Ending all forms of childhood malnutrition, including stunting, wasting and underweight, is a global priority(1,2) . In 2021, a multi-agency report estimated that the global prevalence of stunting had decreased from approximately 33·0 % in 2000 to 22·0 % in 2020, and wasting had improved slightly from about 8·0 % to 7·0 % between 2012 and 2020(3). Despite these improvements, there exist global childhood nutrition disparities within and between countries(Reference Kinyoki, Ross and Lazzar-Atwood4–Reference Ahmed, Agho and Page6). Some reports suggest that these improvements are not enough to successfully achieve the global nutrition targets of ending malnutrition by 2030(1,2,7) . In sub-Saharan African countries, including Ethiopia, where there is a high burden of stunted, wasted and underweight children, the possibility of not attaining the nutrition targets is even greater(3,Reference Amaha8) .
Ethiopia is the second most populous country in Africa(9,Reference Mehretu, Marcus Harold and Crummey10) , but also a landlocked country since the 1993 secession of Eritrea(9). In the past two decades, Ethiopia has seen remarkable progress in reducing the burden of under-five mortality (from 166 deaths per 1000 in 2000 to 67 deaths per 1000 in 2016) and stunting (from 58·0 % in 2000 to 37·0 % in 2019)(11–14). Although these improvements are important and commendable, it is concerning that one in fifteen children die before the age of 5 years(12), and undernutrition remains a major contributor (28 %) to these deaths in the country(15). Furthermore, there is an ongoing strain on the Ethiopian economy, from natural and man-made disasters (e.g. conflicts and internal displacements)(16,Reference Rajkumar, Gaukler and Tilahun17) , which subsequently increases the vulnerability to low-yield crop production, food insecurity(Reference Ashraf, Iftikhar and Shahbaz18,19) and malnutrition(Reference Bahwere20–Reference Gaire, Delbiso and Pandey22).
Building on the Sustainable Development Goals(2) and the UN Decade of Action on Nutrition (2016–2025)(1), Ethiopia has implemented several programmes to eliminate childhood malnutrition. In 2015, the ‘Seqota’ Declaration was launched ‘to end stunting in children under 2 years by 2030 in Ethiopia’(23). The Seqota Declaration employed a multisectoral approach and comprises three phases – the Innovation, Expansion, and Scale-up phases, and three pathways – nutrition-specific, nutrition-sensitive and infrastructure interventions(23). To provide a national framework for the coordinated implementation of nutritional interventions, the National Nutrition Program (NNP-II) was developed in 2016. This programme aimed to reduce undernutrition and micronutrient deficiencies, improve maternal and child health, and enhance the capacity of the health system to deliver quality nutrition services(24).
Furthermore, in 2018, the National Food and Nutrition Policy was endorsed, which addresses the immediate and underlying causes of malnutrition in Ethiopia, focusing on the prevention and treatment of undernutrition and micronutrient deficiencies(25). In 2021, the Ethiopian Health Sector Transformation Plan (HSTP-II) was launched to improve the overall population’s health outcomes, including children’s nutritional outcomes, by strengthening the maternal health system and increasing access to quality health services(26). These programmes and policies aim to enhance the effectiveness and sustainability of Ethiopia’s efforts to combat childhood malnutrition.
Despite the implementation of these strategic policy interventions to improve the nutritional and growth outcomes of Ethiopian children, no systematic review has examined the impacts of these interventions. Information on the effectiveness of these interventions is essential in understanding current gains, gaps and future priorities, where decision-makers and public health practitioners can increase efforts to improve the nutritional status of children. Accordingly, the main aim of this systematic review is to investigate the impacts of community-based and health facility interventions that set out to address the nutritional status of under 5 years of age children in Ethiopia.
Methods
This systematic review was reported following the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement(Reference Moher, Shamseer and Clarke27) (see online Supplemental file 1)
Eligibility criteria
The eligible studies for this study needed to fulfil the following criteria:
-
1) Study design: Experimental or quasi-experimental studies, including randomised controlled trials (RCTs), non-RCTs, before and after studies, and interrupted time-series studies, with or without comparison groups or clusters;
-
2) Interventions: Community-based and health facility interventions targeted pregnant women and mothers with children under 5 years of age. These interventions included nutritional education and counselling, interpersonal communication, mass media campaigns, nutrition-sensitive agricultural activities, group recipe demonstration sessions, micronutrient supplementation, and the strengthening of health facilities. Our study excluded interventional studies on vulnerable groups, such as pregnant women and children, in emergencies;
-
3) Outcome measures: Measurement of child anthropometric outcomes, such as stunting (height/length-for-age z-scores), wasting (weight-for-length/height z-scores) and underweight (weight-for-age z-score), in continuous or dichotomous forms; and
-
4) Language and location: The studies needed to be published in the English language and conducted in Ethiopia from the year 2000 to November 2022.
The primary reason for selecting this period was to analyse the impacts of global initiatives, such as the Millennium Development Goals (MDG)(28) and the current Sustainable Development Goals, on the nutritional status of children in Ethiopia(29).
Information sources and search strategy
A three-stage search strategy was implemented to locate both peer-reviewed articles and grey literatures, consistent with prior systematic reviews(Reference Dol, Richardson and Tomblin Murphy30–Reference Ahmed, Agho and Page32). In stage one, we conducted a manual search to check for previously published systematic reviews of interventions on childhood malnutrition in Ethiopia. In stage two, an initial search was conducted using PubMed ID to generate standard and key terms through the online tool ‘Yale MeSH Analyser’ (https://mesh.med.yale.edu/). In the last stage, a full search was performed on five computerised electronic databases (including Embase/Ovid, PsychINFO/EBSCOhost, Academic Search database/EBSCOhost, MEDLINE(Ovid)/PubMed and Cumulative Index to Nursing and Allied Health Literature (CINAHL)/ EBSCOhost) to locate peer-reviewed articles. Whereas Google Scholar and Open Dissertation were used to locate grey literatures. The search strategy was devised with the Population Intervention Comparator Outcome (PICO) criteria, and all identified index and keywords terms were slightly adapted for each of the information sources. The initial and the top-up searches were conducted in August 2022 and November 2022, respectively. Supplemental file 2 provides the search strategy for the MEDLINE (Ovid) database.
The search terms/keywords used included:
Term 1 (Population): child, infant, newborn, baby, neonate, perinatal, postnatal, kid, toddler, young child, paediatric, mother, female, women and caregiver.
Term 2 (Interventions)
-
Education and counselling: breast-feeding promotion, breast-feeding support, breast-feeding education, health education, health promotion, nutrition education, food education, parent education, mother education, counselling, and nutritional counselling.
-
Social behavioural change communication: health behaviour, health-related behaviour, behaviour change, communication, interpersonal communication, information education communication, behaviour change communication (BCC), social change, social movement, social mobilisation, social behaviour, social network, peer group, advocacy, advocacy group, mass communication, mass media, print media, mobile phone, mHealth, eHealth, internet, radio, social media, television, text message and social market.
-
Community-based approaches: baby-friendly community initiative, community programme, community project, home visit, community health action, community health service, community healthcare, community intervention, community engagement, community leader, community mobilisation, demonstration, cooking demonstration, community role play, model breast-feeding community, community health worker and health extension worker.
-
Facility-based approaches: maternal care, child healthcare, child health service, paediatric healthcare, neonatal care, newborn care, rooming-in-care, newborn nursery, essential nutrition action, caregiver contact, baby-friendly hospital initiative, BFHI, antenatal care, postnatal care, Kangaroo care and skin-to-skin contact.
-
Intervention designs: effectiveness, impact, evaluation study, programme evaluation, healthcare programme, project, health project, experimental study, interventional study, quasi-experimental study, RCT, clinical trial, cluster-randomised trial, time-series study, control, placebo, comparison and usual care.
Term 3 (Context): Ethiopia.
Term 4 (Outcomes): stunting, wasting, undernutrition, malnutrition, thinness, hunger, growth disorders, developmental disorders, nutritional disorders and nutritional status.
Study selection
All documents retrieved from the search database were exported to EndNote library version 20.2.1 (The EndNote Team, Philadelphia) for initial title/abstract screening(33). Two reviewers (K.Y.A. and F.A.O.) independently conducted the title and abstract screening using the pre-formed inclusion and exclusion criteria. Articles passing the initial screening were subjected to a full-text review. The full text of the included studies was then checked independently by two reviewers (K.Y.A. and F.A.O.) using the eligibility criteria. We excluded studies that did not meet the eligibility criteria and the reasons for the exclusion of studies recorded and reported. Disagreements between the two independent reviewers were resolved by consensus and arbitration with the third reviewer (T.K.T.).
Data collection process and data items
Using an adapted form from the Cochrane Pregnancy and Childbirth Group for Systematic Reviews(34), K.Y.A. carried out the data extraction and F.A.O. independently verified the extracted data. Eligible studies were identified using the following information: first author, publication year, study design and setting, study participants, sample size, geographical region, intervention components, location of intervention delivery, target group, intervention period, outcome measures, statistical analysis, and results. For eligible studies with incomplete information, a total of two contact attempts were made, and if no response was received, only the information available was used.
Risk of bias assessment
Two reviewers (K.Y.A. and T.K.T.) independently checked eligible studies for selection, performance, attrition, detection and reporting biases. The Cochrane risk of bias tools for randomised trials (ROB 2.0) for individual RCT, the revised ROB 2.0 CRT for cluster RCT(Reference Higgins and Green35,Reference Sandra, Marion and Michael36) and the risk of bias in non-randomised studies – of interventions (ROBINS-I) for quasi-experimental studies(Reference Sterne, Hernán and Reeves37) were used for the risk of bias assessment. Cluster-randomised trials were assessed for six domains (i.e. bias from randomisation process, identification or recruitment bias, deviations from intended interventions, missing data, measurement of outcomes and selection of reported result), and quasi-experimental studies were assessed for seven domains (i.e. confounding, selection of participants, classification of interventions, deviations from intended interventions, missing data, measurement of outcomes and selection of reported result). For RCT, the overall risk of bias included low risk, some concerns and high risk(Reference Higgins and Green35,Reference Sandra, Marion and Michael36) . Likewise, for quasi-experimental studies, the overall risk of bias included low, moderate, serious and critical risk of bias(Reference Sterne, Hernán and Reeves37).
Results synthesis
Given the heterogeneity of participants, intervention duration, type of interventions and outcome measures, we narratively reported the author’s reports of effect size measures for each study. Effect size measures included a comparison between experimental and control groups (e.g. OR), the difference in proportion between pre- and post-outcome measures (e.g. change in proportion) and the difference-in-difference (DID) measures. As appropriate, 95 % CI and P-values were also obtained from eligible studies.
Results
Description of studies
Our database search identified 4443 studies, and 1626 duplicates were removed from this subset of studies. Out of 2817 articles screened for titles and abstracts, seventy-eight were retained for full-text eligibility checks and eighteen articles were found to be eligible for this study (Fig. 1). Supplementary file 3 presents the list of excluded studies.

Fig. 1 The 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart for the selection of eligible studies(Reference Page, McKenzie and Bossuyt74)
The included studies were ten cluster RCT(Reference Ferede Habtmiriam, Belachew Lema and Abera Wordofa38–Reference Han, Kim and Park47), six quasi-experimental studies(Reference Mekonnen, Tadesse and Dawed48–Reference Fenn, Bulti and Nduna53) and two RCT(Reference Akalu, Taffesse and Gunaratna46,Reference Argaw, Wondafrash and Bouckaert54) . The most common location for the delivery of interventions was Oromia Region(Reference Ferede Habtmiriam, Belachew Lema and Abera Wordofa38,Reference Abdulahi, Fretheim and Argaw40,Reference Passarelli, Ambikapathi and Gunaratna42,Reference Kang, Kim and Sinamo45–Reference Han, Kim and Park47,Reference Bidira, Tamiru and Belachew49,Reference Samuel, Brouwer and Feskens50,Reference Argaw, Wondafrash and Bouckaert54) , followed by Amhara Region(Reference Ayalew and Belachew39,Reference Passarelli, Ambikapathi and Gunaratna42–Reference Kim, Nguyen and Yohannes44,Reference Mekonnen, Tadesse and Dawed48,Reference Fenn, Bulti and Nduna53) . Additionally, there were studies conducted in the Southern Nations Nationalities and Peoples (SNNP)(Reference Teshome, Whiting and Green41,Reference Passarelli, Ambikapathi and Gunaratna42,Reference Akalu, Taffesse and Gunaratna46,Reference Samuel, Brouwer and Feskens50–Reference Kim, Rawat and Mwangi52) and Tigray regions(Reference Kim, Rawat and Mwangi52). In the review, no interventional studies were published for the regions of Afar, Somali, Harari, Gambella, and Benishangul, or Addis Ababa and Dire Dawa city administrations.
The most common type of interventions were BCC such as nutritional education(Reference Abdulahi, Fretheim and Argaw40,Reference Mekonnen, Tadesse and Dawed48,Reference Bidira, Tamiru and Belachew49,Reference Mulualem, Henry and Berhanu51,Reference Fenn, Bulti and Nduna53) , educational materials(Reference Ferede Habtmiriam, Belachew Lema and Abera Wordofa38,Reference Ayalew and Belachew39,Reference Kim, Nguyen and Yohannes44,Reference Bidira, Tamiru and Belachew49) , cooking demonstrations(Reference Ferede Habtmiriam, Belachew Lema and Abera Wordofa38,Reference Ayalew and Belachew39,Reference Teshome, Whiting and Green41,Reference Kang, Kim and Sinamo45,Reference Bidira, Tamiru and Belachew49,Reference Mulualem, Henry and Berhanu51) , group discussion forums(Reference Ayalew and Belachew39,Reference Abdulahi, Fretheim and Argaw40,Reference Bidira, Tamiru and Belachew49) , home visits and supervision(Reference Ayalew and Belachew39,Reference Teshome, Whiting and Green41,Reference Kang, Kim and Sinamo45,Reference Mekonnen, Tadesse and Dawed48) , breast-feeding support(Reference Abdulahi, Fretheim and Argaw40) and community mobilisation(Reference Kim, Nguyen and Yohannes44,Reference Kim, Rawat and Mwangi52) . Additionally, there were interventions involving food vouchers(Reference Han, Kim and Park47), micronutrient supplementations(Reference Mohammed, Marquis and Aboud43,Reference Samuel, Brouwer and Feskens50,Reference Argaw, Wondafrash and Bouckaert54) , provision of chicken(Reference Passarelli, Ambikapathi and Gunaratna42) and quality protein maize (maize varieties fortified with elevated lysine and tryptophan levels)(Reference Akalu, Taffesse and Gunaratna46). A publication by Akalu et al. reported two different studies in a single article(Reference Akalu, Taffesse and Gunaratna46). Table 1 shows the summary of eligible studies.
Table 1 Summary of eligible studies

BCC, behaviour change communication; ACGG, African Chicken Genetic Grains; ATONU, agriculture to nutrition; SNNP, Southern Nations Nationalities and Peoples; RCT, randomised controlled trials.
Risk of bias in included studies
Of the ten cluster RCT, six had a high risk of bias(Reference Ferede Habtmiriam, Belachew Lema and Abera Wordofa38,Reference Ayalew and Belachew39,Reference Passarelli, Ambikapathi and Gunaratna42,Reference Kang, Kim and Sinamo45–Reference Han, Kim and Park47) and two studies had a low risk of bias(Reference Abdulahi, Fretheim and Argaw40,Reference Kim, Nguyen and Yohannes44) (Fig. 2). Similarly, of the six quasi-experimental studies, three studies had a serious risk of bias(Reference Mekonnen, Tadesse and Dawed48,Reference Mulualem, Henry and Berhanu51,Reference Fenn, Bulti and Nduna53) , while two had a moderate risk of bias(Reference Samuel, Brouwer and Feskens50,Reference Kim, Rawat and Mwangi52) (Fig. 3). One of the two RCT was judged to have a high risk of bias(Reference Akalu, Taffesse and Gunaratna46) (Fig. 4).
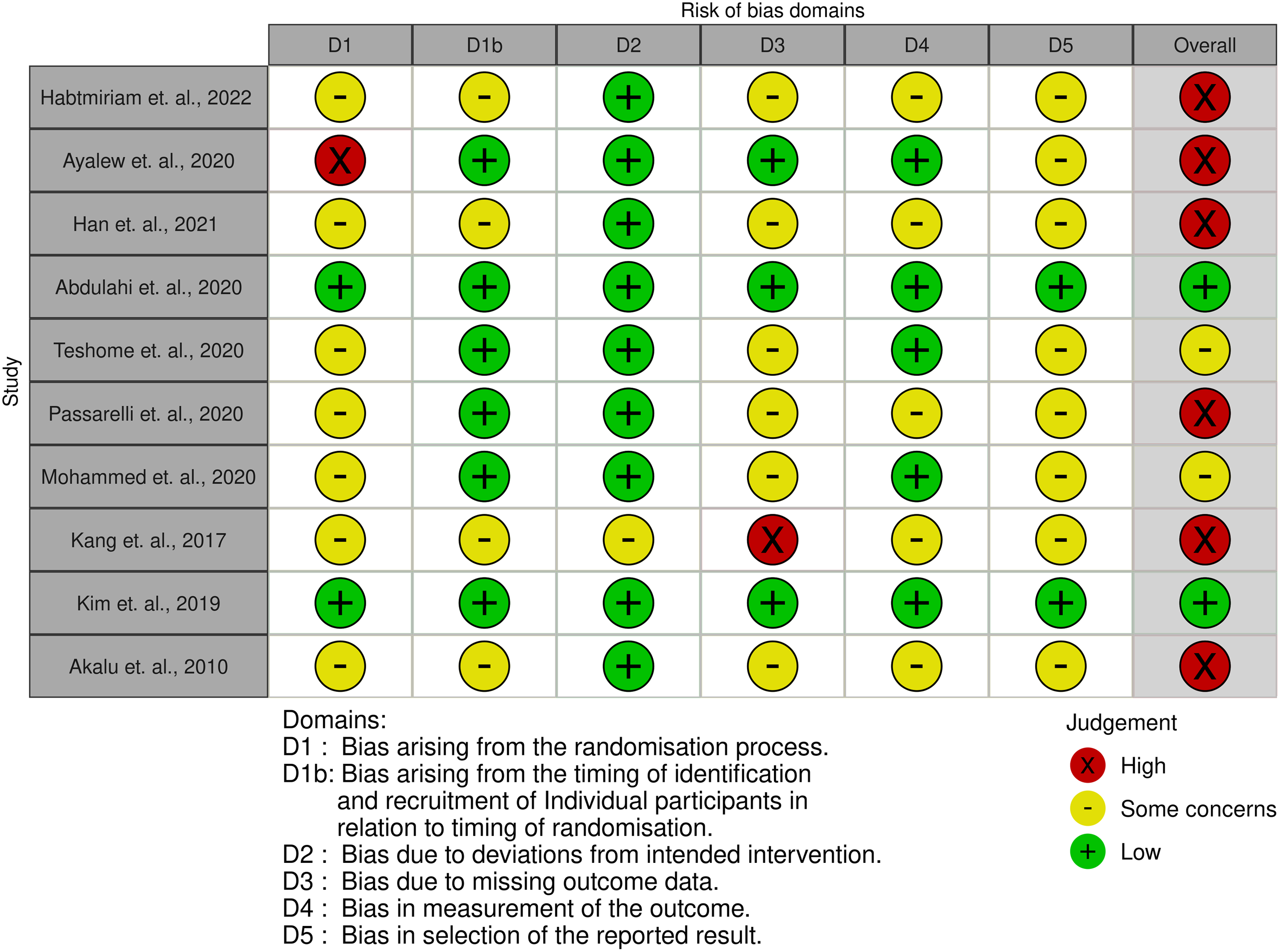
Fig. 2 Risk of bias traffic light plot for cluster RCT: review authors’ judgements about each risk of bias item for each study

Fig. 3 Risk of bias traffic light plot for quasi-experimental studies: review authors’ judgements about each risk of bias item for each study

Fig. 4 Risk of bias traffic light plot for individual RCT: review authors’ judgements about each risk of bias item for each study
Impact of interventions on stunting/height-for-age Z-score
This review included eighteen eligible studies, three of which focused on pregnant women, while the remaining fifteen studies targeted postpartum mothers and children aged 0–59 months. The interventions for pregnant women included breast-feeding education and peer support(Reference Abdulahi, Fretheim and Argaw40), community-level salt monitoring and control(Reference Mohammed, Marquis and Aboud43), and water, sanitation and hygiene (WaSH) programmes(Reference Fenn, Bulti and Nduna53). However, except for WaSH interventions that targeted pregnant mothers and children under 2 years of age in the form of protected water supply and sanitation education(Reference Fenn, Bulti and Nduna53), none of the studies targeting pregnant women demonstrated a significant impact on stunting.
Of the fifteen interventional studies implemented on postpartum mothers and children aged 0–59 months, only five studies showed significant impacts of the interventions. Mekonnen et al. reported improvements in children’s length-for-age z-score through nutritional education interventions for mothers/caregivers of infants aged less than 1 year (MD = −0·73; 95 % CI (−1·40, −0·06), P-value = 0·034)(Reference Mekonnen, Tadesse and Dawed48). A 16-week combination of BCC and food vouchers for mothers/caregivers of children aged 6–20 months resulted in a significant decrease in childhood stunting (percentage change in proportion = 9·7 %, P-value < 0·05). However, separate interventions of BCC and food vouchers did not have impacts on stunting(Reference Han, Kim and Park47). Kang et al. found improvements in the height-for-age z-score of children with a 12-month complementary feeding programme (including group nutritional sessions and cooking demonstrations for mothers, and supervision and training of health workers) for mothers/caregivers with children aged 6–12 months (MD = 0·32; 95 % CI (0·08, 0·56), P-value < 0·001)(Reference Kang, Kim and Sinamo45) (Table 2).
Table 2 Summary of evidence from review studies
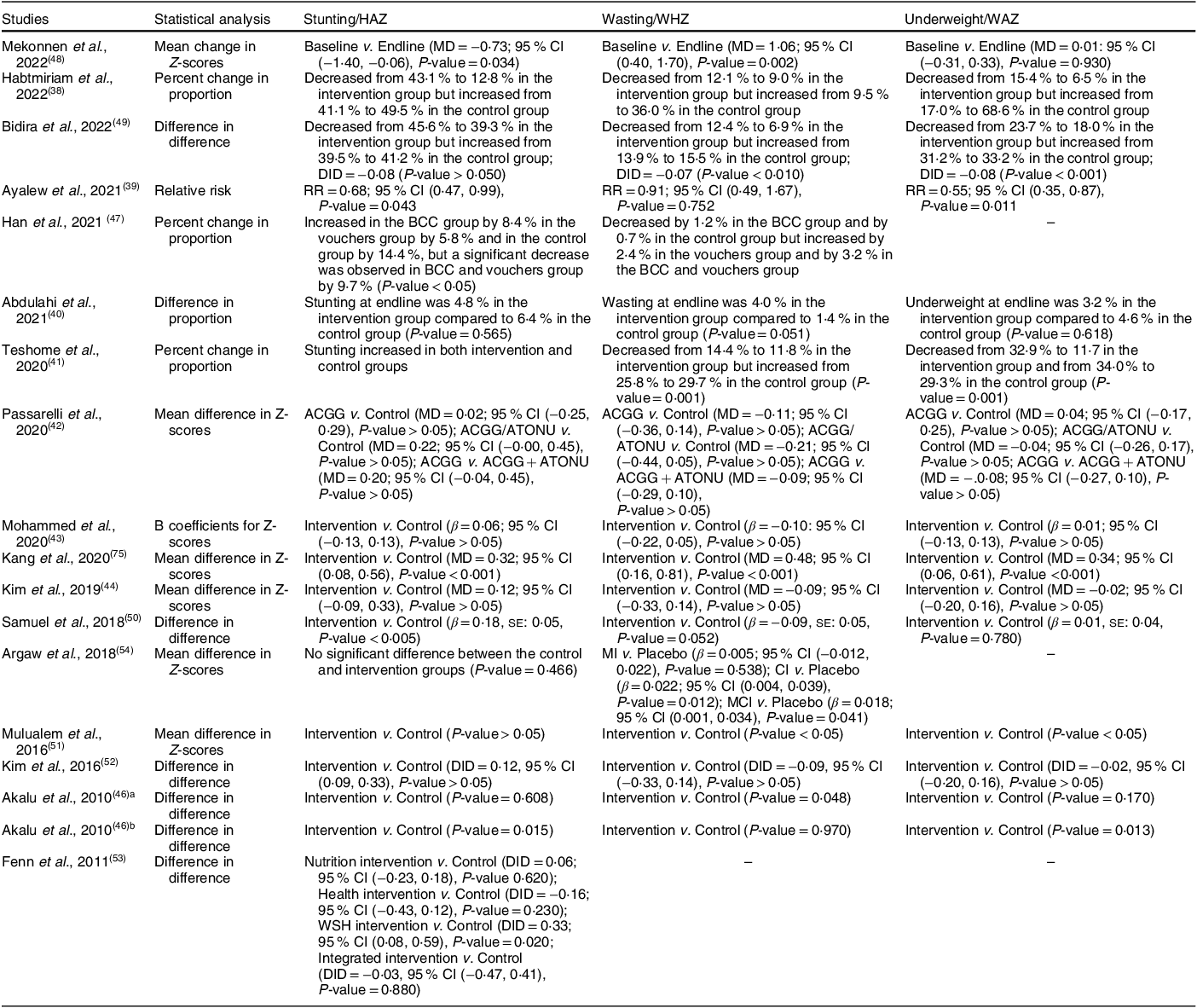
HAZ, height-for-age z-score; WHZ, weight-for-height z-score; WAZ, weight-for-age z-score; MD, mean difference; DID, difference in difference; RR, relative risk; BCC, behaviour change communication: ACGG, African Chicken Genetic Grains; ATONU, agriculture to nutrition.
A 12-month intervention using micronutrient powder supplementation for mothers/caregivers with children aged 6–12 months showed an improvement in children’s length-for-age z-score (β = 0·18, se: 0·05, P-value < 0·005)(Reference Samuel, Brouwer and Feskens50). Additionally, an RCT demonstrated a positive impact on children’s height-for-age z-score when quality protein maize was provided to mothers/caregivers with children aged 7–56 months for 11 months (P-value = 0·015)(Reference Akalu, Taffesse and Gunaratna46)(Table 2). However, two studies showed an increase in the level of stunting after the implementation of BCC interventions(Reference Ayalew and Belachew39,Reference Teshome, Whiting and Green41) , and one study reported a decrease in the proportion of stunting but did not report statistical significance(Reference Ferede Habtmiriam, Belachew Lema and Abera Wordofa38). The remaining studies did not demonstrate positive impacts of relevant nutritional interventions on stunting(Reference Passarelli, Ambikapathi and Gunaratna42,Reference Kim, Nguyen and Yohannes44,Reference Bidira, Tamiru and Belachew49,Reference Mulualem, Henry and Berhanu51,Reference Kim, Rawat and Mwangi52,Reference Argaw, Wondafrash and Bouckaert54) (Table 2).
Impacts of interventions on wasting/weight-for-height z-score
Six out of seventeen eligible studies reported the significant impacts of interventions on wasting/weight-for-height z-score. Among these six studies, two interventions targeting pregnant women did not demonstrate significant impacts on wasting. Mekonnen et al. conducted a 12-month nutritional education programme for mothers/caregivers with children aged less than a year that resulted in significant improvements in the weight-for length z-score of the children (MD = 1·06; 95 % CI (0·40, 1·70), P-value = 0·002)(Reference Mekonnen, Tadesse and Dawed48). Bidira et al. showed improvements in wasting using nutritional education for mothers/caregivers with infants aged < 6 months of age (DID = -0·07; P-value < 0·010)(Reference Bidira, Tamiru and Belachew49), and Teshome et al. demonstrated the effects of BCC on wasting for mothers/caregivers with children aged < 35 months of age (P-value = 0·001)(Reference Teshome, Whiting and Green41). Complementary feeding programmes (such as group nutrition sessions, cooking demonstrations, and supervision and training of healthcare workers) targeting mothers/caregivers with infants aged 6–12 months showed significant effects on the weight-for-height z-score of children (MD = 0·48; 95 % CI (0·16, 0·81), P-value < 0·001)(Reference Kang, Kim and Sinamo45) (Table 2).
The implementation of a 6-month BCC intervention (including nutrition education, health belief model and recipe demonstrations) for mothers/caregivers with children aged 6–18 months resulted in a significant improvement in the weight-for-height z-score of children (P-value < 0·05)(Reference Mulualem, Henry and Berhanu51). Providing fish oil supplementation for children (β = 0·022; 95 % CI (0·004, 0·039), P-value = 0·012), as well as for both mothers and children (β = 0·018; 95 % CI (0·001, 0·034), P-value = 0·041), improved the weight-for-length z-score of infants aged 6–12 months(Reference Argaw, Wondafrash and Bouckaert54). Except for two studies that did not report the level of statistical significance, the remaining studies did not show the significant impacts of interventions on wasting (Table 2).
Impacts of interventions on underweight/weight-for-age Z-score
Out of fourteen studies, six reported significant impacts of interventions on underweight. Among these six studies, two studies implemented to target pregnant women did not show significant impacts. Bidira et al. implemented a nutritional education programme for mothers/caregivers with infants aged < 6 months of age, which resulted in a reduction in underweight (DID = -0·08, P-value < 0·001)(Reference Bidira, Tamiru and Belachew49), while Ayalew et al. observed impacts on underweight through BCC interventions for the same age group (relative risk = 0·55; 95 % CI (0·35, 0·87), P-value = 0·011)(Reference Ayalew and Belachew39). Two studies that implemented BCC interventions indicated the significant impacts of interventions on underweight(Reference Teshome, Whiting and Green41,Reference Mulualem, Henry and Berhanu51) . Kang et al. used a complementary feeding programme for mothers/caregivers with infants aged 6–12 months that reduced underweight (MD = 0·34; 95 % CI (0·06, 0·61), P-value <0·001)(Reference Kang, Kim and Sinamo45). Providing quality protein maize for households with children under 5 years of age also improved the weight-for-age z-score of children (P-value = 0·013)(Reference Akalu, Taffesse and Gunaratna46). However, except for two studies that did not report the level of statistical significance, the remaining studies did not show the impacts of interventions on underweight (Table 2).
Discussion
Our study revealed that some BCC interventions, food vouchers, micronutrient supplementations and quality protein maize were effective in improving stunting. Similarly, BCC and fish oil supplementation also showed potential in reducing wasting, while BCC and the provision of quality protein maize reduced underweight. Furthermore, WaSH interventions that targeted pregnant mothers and children under 2 years of age were found to significantly reduce childhood stunting. Our searches did not locate any interventional study on the nutritional status of under 5 years of age children for Afar, Somali, Harari, Gambella and Benishangu regions, or Addis Ababa and Dire Dawa city administrations.
Recent global evidence demonstrated the importance of a systems-based approach to improve children’s diets and accelerate the reduction of malnutrition(Reference D’Aloisio55,Reference Scott, Delport and Hainsworth56) . Our findings showed that almost two-thirds of published interventions in Ethiopia revealed no impact on childhood stunting and wasting, and more than half had no impact on underweight. Two explanations for this lack of impact are the short duration of intervention implementation, which may have limited their effectiveness, and the failure of most studies to recognise the importance of a systems-based approach. Crucially, integrating food (fruits, vegetables and animal foods), health (maternal and childcare), environment (clean water and adequate sanitation) and social protection (food vouchers) can all improve the nutritional status of children(Reference D’Aloisio55). An appropriate systems-based approach requires a shared vision, joint planning and monitoring across stakeholders. Future child nutrition interventions in Ethiopia should adopt an integrated approach that combines the positive effects of interdependent systems such as BCC interventions, food programmes that boost protein and micronutrients, quality maternal and childcare interventions, clean water and adequate sanitation, and social protection systems (e.g. monetary support and income schemes).
Nutrition social and BCC strategies (such as interpersonal communication, social change approaches, community mobilisation, mass media and policy advocacy) encourage healthy behaviours while also reducing barriers to change(57). Accordingly, interventional studies in Ethiopia have shown that BCC is a great measure to reduce childhood malnutrition(Reference Ahmed, Agho and Page32). Nevertheless, nutritional outcomes are also influenced by multiple factors, including household food security, individual behaviours, healthcare providers, school teachers, farmers, agricultural agents, religious and community leaders, private enterprises, and policymakers(57,Reference Fox and Obregón58) . We, therefore, recommend that future BCC interventions in Ethiopia that aim to improve childhood malnutrition should consider locally specific factors that cover the households, communities and schools. Particular emphasis should also be given to implementing household food security interventions as a pivotal component of these strategies.
Animal-source foods (including meats, fish, poultry, organ meats and eggs) are rich sources of high-quality proteins and essential micronutrients(Reference Murphy and Allen59–Reference Melse-Boonstra61). Inadequate consumption of animal-source foods is substantially contributing to malnutrition and the suboptimal development of children in LMIC (including Ethiopia)(Reference Adesogan, Havelaar and McKune62). In these countries, animal-source foods are not affordable to many low- and middle-income households and a significant number of families depend on starchy monotonous diets (e.g. grains, tubers and roots)(Reference Adesogan63–Reference Zaharia, Ghosh and Shrestha65). Findings from eligible studies have shown the impacts of providing micronutrients and quality protein maize to households on stunting and wasting(Reference Akalu, Taffesse and Gunaratna46,Reference Samuel, Brouwer and Feskens50) . While micronutrient supplementation and plant proteins are important, they are not sustainable solutions for animal-source foods(Reference Young, Neufeld, Hendrix and Caballero66). Ensuring access and affordability to animal-source foods (e.g. eggs, chicken and other livestock production) using national and subnational policy interventions can sustainably improve the consumption of animal-source foods for Ethiopian children.
Repeated childhood infections due to a lack of access to clean water and adequate sanitation contribute to the burden of malnutrition in LMIC, including Ethiopia(Reference Deshpande, Miller-Petrie and Lindstedt67). In our review, Fenn et al. showed the impacts of WaSH interventions in the form of protected water supply and sanitation education on childhood stunting in Ethiopia(Reference Fenn, Bulti and Nduna53). However, recently published RCT documented a lack of impact of WaSH interventions on the nutritional status of children(Reference Humphrey, Mbuya and Ntozini68–Reference Null, Stewart and Pickering70). This lack of impact of WaSH interventions questioned the validity of the old hypothesis that WaSH has an independent effect on the linear growth of children(Reference Maleta and Manary71). Integrating WaSH interventions with food, health and social protection systems can successfully improve nutritional outcomes for children.
Reducing inequalities across regions and implementing effective strategies for malnutrition is essential to ensure that no child is left behind in Ethiopia. To date, no intervention studies on stunting, wasting and underweight have been published for Afar, Somali, Gambella and Benishangu regions, or Addis Ababa and Dire Dawa city administrations. Indeed, the government of Ethiopia has endorsed several global and national strategies to end malnutrition for the entire country; unfortunately, Addis Ababa, Dire Dawa and other city administrations have even higher rates of urbanisation driving the poor nutritional status of children in urban slums(Reference Benti, Terefe and Callo-Concha72,Reference Gelu, Edris and Derso73) . The observed inequalities warrant the need to expand successful interventions and strategies to reduce subnational inequalities for malnutrition.
The systematic review had some limitations. First, there was a wide heterogeneity of individual studies in intervention design and outcome measures, which ruled out the possibility of a meta-analysis. Second, nearly half of eligible studies were rated as high risk of bias (RCT and cluster RCT) or a serious risk of bias (quasi-experimental studies). The main reasons for not achieving a positive rating were the lack of allocation concealment methods, a higher number of concern decisions due to lack of information and the lack of RCT. To enhance the evidence base and ensure the reliability of future systematic reviews in this field, it is essential to conduct RCT with larger sample sizes and longer intervention durations.
Last, there is a chance of publication bias as studies showing negative results are less likely to be submitted for journal publication. Nevertheless, we conducted hand literature searches to locate grey literatures. Despite the above limitations, the study is the first systematic review of experimental and quasi-experimental studies to improve the nutritional status of children in Ethiopia. Our findings provide the best evidence for previously implemented interventions in Ethiopia.
Conclusion
Our findings showed that almost two-thirds of published interventions had no impact on childhood stunting and wasting, and more than half had no impact on underweight. Future childhood nutritional interventions in Ethiopia should adopt an integrated approach that combines the positive effects of interdependent systems such as BCC interventions, food supplemental programmes (e.g. boosting protein and micronutrients), health interventions (e.g. strengthening maternal and childcare), clean water and adequate sanitation and social protection systems (e.g. monetary support and income schemes).
Acknowledgements
The authors are grateful to Charles Sturt University and Western Sydney University digital libraries for access to electronic searching databases.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The authors declare that they have no competing interests.
Authorship
K.Y.A. conceptualised the study idea, performed the literature searching, selected the paper of interests, performed data extraction and critically revised the manuscript. H.D. and A.A. critically revised the manuscript for intellectual content. T.K.T. performed the risk of bias assessment and critically revised the manuscript. F.A.O. contributed to the study selection, performed data extraction and critically revised the manuscript. A.G.R. contributed to the conception of the research idea and and critically revised the manuscript. All authors read and approved the final manuscript.
Ethics of human subject participation
Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980023002410









