Bangladesh is experiencing ‘double burden’ malnutrition( Reference Shafique, Akhter and Stallkamp 1 ). Data show a steady increase in the prevalence of overweight and a steady decrease in underweight among Bangladeshi women of reproductive age( Reference Shafique, Akhter and Stallkamp 1 , Reference Khan and Talukder 2 ) and children( Reference Khan and Talukder 2 – Reference Das, Chisti and Malek 4 ). Compared with pre-1960s, mothers in a post-1985 cohort were 22 % less likely to be underweight and four times more likely to be overweight, indicating a secular trend( Reference Mohsena, Goto and Mascie-Taylor 5 ).
A rising secular trend in hypertension (HTN) and type 2 diabetes mellitus (T2DM) has also been observed in Bangladesh( Reference Saquib, Saquib and Ahmed 6 ). According to a recent national estimate, one in four adults had HTN and one in ten adults had T2DM( Reference Rahman, Gilmour and Akter 7 , Reference Akter, Rahman and Abe 8 ) Studies have identified older age, female sex, higher education and wealth, less physical activity and higher BMI as independent risk factors for both HTN and T2DM in Bangladesh( Reference Rahman, Gilmour and Akter 7 – Reference Tareque, Koshio and Tiedt 9 ). Among these, physical inactivity and overweight/obesity are important modifiable risk factors( Reference Rahman, Nakamura and Seino 10 , Reference Chen, McClintock and Segers 11 ).
Bangladesh is developing economically at a rapid pace and is aiming to become a middle-income country by 2021( Reference Bishwajit 12 ). Wealthier people are more likely to be overweight/obese and to engage in sedentary lifestyles and less physical labour. Therefore problems of overweight and obesity, especially among the urban dwellers, are likely to increase in future.
BMI, calculated by dividing weight in kilograms by the square of height in metres (kg/m2), is widely used in public health to identify high-risk individuals, reinforce health promotion and assess the effect of public health interventions. BMI cut-off points are a proxy for body fatness or fat accumulation in the body. However, BMI cannot distinguish between body fat and lean body mass, which are affected by body structure and muscularity. Lean muscle mass may also decrease with ageing. The relationship between BMI and body fat percentage depends on age, sex and ethnicity. Consequently universal BMI cut-off points may not be appropriate( Reference Deurenberg-Yap, Chew and Deurenberg 13 ).
There is increasing evidence that Asian populations differ in body fat percentage, body fat distribution and BMI-related CVD risks, and that they have higher percentage of body fat at a lower BMI than white or European populations( Reference Deurenberg, Deurenberg-Yap and Guricci 14 ). The WHO’s recommended BMI cut-off points for overweight (≥25·0 kg/m2) and obesity (≥30·0 kg/m2) are based on increased non-communicable disease risks among European populations( 15 ). However, compared with Europeans, increased T2DM and CVD risks have been observed for Asian populations at lower BMI (22·0–25·0 kg/m2)( Reference Razak, Anand and Shannon 16 , Reference Narksawat, Podang and Punyarathabundu 17 ). The WHO has acknowledged that countries may need to adopt different BMI cut-off points such as 23·0 kg/m2 or 27·5 kg/m2 for potential public health action, but has refrained from redefining population-specific cut-off points( 15 ).
Most studies from Bangladesh have analysed CVD risks associated with higher BMI/overnutrition based on the WHO guidelines. Among those very few studies that explored risks for moderately overweight individuals, Chen et al. reported an increased risk of all-cause deaths (hazard ratio=1·35; 95 % CI 1·05, 1·73) and CVD deaths (hazard ratio=1·34; 95 % CI 0·94, 1·90) for individuals with BMI≥21·5 kg/m2, compared with BMI of 19·3–21·4 kg/m2, but found no association between BMI and cancer deaths( Reference Chen, Ge and Parvez 18 ). An increased risk for heart disease (age- and sex-adjusted hazard ratio=1·79; 95 % CI 1·08, 2·97) with BMI greater than 22·0 kg/m2 has also been reported( Reference Chen, McClintock and Segers 11 ). To our knowledge, no study in Bangladesh has tried to quantify HTN and T2DM risk associated with a moderately increased BMI (23·0–24·9 kg/m2), i.e. among those who are ‘at risk of overweight’. The purpose of the current study was to assess the increased prevalence of HTN and T2DM with excess weight, especially among those with moderately increased BMI (23·0–24·9 kg/m2), from cross-sectional data of a nationally representative sample of adults, compared with a reference BMI group of 18·5–22·9 kg/m2.
Methods
Data source: Bangladesh Demographic and Health Survey 2011
The most recently available Bangladesh Demographic and Health Survey (6th BDHS) data set was used for the present study. Participants were identified using multistage sampling with a geographically clustered, probability-based sample of households. Data collection was carried out between July and December, 2011. The detailed methodology of the data collection procedure has been described previously( 19 ).
The study population was a nationally representative sample of women and men aged 35 years or older, who provided consent for blood pressure and fasting plasma glucose measurements. Participation was 86 % among men (n 4524) and 92 % among women (n 4311). The final sample size with complete information on blood pressure and fasting plasma glucose was 7434 (3685 males, 3749 females) and 7286 (3606 males, 3680 female), respectively. All participants provided informed verbal consent.
Variables
Dependent variables
HTN and T2DM prevalence were the main outcomes of interest.
For analytical purposes, the blood pressure data were made dichotomous (persons with/without HTN). Blood pressure was measured using a LifeSource® UA-767 Plus Blood Pressure Monitor. Three measurements were taken by trained health workers, with the participant in the seated position, at approximately 10 min intervals. The average of the second and third measurements was used to record blood pressure. Persons with systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg or current use of antihypertensive medication (self-reported) were considered as having HTN.
Similarly, blood glucose data were dichotomised (persons with/without T2DM). Whole blood was obtained from the middle or ring finger from adults after an overnight fast. The HemoCue 201+ blood glucose analyser was used. Each fasting whole-blood glucose value was multiplied by 1·11 to adjust to the corresponding fasting plasma glucose value. Persons with fasting plasma glucose ≥7·0 mmol/l or taking antidiabetes medication at the time of the survey (self-reported) were considered as having T2DM.
Independent variables
Demographic variables
Demographic variables considered were age at the time of interview (35–55 years, 56 years or older) and sex (male, female).
Socio-economic variables
Place of residence (urban or rural), respondent’s wealth index based on principal component analysis (poorest/poorer, middle, richer/richest) and highest educational attainment (no education/pre-school, 1–5 year/primary, secondary or higher) were the socio-economic variables. The wealth quintile index was constructed using information on housing materials, sources of drinking-water, sanitation facilities, use of soap and water for hand washing, availability of electricity, housing amenities, possession of household durable goods, and home and land ownership( 19 ).
BMI
Height (in centimetres) and weight (in kilograms) of the respondents were measured using a standard protocol. Height was measured with an adjustable measuring board, which can provide accurate measurements to the nearest 0·1 cm. Weight was measured using an electronic scale with a precision of 0·1 kg. BMI (kg/m2) was calculated as the ratio of weight to height squared.
BMI (kg/m2) data were categorised based on cut-offs for Asian populations into seven BMI categories: <16·0 (severe underweight), 16·0–16·9 (moderate underweight), 17·0–18·4 (mild underweight), 18·5–22·9 (normal weight), 23·0–24·9 (moderately overweight), 25·0–29·9 (overweight) and ≥30·0 (obese)( 15 ).
Statistical analysis
We initially provided descriptive information of the distributions of categorical variables by different BMI cut-off points. For descriptive analysis we stratified the population according to seven BMI categories. Mean blood pressure and blood glucose (systolic blood pressure, diastolic blood pressure, fasting plasma glucose) by BMI category were calculated, again separately for males and females.
HTN and T2DM prevalence by BMI category were calculated for selected categorical variables, separately for males and females. The χ 2 test or t test was used to explore the differences in proportions and means of dependent variables (HTN, T2DM) for selected independent variables as required. Trends in HTN and T2DM prevalence (by increasing BMI cut-offs) were assessed. The analysis compared HTN and T2DM prevalence for one BMI category with the previous highest BMI category, using the lincom command. A P value of 0·05 or lower was considered as statistically significant.
Using modified Poisson regression models with robust error variance, we calculated the prevalence ratio (PR) and 95 % confidence interval for HTN or T2DM for different BMI categories, considering BMI=18·5–22·9 kg/m2 as the reference, separately for males and females. For this purpose, we considered four different models as follows. (i) Model I (unadjusted): HTN/T2DM and BMI; (ii) model II: model I adjusted for age; (iii) model III: model I additionally adjusted for wealth and education; (iv) model IV: combination of models II and III additionally adjusted for residence.
Statistical analyses were performed using the statistical software package Stata version 12 for Windows.
Results
According to the modified BMI cut-offs for Asian populations, about half of the population had BMI within the normal range (BMI=18·5–22·9 kg/m2), 2 % were obese (BMI≥30·0 kg/m2) and about 6 % were severely underweight (BMI<16·0 kg/m2). About one in ten or 12 % (both males and females) were moderately overweight (BMI=23·0–24·9 kg/m2) and about a quarter (25·1 %, 1872/7433) of the adults had BMI above 23·0 kg/m2 (see online supplementary material, Supplemental Table 1).
According to the modified cut-off, overweight or obesity (BMI≥23·0 kg/m2) prevalence was significantly higher among women (30 % v. male 20 %; P<0·001) and was significantly associated with young age (28 % v. older age 18 %), urban areas (43 % v. rural 20 %), higher wealth (richer 41 % v. poorer 10 %) and higher education (43 % v. primary 23 % and no education 17 %; all P<0·001). About one-third of the population was underweight (BMI<18·5 kg/m2). No sex difference was observed in underweight prevalence (see online supplementary material, Supplemental Table 1).
Overall, 19·3 % of males and 31·6 % of females had HTN. T2DM prevalence was 10·7 and 11·3 % among males and females, respectively. Figure 1 presents HTN and T2DM prevalence by the seven BMI categories, for male and females separately. Further analyses by different factors are presented in the online supplementary material, Supplemental Tables 2 (HTN) and 3 (T2DM). In general, HTN prevalence of moderately overweight persons (BMI=23·0–24·9 kg/m2) was significantly higher than that of normal-weight persons (BMI=18·5–22·9 kg/m2), among both males and females. HTN prevalence of those moderately overweight (BMI=23·0–24·9 kg/m2) was statistically similar to that of overweight persons (BMI=25·0–29·9 kg/m2). About half of obese adults, both male and female, had HTN. HTN prevalence was significantly higher among obese people than among those overweight, even though obesity prevalence was very low in the nationally representative sample (males 0·7 % and females 2 %).
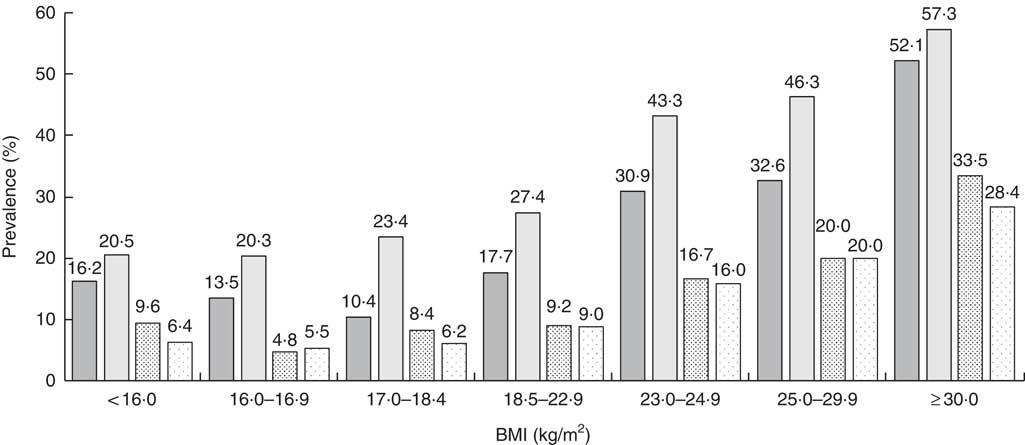
Fig. 1 Hypertension (HTN) and type 2 diabetes mellitus (T2DM) prevalence (weighted estimates) by BMI category and sex (![]() , HTN, males;
, HTN, males; ![]() , HTN, females;
, HTN, females; ![]() , T2DM, males;
, T2DM, males; ![]() , T2DM, females) among Bangladeshi adults (n 7433) aged ≥35 years, Bangladesh Demographic and Health Survey, 2011
, T2DM, females) among Bangladeshi adults (n 7433) aged ≥35 years, Bangladesh Demographic and Health Survey, 2011
T2DM prevalence was similar (9 %) among normal-weight males and females (BMI=18·5–22·9 kg/m2). Moderately overweight males and females (BMI=23·0–24·9 kg/m2) had significantly higher frequency of T2DM than those with normal BMI. Like HTN, moderately overweight (BMI=23·0–24·9 kg/m2) and overweight (BMI=25·0–29·9 kg/m2) individuals had similar T2DM prevalence. Although obese persons (BMI≥30·0 kg/m2) had much higher T2DM prevalence than those who were overweight, the difference was not statistically significant probably due to the small number of obese persons.
Table 1 presents sex-specific PR for HTN based on various models, separately for males and females. Unadjusted results (model I) showed significantly higher HTN prevalence for overnourished adults (BMI≥23·0 kg/m2), both males and females, compared with normal-weight adults (BMI=18·5–22·9 kg/m2). There was a trend for prevalence of HTN to increase from moderate-overweight BMI across higher BMI categories. In general, underweight was protective against HTN.
Table 1 Modified Poisson regression models showing prevalence ratios (PR) and 95 % confidence intervals for hypertension (weighted estimates) by BMI category and sex among Bangladeshi adults (n 7433) aged ≥35 years, Bangladesh Demographic and Health Survey, 2011
Ref., reference category.
Model I, unadjusted; model II, model I adjusted for age; model III, model I additionally adjusted for wealth and education; model IV, combination of models II and III additionally adjusted for residence.
*P≤0·05, **P≤0·01, ***P≤0·001.
The multivariable analysis showed that higher BMI (23·0–24·9, 25·0–29·9, ≥30·0 kg/m2), older age (56 years or more) and upper wealth quintiles (richer/richest) were associated with higher HTN prevalence for both men and women. Urban living (PR=1·14; 95 % CI 0·99, 1·30) and education above primary (PR=1·22; 95 % CI 1·02, 1·44) were associated with higher HTN prevalence for men, but not for women. HTN prevalence was significantly lower among educated women compared with no education. The final model showed that underweight (BMI=17·0–18·4, 16·0–16·9, <16·0 kg/m2) was protective against risk of HTN, but the effect was not statistically significant for severely undernourished (<16·0 kg/m2) males.
Table 2 shows that, similar to HTN, overweight men and women (BMI 23·0–24·9, 25·0–29·9, ≥30·0 kg/m2), in the older age group (56 years or more) and in the upper wealth quintiles (richer/richest) were more likely to develop T2DM. However, no difference was observed between urban and rural areas, whereas above primary education was associated with significantly higher T2DM prevalence for both men and women. In the final model, the protective effect of underweight (BMI 17·0–18·4, 16·0–16·9, <16·0 kg/m2) for T2DM was not statistically significant, except in males with BMI=16·0–16·9 kg/m2.
Table 2 Modified Poisson regression models showing prevalence ratios (PR) and 95 % confidence intervals for type 2 diabetes mellitus (weighted estimates) by BMI category and sex among Bangladeshi adults (n 7433) aged ≥35 years, Bangladesh Demographic and Health Survey, 2011

Ref., reference category.
Model I, unadjusted; model II, model I adjusted for age; model III, model I additionally adjusted for wealth and education; model IV, combination of models II and III additionally adjusted for residence.
*P≤0·05, **P≤0·01, ***P≤0·001.
Discussion
To our knowledge, the present paper is the first one from Bangladesh that reports an association between moderately increased BMI (23·0–24·9 kg/m2) and increased HTN/T2DM prevalence, based on information from a nationally representative sample of adults. Our analysis showed that moderately overweight individuals (BMI=23·0–24·9 kg/m2) had similar HTN and T2DM PR as those of WHO-defined overweight persons (BMI=25·0–29·9 kg/m2), across different factors. It should be noted that about 12 % of Bangladeshi adults, both male and female, were moderately overweight. Apart from BMI, we found that increased age was the strongest predictor of increased prevalence of HTN (adjusted PR: males 2·14, females 1·89) and T2DM (adjusted PR: males 1·74, females 1·66) for both sexes.
We found about one in four (25 %) Bangladeshi adults in this nationally representative sample had BMI≥23·0 kg/m2 and about one-third was undernourished (BMI<18·5 kg/m2). A recent study reported underweight (BMI<18·5 kg/m2), overweight (BMI=23·0–24·9 kg/m2) and obesity (BMI≥25·0 kg/m2) prevalence as 14, 18 and 26 %, respectively, in rural Bangladeshi adults, with no significant sex difference( Reference Siddiquee, Bhowmik and Da Vale Moreira 20 ). Another study in a rural area in Bangladesh found about 33 % of the adults had BMI≥23·0 kg/m2 and an undernutrition prevalence of 21 %, indicating a transition in lifestyle even among the rural population of Bangladesh( Reference Fatema, Zwar and Zeba 21 ).
We found one-third of the females were overweight (BMI≥23·0 kg/m2), significantly more than males (20 %). One publication reported in 2011 that 17 % of Bangladeshi women of reproductive age were overweight using a BMI cut-off of 25·0 kg/m2 and that the increasing trend of overnutrition was similar in urban and rural areas( Reference Khan and Talukder 2 ). Higher BMI among females may have been due to parity, menopausal stage, use of oral contraceptive pills, physical inactivity or high level of central adiposity.
Our findings support the recommendation that calls for setting the optimum BMI for Asian populations to 18·5–23·0 kg/m2 ( Reference Choo 22 ). A report from Bangladesh on detection of T2DM also recommended a BMI cut-off of 21·2 and 21·8 kg/m2, for males and females, respectively( Reference Bhowmik, Munir and Ahmed 23 ). Our findings suggested that HTN prevalence increased among males from the BMI range 18·5–22·9 kg/m2. For females the corresponding BMI range was little higher, 23·0–24·9 kg/m2. Our findings are similar to a previous report that found a lower threshold for CHD risk among males compared with females( Reference Flint, Rexrode and Hu 24 ). We did not observe any sex difference in BMI threshold for T2DM prevalence, which also agrees with previous findings( Reference Boffetta, McLerran and Chen 25 ).
Studies quantifying the relationship between BMI and CHD are rare in Bangladesh. A study in a tertiary-level hospital in Bangladesh found that, compared with the lowest quartile BMI (<23·15 kg/m2), the adjusted OR for CHD was about three times higher among adults in the second BMI quartile (23·16–24·60 kg/m2) and five to nine times higher for men and women in the highest BMI quartile (26·33–30·90 kg/m2), respectively( Reference Khan, Harvey and Leistikow 26 ). A study from the USA showed that, compared with BMI=18·5–22·9 kg/m2, males with a moderately higher BMI (23·0–24·9 kg/m2) had an adjusted relative risk for CHD of 1·22 (95 % 1·04, 1·43) and females had a non-significant relative risk of 1·10( Reference Flint, Rexrode and Hu 24 ). The relative risk of CHD for the obese category (BMI≥30·0 kg/m2) was 1·81 for males and 2·16 for females. Although these two studies differ in ethnicity and design, the findings support that excess risk of CHD is associated with moderately high BMI.
Bangladesh is one of the few developing countries in the world to achieve Millennium Development Goals 5 and 4: considerable reduction in maternal and child mortality( Reference Chowdhury, Bhuiya and Chowdhury 27 ). However, the growing burden of non-communicable diseases, the increased number of older people and the lack of health-system preparedness for management of chronic diseases will be major public health challenges( Reference Streatfield and Karar 28 ). Bangladeshi adults are particularly vulnerable to CVD at younger ages, compared with other countries. Studies have shown that the mean age of experiencing a first acute myocardial infarction for Bangladeshi adults is 51·9 (sd 11·0) years, which is the lowest in South Asia, and much lower than the global mean (58·1 (sd 12·2) years)( Reference Joshi, Islam and Pais 29 ). Approximately 40 % of stroke deaths in Bangladesh occurred in persons below 60 years, indicating non-communicable disease risk prevention programmes must target younger adults( Reference Mateen, Carone and Alam 30 ).
BMI is a WHO-prescribed indicator of nutritional status measurement that is used internationally and is important for comparison across different countries. The main purpose of a BMI cut-off point is to identify people with a high risk of having an adverse health outcome. It should therefore depend on population based-data of ‘increased risk’. The present study proposes using lower BMI cut-off points to identify high-risk individuals for screening, health promotion and monitoring of clinical and public health interventions in Bangladesh and similar settings. However, we suggest that WHO-recommended categories should also be used, especially for reporting purposes, to facilitate international comparisons( 15 ).
Several methodological issues need to be kept in mind while interpreting the observed associations. First of all, the study did not collect information on waist-to-hip ratio, which could be useful in avoiding the potential confounding by different body proportions. Some studies found waist circumference and waist-to-hip ratio to be better markers of obesity, some did not, while some argued that both BMI and waist circumference strongly predict future CHD risks( Reference Flint, Rexrode and Hu 24 ). Bhowmik et al. found waist-to-hip ratio, waist circumference and waist-to-height ratio as better predictors for cardiometabolic risk factors in Bangladesh( Reference Bhowmik, Munir and Diep 31 ). However, Khan et al. recommended using both BMI and waist circumference for assessing CHD risks, rather than a single obesity indicator, in both clinical and community settings( Reference Khan, Harvey and Leistikow 26 ).
Second, the current study did not collect information on co-morbidities. Therefore weight loss (very low BMI) resulting from existing illness may distort the relationship. However, while exploring associations between low BMI and increased mortality in a cohort, Pierce et al. did not find any role of possible confounding by co-morbidity( Reference Pierce, Kalra and Argos 32 ).
Third, the BDHS 2011 did not collect information on tobacco smoking habits at the individual level (only collected information on second-hand smoke at household level). Therefore, we did not include a smoking variable in the regression model, which could potentially influence our findings. It should be noted that even though Bangladeshi men were more likely to smoke tobacco compared with women (55 % v. females 1 %), smokeless tobacco use was high among women (34 % v. males 29 %) especially in poor, rural areas( 33 ).
Conclusions
Policy-level guidelines should be adapted to advocate lower BMI targets (18·5–23·0 kg/m2) by public health managers and health-care professionals. Physicians and public health workers need to be trained on proper counselling and management to promote lifestyle change programmes including leisure-time physical activity.
Acknowledgements
Acknowledgements: The authors thank MEASURE DHS Data Archive, ICF International for providing access to the BDHS 2011 data. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: The authors declare no conflict of interest. Authorship: M.R. formulated the research question, designed the study, and carried out data analysis, interpretation and writing of the article. G.W. and A.A.M. supervised data analysis and participated in manuscript writing. All authors reviewed the final draft. Ethics of human subject participation: Ethical permission was obtained when the Demographic and Health Surveys were carried out. All data in the present study were anonymous and no additional ethical permission was required.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980016003566






