Coronavirus Disease 2019 has originated in Wuhan, China, spread all over the world between December 2019 and early 2020, and significantly threatened human health and life(Reference Jakovljevic, Bjedov and Jaksic1,Reference Qiu, Shen and Zhao2) . The WHO defined the new coronavirus as COVID-19 on 11 February 2020 and declared the situation pandemic on 11 March 2020(3,4) . Since the first case of COVID-19 of 11 March 2020, in Turkey, the total number of patients is 281 509, the rate of pneumonia seen in patients is 7·6 % and the total number of patients recovered is 252·152, while the total number of deaths is 6730(5).
COVID-19 is a respiratory disease caused by the new coronavirus SARS-CoV-2, which has been declared pandemic(3). The virus can be transmitted through the droplets spread from the infected individuals by coughing and sneezing, touching the contaminated surfaces and objects, and touching the mouth, nose or eyes with infected hands(6). Its rapid spread, lack of treatment and lethal course make the effect of the virus important(Reference Aslan, Yuvacı and Köse7). The most important way to prevent the disease is not to be exposed to the virus(8).
There are some measures recommended during the pandemic period and implemented in our country to decrease the speed of the spread. Although the effects of the disease on children are weak, by taking into consideration the possibility of infection of adults by children, effective measures have been taken such as suspending schools, closing universities and dormitories, suspending meetings and events, starting working remotely, and declaring a short-term curfew in major cities for the individuals over the age of 65 years and below 18 years(9).
In addition to the COVID-19 outbreak, incorrect information about the outbreak(Reference Shimizu10), news on TV and social media(Reference Gao, Zheng and Jia11,Reference Goyal, Chauhan and Chhikara12) , travel restrictions and quarantines negatively affect people’s lives(Reference Nguyen, Nguyen and Do13). The pandemic period causes various psychological problems in individuals (such as panic, anxiety and depression)(Reference Jakovljevic, Bjedov and Jaksic1,Reference Qiu, Shen and Zhao2,Reference Wang, Wang and Yang14,Reference Roy, Tripathya and Kar15) , disrupted sleep patterns(Reference Bao, Sun and Meng16,Reference Altena, Baglioni and Espie17) and physical immobilisation(Reference Chen, Mao and Nassis18,Reference Ceravolo, De Sire and Andrenelli19) . The boredom and stress cause an excessive intake of energy by consuming large amounts of fat, carbohydrates (sugary foods) and protein. These unhealthy nutritional behaviours increase the frequency of obesity and chronic diseases such as diabetes and heart disease, which increase COVID-19 complications(Reference Moynihan, Van Tilburg and Igou20–Reference Butler and Barrientos23).
This epidemic is an extraordinary situation; it is very important to keep the immune system strong in terms of preventing infections, and protecting and maintaining health under extraordinary conditions(Reference Chowdhury, Hossain and Kashem24). The most effective methods include healthy and balanced nutrition, adequate physical activity and regular sleep(25,Reference Khaled and Benajiba26) .
Scientific researches in Turkey is often COVID-19 studies to assess its impact on the emotions of individuals in the pandemic period(Reference Özdin and Özdin27–Reference Seçer and Ulaş29). No published scientific research has been found on the physical activity and nutritional status of individuals.
In this study, the aim was to evaluate emotional (depression) and behavioural (nutritional behaviours, physical activity status and sleep patterns) of Turkish adult individuals during the COVID-19 pandemic period.
Methods
Participants
The population of the research consisted of adults in Turkey. In the research, a sample selection method was not used. The individuals, who were between the ages of 18–65 years and agreed to participate voluntarily, were included in the research. Totally, 1120 individuals participated in the research.
Study protocol
The research was carried out electronically by taking into account the current situation experienced due to the COVID-19 pandemic. The informed consent of the participants was obtained electronically before the questionnaire. The participants filled out a questionnaire (developed using Google Forms) that contained descriptive characteristics (age, gender, education, occupation, chronic disease status and marital status), nutritional behaviours (number of meals, food and supplement preferences, and appetite), sleep patterns (no change, I sleep more and I sleep less), physical activity status, anthropometric measurements (body weight and height), COVID-19-related level of knowledge and the questions of the Center for Epidemiological Studies Depression Scale (CES-D Scale) through e-mail or social media (WhatsApp).
The declarations of the participants were taken as a basis for body weight and height measurement values.
COVID-19 knowledge level was evaluated based on six basic questions addressed to the participants: (1) it is/can be transmitted by inhalation of droplets caused by infected/diseased persons through sneezing, coughing and speaking; (2) it is/can be transmitted by touching something that the infected/diseased person touches; (3) the incubation period of the virus does not exceed 14 d; (4) it is/can also be transmitted by contact with an asymptomatic (no signs of infection) person; (5) the disease can be treated with targeted drug studies; and (6) malaria drugs, beverages containing tonic water, drugs containing quinine are not protective against the disease. While each correct answer was evaluated as 1 point, the wrong answers were not scored. Regarding the COVID-19 disease, the participants with a score of ≥ 5 were evaluated as ‘Quite understand’, = 4 as ‘General understand’ and ≤ 3 as ‘Do not understand’(Reference Huang and Zhao30).
CES-D Scale is a four-point Likert-type scale (3 = agree, 2 = partially agree, 1 = disagree and 0 = no idea) consisting of 20 items in which depression symptoms are evaluated. The score that can be obtained from the scale varies between 0 and 60. Higher scores indicate more severe symptoms of depression. In the assessment, 0–9 points showed ‘Normal level’, 10–15 points showed ‘Mild depression’, 16–24 points showed ‘Moderate depression’ and 25–60 points showed ‘Severe depression’(Reference Tatar and Saltukoglu31–Reference Moon, Huh and Song33).
Statistical analysis
Descriptive analyses (percentage, mean and sd) were conducted to describe the demographic characteristic, the time of following developments related to coronavirus on television and the internet during the day, COVID-19-related knowledge, body weight, height, BMI, sleep, and physical activity status, nutritional status, and habits. The prevalence of gender, age, education, profession, marriage and chronic disease stratified by depression were reported, and the χ2 was used to compare the differences between groups. Multivariate logistic regression models were performed to explore potential influence factors (gender, age, education, profession, marriage and chronic disease) for depressive symptoms. Adjusted OR (AOR) and 95 % CI were obtained from logistic regression models. All data were analysed using Statistical Package for Social Sciences (SPSS) version 22.0. P-values of less than 0·05 were considered statistically significant.
Results
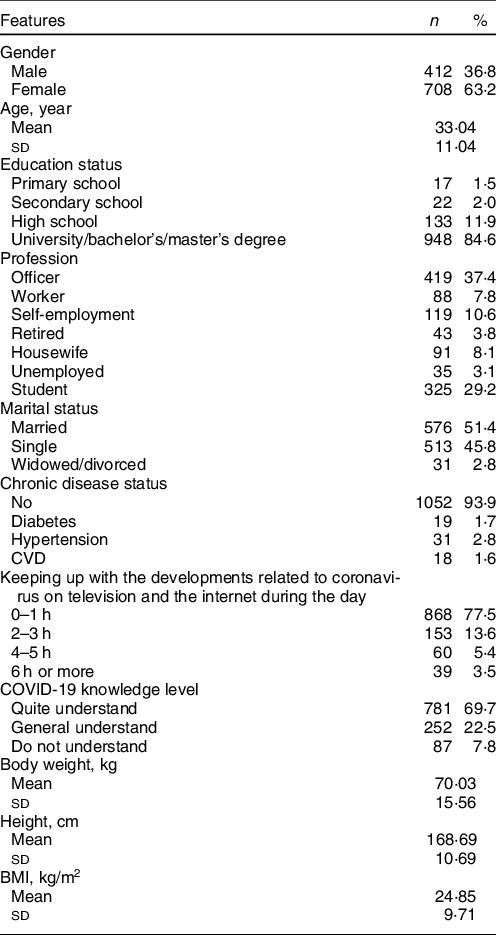
A total of 1120 individuals, 412 (36·8 %) male and 708 (63·2 %) females, participated in the study. The mean age was determined as 33·04 ± 11·04. Among those who participated in the research, 84·6 % of individuals were university/bachelor’s/master’s degree graduates. As for profession, 37·4 % were teachers, 29·2 % were students and 10·6 % were self-employed. There was no chronic disease in 93·9 % of the individuals. The time of following developments related to coronavirus on television and the internet during the day was 0–1 h in 77·5 % of the individuals. In terms of the knowledge level of COVID-19, it was determined that 69·7 % of the individuals ‘quite understood’ the COVID-19 pandemic. The mean BMI of the individuals was calculated as 24·85 ± 9·71 kg/m2 (Table 1).
Table 1 Descriptive features of individuals (n 1120)
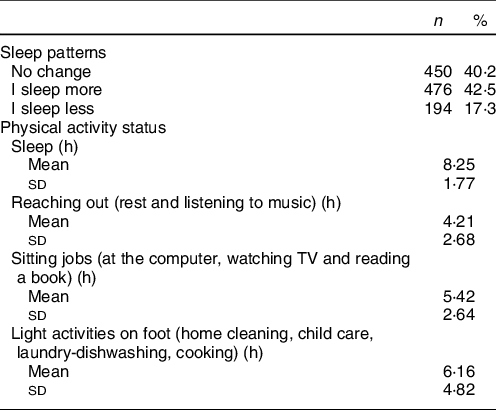
The information regarding the sleep and physical activity status of the individuals are shown in Table 2. And 42·5 % of the individuals stated that they slept more during the pandemic period and 40·2 % stated that there was no change in their sleep patterns. Daily physical activity durations were determined as 8·25 ± 1·77 h for sleep, 4·21 ± 2·68 h for lying down, 5·42 ± 2·64 h for sitting and 6·16 ± 4·82 h for standing activities.
Table 2 Sleep and physical activity status of individuals (n 1120)
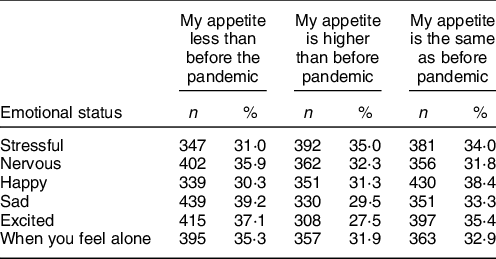
The psychological status experienced by the individuals at different times during the pandemic period when compared to the same psychological status before the pandemic is given in Table 3.
Table 3 Individuals’ appetite according to different emotional status (n 1120)
The information regarding the individuals’ nutritional status and habits are shown in Table 4. The mean number of meals was 2·77 ± 1·04. In this period, while the body weight of 48·6 % of individuals did not change, it was found that body weight of 38·4 % of the participants increased. The most consumed foods during the pandemic period were determined as tea and coffee by 66·6 %, pastries by 56·4 % (e.g. pies, cakes and cookies) and desserts by 49·6 %. Due to the belief that they will strengthen their immune systems, the individuals mostly consumed fruits and vegetables (74·0 %), probiotics (e.g. yogurt, kefir) (55·0 %) and foods containing n-3 (36·2 %). The commonly used supplements were vitamin C (28·1 %), vitamin D (24·2 %), probiotics (18·2 %) and multivitamin-minerals (15·4 %). The consumption of supplements, such as Zn and n-3, was equal (11·1 % for both).
Table 4 Nutritional status and habits of individuals (n 1120)
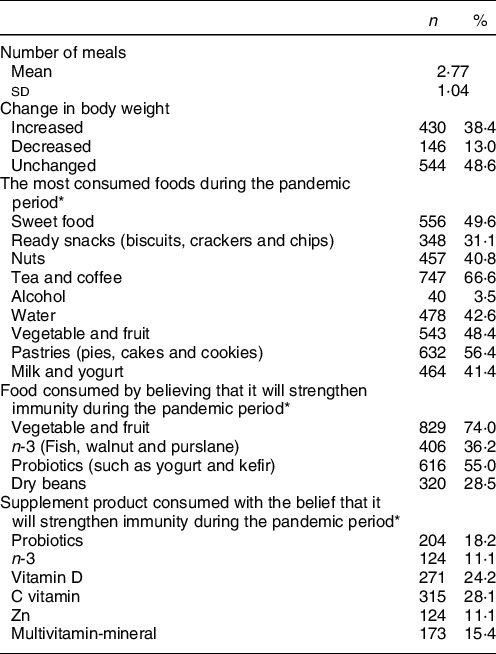
* Evaluation was made on more than one answer.
The relationship between the individuals’ gender, age, education status, profession, marital status, chronic disease status and depression status is shown in Table 5. And 13·3 % of individuals showed normal, 29·1 % mild, 34·2 % moderate and 23·4 % severe depression symptoms. The mean score of the CES-D Scale was determined as 19·02 ± 9·69. A significant relationship was found between gender, age and educational status, marital status and depression levels of the individuals, respectively (χ2 = 35·292, χ2 = 103·46, χ2 = 24·524 and χ2 = 86·208, P < 0·05).
Table 5 The relationship between individuals’ gender, age, education status, profession, marital status, chronic disease status and depression level (n 1120)
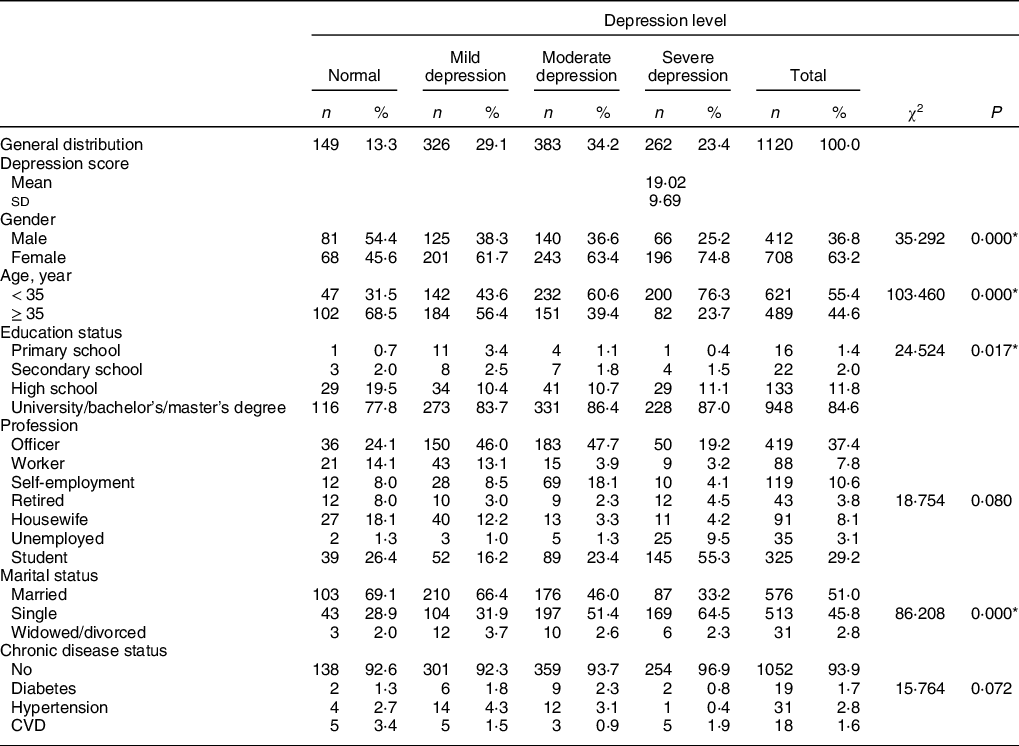
* Pearson ki-kare test (P < 0·05).
Table 6 Multinominal logistic regression analysis results (n 1120)
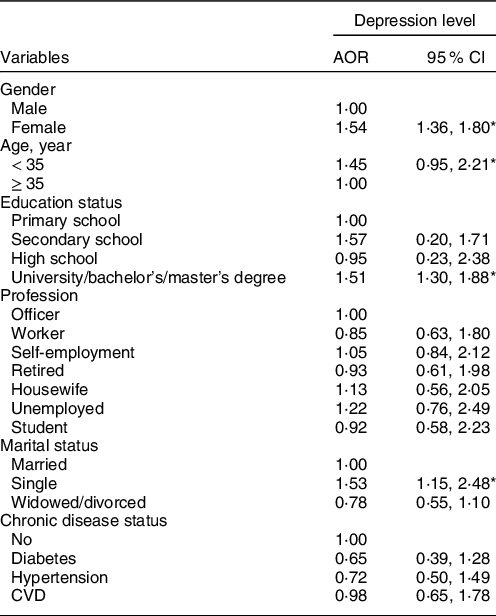
AOR, adjusted OR.
* P < 0·05.
According to the results of the multinominal logistic regression analysis, the female participants compared to the male participants (AOR = 1·54, 95 % CI: 1·36, 1·80), those under 35 years of age compared to the participants above 35 years of age (AOR = 1·45, 95 % CI: 0·95, 2·21), the participants with a university/bachelor’s/master’s degree as educational status (AOR = 1·51, 95 % CI: 1·30, 1·80) and single individuals (AOR = 1·53, 95 % CI: 1·15, 2·48) were associated with a higher risk of depression.
Discussion
With the COVID-19 pandemic, the concern for the spread of the virus has necessitated infection control and safety measures. The implementation of ‘stay at home’ that has been initiated to restrict social life is a basic safety step that can limit infections(Reference Chen, Mao and Nassis18). Such a difference in social life causes some changes in individuals’ psychological status, physical activity levels and nutritional behaviours.
A total of 1120 individuals, 412 (36·8 %) male and 708 (63·2 %) female with a mean age of 33·04 ± 11·04, participated in this research that was conducted to determine the possible changes during the pandemic period. Of the patients, 84·6 % had a university/bachelor’s/master’s degree. When asked about following the developments regarding coronavirus on television and the internet during the day, 77·5 % of the individuals responded as 0–1 h, 13·6 % as 2–3 h, 5·4 % as 4–5 h and 3·5 % as 6 h and above. As a result of the answers given to the questions asked about COVID-19 knowledge levels, it was determined that 69·7 % of the participants understood the pandemic quite well, 22·5 % generally understood and 7·8 % did not understand. Huanga and Zhao (2020) determined that 78·8 % (5702) of 7236 participants were quite understood, 15·7 % (1136) generally understood % 5·5 (398) did not understand(Reference Huang and Zhao30).
It is stated that the psychological status or characteristics of individuals affect their eating behaviours(Reference Moon, Huh and Song33). Increased time spent at home, pandemic news listened and watched, increased anxiety, increased desire to consume food (especially carbohydrate foods) due to mood, and decreased physical activity can cause unwanted increases in body weight. Exercising routinely at home is important to increase the physical activity level of the body and maintain a healthy life during the pandemic period(Reference Chen, Mao and Nassis18). And 42·5 % of individuals stated that they slept more during the pandemic period and 40·2 % stated that there was no change in their sleep patterns. The mean daily activity duration was found as 8·25 ± 1·77 h for sleep, 4·21 ± 2·68 h for works performed lying down, 5·42 ± 2·64 h for works performed sitting and 6·16 ± 4·82 h for light standing activities. As a result, it was determined that most of the day was spent sitting and lying down. The mean BMI was 24·85 ± 9·71 kg/m2, and it was determined that the body weight did not change in 48·6 % of the individuals during the pandemic period, while the body weight increased by 38·4 % of them.
In addition to physically affecting individuals, COVID-19 increased susceptibility to psychological problems such as depression, anxiety and panic disorder(Reference Huang and Zhao30,Reference Hiremath, Kowshik and Manjunath34) . In this study, the mean score received from the CES-D Scale was determined as 19·02 ± 9·69. Of the participants, 13·3 % show normal, 29·1 % mild, 34·2 % moderate and 23·4 % severe depression symptoms. A significant correlation was found between the individuals’ gender, age and educational status and their depression levels (χ2 = 35·292, χ2 = 103·46 and χ2 = 24·524, P < 0·05). According to the results of the multinominal logistic regression analysis, the female participants compared to the male participants (AOR = 1·54, 95 % CI: 1·36, 1·80), those under 35 years of age compared to the participants above 35 years of age (AOR = 1·45, 95 % CI: 0·95, 2·21) and the participants with university/bachelor’s/master’s degree as educational status (AOR = 1·51, 95 % CI: 1·30, 1·80) were associated with a higher risk of depression. In their study, Huanga and Zhao (2020) found similar results; they determined that the risk of depression was higher in individuals under the age of 35 years compared to the individuals above 35 years (AOR = 1·77, 95 % CI: 1·58, 2·07)(Reference Huang and Zhao30). The pandemic situation in China caused an increase in depression, anxiety and panic attacks in humans(8). Ahmed et al. (2020) found that 37·1 % of the participants (n 1074) had depression (mild 10·2 %, moderate 17·8 % and severe 9·1 %), and this rate was higher in the 21–30 years of age group(Reference Ahmed Md, Ahmed and Aibao35). In the study conducted on 7236 people, it was determined that there was a general anxiety state (35·1 %), depression (20·1 %) and a decrease in sleep quality (18·2 %) in the individuals during the pandemic period(Reference Huang and Zhao30). Anxiety and depression were more common among young people (< 35 years) and people who spent a lot of time on the internet and TV by reading and watching the news about COVID-19 (≥ 3 h/d)(Reference Huang and Zhao30). Since young people spend more time outside in their normal lives, having to stay at home caused more psychological problems.
The increase in the time spent at home changed the psychological status of the individuals but also caused them to receive more energy in their diets and consume more amounts of fat, carbohydrates and protein(Reference Moynihan, Van Tilburg and Igou20). In a study investigating the relationship between negative psychological status and high food intake, it was found that negative mood increased food intake more than positive mood(Reference Serin and Şanlıer36,Reference Evers, Adriaanse and de Ridder37) . When the individuals’ appetite status during the pandemic period were compared to their appetite status before the pandemic period, it was found that when they were more stressful (35·0 %), they ate more, when they felt less nervous (35·9 %), sad (39·2 %), excited (37·1 %) and lonely (35·3 %), they ate less, and when they were happy, their appetite status did not change (38·4 %).
Stress causes individuals to search for food that will provide relief quickly, and generally, the tendency towards sugary foods increases(Reference Muscogiuri, Barrea and Savastano38,Reference Özenoğlu39) . The most consumed foods during the pandemic period were determined as tea and coffee by 66·6 %, pastries by 56·4 % (pies, cakes and cookies) and desserts by 49·6 %. In terms of food craving, it is stated that there is a gender difference, and it is remarkably higher in females compared to males(Reference Muscogiuri, Barrea and Savastano38). The results of our study support this information.
There are insufficient data from clinical studies on the effects of nutrients on COVID-19 and the effects of nutritional supplements on COVID-19 prevention in healthy individuals. Although there is no definitive evidence due to the limitation of the studies, it is stated that balanced diets including probiotic-containing foods, immune-enhancing micronutrients such as polyphenols, vitamins A, C, E, D, B1, B6 and B12, and some minerals (especially Se, Zn, and Fe) may be effective in supporting immunity against COVID-19(Reference Olaimat, Aolymat and Al-Holy40–Reference Lanham-New, Webb and Cashman45). However, most guidelines emphasise the importance of fruits, vegetables, whole-grain foods, and vitamins A, C, D and Zn in protecting the immune system(Reference de Faria Coelho-Ravagnani, Corgosinho and Sanches46). While it has been stated that supplementation of vitamin C and D, Zn, and Se as supplements may be beneficial for people with respiratory tract viral infections or those at risk and those with nutritional deficiencies, scientific research is limited and the data are not clear(Reference Chandra47,Reference Chang, Pariantec and Su48) . Also, there are findings that n-3 PUFA can benefit both the physiological and psychological effects of COVID-19 and support immunity(Reference Chang, Pariantec and Su48,Reference Khoramipour, Basereh and Hekmatikar49) . In this study, believing that it will support the immune system, the most consumed foods are fruits and vegetables (74·0 %) and probiotics (55·0 %). The commonly used supplements were vitamin C (28·1 %), vitamin D (24·2 %), probiotics (18·2 %) and multivitamin-minerals (15·4 %). Those who preferred Zn and n-3 as supplements were equal (11·1 % for both). As a result of this study, it has been determined that individuals increase their consumption of vegetables and fruits and probiotics as food and vitamin C as a supplement with the belief of supporting immunity and protecting from COVID-19.
This study has some limitations. First, it is difficult to make causal inferences because the data and related analyses presented here were derived from a cross-sectional design. Second, the study was limited to the COVID-19 outbreak, and we used a web-based survey method to avoid possible infections. That causes the sampling of our study was voluntary and to be conducted online. Therefore, the possibility of selection bias should be considered. Finally, we were unable to assess an individual’s psychological state before the outbreak due to the sudden occurrence of the disaster.
As a result, it was determined that the pandemic period caused changes in the nutrition, physical activity and psychological status of the individuals participating in the research. It was determined that the individuals had different levels of depression risk, and the highest risk was observed in the females under 35 years of age and those with higher educational levels. It was determined that the consumption of carbohydrates increased, physical activity levels decreased and sleep patterns changed due to the increase in the time spent sitting and lying down.
Acknowledgements
Acknowledgements: The authors thank all the participants who participated in this research. Financial support: The authors received no financial support for the research, authorship and/or publication of this article. Conflicts of interest: The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article. Authorship: KYS and EG designed the study. KYS and EG collected the data. KYS analysed the data. EG and KYS prepared the manuscript. All authors, EG and KYS, approved the final version for submission. Ethics of human subject participation: For the research, approval was obtained from the COVID-19 Scientific Research Evaluation Commission under the body of the General Directorate of Health Services of the Ministry of Health of Turkey (2020–05–01T23_20_00) and Erzincan Binali Yıldırım University Human Researches Ethics Committee (decision dated 04/30/2020 and numbered 04–09).









