The latest World Health Organization (WHO) estimates reveal that undernutrition is an underlying cause of 53% of all deaths in children <5 years of ageReference Bryce, Boschi-Pinto, Shibuya and Black1. It has been estimated that more than 2 billion of the world’s population, nearly all in developing countries, are iron-deficient2, 3. Billions of individuals are also at risk for zinc deficiencyReference Prasad4.
Micronutrient deficiency not only affects the health and development of peopleReference Pollitt5–Reference Levin, Pollitt, Galloway, McGuire, Jamison and Mosley9, but also hinders the social and economic development of countries. It is estimated that the loss in economic productivity due to iron deficiency in China is more than 3.6% of the gross national productReference Ross, Chen, He, Gu, Wang and Fu10.
The causes of micronutrient deficiencies include inadequate intakes, impaired absorption and/or utilisation, excessive losses, increased physiological need or the combination of these factorsReference Gibson11. Insufficient intake and poor bioavailability are major causes in developing countries12–Reference Tatala, Svanberg and Mduma14. Micronutrient content and bioavailability can be improved by either increasing the quantity of a micronutrient or increasing enhancing factors/decreasing inhibiting factors in foods using different techniques or sources. Strategies for increasing the effective supply of nutrients fall into two categories, supplementation and food-based approaches. Supplementation is the addition of an element to the diet to solve insufficiency. Food-based approaches consist of food diversification, i.e. increasing the number of different foods or food groups consumed over a given reference periodReference Ruel15, and food fortification. Food fortification is the addition of an ingredient to food to increase the concentration of a particular element, while biofortification is the process of increasing the absolute content or bioavailable concentration of an element in edible portions of crop plants through agronomic intervention or genetic selectionReference White and Broadley16. Supplementation, food fortification and dietary diversification have been the three most widely applied interventions for micronutrient deficiency in past decades. Each intervention has its advantages and disadvantagesReference Allen17.
Information on the magnitude of micronutrient deficiencies and the cost and cost-effectiveness of intervention strategies is needed for prioritising their significance and for developing public policy. However, at the moment, there is a lack of this kind of information in China. The China National Nutrition and Health Survey (CNNHS) conducted in 2002 makes it possible to assess the current situation of micronutrient deficiencies in China and provide information for policy-makers. Therefore, the aims of the present study were to: (1) estimate the populations affected by iron and zinc deficiencies; (2) identify the vulnerable population for intervention; (3) estimate the cost and cost-effectiveness of three interventions; and (4) provide information for policy-makers for developing intervention strategies.
Methods
Estimation of populations with iron and zinc deficiencies
The 2002 CNNHS was a nationally representative survey, which recruited 243 479 individuals from 71 971 households of 132 sites in 31 provinces, autonomous regions and municipalitiesReference Wang18. More detailed information on study designReference Yang, Kong, Zhai, Ma and Jin19 and quality controlReference Piao, Zhang, Zhao, You and Yang20 has been given elsewhere.
Haemoglobin was determined using the cyanomethaemoglobin method (National Committee for Clinical Laboratory Standards, 1994). The WHO definition was used for defining anaemia12. The haemoglobin values were adjusted according to the altitude of the study sites. Anaemia prevalence was adjusted using data of the 2000 China National Population Census21 in order to eliminate the difference in proportion between the sample and the whole population. The population with iron-deficiency anaemia (IDA) was calculated according to the prevalence of anaemia and the ratio of IDA to anaemiaReference Zhang22–Reference He, Wang, Hu and Lin25.
Fasting body weight and height (length) of subjects were measured following the standard procedure26 by trained investigators. The duplicate measurements in subgroups showed a high reproducibility. The absolute technical error of the measurement (TEM) for weight and height were 2.85 and 2.54, respectively, while the relative TEM was 5.6% and 1.73%, respectively. Stunting was defined by Z-score of height-for-age according to WHO criteria27.
Information on food intake was collected using the 24-hour dietary recall method for three consecutive days (two weekdays and one weekend day) by trained interviewersReference Yang, Kong, Zhai, Ma and Jin19. Zinc intake was calculated using the dietary recall data in conjunction with the China Food Composition Table Reference Yang, Wang and Pan28. The bioavailability of dietary zinc is 50%, 30% and 15%, respectively, for people with dietary phytate/zinc ratio in the range <5, 5–15 and >1529. The WHO normative requirements29 of people with different bioavailability were used to assess the inadequacy of zinc intake. The percentage of people with zinc intake below the WHO normative requirement at different phytate/zinc molar ratios was calculatedReference Ma, Jin, Piao, Kok, Bonnema and Jacobsen30–Reference Ma, Li, Jin, Du, Kok and Yang32. The estimation of zinc deficiency is based on zinc inadequacy and not any biochemical markers.
The prevalences of anaemia, stunting and zinc intake inadequacy, in combination with data from the 2000 China National Population Census21, were used for estimation of the absolute number of affected subjects.
Food sources of iron and zinc
The contribution of individual foods to iron/zinc was calculated by summing the amount of iron/zinc consumed from each food by all subjects in each age group and dividing it by the total intake from all foods for all subjectsReference Block, Dresser, Hartman and Carroll33.
Estimated costs and cost-effectiveness of different interventions
The costs per capita and cost-effectiveness of supplementation and fortification for iron and zinc were obtained from the results of the total population-level costs for the Western Pacific Region B, for the year 2000, by WHOReference Murray, Evans, Acharya and Baltussen34. The standard WHO ingredients approach, with separate specification of units of utilisation and costs, is adoptedReference Murray, Evans, Acharya and Baltussen34. Costs are expressed in international dollars (I$) to facilitate more meaningful comparisons across regions. An international dollar has the same purchasing power as the US$ has in the USA. Costs in local currency units are converted to I$ by use of the PPP (purchasing power parity) exchange rate rather than official exchange rates35. The costs of an intervention programme are costs per year (I$, millions) per one million population, i.e. cost per capita. The cost-effectiveness is measured by the cost per disability-adjusted life-year (DALY) saved.
The costs per capita and cost-effectiveness of health education through mass media for the entire populationReference Murray, Lauer, Hutubessy, Niessen, Tomijima and Rodgers36 were used for dietary diversification through health education because more specific information was not available.
The costs of biofortification were calculated based on the literatureReference Bouis37. The areas of rice and wheat harvested were 28 × 106 and 22 × 106 ha, respectively, in China38. For a single staple crop, the estimated central fixed cost of developing iron-dense/zinc-dense varieties over 10 years is I$12.5 millionReference Bouis37. The central fixed costs include costs of nutritional studies to establish efficacy and to demonstrate impact after adoption. The cost for developing iron-dense/zinc-dense rice and wheat varieties is I$25 million for a 10-year period.
The estimated cost for adaptive breeding per province for growing conditions in China for the same 10-year period is I$2.5 million. There are 17 provinces for growing rice and nine provinces for growing wheat. The estimated cost of two crops in those areas is I$65 million [(17 × 2.5 × 106) + (9 × 2.5 × 106)].
The extension costs are estimated to be I$1 per adopted hectare. If adoption occurs on 50% of the rice and wheat areas in China, there will be 25 × 106 ha [(50% of 28 × 106) + (50% of 22 × 106)]. Thus the fixed undiscounted extension cost is I$25 million. The total investment in iron-dense/zinc-dense rice and wheat is therefore I$115 million over 10 years, or I$11.5 million per annum. The estimated cost per capita is I$0.01 (Table 4).
Results
Populations affected by iron and zinc deficiencies in China
Table 1 presents the prevalence of anaemia and the estimated populations affected by anaemia and IDA in China. The overall prevalence of anaemia was 20.1% and 31.1% of children <2 years were anaemic. Nearly 30% of adults >60 years, pregnant and lactating women, and 20% of women of reproductive age were anaemic. The estimated population affected by anaemia was 245 million, and 208 million of these were due to iron deficiency. Three-quarters of these affected populations were found in rural areas.
Table 1 Prevalence of anaemia, and estimated affected populations in China
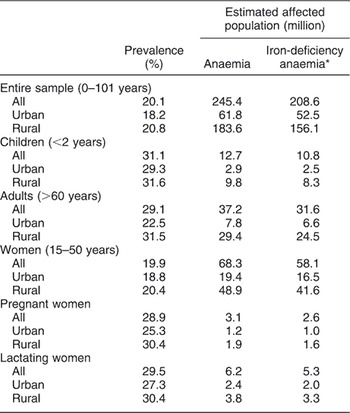
*Anaemia due to iron deficiency is estimated at 85%.
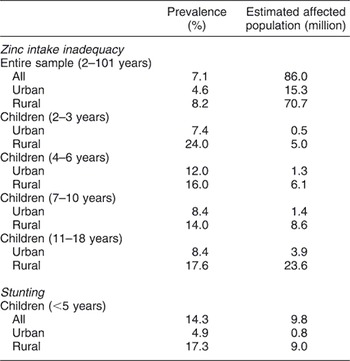
The prevalence of zinc intake inadequacy and stunting, and the estimated affected populations in China, is shown in Table 2. More rural residents had inadequate zinc intake than their urban counterparts (8.2% vs. 4.6%). Zinc intake inadequacy among rural children was two- to threefold greater in comparison with their urban counterparts. In addition, 14.3% of rural children <5 years were stunted. The estimated populations affected by zinc intake inadequacy and stunting were 86 million and 10 million, respectively, and the majority of them were living in rural areas.
Table 2 Prevalence of zinc intake inadequacy and stunting, and estimated affected populations in China
Food sources of iron and zinc for people in China
The food sources of iron and zinc are presented in Table 3. The highest proportions of iron (47.7%) and zinc (53.9%) were found in staple foods including rice, wheat and their products. Staple foods provided even more iron (52.1% vs. 37.0%) and zinc (58.9% vs. 41.4%) for rural residents than for their urban counterparts. As expected, animal products provided more iron (19.6% vs. 10.5%) and zinc (34.5% vs. 18.6%) for urban residents than their rural counterparts because of their higher meat intake. Staple foods were also the major sources of phytate for both rural (82.1%) and urban (77.6%) residents. Vegetables contributed about 17% of iron, 11% of zinc, and only 7% of phytate.
Table 3 Food sources of iron, zinc and phytate of people in China (%)

Costs per capita and cost-effectiveness of different interventions
Table 4 presents the costs per capita and the cost-effectiveness of four interventions for iron and zinc deficiencies. For intervention on iron deficiency, the costs per capita per year of dietary diversification, supplementation, food fortification and biofortification were estimated to be I$1148, I$11.4, I$0.06 and I$0.01, respectively. The cost-effectiveness for supplementation, food fortification and dietary diversification were I$179, I$66 and I$103 per DALY, respectively, and that for biofortification could not be determined.
Table 4 Cost per capita and cost-effectiveness of the interventions

I$ – international dollars; DALY – disability-adjusted life-year; NA – not applicable.
For zinc deficiency intervention, the costs per capita per year of dietary diversification, supplementation, food fortification and biofortification were I$1148, I$0.05, I$0.01 and I$0.01, respectively. The cost-effectiveness for supplementation, food fortification and dietary diversification were I$399, I$153 and I$103 per DALY, respectively.
Discussion
The present study indicated that iron and zinc deficiencies affect over 300 million people in China, most of them being women and children living in rural areas.
It turned out that staple foods provide about 50% of iron and zinc intake but, at the same time, they contain most of the phytate, which inhibits the bioavailability of iron and zinc. The costs per capita and the cost-effectiveness for the different intervention strategies varied considerably. This information is crucial for developing public health policy in China.
The first strength of the present study is that it used the latest nationally representative data for estimation of the magnitude of iron and zinc deficiency and for the identification of vulnerable groups. The second strength is the quality of the dietary assessment method, including an updated food composition table. Moreover, the standard WHO ingredients approach was used for estimating the costs and cost-effectiveness of the different interventions. One limitation is that the data we used to estimate iron deficiency was IDA, not including mild-to-moderate iron deficiency in which anaemia is absent; therefore, there was an underestimation of the prevalence of iron deficiency to some extent. As the dietary intake data covered only a few days which did not represent the ‘usual intakes’, we might have overestimated the zinc inadequacy prevalence in this study. Another limitation is that the cost-effectiveness of biofortification could not be estimated because there are not enough biofortified foods available at present and studies examining the effectiveness of biofortified foods on the micronutrient status of human subjects are lacking.
Interventions to end micronutrient malnutrition are known to be the most cost-effective investments in the health sector39, Reference Horton40. Actions to solve this problem comprehensively and sustainably would cost less than 0.3% of the gross domestic product (GDP). In contrast, failure to take action would result in a loss of 2–3% of the GDP41. The economic and social pay-offs from intervention programmes can reach as high as 84 times the programme costs.
Supplementation, food fortification and dietary diversification have been the three most widely applied interventions for micronutrient deficiencies in past decades. Supplementation of vitamin A, iron and zinc has been proved effective in developing countries for the improvement of mineral status in deficient individualsReference Allen17, Reference Hallberg and Rossander42–45. However, its sustainability is questionable because various economic, social and political difficulties might diminish the effectiveness at reaching all of the people at riskReference McGuire46. Considering the high prevalence of iron and zinc deficiencies among important subpopulations in China and recommendationsReference Yip47, Reference Stoltzfus and Dreyfuss48, supplementation programme(s) targeting the population ‘at risk’ can be considered a short-term intervention.
Fortification has been successfully applied to improve the nutritional quality of the food supply in industrialised countries for many decadesReference Mertz49–Reference Allen52, but has only recently been adopted in developing countriesReference Haas and Miller53, Reference Chen, Zhao, Zhang, Yin, Piao and Huo54. It has the advantage of wide coverage, being easy to implement and cost-effectiveness55. The challenge is to reach the most needed subset of the population who seldom consume processed cereals. In China, more than 60% of the population lives in rural areas and almost all households have their staples processed at the local, small mill instead of getting processed cereals from the market. It is a challenge to reach these people and the subpopulations living in remote and mountainous areas. No further national programme for iron fortification is needed in China at present because programmes of wheat flour and soy sauce fortification have been implemented since 200341.
Lack of dietary diversity is a particular problem among the rural population in China because their diets are predominantly based on staples and often include low amounts of animal foodsReference Zhai, He, Ma, Li, Wang and Hu56. The permanent solution is to persuade people to change their diets. Once the programme succeeds, it will sustain and require no regular re-supply of supplementation/fortification. However, usually it is difficult to change dietary practices. Micronutrient-rich foods are often expensive, and the poor cannot afford themReference Ruel15. Although the costs are high, from a sustainability perspective it would be useful to develop a national health education programme and combine it with existing programmes, such as the Poverty Reduction and Health Education for Peasants, so that resources will be used in the best way. The cost and cost-effectiveness data we used for dietary diversification are in fact the cost of mass media on health education on lowering systolic blood pressure and cholesterol; owing to the paucity of relative research, more studies in this area are surely needed in the future.
In recent years, more and more scientists in the fields of both of agriculture and nutrition have come to believe that biofortification is a promising, cost-effective and sustainable intervention for alleviating micronutrient deficiency, especially for developing countries. Genetic variation in concentrations of minerals and phytate exists among cultivars, which makes the selection of nutritionally appropriate breeding materials possibleReference White and Broadley16. However, most biofortified cereals are still in the development stage at present, and only one small randomised controlled trialReference Haas, Beard, Murray-Kolb, del Mundo, Felix and Gregorio57 on iron-biofortified rice has been conducted. Zinc-dense wheat varieties have been developed and are already being grown on a commercial basis in Australia (Adelaide, VictoriaReference White and Broadley16).
Biofortification has the potential to have a great impact on the micronutrient intake of people in China, who derive about 50% of their iron and zinc from two staples, rice and wheat, and their products. The bioavailability of iron and zinc in the diet depends not only on the absolute content of iron, zinc and phytate, but also on the relative content (i.e. the molar ratio of phytate to minerals). Simultaneously increasing the mineral content and decreasing the phytate content of staple foods through biofortification would have a direct and profound influence on the nutritional status of the entire population. But more trials are needed to demonstrate that these new biofortifed cereals are efficacious in preventing deficiencies of iron and zinc. Biofortification of vegetables can also be considered as an option, especially with adequate energy in the food, because vegetables are rich in ascorbic acid which may enhance iron absorption and play an important role in the daily diet. Biofortification provides a feasible means of reaching populations in remote and rural areas, delivering naturally fortified foods to people with limited access to supplementation/commercially marketed fortified foodsReference Bouis37. In this way, there would be no need to change dietary practices. Biofortification is cost-effectiveReference Haas, Beard, Murray-Kolb, del Mundo, Felix and Gregorio57, Reference Bouis, Roos, Bouis, Hassan and Kabir58, although detailed cost-effectiveness estimates are not available. The annually recurrent costs are low after the one-time investment to develop varieties, and germplasm with increased minerals and decreased phytate content can be shared internationally. Moreover, as the trace mineral requirements between human and plant nutrition are similar, biofortification could improve human nutrition as well as plant yield in a way that is environmentally beneficialReference Suharno, West, Muhilal, Karyadi and Hautvast43, Reference Ridwan, Schultink, Dillon and Gross44. However, there are still a lot of questions left to be answered, like regulation and policy, safety, bioavailability, cost-effectiveness and consumer acceptance, before it can be widely applied. A link between the agriculture and nutrition sector needs to be established to solve the problem of micronutrient deficiency. The agricultural sector must adopt a specific goal of improving human nutrition and health, while the nutrition and health sectors must adopt agricultural interventions as a primary tool to fight malnutritionReference Welch59.
It is acknowledged that no single intervention by itself can solve the micronutrient deficiency problem. The success of biofortification does not mean there is no need for other strategies in the future. Supplementation, fortification and dietary diversification will continue to be used not only for ending nutritional deficiencies but also for preventing diet-related diseasesReference Caballero60.
In conclusion, iron and zinc deficiencies affect a large number of people in China, especially women and children in rural areas. Supplementation and fortification can be used as short-term interventions for micronutrient deficiencies, while dietary diversification and biofortification could be long-term interventions. Biofortification might be a feasible, cost-effective and sustainable solution for the rural population in China.
Acknowledgements
The 2002 China National Nutrition and Health Survey was supported by the Ministry of Health and the Ministry of Science and Technology, China (2001DEA30035, 2003DIA6N008). We thank all team members and all participants from 31 provinces. We are very appreciative of the support of UNICEF, WHO, Unilever China and the Danone Nutrition Institute China.






