Double burden of malnutrition (DBM) refers to the coexistence of undernutrition and overnutrition in the same setting( Reference Sekiyama, Jiang and Gunawan 1 , Reference Ramirez-Zea, Kroker-Lobos and Close-Fernandez 2 ). This phenomenon can occur at individual level, household level and even at population level( Reference Sekiyama, Jiang and Gunawan 1 ). DBM becomes evident when the slower reduction rate of undernutrition is coupled with a faster increasing rate of overnutrition( Reference Kimani-Murage, Muthuri and Oti 3 ). Evidence suggests that along with demographic and socio-economic transitions, developing countries are experiencing a nutritional transition( Reference Kapoor and Anand 4 ). Rapid urbanization, economic development, consumption of less plant-based, more refined and energy-dense foods, and decreased physical activity are the factors reported to be responsible for this( Reference El Kishawi, Soo and Abed 5 ). Over- and undernutrition – both axes of malnutrition – are equally harmful. Undernutrition hinders physical and intellectual development( Reference Dewey and Begum 6 ), whereas overnutrition acts as a significant contributor to various non-communicable diseases( Reference Misra, Singhal and Sivakumar 7 ). At household level the most common duo is the coexistence of undernourished children and overweight or obese mothers, which is commonly known as mother–child dual burden (MCDB) of malnutrition( Reference Doak, Adair and Monteiro 8 , Reference Hanandita and Tampubolon 9 ).
Studies done in different parts of the world have reported the presence of MCDB of malnutrition at household level. In Brazil the prevalence of MCDB was 11·0 % and in China it was 8·0 %( Reference Doak, Adair and Monteiro 8 ). A study done in rural west Java reported the prevalence of household-level MCDB as 30·6 %, whereas in the Gaza Strip of Palestine it was 15·7 %( Reference El Kishawi, Soo and Abed 5 ). According to the Bangladesh Nutritional Surveillance Project (2003–2006), the prevalence of MCDB of malnutrition in rural Bangladesh was 4 %( 10 – Reference Oddo, Rah and Semba 12 ). Reports from national surveys indicate that the trend of being overweight or obese among Bangladeshi women of reproductive age is on a steady rise, whereas the prevalence of childhood undernutrition is not declining at a desired rate( 10 ). Among Bangladeshi children under 5 years of age, 36 % are stunted, 14 % are wasted and 33 % are underweight, whereas the prevalence of overweight/obesity among ever-married Bangladeshi women is 24 %( 10 ). But to our knowledge, no analysis has been done using countrywide data to explore the existing scenario of household-level DBM among mother–child pairs living in Bangladesh.
Household-level DBM is an important concern from a public health perspective. The burden has been accelerated in low- and middle-income countries (LMIC) over the past few decades and confers serious impact on health, productivity and economic growth( 13 ). It has already been reported that the malnutrition double burden is linked with persistence of adverse conditions such as high level of food insecurity, intake of energy-dense foods, higher prevalence of infection, and inadequate access to water and health-care services( Reference Kimani-Murage, Muthuri and Oti 3 ). These factors, in association with rapid population growth and urbanization, may lead to an increase in the prevalence of DBM and subsequent adverse effects in the country. Hence, identifying the determinants of MCDB of malnutrition can help nutritionists as well as policy makers to direct effective and specific interventions for preventing and controlling malnutrition in all its forms. Understanding the DBM and its determinants is essential to meet the health-related Sustainable Development Goals( 13 ). Considering the above-mentioned context, we aimed to measure the prevalence and to identify sociodemographic determinants of household-level MCDB of malnutrition in Bangladesh.
Methods
Study design
The present study is based on analysis of Bangladesh Demographic and Health Survey (BDHS) 2014 data. The 2014 BDHS was a nationally representative cross-sectional survey conducted between 28 June and 9 November of 2014 by the National Institute of Population Research and Training, ICF International (USA), and Mitra and Associates. Participants in the BDHS were selected using probability-proportional-to-size sampling based on a two-stage cluster sample of households and stratified by rural and urban areas in the seven administrative regions of Bangladesh. The detailed protocol and methods have been published elsewhere( 10 ). The survey selected 18 000 residential households, where 17 565 were found occupied. Interviews were successfully completed in 17 300 (99 %) households with a response rate of 98 % from ever-married women aged 15–49 years. Informed consent was obtained from the participants after notifying them about the purpose of the survey.
Anthropometric measurements and nutritional status
In order to assess nutritional status, height and weight of the participants were measured by trained field research staff using standardized procedures. For mothers, BMI was calculated as [weight (kg)]/[height (m)]2. The BMI cut-off used for overweight was 25·0 to <30·0 kg/m2, and for obesity it was ≥30·0 kg/m2 ( 14 ). Children were referred as undernourished when they were stunted, wasted or underweight. Stunting was defined as length-for-age or height-for-age less than 2 sd below the median length-for-age or height-for-age of the WHO reference population (i.e. length-for-age Z-score (LAZ) or height-for-age Z-score (HAZ)<–2). Wasting was defined as having a weight-for-length Z-score (WLZ) or weight-for-height Z-score (WHZ) of <−2, and underweight as having a weight-for-age Z-score (WAZ) of <−2, compared with the respective median of the WHO reference population.
Outcome variables
The extent of our current analysis was limited to household-level DBM where the mother was overweight or obese (OWOBM) and at least one of her children under 5 years of age was undernourished. We had four different forms of DBM in the analysis as outcome variables. In all the forms, the mother was either overweight or obese. If the child was underweight, then the DBM was termed as OWOBM/UWC; OWOBM/STC indicates that the child was stunted, OWOBM/WSC indicates that the child was wasted; and OWOBM/USWC indicates the overweight or obese mother was paired with her child having at least one form of undernutrition (underweight or stunted or wasted).
Sociodemographic factors
Sociodemographic characteristics of the participants were collected using a validated questionnaire which was administered during a face-to-face interview. Education variables were categorized as no education (indicating 0 grade), primary education (indicating completed grade 1–5), secondary education (indicting completed grade 6–10) and higher education (indicating completed more than grade 10). Households were categorized based on living in urban or rural areas. A composite score named the ‘household wealth index’, which was calculated using principal components analysis and already included in DHS data set, was used for the current analysis. The index was calculated based on the household’s ownership of selected assets, availability of electricity supply, television and bicycle; materials used for housing construction; types of water access and sanitation facilities; use of health and other services; and health outcomes. Information on child’s size at birth was collected according to the recall statement of the mother.
Statistical analysis
A total of 5951 households where a mother had at least one child under 5 years of age were included in the analysis. If a family had two or more children within the age range (0–59 months), the oldest one was selected for the mother–child pair. Prevalence was calculated by dividing the number of DBM households by the total number of households and multiplying by 100. We applied frequency distribution to summarize the categorical variables and descriptive statistics to summarize the continuous variables. Firth’s logistic regression analysis was performed to identify the sociodemographic factors associated with the DBM. Firth’s penalization stabilizes the bias in predicted probabilities when the outcome of interest is rare( Reference Firth 15 ). The variables found to be statistically significant (P<0·05) in the bivariate analysis were considered for the multivariable analysis. Households having normal-weight mother (BMI=18·5–24·9 kg/m2) and non-malnourished child pairs (1778 households, 29·9 %) were counted as the comparison group for regression analysis. We reported OR with 95 % CI and considered P<0·05 as the cut-off level of statistical significance. The complex sampling design with weighted sample was adjusted for in all statistical analyses. We performed likelihood ratio tests to evaluate the model goodness-of-fit (see online supplementary material, Supplemental Table 1) and the statistics suggested that all the models were a good fit (likelihood ratio test values for OWOBM/UWC, OWOBM/STC, OWOBM/WSC and OWOBM/USWC models are 74·79221 (P=0·0014), 74·46098 (P=0·00083), 25·76653 (P=0·04) and 112·8807 (P=0·0014), respectively). Firth’s logistic regression analyses were performed using the ‘logistf’ package in R ( Reference Heinze, Ploner and Dunkler 16 ).
Results
Sociodemographic characteristics
Table 1 describes the sociodemographic characteristics of the participants. The mean age of the mothers was 25·65 (sd 5·98) years. Only 14·8 % of mothers did not receive any formal education and 11·1 % had higher education. Only half of the mothers (47·1 %) and one-third of the fathers (31·3 %) attained secondary education. Approximately 75 % of the mothers did not have any employment and the remaining 25 % were working to earn money. Almost two-thirds of the participants lived in rural areas. Two-thirds (63·5 %) of the families had never been exposed to any type of information media. The mean age of the mothers at first pregnancy was 18·27 (sd 3·33) years. Of the mothers, 60 % delivered their child at home and 76 % of the deliveries were normal deliveries. A total of 18·8 % of the children were born smaller than average.
Table 1 Sociodemographic characteristics of the respondents (n 5951). Data from the Bangladesh Demographic and Health Survey 2014
NGO, non-governmental organization; C-section, caesarean section.
Prevalence of double burden of malnutrition
Figure 1 represents the prevalence of different forms of DBM among mother–child pairs. The prevalence of overweight or obese mother and underweight child was 3·8 (95 % CI 3·3, 4·3) %, of overweight or obese mother and stunted child was 4·7 (95 % CI 4·2, 5·3) % and of overweight or obese mother and wasted child was 1·7 (95 % CI 1·4, 2·1) %. The coexistence of overweight or obese mother and undernourished child (underweight or stunted or wasted) was observed in 6·3 (95 % CI 5·8, 7·1) % of households.
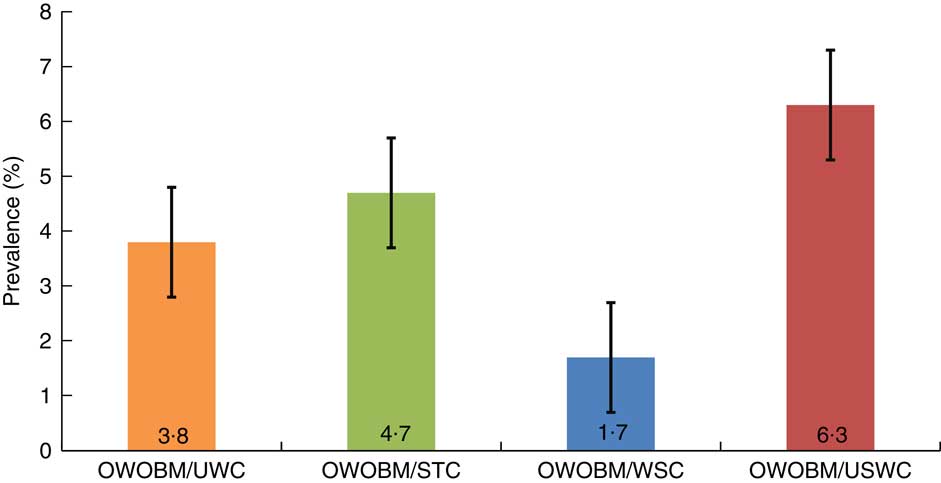
Fig. 1 (colour online) Prevalence of household-level mother–child double burden of malnutrition in Bangladesh (n 5951), with 95 % CI represented by vertical bars. Data from the Bangladesh Demographic and Health Survey 2014 (OWOBM/UWC, overweight or obese mother and underweight child; OWOBM/STC, overweight or obese mother and stunted child; OWOBM/WSC, overweight or obese mother and wasted child; OWOBM/USWC, overweight or obese mother and underweight or stunted or wasted child)
Factors associated with household-level double burden of malnutrition
Table 2 presents the factors associated with DBM among mother–child pairs at household level in the bivariate analysis, and Table 3 presents the results of the multivariable analysis. The presence of OWOBM/UWC showed statistically significant positive associations (all P<0·05) with mother’s age being 21–25 years at first birth (OR=2·40; 95 % CI 1·32, 4·52), middle wealth index group (OR=3·23; 95 % CI 1·56, 7·22), family never exposed to information media (OR=1·90; 95 % CI 1·13, 3·27), having two or three children (OR=2·71; 95 % CI 1·07, 4·47) and having four or more children (OR=4·03; 95 % CI 2·14, 7·54). Size of the child larger than average at birth was found to be protective against OWOBM/UWC (OR=0·41; 95 % CI 0·18, 0·83; P<0·05).
Table 2 Bivariate analysis of unadjusted OR with 95 % CI for different forms of household-level mother–child double burden of malnutrition in Bangladesh, by maternal and child characteristics (n 5951). Data from the Bangladesh Demographic and Health Survey 2014
OWOBM/UWC, overweight or obese mother and underweight child; OWOBM/STC, overweight or obese mother and stunted child; OWOBM/WSC, overweight or obese mother and wasted child; OWOBM/USWC, overweight or obese mother and underweight or stunted or wasted child; C-section, caesarean section; ref., reference category.
*Statistical significance at P<0·05.
Table 3 Multivariable analysis using Firth’s logistic regression to determine the factors associated with different forms of household-level mother–child double burden of malnutrition in Bangladesh (n 5951). Data from the Bangladesh Demographic and Health Survey 2014
OWOBM/UWC, overweight or obese mother and underweight child; OWOBM/STC, overweight or obese mother and stunted child; OWOBM/WSC, overweight or obese mother and wasted child; OWOBM/USWC, overweight or obese mother and underweight or stunted or wasted child; C-section, caesarean section, ref., reference category.
*Statistical significance at P<0·05.
A similar result was found for OWOBM/STC households. The statistically significant determinants (all P<0·05) of OWOBM/STC included mother’s age at first birth being 16–20 years (OR=1·83; 95 % CI 1·10, 3·24) and 21–25 years (OR=2·45; 95 % CI 1·32, 4·70), middle wealth index group (OR=1·96; 95 % CI 1·07, 3·70), having two or three children (OR=2·49; 95 % CI 1·66, 3·80) and having four or more children (OR=4·09; 95 % CI 2·35, 7·06). No history of being vaccinated was found to be protective against OWOBM/STC (OR=0·67; 95 % CI 0·47, 0·97; P<0·05).
For OWOBM/USWC, households with mother’s age being 21–25 years at first birth (OR=1·97; 95 % CI 1·18, 3·32; P<0·05), no exposure to information media (OR=1·47; 95 % CI 1·01, 2·22; P<0·05), delivery of child through caesarean section (C-section; OR=1·68; 95 % CI 1·20, 2·33; P<0·05), having two or three children (OR=2·59; 95 % CI 1·84, 3·71; P<0·05) and having four or more children (OR=4·72; 95 % CI 2·93, 7·60, P<0·05) were associated with significantly higher odds of MCBD of malnutrition. No such statistically significant associations were found between selected sociodemographic determinants and OWOBM/WSC households.
Discussion
Our study found a low prevalence of household-level MCDB of malnutrition in Bangladesh. This finding is in line with the results from other studies conducted in LMIC. The proportion of OWOBM/STC was less than 10 % in most of the countries, except in some African and Latin American countries such as Egypt (12·5 %), Ghana (12·5 %), Nicaragua (12·5 %), Bolivia (15 %), Peru (16 %) and Guatemala (23 %)( Reference Jehn and Brewis 17 ). Previous studies conducted in rural Indonesia and Bangladesh estimated the prevalence of OWOBM/STC at household level to be 11 and 4 %, respectively( Reference Oddo, Rah and Semba 12 ). Our result regarding household-level OWOBM/UWC burden is in accordance with the reports from eighteen LMIC of South Asia, Africa and Latin America, where the prevalence of OWOBM/UWC ranged from 0·3 to 5·3 %( Reference Wong, Zalilah and Chua 18 , Reference Oddo, Rah and Semba 19 ). We found that the prevalence of OWOBM/WSC is only 1·7 % in Bangladesh. The prevalence of wasting (14 %) is much lower in the country compared with stunting (36 %) and underweight (33 %)( 10 ). This might be the possible cause behind finding a lower proportion of OWOBM/WSC in the current analysis.
Over 6 % of households had a coexistence of an overweight or obese mother and an undernourished child (OWOBM/USWC). It is well established that such coexistence of over- and undernutrition is a consequence of nutrition transition in LMIC( Reference Dieffenbach and Stein 20 ). Nutrition transition brings changes in dietary habits and consumption of high-energy-dense foods which, along with less physical activity, result in excessive weight gain among mothers as well as adults in the family( Reference Dieffenbach and Stein 20 , Reference Kosaka and Umezaki 21 ). Foods with high energy density are poor in nutrient content( Reference Dieffenbach and Stein 20 ). So, the children receive inadequate nutrition which leads to undernutrition( Reference Kimani-Murage, Muthuri and Oti 3 , Reference Dieffenbach and Stein 20 ). This can be a possible explanation of MCDB of malnutrition in Bangladesh, as the country has been experiencing a shift in dietary habits over the past few years.
Previous studies showed that MCDB was associated with middle-income households( Reference Sekiyama, Jiang and Gunawan 1 , Reference Lee, Houser and Must 22 ). Similar to those reports, we also found the middle wealth index category to be associated with OWOBM/STC and OWOBM/UWC. This indicates that poverty is not the cause of MCDB of malnutrition in Bangladesh. Adults from the middle wealth quintile might be more exposed to changes in dietary habits due to nutrition transition in the country, which is evident in many LMIC( Reference Sekiyama, Jiang and Gunawan 1 ). Due to increased per capita income, families from the middle wealth quintile are having access to Western foods which is causing excess energy intakes( Reference El Kishawi, Soo and Abed 5 , Reference Lee, Houser and Must 22 ). Excess energy intake contributes to adult overweight and obesity( Reference Leroy, Habicht and González de Cossío 23 ), but the phenomenon is complex in children. Childhood undernutrition is interlinked with biological responses to environmental conditions, caring behaviours in the family, diet quality, micronutrient adequacy and morbidity( Reference Garrett and Ruel 24 ). Perhaps families with excess energy intake lack improvement in most of those factors as well as sufficient micronutrient intakes for children, which ultimately leads to DBM. In addition, there might be some social or cultural norms pertaining to food choices and intra-family food distribution that need to be investigated. Several studies revealed that the coexistence of overweight or obese mother and underweight child is more common in urban settings( Reference Sekiyama, Jiang and Gunawan 1 , Reference Jehn and Brewis 17 ). We also found the same result for OWOBM/UWC, OWOBM/STC and OWOBM/USWC in bivariate analyses. In urban areas, adult family members have to work outside the home to earn money; hence the family depends on commercially available low-priced foods which are poor in nutrient content. Commercially prepared foods are usually energy-dense and provide energy to adults, but adversely affect the nutritional status of children( Reference Jehn and Brewis 17 , Reference Caballero 25 ). This can be the probable explanation for higher risks of MCDB among those living in urban areas. However, the findings became insignificant after adjusting for the confounders in our multivariable analyses.
We found maternal age at first child birth and having more than one child to be significantly associated with the risk of MCDB of malnutrition. Females are prone to attaining excess BMI with increase of age and parity( Reference Jehn and Brewis 17 ). Several studies have also suggested that mother’s age is positively associated with MCDB( Reference Oddo, Rah and Semba 19 ). Whether this is related to poor postpartum resolution of the weight gained during pregnancy is not known for Bangladesh. Moreover, a larger number of young children in the same household is known to affect the availability of foods for children( Reference Jehn and Brewis 17 ). This might be indicative of rendering less care and attention towards the younger children of the family.
The present study revealed that households not at all exposed to information media are more at risk of developing MCDB of malnutrition, especially in the forms of OWOBM/UWC and OWOBM/USWC. Television, radio and newspapers can influence behaviour and prevent negative health-related practices( Reference Wakefield, Loken and Hornik 26 ). Therefore, exposure to mass media campaigns may reduce the risk of MCDB of malnutrition.
Child delivery through C-section was found to be a significant contributor to DBM in Bangladesh. C-section was significantly associated with OWOBM/STC, OWOBM/WSC and OWOBM/USWC in bivariate analyses. After adjustment, only OWOBM/USWC was significantly associated with C-section delivery of the child. Studies have confirmed that undernutrition and obesity, both forms of malnutrition, are linked with gut microbiota alterations in children( Reference Pekmez, Dragsted and Brahe 27 ). It is also reported that C-section delivery contributes to microbial alterations in the small intestine( Reference Dominguez-Bello, Costello and Contreras 28 , Reference Grölund, Lehtonen and Eerola 29 ). Therefore, the association of DBM with delivery through C-section is consistent with the previous study results.
Size of the child at birth larger than average was found to be protective against OWOBM/UWC. Since data regarding size at birth were subjective, there might be chance of recall bias. We observed that history of no vaccination was protective against DBM, especially against OWOBM/UWC. However, we did not find any scientific explanation supporting this finding and recommend future prospective studies to elucidate the association of vaccination with the presence of DBM.
The present study depicts the current scenario of different forms of household-level DBM and its relationship with important sociodemographic correlates. The use of a nationwide representative sample from both urban and rural areas is the strength of the study. However, the study has some limitations. Because the study design was cross-sectional, establishment of causality between the identified factors and DBM was not possible. The BDHS 2014 was not designed to address and analyse the presence of household-level DBM. Therefore, we were not able to follow any conceptual framework to comprehensively explain the burden in the context of Bangladesh. We only analysed the sociodemographic determinants of DBM. Determinants such as dietary intake, physical activity, caregiving practices, postpartum weight resolution and cultural influences were not evaluated. So, further exploration is warranted to ascertain the contribution of these potential determinants on development of various forms of MCDB of malnutrition in Bangladesh.
Conclusion
Nutrition and socio-economic transition are playing crucial roles in pulling the trend of DBM upwards in Bangladesh and other LMIC. The current study indicates the existence of MCDB of malnutrition in Bangladesh with the persistence of potential sociodemographic correlates contributing to the burden. The findings of the current study reinforce that malnutrition prevention programmes must not ignore the nutrition concerns of the whole household to prevent the burgeoning risk of MCDB in Bangladesh. Such programmes also need to be tagged with family planning and increasing awareness through social and behaviour change counselling and exposure to information media.
Acknowledgements
Acknowledgements: The authors would like to acknowledge the DHS Program and the BDHS 2014, which was made possible by the generous support of the American people through the US Agency for International Development (USAID). They also acknowledge the contribution of icddr,b’s core donors (including Government of the People’s Republic of Bangladesh; Global Affairs Canada (GAC), Canada; Swedish International Development Cooperation Agency (SIDA); and the Department for International Development, UKAid) for their continuous support and commitment to the icddr,b’s research efforts. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None of the authors had any conflict of interest to declare. Authorship: S.D. and S.M.F. are joint first authors. S.D. and S.M.F. developed the study concept. S.D., S.M.F. and T.B. contributed to the study design. S.D., M.S.I. and S.M.F. participated in the data analysis and discussion. S.D. and S.M.F. wrote the first draft. S.D., S.M.F., T.B., T.A. and M.M. critically reviewed the drafts. All authors have seen and approved the final draft of the manuscript. Ethics of human subject participation: Informed consent was obtained from the participants of BDHS 2014 after notifying them about the purpose of the survey.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980018003580






