference Sahyoun, Lin and Krall5, Reference Sheiham and Steele17, Reference Shinkai, Hatch, Sakai, Mobley, Saunders and Rugh18). The fewer teeth an individual has, the more likely he or she is to have lost functioning teeth and thereby suffer compromised nutritional status.
In 1995, the US Department of Agriculture (USDA) introduced the Healthy Eating Index (HEI) to provide an approach to assess how closely diets conformed to the then-current USDA dietary recommendations(Reference Kennedy, Ohls, Carlson and Fleming19). The original HEI included a total score calculated from dietary components that represented types and amounts of foods(Reference Kennedy, Ohls, Carlson and Fleming19). Since its introduction, HEI scores have been used to characterize the association between impaired dental status and diet quality. Lower total HEI scores in older adults have been associated with the presence of fewer pairs of posterior teeth, denture use, poorly fitting dentures, and persistent chewing, swallowing and mouth pain(Reference Sahyoun, Lin and Krall5, Reference Shinkai, Hatch, Sakai, Mobley, Saunders and Rugh18, Reference Bailey, Ledikwe, Smiciklas-Wright, Mitchell and Jensen20–Reference Shinkai, Hatch, Rugh, Sakai, Mobley and Saunders22). The HEI concept that considers overall diet quality and its component foods has been useful for considering implications of impaired dental status on the diet quality of older adults.
In 2005, new dietary guidelines were issued by the USDA (the 2005 Dietary Guidelines for Americans). In response to the new guidance, the HEI was revised(Reference Guenther, Reedy, Krebs-Smith, Reeve and Basiotis23). This revision, now referred to as Healthy Eating Index-2005 (HEI-2005), reflects the Dietary Guidelines’ increased emphasis on whole grains (particularly vegetables), certain oils, and energy from sweets, solid fats and alcohol. A second important consideration for the HEI-2005 was the use of density standards rather than absolute amounts of food (i.e. the food amounts per 4184 kJ (1000 kcal) of intake compared with the amounts per day)(Reference Ritchie, Joshipura, Hung and Douglass24). The use of this standard allows comparisons of nutrient intake to be independent of an individual’s reported energy intake. Thus, for older adults who often have reduced energy intake(Reference Quandt, Vitolins, Smith, Tooze, Bell, Davis, DeVellis and Arcury25–Reference Tooze, Vitolins, Smith, Arcury, Davis, Bell, DeVellis and Quandt27), the HEI-2005 density standard approach provides a useful method for understanding food choices of older adults regardless of the total amounts of food(Reference Ritchie, Joshipura, Hung and Douglass24). To date, the HEI-2005 has not been examined among older adults, particularly those with compromised dental status.
The present paper uses data from a population-based survey that considered the oral health status and diet quality of a multi-ethnic older adult population. Its objectives are: (i) to quantify the association between the number of teeth and overall diet quality as measured by the HEI-2005; and (ii) to compare the number of teeth with the individual components of the HEI-2005.
Methods
Sampling plan and recruitment
Between January 2006 and March 2008, the Rural Nutrition and Oral Health Study conducted a cross-sectional survey of the oral health and dietary intake of an ethnically diverse sample of older adults living in rural areas of the southern USA. Participants were located using a random dwelling selection and screening procedure in which the primary sampling units (clusters) were stratified and selected with probability proportional to size. The University of Illinois Survey Research Laboratory consulted on the design and implementation of the procedure and provided final participant weights.
Clusters were stratified into four categories, based on the racial/ethnic composition of their residents, as predominantly (more than 50 %) African-American, American Indian, white or mixed (no ethnic group comprising 50 % of the residents). Twenty clusters were randomly selected from each of the four types for a total of eighty clusters.
Within the eighty mapped clusters, 5545 dwelling units were identified (Fig. 1). Individuals were considered eligible if they were 60 years or older, spoke English, were able to give informed consent and were physically able to complete the interview. Thirty-nine dwelling units were not screened, 4647 were screened but did not include an eligible participant and 859 included an eligible participant, yielding a screening rate of 99·3 %.
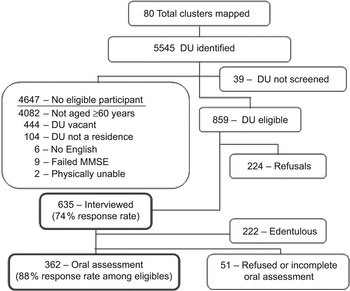
Fig. 1 Sample and recruitment for the Rural Nutrition and Oral Health Study (DU, dwelling unit; MMSE, Mini-Mental State Examination)
The eligible residents in 635 of the 859 eligible dwelling units completed the interview and 224 refused to complete the interview, for a response rate of 73·9 %. The weights for each participant were based on size of the cluster from which he/she was selected and his/her probability of selection within each dwelling unit. Eighty-eight per cent of those who had at least one tooth underwent an in-home oral assessment.
Data collection
All data collection procedures were approved by the university’s Institutional Review Board. The data were collected in face-to-face interviews at participants’ homes, lasting 1·5 to 2·5 h. Data collection included the 1998 version of the Block Food Frequency Questionnaire (FFQ) (Block 98·2; NutritionQuest, Berkeley, CA, USA), which assesses the usual intake of 110 foods. The use of the FFQ among this population was previously validated with a sample recruited from the same region (rural southern USA)(Reference Quandt, Vitolins, Smith, Tooze, Bell, Davis, DeVellis and Arcury25). Participants were asked about the typical frequency and portion sizes of foods they had eaten within the past year. Questions were read to participants and cue cards with response categories were used if necessary. All interviewers completed 8 h of training and 6 h of practice interviews. Ten per cent of interviews were verified by telephone. To maintain quality after initial training, one interview every month was audio-recorded for each interviewer. This tape and the accompanying completed FFQ were reviewed by research staff, who provided written feedback about recording errors or misinterpretations of the participants’ responses. Dental examinations quantified tooth counts and functional occlusal contacts clinically. Two dental hygienists conducted all dental examinations. They underwent an initial 1 d of training and 1 d of calibration with a research dentist, using volunteers representative of the study population. Calibration was repeated annually. The research dentist conducted five replicate examinations with each hygienist, and performed an ongoing review of data collection forms to check for correct logic, legal values and data ranges.
Demographic measures
Ethnicity based upon self-report was categorized as African-American, American Indian or white. Income was dichotomized as either above the poverty line or below the poverty line using current-year federal poverty guidelines, taking into account household size(28). Education was categorized as (i) less than high school graduate, (ii) high school graduate or (iii) more than high school, based on the participants’ highest level of education completed.
Dietary assessment and Healthy Eating Index-2005 scoring
The HEI-2005 scores were calculated from the food frequencies and completed questionnaires were scanned by NutritionQuest. In addition to standard output variables (daily micro- and macronutrient intakes and USDA food group servings of food), gram amounts and energy of each questionnaire item were provided by NutritionQuest to assist in the calculation of HEI-2005 component scores. The USDA Food Search Tool 3·0(29) was used to provide necessary information to calculate HEI-2005 components, such as grams per cup or ounce, amounts of fat, or added sugar in certain reference foods.
HEI-2005 contains twelve components(Reference Guenther, Reedy, Krebs-Smith, Reeve and Basiotis23). These include cup equivalent (eq)/4184 kJ (1000 kcal) of Total Fruit, Whole Fruit, Total Vegetables, Dark Green and Orange Vegetables and Legumes (after the Meat and Bean component reaches maximum values), and Milk (including soya milk). Meat and Beans (which includes eggs, nuts and soya foods excluding drinks), Total Grains and Whole Grains are calculated in oz eq/4184 kJ (1000 kcal). The amounts of Oils (those found in mayonnaise, margarine, salad dressing, nuts and seeds, and fish) and Sodium, measured in g/4184 kJ (1000 kcal), and the percentage of energy from Saturated Fat and Solid Fat, Alcohol and Added Sugar comprise the remaining components. The total HEI-2005 score, which ranges from 0 to 100, is the sum of the weighted scores for each component; the contribution (weighting) of each component to the total score varies. A maximum score of 5 was assigned to component values that met or exceeded recommended intakes of Total Fruit, Whole Fruit, Total Vegetables, Dark Green and Orange Vegetables and Legumes, Total Grains and Whole Grains. A maximum score of 10 was assigned for meeting or exceeding recommended amounts of Milk, Meat and Beans, and Oils. Maximum values of 10 were also assigned when Saturated Fat and Sodium were equal to or less than recommended intake. And, finally, the recommended percentage of energy contributed by Saturated Fat and Solid Fat, Alcohol and Added Sugar was assigned a score of 20 if it was equal to or less than the recommendations. With the exception of Saturated Fat, Sodium and Saturated Fat and Solid Fat, Alcohol and Added Sugar, scores of zero were assigned to values of 0 for each of the components; and intermediate values were assigned proportionally between 0 and the maximum values.
Anthropometrics
Interviewers were trained and certified to use portable, calibrated electronic scales with a maximum weight capacity of 200 kg (Tanita BWB-800A; Tanita Corp., Arlington Heights, IL, USA) and portable stadiometers (Seca 214 Road Rod; Seca Corp., Hanover, MD, USA) to weigh and measure height. Participants wore light clothing when measured and measures were taken twice and then averaged. BMI was calculated as kg/m2. Participants were classified as obese if their BMI was ≥30 kg/m2.
Oral health measures
Self-reported oral health was assessed by asking participants to rate the condition of their mouth and teeth, including prosthetic teeth and dentures, as excellent, very good, good, fair or poor.
Number of remaining natural teeth was a four-level categorical variable: 0 teeth, 1–10 teeth, 11–20 teeth and 21 or more teeth. Self-reported number of teeth was used to categorize those reporting 0 teeth or those dentate participants who refused the oral exam; otherwise, dentate participants were categorized based upon the clinical examination. The Pearson correlation between the self-reported and examination values for number of teeth was 0·92 for those who agreed to the oral assessment.
The number and location (anterior or posterior) of functional units was based on a count of functional contacts between two natural teeth, a natural tooth and a fixed prosthesis, or between two fixed prostheses. Data on functional contacts were available only for the 362 oral assessment participants and those reporting zero teeth.
Statistical analysis
All data analyses incorporated the multistage cluster sampling design. The Rao–Scott χ 2 test was used to quantify associations between gender and ethnicity, income, education, dental insurance, self-rated dental health and obesity. This test is a design-adjusted version of the Pearson χ 2 test. For continuous variables such as age, comparisons were made through regression analysis. Linear regression models were used to test for the unadjusted effects of age, ethnicity, gender, poverty status, education, dental insurance and BMI on total HEI score. Further analyses of the effects of two number of teeth categories (0–10 teeth and 11+ teeth) on total HEI score and its components were performed using a linear regression model after adjusting for covariates (age, gender, ethnicity, education, poverty and dental insurance). In addition, percentages meeting the requirements were calculated for 0–10 teeth and 11+ teeth categories. Odds ratios were calculated after adjusting covariates mentioned above using logistic regression. The distributions of total HEI score and its components were checked using histograms and the majority of these measures were bell-shaped, with exceptions that Total Fruit, Whole Fruit, Dark Green and Orange Vegetables, and Milk were right-skewed. However, no transformations were made to the latter variables since the study sample was relatively large and asymptotically the distributions approached normality. All analyses were performed using the SAS statistical software package version 9·1 (SAS Institute, Cary, NC, USA) and the significance level was set at 0·05.
Results
The sample comprised 344 women (54·1 %) of whom 40·4 % were white, 35·5 % American Indian and 24·2 % African-American (Table 1). Among men (N 291), 56·7 % were white, 25·3 % American Indian and 18·1 % African-American. Women were less likely to be married (33·5 % v. 62·1 %, P < 0·001) and more likely to have income below the poverty line (39·7 % v. 23·2 %, P = 0·001). More than half of the participants (55·7 %) had less than a high school education. Fifty-five per cent of participants reported having excellent, very good or good oral health, and 45 % reported fair or poor oral health. Ten per cent had private dental insurance. Women were more likely to be categorized as obese as defined as BMI ≥ 30 kg/m2 (44·0 % v. 30·9 %, P = 0·03).
Table 1 Demographic and health characteristics of participants: ethnically diverse community-dwelling older adults in the Rural Nutrition and Oral Health Study, southern USA, January 2006–March 2008
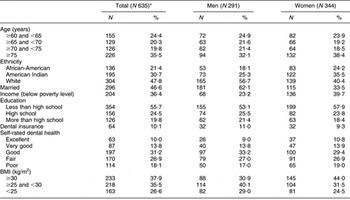
*N = weighted sample size.
Mean (se) daily energy intake and macronutrient composition among men were 10615 (464) kJ (2537 (111) kcal) and 39·8 (0·56) % from fat, 12·9 (0·30) % from protein and 48·0 (0·7) % from carbohydrates. Women consumed 9088 (289) kJ (2172 (69) kcal) each day, with 39·1 (0·47) % from fat, 12·8 (0·17) % from protein and 50·0 (0·60) % from carbohydrates.
Participants aged 60–65 years had lower total HEI-2005 scores (mean (se)) compared with those 75 years and older (58·68 (1·26) v. 62·97 (1·08), P = 0·02; Table 2). Women had higher total HEI-2005 scores than men (63·18 (1·01) v. 59·19 (0·72), P = 0·0008). Higher total HEI-2005 scores were associated with being above the poverty level (62·76 (0·87) v. 58·38 (1·03), P = 0·0004) and having more than a high school education (66·18 (1·06)) compared with those with only high school (62·22 (1·20), P = 0·009) and less than a high school education (59·26 (0·76), P < 0·0001). Total HEI-2005 score was not associated with ethnicity, having dental insurance or BMI.
Table 2 Bivariate relationships between the total HEI-2005 score and descriptive and oral health characteristics: ethnically diverse community-dwelling older adults (N 635)Footnote * in the Rural Nutrition and Oral Health Study, southern USA, January 2006–March 2008
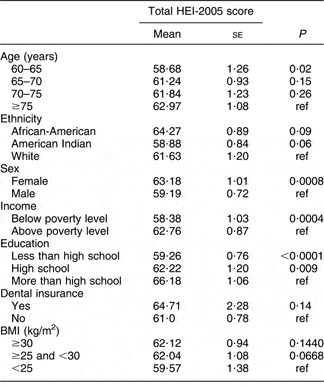
HEI-2005, Healthy Eating Index-2005; ref, reference value.
* N = weighted sample size.
Participants with 1–10 teeth had few teeth (median = 5 teeth), a median number of zero anterior or posterior functional units, and 11·2 % had at least one or more functional units (Table 3). The overall dental status of this category is very similar to individuals without any teeth. In contrast, participants with 11–20 teeth had a median number of 16 teeth with 97·5 % having one or more functional units. Participants in the 21+ category had a median of 25 teeth with 100 % having one or more functional units. Those with 11–20 teeth had fewer functional units in both anterior and posterior locations. Based on the similarities between the zero and 1–10 categories and the 11–20 and 21+ categories, we evaluated diet quality with two categories, severe tooth loss (0–10 teeth; N 326) and moderate to low tooth loss (11+ teeth, N 309).
Table 3 Number of teeth, anterior functional units and posterior functional units by number of teeth category: ethnically diverse community-dwelling older adults in the Rural Nutrition and Oral Health Study, southern USA, January 2006–March 2008
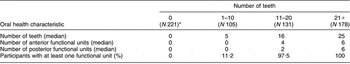
*N = weighted sample size.
After adjusting for gender, ethnicity, age, poverty status and dental insurance, participants with 11+ teeth had a higher total HEI-2005 score (mean (se): 64·89 (0·04)) than those with 0–10 teeth (59·39 (0·87), P < 0·0001; Table 4). Those with 0–10 teeth compared with those with 11+ teeth consumed less Total Fruit (0·53 (0·03) v. 0·62 (0·04), P = 0·015), Meat and Beans (2·19 (0·08) v. 2·43 (0·08), P = 0·01), and Oils (4·81 (0·52) v. 6·10 (0·38), P = 0·011). Those with 0–10 teeth had higher intake of energy from Saturated Fat and Solid Fat, Alcohol and Added Sugar (29·31 (0·67) v. 26·38 (0·56), P = 0·0001) compared with those with 11+ teeth. In addition, two trends were found. When compared with participants having with 11+ teeth, those with 0–10 teeth consumed fewer Total Vegetables (0·77 (0·06) v. 0·88 (0·04), P = 0·08) and Dark Green and Orange Vegetables and Legumes (0·40 (0·04) v. 0·47 (0·03), P = 0·08).
Table 4 Total HEI-2005 score, estimated intake of HEI components and the percentage of participants meeting HEI-2005 recommendations for each category: ethnically diverse community-dwelling older adults in the Rural Nutrition and Oral Health Study, southern USA, January 2006–March 2008
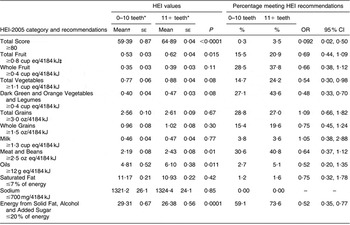
HEI-2005, Healthy Eating Index-2005.
*Weighted samples for tooth loss categories: 0–10 teeth, n 326; 11+ teeth, n 309.
†Adjusted for gender, ethnicity, age, poverty status and dental insurance.
‡4184 kJ = 1000 kcal.
While few participants met the overall recommendation for total HEI-2005 score, less than 1 % of those with 0–10 teeth met the recommendation as compared with 3·5 % of those with 11+ teeth (OR = 0·092, 95 % CI 0·02, 0·50). Those with 0–10 teeth were also less likely to meet recommendations than those with 11+ teeth for Total Vegetables (14·7 % v. 24·2 %; OR = 0·54, 95 % CI 0·30, 0·98), Dark Green and Orange Vegetables and Legumes (27·1 % v. 43·6 %; OR = 0·48, 95 % CI 0·33, 0·70) and energy from Saturated Fat and Solid Fat, Alcohol and Added Sugar (59·1 % v. 73·6 %; OR = 0·52, 95 % CI 0·35, 0·77).
For six of the twelve HEI food components, there were no significant differences between the number of teeth categories for either mean intake or percentage meeting recommended values. Whole Fruit and Total and Whole Grains requirements were met by approximately 20–35 % of all participants. Fewer than 5 % of participants met Milk and Saturated Fat recommendations. All participants exceeded recommended Sodium intake.
Discussion
In this ethnically diverse sample of older adults, we found that approximately half of the sample had severe tooth loss (0–10 teeth remaining) and that these individuals had lower adherence to the USDA 2005 Dietary Guidelines(Reference Fogli-Cawley, Dwyer, Saltzman, McCullough, Troy and Jacques30) compared with those with 11+ teeth. Our findings that those with 0–10 teeth had few functional units in any location are consistent with reports of older adults with chewing problems having fewer teeth, fewer total functional units and fewer posterior functional units compared with those without chewing complaints(Reference Hildebrandt, Dominguez, Schork and Loesche9). Independent of the effects of age, sex, poverty status, dental insurance status and education, having 0–10 teeth was associated with a 5-point lower diet quality score compared with those with 11+ teeth. This difference was comparable to or greater than differences found in total HEI scores associated with age, sex, poverty status and education.
The participants with fewer teeth had either low intake or low rates of adherence to recommendations for six of the twelve food groups emphasized by the current USDA guidance(Reference Fogli-Cawley, Dwyer, Saltzman, McCullough, Troy and Jacques30). Differences in estimated intake per 4184 kJ (1000 kcal) of Total Fruit, Whole Fruit, Total Vegetables, Meat and Beans, and Oils between those with 0–10 teeth and those with 11+ teeth represented about 10 % of the recommended amounts of these food categories. The differences in Dark Green and Orange Vegetables and Legumes and energy from Saturated Fat and Solid Fat, Alcohol and Added Sugar represented 15 % of current recommendations.
The six components related to the number of teeth represent 55 % of the 100 points that comprise the total HEI-2005 score. The remaining 45 % of this score included Whole Fruit, Total and Whole Grains, Milk, Saturated Fat and Sodium components. Regardless of the number of teeth, at least 96 % of participants failed to consume enough milk products and exceeded guidelines for saturated fat and sodium. The majority (70–80 %) of all participants failed to consume adequate amounts of Whole Fruit and Total and Whole Grains.
A report using the original HEI index found that total HEI and HEI fruit component scores were higher for those with five to eight posterior functional units than for those with fewer functional units, those without teeth and those with a full denture(Reference Sahyoun, Lin and Krall5). However, another report found few associations between the number of posterior functional units and the original HEI total and component scores(Reference Shinkai, Hatch, Sakai, Mobley, Saunders and Rugh18). Among older adults assessed for their consumption of certain foods, nutrient and dietary intake, and nutritional status, those with 1–10 teeth had significantly more difficulty eating apples and certain kinds of bread and vegetables(Reference Sheiham and Steele17). Those with fewer teeth had lower intakes of fibre, total carbohydrates, energy, protein, fat and certain micronutrients, and comparable differences were found for those with fewer posterior functional units(Reference Sheiham and Steele17). It appears that both number of teeth and number of posterior functional units have similar relationships with dietary intake and nutritional status.
Two-thirds of participants in the present research with severe tooth loss (0–10 teeth) were edentulous (having no teeth) and, among the remaining third, only 11 % had any functional units. The USDA has found that edentulous persons have less varied and poorer-quality diets containing fewer servings of fruits and vegetables, compared with the population as whole(Reference Ervin31). Among older adults (age 70–79 years), edentulous persons consumed less energy from protein, dietary fibre, and fruits and fruit juices, as well as more sweets, desserts, fats and oils(Reference Lee, Weyant, Corby, Kritchevsky, Harris, Rooks, Rubin and Newman32). Within a large sample of male health professionals, those who were edentulous consumed fewer vegetables and less dietary fibre, apples, pears and carrots than those with 25 or more teeth(Reference Joshipura, Willett and Douglass2). A report from the National Health and Nutrition Examination Survey (1988–94) found that those who had only 1–10 teeth consumed fewer carrots and salads and had lower serum levels of β-carotene, folate and vitamin C(Reference Nowjack-Raymer and Sheiham33). This is consistent with the present findings where those with severe tooth loss ate fewer fruits and vegetables and consumed less meat and more energy from solid fat and added sugar.
The effect of impaired dental status on efforts to improve the diets of older adults has important implications for public health nutrition, particularly as it relates to fruit and vegetable consumption. Younger and older adults who were more socially isolated, had poor self-reported health, were obese and had fewer pairs of posterior teeth were at the highest risk of consuming low amounts of fruits and vegetables(Reference Sahyoun, Zhang and Serdula6). Lack of dental insurance leading to tooth loss was identified by older low-income women as a barrier to increased fruit and vegetable consumption(Reference Dye and Cason34). Perceived chewing ability explained 4 % of the variance in fruit and vegetable consumption among middle-aged to older adults(Reference Bradbury, Thomason, Jepson, Walls, Mulvaney, Allen and Moynihan35).
Fruit and vegetable interventions for older adults have focused on psychosocial variables, such as locus of control or self-efficacy(Reference Greene, Fey-Yensan, Padula, Rossi, Rossi and Clark36). Others were designed to increase knowledge and skills related to healthful recipes and shopping(Reference Bernstein, Nelson, Tucker, Layne, Johnson, Nuernberger, Castaneda, Judge, Buchner and Singh37, Reference Hendrix, Fischer, Reddy, Lommel, Speer, Stephens, Park and Johnson38). Including recipes modified for those with impaired chewing ability may be a useful strategy for older adults(Reference Bradbury, Thomason, Jepson, Walls, Allen and Moynihan39). When barriers to fruit and vegetable intake were measured at baseline, ‘chewing or dental problems’ were reported by 19 % of participants – exceeded only by ‘cost’ (24 %) and ‘difficulties with digestion’ (20 %)(Reference Hendrix, Fischer, Reddy, Lommel, Speer, Stephens, Park and Johnson38). The perception of ‘chewing or dental problems’ remained unchanged at the end of the 4-month intervention(Reference Hendrix, Fischer, Reddy, Lommel, Speer, Stephens, Park and Johnson38). The large number of participants with 0–10 teeth in the present study suggests that dietary interventions targeted at older adults should consider categorizing participants based on the simple measure of the number of teeth to assess the severity of their tooth loss. Intervention strategies to address the needs of those with severe tooth loss should be considered.
Our study has several strengths. It is a population-based sample that includes older adults from three ethnic groups and considers oral health status along with diet quality. It utilizes the HEI-2005 scoring system, which represents the most recent USDA recommendation, and as such provides an opportunity to examine the components based on a density standard. Although many reports have considered the effectiveness of posterior functional units in relation to diet quality, we have demonstrated that categorizing individuals based on severe tooth loss v. moderate to low losses can provide useful information about diet quality of older adults.
The study has limitations. First, the HEI-2005 as developed by USDA relies on a single 24 h recall to assess individual food choices(Reference Freedman, Guenther, Krebs-Smith and Kott40). We adapted the HEI-2005 scoring system to the FFQ output using an approach to categorizing foods similar to HEI-2005 guidance. The use of the FFQ is considered to be a valid approach for comparison of groups, providing a better description of usual diet than a single 24 h recall, and is suitable for the present investigation(Reference Subar, Thompson, Kipnis, Midthune, Hurwitz, McNutt, McIntosh and Rosenfeld41). Prior research validated the FFQ using the average of six 24 h recalls for comparison. The FFQ provided results that allowed the comparison of dietary intake across participants in the present study population(Reference Quandt, Vitolins, Smith, Tooze, Bell, Davis, DeVellis and Arcury25). Second, under-reporting of energy intake by rural older adults can potentially introduce bias into comparisons between groups(Reference Tooze, Vitolins, Smith, Arcury, Davis, Bell, DeVellis and Quandt27, Reference Bailey, Mitchell, Miller and Smiciklas-Wright42). These previous reports have found that rural older adults are failing to report both healthful and unhealthful foods. The HEI-2005 density standard approach can minimize the impact of under-reporting by allowing scoring to be independent of individual’s reported energy intake(Reference Guenther, Reedy, Krebs-Smith, Reeve and Basiotis23). Third, our study was a cross-sectional investigation, and thus a causal relationship between oral health status and food choices cannot be established.
In summary, older adults with severe tooth loss have low adherence to the USDA 2005 Dietary Guidelines for Americans. Although overall older adults were not meeting recommendations, our findings showed that in food groups emphasized in the 2005 USDA guidance, older adults with severe tooth loss had a greater disadvantage compared with those with more teeth. The oral health status of older adults should become a key consideration in efforts to understand and improve the diet quality of older adults.
Acknowledgements
Support for this research was provided by the National Institute for Dental and Craniofacial Research, grant R01 DE017092. No authors have any conflicts of interest. M.R.S. developed the analytic strategy, interpreted the data, wrote the initial manuscript and oversaw the preparation of the final manuscript; T.A.A. contributed to study design and interpreted the data; X.L. conducted the statistical analysis and interpreted the data; H.C. conducted the statistical analysis and interpreted the data; R.A.B. contributed to study design and interpreted the data; A.M.A. provided statistical analyses; T.K. acquired the subjects and participated in manuscript preparation; R.J.F. contributed to the literature review, interpreted the data and participated in manuscript preparation; G.H.G. interpreted the data; and S.A.Q. oversaw study design, interpreted the data and participated in writing of the manuscript. All authors participated in writing of the final manuscript.







