Neural tube defects (NTDs), being the most common congenital malformations, are a major cause of stillbirth and infant mortality, and account for up to a third of stillbirths and a quarter to a third of neonatal deaths in China. Within China, the prevalence rate of NTDs varies dramatically between the north, which has a very high rate, and the south, which has a much lower rate; as well as between urban and rural areas, with rural areas reporting higher ratesReference Moore, Li, Li, Hong, Gu and Berry1, Reference Xiao, Zhang, Su, Liu, Yan and Jiang2. Shanxi Province, located in northern China, has one of the highest birth prevalences of NTDs in the world. The prevalence was reported as 10.55 per 1000 births in 1986/87 by a hospital-based surveillance systemReference Xiao, Zhang, Su, Liu, Yan and Jiang2, and as 14.9 per 1000 births in 1997 from a local government retrospective investigation. These rates are over 10 times higher than those reported from southern China or the USA during the same periodReference Moore, Li, Li, Hong, Gu and Berry1.
The relationship between folic acid supplementation during the periconceptional period and reduced incidence of NTDs is well established3–Reference Berry, Li, Erickson, Li, Moore and Wang5. In 1992, the US Public Health Service took the lead in recommending that all women capable of becoming pregnant should consume 400 μg of folic acid per day to prevent NTDs6. This recommendation was subsequently followed by agencies and societies in many other countries. In China, the Ministry of Health recommended in 1992 that all women who are newly married or planning pregnancy should consume a daily supplement containing 0.4 mg of folic acid to prevent NTDsReference Li, Moore, Li, Berry, Gindler and Hong7.
Recently, an increasing number of studies have been conducted to assess the compliance of intake of folic acid supplements and to discuss the best method of administration of folic acid to womenReference Ray, Singh and Burrows8–Reference Canfield, Anderson, Waller, Palmer and Kaye20. However, few to date have reported on the actual use of folic acid supplements in the Chinese population. Therefore the main aim of the present study was to understand the actual use of folic acid supplements during the periconceptional period and its association with selected sociodemographic and obstetric characteristics in the high NTD prevalence area of Shanxi Province, China.
Materials and methods
Study setting
The study was conducted in four counties (Pingding, Xiyang, Taigu, and Zezhou) in Shanxi Province, China. In 2003, our population-based surveillance data showed the overall birth prevalence rate of NTDs (including terminations) to be 13.9 per 1000 births in the four-county area. The prevalence rate of each county was greater than 10 per 1000 births.
Data collection
Beginning in November 2002, a case–control study was conducted to probe the risk factors of external structural birth defects in the study area. When any external malformation was identified by the birth defects surveillance system, a newborn infant without identified congenital anomaly in the same county and of the same sex, maternal ethnic group and with the closest date of conception to the case was selected as a control. Trained health-care workers collected the data through face-to-face interviews with mothers of cases and controls in hospitals, private or community general practice clinics, or at home, within the first week after delivery. A structured questionnaire was used to collect the information on the women's sociodemographic characteristics, use of folic acid supplements as well as other potential risk factors. The study was approved by the institutional review boards of Peking University.
In the present analysis, data on the folic acid intake and sociodemographic and obstetric characteristics of control mothers between January 2003 and May 2005 were extracted to evaluate the periconceptional use of folic acid and its association with selected characteristics in the study population.
Definition of folic acid use
Two types of folic acid use were analysed in this study. ‘Any use of folic acid’ was defined as having ever used folic acid supplements related to the last pregnancy regardless of the duration and timing. ‘Periconceptional use of folic acid’ was defined as having used folic acid supplements between 2 months before and 1 month after the last menstrual period and continued for at least 1 month.
Data analysis
Data were entered and checked using EpiData Software (version 2.0; EpiData Association). Statistical analysis was performed with SPSS for Windows (version 11.5; SPSS Inc.). The chi-square test or Fisher's exact test (two-tailed) was used to analyse differences in the rates or proportions among two or more groups in univariate analyses. In multivariate analyses, all variables significant in univariate analyses were added into the logistic regression models simultaneously to evaluate their independent effect, adjusting for each other. Risks were estimated by the odds ratio (OR), and the precision of the OR was assessed by its 95% confidence interval. P < 0.05 was the criterion for significance in univariate analyses. Considering the relatively small sample sizes for multivariate analyses, we used P < 0.10 as the criterion for significance in multivariate logistic regression models.
Results
General characteristics of the study population
From January 2003 to May 2005, 503 control mothers were interviewed. Of the 503 control mothers, 23 (4.6%) did not provide information on folic acid intake, leaving 480 (95.4%) in this analysis. The median age of the women was 25 years, ranging from 16 to 41 years. Most women (477, 99.4%) were Han nationality. The distribution for other demographic and obstetric characteristics is shown in Table 1.
Table 1 Demographic and obstetric characteristics of the 480 respondent women

Status of folic acid use
The status of folic acid use of the respondent women is shown in Table 2. Of the 480 respondents, 49 women (10.2%) reported ever using folic acid supplements related to their last pregnancy, and only 16 women (3.3%) took supplements during the periconceptional period according to our definition. Of the 49 folic acid users, 47 (95.9%) took supplements containing folic acid alone and only one women used a multivitamin containing folic acid. The median cumulative duration of intake was 60 days, ranging from 3 to 212 days.
Table 2 Status of folic acid use among the 480 women who responded

LMP – last menstrual period.
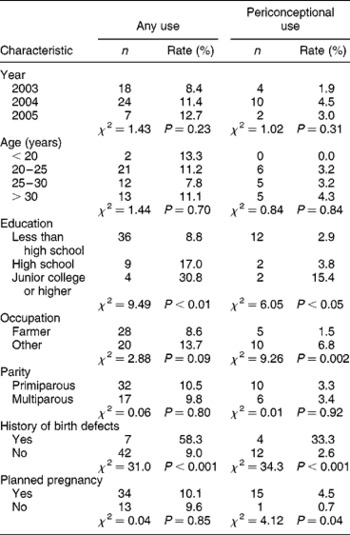
Distribution of folic acid use by selected characteristics
Table 3 presents the distribution of folic acid use by selected characteristics. The percentages of women who reported any use and periconceptional use of folic acid were not significantly different by study year. Both any use of folic acid and periconceptional use were significantly more frequent among women with higher levels of education (P < 0.01 for any use, P < 0.05 for periconceptional use) and among women with a history of birth-defect-affected pregnancy (P < 0.001 for both). Women farmers were less likely to use supplements during the periconceptional period than women with other occupation (P < 0.01). Women who planned their pregnancy more frequently used folic acid during the periconceptional period (P < 0.05). The percentages of any use and periconceptional use did not differ between four age groups or between two parity groups.
Table 3 Distribution of folic acid use by demographic and obstetric characteristics
Multivariate analyses
According to the results of univariate analyses, we employed two logistic regression models in multivariate analyses. In one model, any use of folic acid served as dependent variable, and the variables of education and history of birth defects, which were significant characteristics in univariate analyses, were added into the model as independent variables. In the second model with periconceptional use of folic acid as the dependent variable, education, occupation, history of birth defects and planned pregnancy were added into the model simultaneously as independent variables. The results of multivariate analyses are presented in Table 4. Any use of folic acid was significantly increased among women with high school education (OR = 2.37, P < 0.05) and with junior college or higher education (OR = 4.25, P < 0.05) compared with those having less than high school education, and among women with a history of birth-defect-affected pregnancy (OR = 17.85, P < 0.05). Higher periconceptional use of folic acid was significantly related to junior college or higher education (relative to less than high school; OR = 4.57, P < 0.10), non-farmer occupation (OR = 4.72, P < 0.05), history of birth-defect-affected pregnancy (OR = 32.73, P < 0.05) and planned pregnancy (OR = 7.88, P < 0.10).
Table 4 Results of multivariate logistic regression analyses (α=0.10)
OR – odds ratio; CI – confidence interval.
*P < 0.10; **P < 0.05.
Discussion
In recent years, a number of studies from different countries have reported the status of folic acid use during the periconceptional period. The rate of periconceptional use of folic acid in different regions varied dramatically, from 0.5% to 52%Reference Ray, Singh and Burrows8. According to results from the March of Dimes surveys, 31% of women of childbearing age in the USA reported daily folic acid supplementation in 20029. In Canada, current periconceptional use was reported to be 28% among Toronto womenReference Tam, McDonald, Wen, Smith, Windrim and Walker10. In Israel, the figure was 30.5% in 2002Reference Amitai, Fisher, Haringman, Meiraz, Baram and Leventhal11. In the northern Netherlands, a study performed at the end of 2000 revealed that 61% of women used folic acid in some part of the advised period and 36% used it in the entire advised periodReference De Walle and De Jong-van den Berg13. In a Mediterranean area, although 68% of women had taken folic acid at some time during pregnancy, only 6.9% of the women had taken folic acid during the effective period from 4 weeks before conception to 4 weeks after conception in 2000Reference Coll, Pisa, Palacio, Quinto and Cararach14. In the United Arab Emirates in 1999, 67.9% of women reported intake of supplementary folic acid any time, and 45.5% used it periconceptionallyReference Abdulrazzaq, Al-Gazali, Bener, Hossein, Verghese and Dawodu15. Our study determined that only 10.2% of women reported having ever used folic acid, and very few women (3.3%) used folic acid supplements periconceptionally. The figures did not change markedly from 2003 to 2005. Thus the rates of periconceptional folic acid use among this Chinese population were among the lowest of those reported from other countries.
Although two other approaches can also be used to increase the consumption of folic acid (increasing dietary consumption and fortification of food with folic acid), daily use of supplements is still currently the preferred method in our country. Increased dietary folic acid consumption is not easy to achieve for rural populations owing to poor economic conditions and great difficulty in modifying individual dietary habits. Furthermore, evidence suggests that it is hard to achieve adequate intake of folic acid by diet alone for NTD prevention16. Fortification of food with folic acid was considered the most cost-effective method in other countriesReference Mathews, Honein and Erickson17. But it seems not to be effective in our setting, since most residents in rural areas consume self-planted and self-processed food supplies. In China, tablets containing 0.4 mg folic acid alone were the most common supplements used. A cohort study with very large sample size conducted in our country has indicated that periconceptional intake of supplements containing 0.4 mg folic acid alone can reduce the risk for NTDs by 85% in northern areas of ChinaReference Berry, Li, Erickson, Li, Moore and Wang5. In addition, the tablets are easy to transport, distribute and store, and the cost of folic acid alone is relatively lower than the other two approaches.
Attained education level has been reported in several studies to be positively related to the frequency of folic acid useReference Amitai, Fisher, Haringman, Meiraz, Baram and Leventhal11, Reference Abdulrazzaq, Al-Gazali, Bener, Hossein, Verghese and Dawodu15, Reference Sen, Manzoor, Deviasumathy and Newton18, Reference Sayers, Hughes, Scallan and Johnson19. Our findings have confirmed this association again. Any use of folic acid was more frequent among women with high school education (OR = 2.37, P < 0.05) and with junior college or higher education (OR = 4.25, P < 0.05), compared with those with less than high school education. However, periconceptional use of folic acid was more frequent only among women with education more than high school (OR = 4.57, P < 0.10), and not with high school education (OR = 1.01, P>0.10). This result suggests that high school education increased the frequency of use, but not the frequency of correct use; while education more than high school increased not only the frequency of use, but also the frequency of correct use of folic acid. In our study population, 85.4% of women were educated to junior high school level or lower and only 2.7% of women had education level more than high school. Therefore, education characteristics should sufficiently be taken into account in developing measures of public education during the following campaign.
A Texas study indicated that women at high risk (i.e. those with a history of having an infant with an NTD) were more likely to recall and follow recommendations to use folic acid. Approximately 56.4% of mothers who had infants affected by an NTD recalled receiving postpartum advice to use folic acid, compared with 25.6% of control mothers (P < 0.01)Reference Canfield, Anderson, Waller, Palmer and Kaye20. Our results agree with these findings. Of the 12 mothers with a history of birth-defect-affected pregnancy, seven (58.3%) reported any use of folic acid and four (33.3%) reported periconceptional use, compared with 9.0 and 2.6%, respectively, among the women without birth defects history. Dramatically increased rates of folic acid use were found among mothers with a history of birth-defect-affected pregnancy (OR = 17.85, P < 0.05 for any use; OR = 32.73, P < 0.05 for periconceptional use).
Planned pregnancy was markedly related to periconceptional use of folic acid in our study (OR = 7.88, P < 0.10). This finding is consistent with many other reports from different countriesReference Ray, Singh and Burrows8, Reference Tam, McDonald, Wen, Smith, Windrim and Walker10, Reference Coll, Pisa, Palacio, Quinto and Cararach14, Reference Boome21, Reference Bonin, Bretzlaff, Therrien and Rowe22. In our population the percentage of unplanned pregnancy was 28.3%, similar to that in the Mediterranean area (30.1%)Reference Coll, Pisa, Palacio, Quinto and Cararach14 but markedly higher than that in the northern Netherlands (15%)Reference De Walle and De Jong-van den Berg13.
Another characteristic in our study associated with periconceptional folic acid use was occupation. Women farmers were more likely not to use the folic acid during the periconception period (OR = 4.72, P < 0.05). Noteworthy is that the majority (67.9%) of the women in our population were farmers, of whom 95.6% were less educated (with education less than high school). Therefore farmer women constitute an important population who should be the focus of future public education.
Some studies have revealed a significant association of folic acid intake with age. Hilton reported that inadequate folic acid intake was common in young women aged 18–24 years; the young women frequently had poor nutritional habits and were usually non-contemplators of pregnancyReference Hilton23. Amitai et al. reported that 17–19-year-old women had a lower rate of folic acid utilisation than 25–29-year-old women in the Israeli populationReference Amitai, Fisher, Haringman, Meiraz, Baram and Leventhal11. However, we did not find any marked difference of folic acid use between age groups. In our study, only 15 (3.1%) women were younger than 20 years; therefore the rates of folic acid use may not stable in this age group owing to small sample size.
Our study also revealed that folic acid use was not different between primiparous and multiparous women (10.5 vs. 9.8% for any use, 3.3 vs. 3.4% for periconceptional use). This finding is consistent with results reported by Coll et al.; in their study, the percentage of correct folic acid use was 7.6 and 6.0% for primiparas and multiparas (P = 0.208), respectivelyReference Coll, Pisa, Palacio, Quinto and Cararach14.
To our knowledge, this is the first report on the status of folic acid use in the population of northern China, where the NTD prevalence rate is among the highest in the world. However, our study has some limitations. The subjects of this study were the control mothers from a case–control study. Therefore, they may not represent a completely random sample of the whole population although the study was population-based. The interviews were conducted during the postpartum period and recall bias may have existed to a certain extent. Another limitation of our study could be that the sample size was not large enough. The overall rate of folic acid use in the study population was very low; therefore more subjects were needed to analyse the distribution of folic acid use by characteristics. In order to solve this limitation, we used P < 0.10 as the criterion of significance in multivariate analyses. In addition, items about awareness and knowledge of folic acid, and other important factors which impact on folic acid use, were not included in the questionnaire; therefore the reason for the lower rate of folic acid intake in this population could not be analysed in detail. Further studies should be performed in this population to probe the specific reasons for infrequent folic acid use, such as the cost of supplements, awareness and knowledge, belief, cultural barriers, approaches of public education and so on, so as to provide sufficient evidence for making an effective strategy for a folic acid campaign.
In conclusion, our study findings suggest that the rates of periconceptional folic acid use in our study population were much lower than those in most other countries. The use of folic acid is much more infrequent among less educated women, unexpectedly pregnant women or women who are farmers. Taking into consideration the fact that northern China has an extremely high prevalence rate of NTD, more work should be done in this region to improve preconceptional use of folic acid, with the next step focusing special attention on less educated women and women farmers in the rural area.
Acknowledgements
This work was supported by the Key Technologies Research and Development Program (Grant No. 2002BA709B11) of the Tenth Five-year-Plan for the Nation Scientific and Technological Development of the People's Republic of China.
We are grateful to many local investigators from Pingding, Xiyang, Taigu and Zezhou counties in Shanxi Province for their assistance with data collection, and to the women and their relatives who participated in this research project. We also thank our colleagues in Peking University Health Science Center who contributed to part of the project.
This paper has not been submitted for consideration elsewhere. We declare no competing interests on this paper.






