The adverse association between low income and psychological distress has been established across time and around the world(Reference Sareen, Afifi and McMillan1,Reference Wickham, Whitehead and Taylor-Robinson2) . In longitudinal studies, individuals who experience decreases in income or transition into poverty report subsequent declines in mental health(Reference Sareen, Afifi and McMillan1,Reference Wickham, Whitehead and Taylor-Robinson2) . Recent evidence further indicates that living in poverty predicts psychological distress more strongly among people with disabilities than those without disabilities(Reference Williams and Do3). This finding is particularly concerning given that people with disabilities are over twice as likely as those without disabilities to report incomes below the poverty threshold(Reference Williams and Do3). Moreover, research suggests that even small increases in levels of psychological distress can have serious consequences for health, predicting increased odds of engaging in health-harming behaviours, developing preventable chronic diseases and dying prematurely(Reference McLachlan and Gale4–Reference Bell, Russ and Kivimaki6). Despite these risks, factors that might explain the stronger adverse association between poverty and poor mental health for people with disabilities have yet to be explored.
Most studies investigating potential mediators in the relationship between poverty and mental health among the general population have focussed on psychosocial factors. Results from extant research are inconclusive, with some studies finding that financial hardship contributes to poorer mental health by reducing individuals’ sense of agency, control and self-esteem, and others finding no evidence that psychological factors play a role in the relationship between income and mental health(Reference Frankham, Richardson and Maguire7). Fewer studies have examined whether material hardship explains the association between poverty and psychological distress. These studies typically rely upon a composite index of material deprivation that combines multiple measures (e.g. food insecurity, transportation, housing, telephone and Internet). Findings indicate that material hardships explain much, but not all, of the association between poverty and poor mental health among pregnant women(Reference Katz, Crean and Cerulli8), mothers(Reference Heflin and Iceland9) and low-income service workers(Reference McCarthy, Carter and Jansson10). For instance, one study found that increases in material hardships explained 43 % of this adverse association(Reference McCarthy, Carter and Jansson10). Another demonstrated that material deprivation explained 32 % of the observed decline in mental health among individuals who developed a disability, compared to only 5 % for behavioural and 1 % for psychosocial factors(Reference Aitken, Simpson and Gurrin11).
The role of one specific type of material deprivation, food insecurity, has seldom been examined in isolation. Only two studies, to the best of our knowledge, have investigated the potential mediating role of food insecurity in the adverse association between poverty and poor mental health. In a cross-sectional study of Singaporean adults(Reference Nagpaul, Sidhu and Chen12), food insecurity fully explained the detrimental relationship between poverty and psychological distress. In another study, a poverty-alleviation intervention was delivered to ultra-poor women in Bangladesh(Reference Jalal, Frongillo and Warren13). The intervention reduced distress among participants, with improved food security explaining 48 % of this decrease(Reference Jalal, Frongillo and Warren13).
The lack of research investigating the role of food insecurity in the adverse association between poverty and psychological distress is striking given that food insecurity is more strongly associated with a family’s income-to-poverty ratio (IPR) than crime, housing issues, neighbourhood problems, access to consumer durables, healthcare and difficulty meeting basic needs, and is correlated with even very small and short spells of poverty(Reference Iceland and Bauman14). Moreover, a large body of cross-sectional and longitudinal studies, systematic reviews and meta-analyses demonstrates that as food security decreases, scores on self-rated mental health, depression and psychological distress scales worsen(Reference Bruening, Dinour and Chavez15–Reference Jones18).
Those living in food insecure households often consume lower-quality, less-balanced and nutrient-poor diets, all of which have been shown to directly contribute to the development of depression, anxiety and distress(Reference Popa and Ladea19). In the classic Minnesota Starvation Experiment(Reference Keys, Brozek and Henschel20), formerly healthy young men subjected to semi-starvation displayed symptoms of depression, irritability, anxiety and impaired cognition. As participants entered the rehabilitation phase of the experiment, decreases in depression scores correlated strongly with calories consumed, with those who received diets containing the most calories experiencing the most rapid improvements in depression(Reference Keys, Brozek and Henschel20). Mental health can also be compromised by the stress and worry that accompanies food insecurity. Food insecure individuals report feeling stress, shame, guilt, social alienation and powerlessness due to their difficulty obtaining adequate food in a socially acceptable manner(Reference Myers16).
Theory further suggests that the influence of financial and material deprivation on health outcomes may be magnified for people with disabilities. The World Health Organisation’s(21) International Classification of Functioning, Disability and Health (ICF) proposes that an individual’s social and environmental circumstances, including income and food security, dynamically interact with their underlying health conditions, leading to greater disability and worse health outcomes than would be expected based on their underlying conditions alone. This framework is consistent with extant research demonstrating that low income more strongly predicts poor mental health among people with disabilities than among those without disabilities(Reference Williams and Do3). It is possible that food insecurity also plays a disproportionate role in explaining the adverse association between low income and poor mental health for people with disabilities.
For instance, even within the same level of income, individuals with disabilities are more likely to experience food insecurity(Reference Huang, Guo and Kim22–Reference Brucker and Nord27), report higher competing expenses and experience greater unmet needs for other goods and services than those without disabilities(Reference Mitra, Palmer and Kim28). Many people with disabilities require expensive, high-quality and speciality dietary items to effectively manage their medical conditions(Reference Schwartz, Buliung and Wilson25), the absence of which may aggravate their health and exacerbate stress and worry. While one study found that food insecurity predicted poor mental health similarly among those with and without disabilities(Reference Brucker26), no study, to the best of our knowledge, has investigated the extent to which food insecurity helps explain the burden of poverty on mental health or whether the magnitude of its mediating role differs by disability status.
To address this gap, we investigated whether food insecurity helps to explain the deleterious association between low income and psychological distress in the US population and whether its role differs by disability status. Consistent with the ICF(21), we hypothesised that food insecurity may explain more of the income-psychological distress gradient and play a stronger role in shaping patterns of poor mental health among people with disabilities than those without disabilities, as illustrated in Fig. 1.

Fig. 1 Illustration of the hypothesised relationships between disability status, income, food insecurity and psychological distress. The double-headed arrow between disability and income reflects the bidirectional relationship between disability and income. The unidirectional arrow intersecting the income–food insecurity pathway indicates the potential moderating influence of disability on the income–food insecurity–psychological distress pathway
Methods
Data
We analysed data from the Integrated Public Use Microdata Series version of the 2011–2017 National Health Interview Survey (NHIS)(Reference Blewett, Rivera Drew and King29), the latest years in which both food security measures and the full set of disability questions outlined in the Department of Health and Human Services (2011) data collection standard are available. The NHIS is an annual, cross-sectional survey that collects nationally representative data on the health and socio-demographic characteristics of non-institutionalised US civilians. We restricted all analyses to adults aged 18 and older for whom there were no missing values on our variables of interest. Our analytical sample included 102 598 respondents, of whom 20 952 had a disability.
Measures
Outcome
Our outcome of interest was non-specific psychological distress, measured by the Kessler 6 (K6) Scale. The K6 (Cronbach’s α = 0·89) is a screening tool used in large, nationally representative surveys to assess the prevalence and frequency of six psychological symptoms indicative, but not diagnostic, of non-specific psychological distress(Reference Kessler, Barker and Colpe30,Reference Payton31) . The K6 Scale is composed of questions about the frequency of psychological distress symptoms experienced over the past 30 d, including feeling: (1) sad; (2) nervous; (3) restless and fidgety; (4) hopeless; (5) worthless and (6) that daily activities require too much effort. Responses to each item were assigned a frequency-based score, ranging from 0 for “none” to 4 for “all of the time.” For each respondent, scores from all K6 items were summed, resulting in a continuous K6 score ranging from 0 (i.e. no psychological distress) to 24 (i.e. highest possible level of psychological distress).
Studies of psychological distress often exclude participants with mental illness (e.g. clinically diagnosed schizophrenia, anxiety, depression) in an effort to minimise confounding(Reference Payton31,Reference Sanchez, Rosenthal and Tansey32) . However, psychological distress and mental illness, although related, are separate constructs(Reference Payton31). Accordingly, social and material disadvantages predicting greater levels of psychological distress among people with preexisting mental health conditions(Reference Payton31,Reference Sanchez, Rosenthal and Tansey32) . In light of this evidence, we did not exclude respondents with mental illness from the current study.
Key variables of interest
Our three key variables of interest were income, disability status and food security. We used IPR to measure household income, calculated as the ratio of total combined family income to the poverty threshold as defined by the US Census Bureau. IPR was categorised according to four levels: <1, 1 to <2, 2 to <4, or ≥4. We specified disability status as a binary indicator based on answering yes to at least one of six NHIS questions described in the Department of Health and Human Services(33) data collection standard. These questions are intended to assess whether respondents are deaf or have ‘serious difficulty hearing,’ blind or have ‘serious difficulty seeing’ with glasses, have ‘serious difficulty concentrating, remembering, or making decisions,’ ‘serious difficulty walking or climbing stairs,’ difficulty with dressing or bathing and difficulties running errands or attending medical appointments alone(33).
Food security was assessed using the US Adult Food Security Survey Module(34), a 10-item, three-stage screening tool designed to measure household food security over the past 30 d. Points were assigned according to the respondent’s answers to a series of questions regarding the severity of food shortage, if any. In the first stage, respondents are asked whether three statements were ‘often’, ‘sometimes’, or ‘never’ true because their households did not have enough money for food: (1) they worried they would run out of food; (2) food they bought did not last and (3) they could not eat balanced meals. In stage two, those who indicated any food scarcity (i.e. ‘sometimes’ or ‘often’ true) were asked if, because they did not have enough money for food, they: (1) ate less than they felt they should; (2) did not eat when hungry; (3) lost weight and (4) ate smaller meals or skipped meals and, if so, the number of days they did so. In the final and third stage, respondents were asked if there was ever a full day during which they did not eat because there was not enough money for food and, if so, the number of days this occurred. The scores from each stage of the module were summed, resulting in a total raw score ranging from 0 to 10. Given that even very low levels of food insecurity increase the risk of poor health outcomes, Gundersen and colleagues(Reference Gundersen and Ziliak35) suggest that relying on binary indicators of food security may underestimate the impact of food insecurity on mental health and mask differences in the strength of that relationship by characteristics such as disability status. Thus, consistent with USDA’s recommendations for classification(34), food security was categorised into three levels: food secure (raw score: 0–1), low food security (raw score: 2–5) and very low food security (raw score: 6–10).
Covariates
Analyses adjusted for educational attainment (less than high school, high school or general educational development, some college, bachelor’s degree or more), employment status (employed, unemployed, not in labour force), age (continuous in years), sex (male, female), race/ethnicity (non-Hispanic white, non-Hispanic black, non-Hispanic other, Hispanic), nativity (U.S born, foreign-born), marital status (married, never married, divorced or separated, widowed), health insurance (at least private insurance, public insurance only, uninsured), region of residence (Northeast, Midwest, South, West) and survey year (dummies).
Statistical analyses
Analyses were conducted in Stata se/15.1, and all adjusted for complex survey design. First, we conducted descriptive analyses to summarise demographic characteristics of the full study sample, respondents with disabilities and respondents without disabilities. Next, we estimated the association between income and psychological distress by conducting a series of linear regression models. The A series base models investigated the association between income and psychological distress for the full study sample, first without any interactions and then fully interacted by disability status (i.e. all predictor variables interacted with disability). The A series models adjusted for the entire list of covariates except food security. We then estimated the B series models, which assessed whether access to food helps explain observed associations by adding level of food security to the A series models. Post-estimation adjusted Wald tests were conducted to test whether food security explained a significant proportion of the association between income and psychological distress for each sample and whether the proportion explained differed by disability status.
Results
Sample characteristics
Weighted bivariate descriptive analyses (see Table 1) indicated that, in the general population, adults report an average psychological distress score of 2·56 points on the K6 Scale (sd = 2·62). Most (89·27 %) live in households that are food secure and have incomes at least two times greater than the federal poverty threshold (68·56 %). People with disabilities, on average, reported 2·5 times higher psychological distress levels (mean = 5·03 K6 units, sd = 4·11) than people without disabilities (mean = 2·04 K6 units, sd = 2·09). People with disabilities were also at a disproportionate socio-economic and material disadvantage and were more likely to be members of other marginalised groups. Compared to people without disabilities, those with disabilities were two times more likely to live in poverty (11·46 v. 22·43 %), two times more likely to report low food security (10·50 v. 5·10 %) and nearly three times more likely to report very low food security (11·86 v. 3·17 %). People with disabilities also tended to be less educated and were more likely to be unemployed or not in the labour force; older; female; non-Hispanic black; divorced, separated, or widowed; born in the USA; receiving only public health insurance; and residents of the South than those without disabilities. All observed bivariate differences in sample characteristics between adults with and without disabilities were statistically significant at the α = 0·01 level.
Table 1 Weighted characteristics of US adults included in a study of income, food security and psychological distress, by disability, National Health Interview Survey, 2011–2017*

GED, general educational development.
* T and χ2 tests indicated that all characteristics were statistically different between those with and without disabilities at the 5 % level.
Linear regression results
Results for the A and B series models are presented in Table 2. Model 1A explored the association between income and psychological distress among the general population. Models 2A and 3A reflect results from the model that was fully interacted with disability status. For clarity of presentation, we present coefficients from models stratified by disability, which are mathematically equivalent to the total effect of each coefficient in the fully interacted model (i.e. main coefficient added to the coefficient for the interaction term) for those without disabilities (Model 2A) and those with disabilities (Model 3A). Differences in the magnitude of associations by disability status reflect coefficients of the corresponding interaction terms.
Table 2 Linear regression results for psychological distress among US adults, National Health Interview Survey, 2011–2017†

IPR, income to poverty ratio; GED, general educational development; HS, high school; NILF, not in labour force; ref, reference category.
* Indicates P < 0·05.
† All models controlled for gender, age, race/ethnicity, nativity, marital status, insurance, region and survey year.
Consistent with extant evidence(Reference Williams and Do3), psychological distress increased as income decreased in a stepwise fashion, regardless of disability status. Compared to adults with incomes at least four times the poverty threshold, those in the general population with incomes 2 to <4, 1 to <2 and <1 times the poverty threshold scored 0·48 (95 % CI (0·41, 0·56)), 1·00 (95 % CI (0·90, 1·11)) and 1·45 (95 % CI (1·32, 1·58)) points higher on the K6 Scale, respectively. As observed in previously published research(Reference Williams and Do3), the coefficients for interaction terms between IPR and disability status indicated that the inverse association between income and psychological distress was stronger for those with disabilities than for those without disabilities at the α = 0·01 level. For instance, compared to those in the highest income category, individuals without disabilities living below the poverty threshold scored 0·81 (95 % CI (0·69, 0·93)) points higher on the K6 Scale. In comparison, individuals with disabilities living below the poverty threshold reported a difference in K6 score that was an additional 1·30 (95 % CI (0·93, 1·67)) points larger. Based on the results from Models 2A and 3A, predicted levels of psychological distress by IPR and disability status are presented in Fig. 2. Consistent with a more severe impact of financial hardship on mental health for those with disabilities, the disparity in psychological distress between people with and without disabilities widens as income decreases.

Fig. 2 Predicted psychological distress among US adults by income and disability status, National Health Interview Survey, 2011–2017. Predicted levels were calculated based on results from Models 2A and 3A, holding all covariate values at their sample means. Dashed lines indicate 95 % CI
To assess whether insufficient access to food helps explain the observed income-psychological distress relationship, food security was added in the B series models. A significant association between food insecurity and psychological distress and a reduction in the estimated income–psychological distress association were observed. Post-estimation adjusted Wald tests indicated that, regardless of disability status, food insecurity explained a statistically significant proportion of the detrimental relationship between low income and psychological distress. In the general population, accounting for food security reduced the income disparity between those living in poverty and those in the highest income category by 0·63 (95 % CI (0·59, 0·68)) points on the K6 Scale (or 44 %). Post-estimation adjusted Wald tests of interaction terms between IPR and disability status demonstrated that the proportion of the adverse association between income and psychological distress explained by food insecurity statistically differed by disability status. That is, accounting for food insecurity reduced the steepness of the income-psychological distress gradient significantly more for adults with disabilities than those without disabilities at the α = 0·01 level. For instance, among individuals with disabilities, accounting for food insecurity reduced the mental health disparity between those in poverty and those in the highest income category by 0·96 points (95 % CI (0·83, 1·10)) on the K6 Scale (or 46 %). In contrast, food insecurity only reduced the income disparity for those without disabilities by 0·34 points (95 % CI (0·31, 0·38)) (or 42 %). Consequently, the K6 poverty disparity between those with and without disabilities was reduced by a statistically significant proportion, 48 % or 0·62 points (95 % CI (0·49, 0·76)). Figure 3 presents predicted levels of psychological distress across income levels for people with and without disabilities based on the results from Models 2B and 3B. Compared to Fig. 2, Fig. 3 illustrates that after accounting for food insecurity, the steepness of the income-psychological distress gradient observed among people with disabilities more closely resembles the gradient for those without disabilities (i.e. the difference in the magnitude of the association between income and psychological distress for those with and without disabilities, after accounting for food insecurity, was reduced).
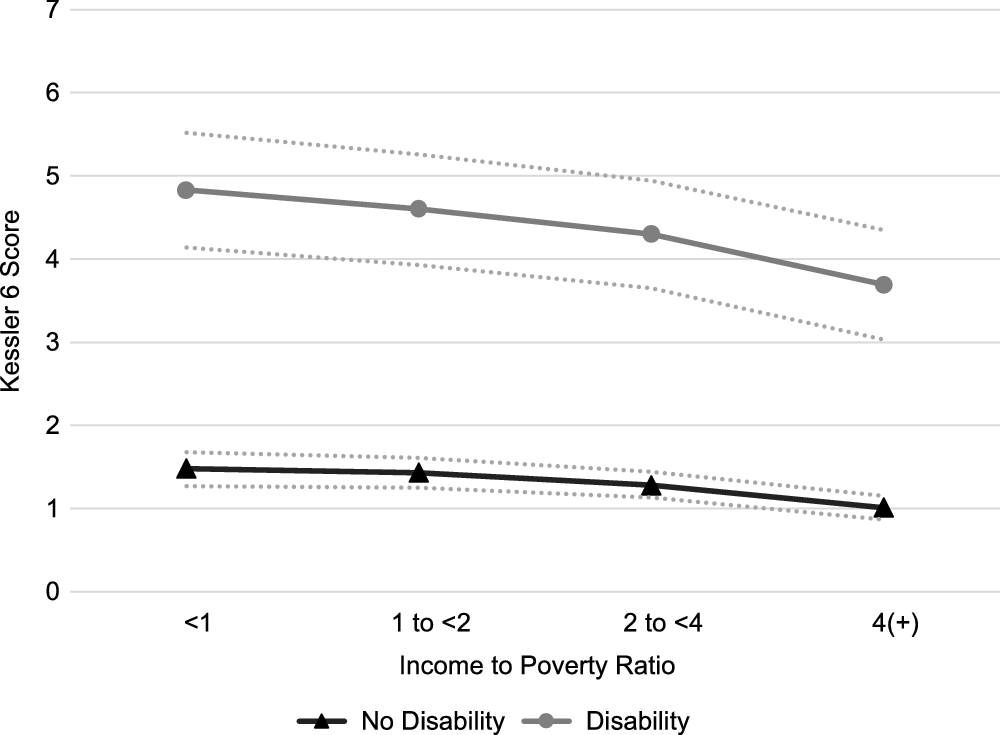
Fig. 3 Predicted psychological distress among US adults by income and disability status after controlling for food security, National Health Interview Survey, 2011–2017. Predicted levels were calculated based on results from Models 2B and 3B, holding all covariate values at their sample means. Dashed lines indicate 95 % CI
Independent of income, education and employment, the association between food security and psychological distress also followed a consistent, stepwise, inverse association (Models 1B, 2B and 3B). Compared to the food secure, those in the general population who experienced low and very low food security scored 1·88 (95 % CI (1·72, 2·04)) and 4·04 (95 % CI (3·82, 4·26)) points higher on the K6 Scale, respectively. Individuals with and without disabilities experiencing low food security scored 1·68 (95 % CI (1·34, 2·03)) and 1·49 (95 % CI (1·30, 1·66)) points higher on the K6 Scale than those who were food secure, respectively. The difference in the increase in K6 score between those with and without disabilities for low food security was not statistically significant. Very low food security, however, predicted psychological distress more strongly among people with disabilities than among those without disabilities. Compared to the food secure, individuals without disabilities experiencing very low food security scored 2·76 (95 % CI (2·51, 3·02)) points higher on the K6 Scale. Among individuals with disabilities, those reporting very low food security scored 4·11 (95 % CI (3·74, 4·49)) points higher than the food secure, a difference that was 1·35 (95 % CI (0·89, 1·81)) points larger than observed among those without disabilities.
Discussion
To the best of our knowledge, this study is the first to investigate whether food insecurity helps explain the deleterious association between low income and psychological distress and whether its role differs by disability status in a nationally representative sample. Consistent with extant evidence, we observed an inverse association between income and poor mental health for the general population as well as for subgroups with and without disabilities(Reference Sareen, Afifi and McMillan1–Reference Williams and Do3). Further, this adverse association was amplified for individuals with disabilities, echoing results of previous research(Reference Williams and Do3). That is, as income decreased, psychological distress increased more severely among people with disabilities than those without disabilities. Accounting for food insecurity reduced the compounded burden of poverty on mental health for people with disabilities by nearly half. These findings are consistent with the ICF framework(21), which posits that social and environmental circumstances, including poverty and food insecurity, interact with an individual’s underlying medical condition to exacerbate disability and worsen health outcomes.
Results suggest that food insecurity plays a more important role in shaping patterns of poor mental health among people with disabilities than among those without disabilities, predicting psychological distress more strongly and explaining more of the income–psychological distress gradient. Among adults with disabilities, accounting for food insecurity reduced the disparity in K6 score for those living in poverty compared to the highest income category by nearly one full point, compared with only a third of a point for those without disabilities. Independent of income, very low food insecurity was further associated with an approximately four-point increase in psychological distress scores on the K6 Scale for those with disabilities, compared to less than 3 points for those without disabilities. To put these estimates into perspective, one study found that an increase of as little as two points in K6 score predicted increased odds of dying at an early age(Reference Pratt5).
In addition to these findings, supplemental analyses conducted using consistent measures and model specifications (results available upon request) demonstrated that the magnitude of the difference in the adverse association between food insecurity and mental health by disability status was larger than what has been reported by characteristics such as age, gender and region(Reference Arenas, Thomas and Wang17,Reference Jones18,Reference Pourmotabbed, Moradi and Babaei36) . Food insecurity also explained a greater proportion of the difference in the magnitude of the income-mental health association by disability status than by these demographic characteristics. Our findings, however, differ somewhat from those of Brucker(Reference Brucker26). While results from both studies indicated that food insecurity increased the odds of reporting poor mental health, Brucker(Reference Brucker26) did not observe a difference in the strength of this relationship by disability status. Whereas Brucker’s(Reference Brucker26) study analysed one year of NHIS data and utilised binary indicators for both food insecurity and poor mental health, our study pooled seven years of NHIS data (i.e. a sample size that was nearly eight times larger) and used finer gradations of indicators (i.e. three levels of food security and a continuous measure of psychological distress), both of which may have enhanced our ability to detect differences in the magnitude of associations examined(Reference Pratt5,Reference Gundersen and Ziliak35) .
There are several reasons why food insecurity may explain more of the income–psychological distress gradient and be more predictive of psychological distress, net of income, among people with disabilities. First, even at the same level of income, people with disabilities are more likely to experience food insecurity than individuals without disabilities(Reference Huang, Guo and Kim22,Reference She and Livermore23) . To be food secure, people with work-related disabilities require an income at least 2·7 times higher than individuals without disabilities(Reference She and Livermore23). Those with disabilities may require higher-cost foods to manage their health conditions and spend more to access the same foods as those without disabilities. To manage their underlying health conditions, many individuals with disabilities must purchase higher-cost, higher-quality and specialty dietary items(Reference Schwartz, Buliung and Wilson25). Those with difficulty travelling to stores, shopping for groceries and preparing food may have to spend more to purchase already prepared foods or have them delivered to their homes(Reference Schwartz, Buliung and Wilson25).
Food insecure households also practice many cost-saving strategies that can directly harm health and exacerbate existing medical conditions, including skipping, delaying or taking less medication than prescribed; postponing or refusing needed medical care; failing to follow recommended diets for their health conditions or consuming lower-quality, higher-calorie foods(Reference Berkowitz, Seligman and Choudhry37,Reference Silverman, Krieger and Kiefer38) . Reference Berkowitz, Seligman and Choudhry Reference Berkowitz, Seligman and Choudhry Compared to individuals without disabilities, those with disabilities have more competing demands on their limited financial resources and greater unmet needs for basic necessities such as medications; medical equipment, services and supplies; housing and transportation(Reference Huang, Guo and Kim22,Reference Mitra, Palmer and Kim28) . One in three adults with chronic illness cannot afford their medications, food or both(Reference Berkowitz, Seligman and Choudhry37). Chronically ill adults experiencing very low food security have four times higher odds of underusing prescribed medications because of cost than those who are food secure(Reference Berkowitz, Seligman and Choudhry37). Hence, people with disabilities may be constantly faced with making distressing choices between quality and quantity of food or healthcare and medication(Reference Huang, Guo and Kim22,Reference Brucker26) .
Our findings are particularly concerning given that food insecurity seems to be more entrenched among those with disabilities. Although the prevalence of food insecurity decreased in the general population from 14·6 % in 2008 to 11·1 % in 2018, food insecurity among people with work-related disabilities remained constant at 33 %(Reference Coleman-Jensen24). Further, many safety net programmes designed to improve food security are insufficient to meet the needs of people with disabilities(Reference Schwartz, Buliung and Wilson25). Community gardening and free meal programmes have demonstrated little utility for improving food security among people with disabilities and are often inaccessible to participants with disabilities(Reference Schwartz, Buliung and Wilson25). Hot meal programmes and food pantries often fail to consider transportation and mobility barriers, requiring consumers to travel to the site, use the services within a limited window of time and, in some cases, transport goods back home without assistance(Reference Schwartz, Buliung and Wilson25).
Research demonstrates that even adult with disabilities who receive income assistance through Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) have disproportionately high odds of experiencing food insecurity(Reference Brucker and Nord27). Evidence suggests that monetary support provided by these programmes is insufficient to meet the basic material needs of many people with disabilities. Nearly 45 % of adults who receive SSI and 20 % who receive SSDI live in households with total incomes below the federal poverty threshold(Reference Bailey and Hemmeter39). Because these programmes, along with Medicaid and the Supplemental Nutrition Assistance Program, are means-tested and impose strict limits on assets, individuals with disabilities are additionally discouraged from building assets that could reduce the impact of short-term income losses and unexpected medical costs on food security(Reference Huang, Guo and Kim22). Huang and colleagues(Reference Huang, Guo and Kim22) found that, among people with disabilities, household assets such as a homeownership, savings and net worth are more protective against food insecurity than income. Thus, it is not surprising that, in addition to partially explaining the relationship between poverty and poor mental health, we found that very low food insecurity predicts psychological distress more strongly among adults with disabilities than those without disabilities independently of income.
Limitations
Our findings should be interpreted in light of the study’s limitations. A scoping review of extant literature suggests that people with disabilities can be trapped in complex, multidirectional cycles of poverty, food insecurity and disability(Reference Schwartz, Buliung and Wilson25). Because the NHIS is a cross-sectional survey, we were unable to draw inferences about the direction or causality of the relationships observed. Second, the NHIS sampling frame excludes people experiencing homelessness and those living in institutional settings. While institutionalised populations might be more likely to be food secure than those living in the community, they often have less control over the type, quality and quantity of food they consume(Reference Schwartz, Buliung and Wilson25). As a consequence, our results may not be generalisable to these subgroups. Third, people with chronic conditions and disabilities commonly underreport symptoms of poor mental health, scoring higher on social desirability bias measures than those without disabilities(Reference Nelson and Liebel40,Reference Stonerock, Smith and Hoffman41) . Finally, the K6 Scale only measures symptoms of psychological distress experienced in the last 30 d(Reference Kessler, Barker and Colpe30). As a result, it may capture emotional responses to short-term stressors in addition to symptoms of longer-term psychological distress(Reference Kessler, Barker and Colpe30).
Conclusions
Results suggest that socio-economic and material disadvantages, including poverty and food insecurity, may be stronger determinants of poor mental health among people with disabilities than those without disabilities. Consistent with extant evidence(Reference Williams and Do3), we observed a stronger detrimental association between poverty and psychological distress among people with disabilities than among those without disabilities. Food insecurity explained more of the income–psychological distress gradient among people with disabilities than those without disabilities and predicted psychological distress more strongly independent of income, education and employment status. These findings are particularly troubling given that people with disabilities, who are a large and growing population, are two times more likely to live in poverty and three times more likely to report very low food security than people without disabilities. Reducing food insecurity may help reduce long-entrenched mental health disparities experienced by people with disabilities.
Acknowledgements
Financial support: This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Authorship: M.R.W. developed the research question, conceptual framework and design of the study, conducted the analyses and drafted the manuscript. D.P.D. reviewed analyses, assisted with interpretation of results and edited the manuscript. Ethics of human subject participation: Because this study involved secondary analysis of the publicly available National Health Interview Survey dataset, ethical approval was not required.
Conflicts of interest:
There are no conflicts of interest.








