Despite considerable attempts have been performed to improve the nutrition and physical activity (PA) behaviours for an entire population, inadequate PA and obesity are generally more prevalent in the world(1,Reference Vandevijvere, Chow and Hall2) . According to the WHO report in 2015, approximately 23 % of adults aged 18 years and over (27 % women and 20 % men) did not have enough activity to achieve health benefits(Reference Aligol, Mohammadi and Mohamadbeigi3,Reference Dashti, Joseph and Esfehani4) . Obesity and overweight are an epidemic among the adult population, particularly in low- and middle-income countries. In 2016, the WHO demonstrated that approximately 1·9 billion (39 %) adults aged 18 years or older were obese and overweight(5). In Iran, a previous study in 2016 reported that 82 % of adults were either overweight (59·3 %) or obese (22·7 %)(5,Reference Djalalinia, Saeedi Moghaddam and Sheidaei6) . Therefore, the obesity rate is at an unacceptably high level in Iran and remains a health priority that needs further and maintained educational intervention.
In Iran, despite significant changes in the epidemiological profile of the population, changes in lifestyle, such as increasing irregular eating patterns and the consumption of sugary drinks, combined with insufficient PA, are the main factors in creating an ‘obesogenic’ society that powers unhealthy behaviour patterns(Reference Tabatabaei, Ardabili and Haghdoost7,Reference Khodaveisi, Omidi and Farokhi8) . Notably, in Iran, women were less active and more obese than men, and their healthy lifestyle pattern is the primary concern. It seems that Iranian women face unique challenges of religious and cultural barriers that affect healthy behaviours among the women’s population(Reference Tabatabaei, Ardabili and Haghdoost7,Reference Khodaveisi, Omidi and Farokhi8) . As documented by Kulie et al. in the USA(Reference Kulie, Slattengren and Redmer9) and Klumb and Lampert in Germany(Reference Klumb and Lampert10), the health education intervention for women allows the improvement of family behaviour patterns and leads their generation to have a better quality of life at any stage of development.
In recent decades, a variety of health promotion models (HPM) have been developed to enhance knowledge in the field of health promotion(Reference Basu and Goldhaber-Fiebert11). Pender’s HPM is a theoretical framework for evaluating the determinant that contributes to the promotion of healthy lifestyle behaviours and individuals’ commitment to healthy behaviours(Reference Pender12). This model is derived from the social cognitive theory with nine potential constructs. Individual characteristics and experience (prior behaviours) is the first scale of the HPM model to evaluate experience factors and innate factors that influence health promotion behaviours(Reference Srof and Velsor-Friedrich13). The behaviour-specific cognitions and effects are evaluated by the following constructs: perceived barriers, benefits, self-efficacy and activity-related affect. Most HPM research focuses on these constructs to perceive the positive consequences, barriers, beliefs and intentions to engage in a specific healthy behaviour(Reference Pender12,Reference Sakraida14) . Perceived self-efficacy is a central scale to evaluate personal capability and self-confidence in the development of healthy behaviours. The situational and interpersonal influences are the main constructs to examine the effect of social (family and friend support and interference) and environmental support (home and neighbourhood) on healthy behaviour(Reference Pender12,Reference Heydari and Khorashadizadeh15) . Commitment to a plan and behavioural outcomes are the target to examine the individuals’ belief, intention and health decision-making regarding behaviours end point (online supplementary material, supplemental Fig. 1). This model is implemented in numerous intervention programmes to modify health-promoting behaviours such as taking responsibility for health, nutrition, exercise, stress management and interpersonal support(Reference Srof and Velsor-Friedrich13,Reference Sakraida14) .
In this respect, this study was designed to evaluate PA and nutrition behaviours to better understand the determinants that influence health-promoting behaviours in women. The main objective of this study was to examine the effectiveness of Pender’s HPM-based intervention at improving nutrition behaviours and PA levels among women population enrolled in centre-based healthcare.
Methods
Participants
A randomised controlled field trial evaluated the efficacy of an educational intervention based on Pender’s HPM to improve PA and nutrition behaviours. In this study, women were eligible if they: (a) had a history of physical health, (b) were able to complete all relevant questionnaires, (c) were aged 18–50 years and (c) could speak and read their Persian language. Participants were excluded if they: (a) unwilling to participate and (b) had suffered mental disturbance, chronic disease (including diabetes and CHD), visual impairment and upper limb disability because participants with different types of disease and disability need different education programmes based on their physical and mental condition. Therefore, these populations were excluded from this study, and we only included women with health who met inclusion criteria.
Recent studies exploring the effectiveness of HPM’s intervention on health promotion behaviours targeting Iranian females showed that all intervention programmes had a small-to-moderate effect (e.g., = 38 %) on changing nutrition behaviours and PA level(Reference Khodaveisi, Omidi and Farokhi8,Reference Mohsenipoua, Majlessi and Shojaeizadeh16) . According to Cohen(Reference Cohen17), an experimental study with two groups would need 166 participants (eighty-three participants per group) assuming a small-to-moderate effect, an α of 0·05 and a power level of 0·80. In this study, healthcare centres were considered as units (clusters). Thus, we adjusted the sample size to estimate the clustering effect using the following equation:
where k is the anticipated cluster size (number of centres); D is the design effect; ρ is the intra-cluster correlation coefficient. In this study, the design effect for ten centres was 1 + 0·05 (10–1) = 1·2. Then, the sample size was estimated to be 83 × 1·2 = 100 for each group. We assumed a loss to follow-up rate of 20 %; our final target was to recruit at least 240 women (120 per group) from ten healthcare centres. All eligible participants filled out consent and completed study instruments.
Randomisation and recruitment
This study was conducted from April 2016 to February 2017, among the population of women living in Bojnourd, Iran. The intervention was conducted from August 2016 to October 2016 (see Fig. 1). Random allocation of healthcare centres was done before individual recruitment based on the consort checklist and flow diagram (Fig. 2). Ten healthcare centres were randomly selected from a list of centres. We randomly assigned these centres to the intervention (n 5) and control (n 5) groups. In each centre, the health secretary provided a list of women based on demographic data and health history, and all the women were assigned a number. Then, we used tables of random numbers to select each number of the women. Briefly, 365 women were randomly selected, of whom 125 have not met inclusion criteria, and thirty-eight participants refused to participate in follow-up because of the travelling (n 12), pregnancy (n 10) and employment problems (n 16). Finally, 202 women were included in the data analysis, and they completed the baseline (before intervention) and follow-up (post-intervention and 3 months after intervention) process (Fig. 2).

Fig. 1 Intervention timeline for the supporting healthy behaviours (physical activity and nutrition behaviours)

Fig. 2 Flow of participants through each stage of the programme
Intervention
The intervention was undertaken based on the Template for Intervention Description and Replication checklist (Table 1)(Reference Campbell, Piaggio and Elbourne18). The Pender’s HPM was used as a guide to develop the intervention because it is an appropriate social–ecological model for evaluating the determinants that promote healthy lifestyle behaviours and individuals’ commitment to healthy behaviours (online supplementary material, supplemental Fig. 1). This model recognises that multiple levels of influence affect behaviours and that health interventions are effective when they aim at changes in environmental domains, perceived self-efficacy, feeling, perceived benefits and barriers, and situational and interpersonal influences. The intervention group received a 3-month intervention that included nine 4-h training sessions (every 10 d) with a focus on the key constructs of the Pender’s HPM, which are detailed in Table 2. Likewise, consulting support was conducted by phone contact and internet messaging service to encourage women to be more active and to make better healthier diet and food selections. Educational intervention was conducted by a qualified exercise specialist, dietician (first session) and training health educator (sessions 2–9).
Table 1 Template for Intervention Description and Replication checklist of the study

Table 2 A Pander’s HPM-based educational intervention to improve physical activity and nutrition behaviours

We also used teach-back video, educational pamphlets, review action planning reminder card and focus group dissection to conduct intervention. All details related to dissemination/instruction’s intervention are described in Table 2. Subjects in the control group had not received any training during the intervention period, and they accessed a lifestyle-training package after 6 months when the health intervention and the 3 months of follow-up periods were finished.
Tools of assessment
The outcome of this study was to improve nutrition and PA behaviours based on changing women’s perceived self-efficacy, feeling, interpersonal and situational factors, perceived benefits and barriers, and commitment to a plan of action. The intervention based on Pender’s HPM was the independent variable, and the covariates studied were demographic characteristics including age, education, gender, income, employment status, marital status, height, weight, number of children and homeownership.
In this study, we used the nine constructs of Pender’s HPM as a framework to design the nutrition and PA questionnaires. To design the HPM items, we studied the literature of the HPM model(Reference Pender12) and interviewed thirty women to collect their opinions concerning nutrition and PA behaviours. Then, an expert panel of ten specialists in exercise, health education and diet edited all the questionnaires. They evaluated the necessity and relevance of all items to quantify the content validity index and content validity ratio. In this investigation, the average content validity ratio for the nutrition and PA behaviours questionnaires was 0·88 and 0·98, and content validity index for these questionnaires was 0·94 and 0·92, respectively.
We pilot tested the questionnaires with fifty women to evaluate all items based on their clarity, readability and simplicity(Reference Jenkinson and McGee19). The reliability coefficients (Cronbach’s α) of nutrition and PA behaviour questionnaires were 0·88 and 0·85, respectively, indicating a strong internal consistency of the questionnaire’s criterion(Reference Cronbach20). The correlation coefficient between all constructs was more than 0·65, which was considered satisfactory(Reference Landis and Koch21). Eligible participants in both groups completed instruments at baseline (before intervention), immediately after the intervention, and at 3-month follow-up. A demographic questionnaire was only completed at baseline.
Nutrition behaviours
Diet characteristics and experiences were evaluated using a semi-quantitative FFQ(Reference Mirmiran, Esfahani and Mehrabi22). On this scale, twenty short items on food habits (food consumption from main healthy food groups and low-nutrition/energy-dense foods, breakfast consumption) (online supplementary material, supplemental Table 2) with a five-point scale ranged from 0 (never) to 4 (always). Cronbach’s α of this construct was 0·85. Perceived self-efficacy was examined by eight items based on existing diet self-efficacy scale (e.g., how much degree of confidence do you have to make a better food selection even if you were tired?), which were ranged on a five-point scale from 0 (no confidence) to 4 (great confidence)(Reference Philippaerts, Matton and Wijndaele23,Reference Dehdari, Rahimi and Aryaeian24) .
We also used six items to assess activity-related affect (e.g., eating healthy food groups and breakfast is enjoyable to me) with a five-point scale ranging from 0 (completely disagree) to 4 (completely agree). Perceived barriers and benefit constructs contain six and eight items, respectively. Participants were asked to rate how much they agree with the perceived barriers (e.g., I could not perform regular healthy cooking if I don’t have enough money, or I don’t like eating breakfast early in the morning) and perceived benefits (e.g., a reason I eating healthy food groups, I feel they improve my physical appearance/or decrease my nervousness; I eating breakfast because it decreases the consumption of low-nutritional snacks)(Reference Dehdari, Rahimi and Aryaeian24,Reference Pender, Murdaugh and Parsons25) . Items in these constructs were ranged from 0 (completely disagree) to 4 (completely agree). We used two items to examine an individual’s commitment (e.g., do you have a regular schedule to use healthy food groups? or do you have a commitment to your regular schedule regarding healthy diets?). Items of this scale were rated from 0 (never) 4 (always)(Reference Pender, Murdaugh and Parsons25). We used ten items to measure interpersonal influences (e.g., how often does your husband/parents expect you to eat breakfast every day? or does your parents/husband expect you to do healthy cooking?). All questions were estimated on a five-point scale ranging from 0 (never) to 4 (always). A situational influence was measured using four items (e.g., I think it is easy for me to access healthy food groups in the neighbourhood) with a five-point Likert scale ranging from 0 (completely disagree) to 4 (completely agree). A behavioural outcome was measured using four items (e.g., how many times during the week do you eat five main healthy food groups?) with a five-point Likert scale ranging from 0 (never) to 4 (always)(Reference Dehdari, Rahimi and Aryaeian24).
Physical activity behaviours
PA is defined as ‘any bodily movement produced by skeletal muscles that requires more energy than resting, such as walking, cycling, or participating in sports – these have significant benefits for health’(Reference Caspersen, Powell and Christenson26). We used the long version of the self-administered International Physical Activity Questionnaire (IPAQ-L) to measure the individual PA characteristics and experiences over the week (MET-min/week) (see online supplementary material, supplemental Table 3)(27,Reference Kelishadi, Ardalan and Gheiratmand28) . This questionnaire includes twenty-four validated short questions on regular PA (frequency and duration of work, leisure, household/yard activities and commuting during the last 7 d) to evaluate the individual’s experiences that influence the level of PA. Cronbach’s α on this scale was 0·83. The scale of self-efficacy contained eight items (e.g., how much degree of confidence do you have to conduct PA even if you were tired?) with a five-point scale ranging from 0 (no confidence) to 4 (great confidence)(Reference Philippaerts, Matton and Wijndaele23). Activity-related affect was measured using five items (e.g., how much they agree with PA behaviour enjoyment or affect), which were ranged from 0 (completely disagree) to 4 (completely agree). Perceived barriers and benefit constructs contain twenty items. Participants were asked to rate how much they agreed with the perceived barriers (e.g., I might not do regular PA if I did not have enough time) and perceived benefits (e.g., one of the reasons I do regular PA is that I believe exercise improves my physical appearance/or decreases my nervousness). Items in these constructs ranged from 0 (completely disagree) to 4 (completely agree)(Reference Garcia, Broda and Frenn29,Reference Taymoori, Niknami and Berry30) . Commitment to a plan contains two items (e.g., do you have a regular schedule to perform PA?) with a two-point scale rating from 0 (no) to 1 (yes)(Reference Pender12). Interpersonal influences were measured using eight items (e.g., how often does your husband/parents change their schedule so they can exercise with you? or my parents/husband expect me to exercise) on a five-point Likert scale ranging from 0 (never) to 4 (always). We measured situational influences using six items (e.g., I think it is easy for me to access exercise facilities/in home/neighbourhood, I think that the cost of exercise is reasonable in my city). This construct was rated from 0 (completely disagree) to 4 (completely agree)(Reference Garcia, Broda and Frenn29,Reference Taymoori, Niknami and Berry30) . We used eight items to assess health outcomes (e.g., I consider regular schedule to perform PA during the week, I manage my time to engage in regular PA despite various conflicting situations), which rated from 0 (never) to 4 (always)(Reference Pender12).
Statistical analyses
In this study, descriptive analysis was done using mean score and standard deviation. The bivariate analyses (t-test, chi-square, ANOVA) were used to compare variables between the control and experimental groups. The bivariate correlations between the outcome variables and covariates were analysed using Pearson’s correlations. A repeated measure ANOVA was also used to determine differences in outcome variables from baseline to follow-up in control and intervention groups.
The random affects least squares regression model was used, with the main effects of study arm assignment (control v. intervention), time period (baseline v. follow-up) and their interaction included. This model decreases concerns regarding missing data because all errors are shaped within the design as a random effect. Likewise, this analytical model allows for the accounting of cluster effects between behaviour outcomes and HPM constructs that are nested within an intervention programme. We assumed health promotion intervention to be nested within modifying healthy behaviours via the Pender’s constructs. Regression analysis involved adjustment for baseline covariates that had a significant effect on outcomes because the main target in this study was only testing the effectiveness of the HPM model and their constructs on improving nutrition and PA behaviours. The estimated parameters for the determinants of healthy behaviours are accompanied by their 95 % CI. Significant differences were taken as P < 0·05, and R version 3.0.2 and Statistical Package for Social Sciences software (SPSS 16) were used to conduct multiple statistical analyses.
Results
At baseline, there were no significant differences (P > 0·05) in the demographic measures from control and intervention groups. The result showed that the mean (±sd) of age, weight and height for the eligible participants were 30·05 (±9·4), 61·3 (± 8·8) and 161·2 (±5·4), respectively. A majority of the eligible women were married (88 %), housekeepers (88·2 %), moderate-income families (65 %), high school diploma (34 %) or bachelor’s degree (26 %) with three or four children (Table 3). In this study, we observed that the women’s physical and nutrition behaviours were significantly correlated with their educational level, number of children, employment status and family income (Table 3).
Table 3 Participant’s socio-demographic characteristics and healthy behaviours
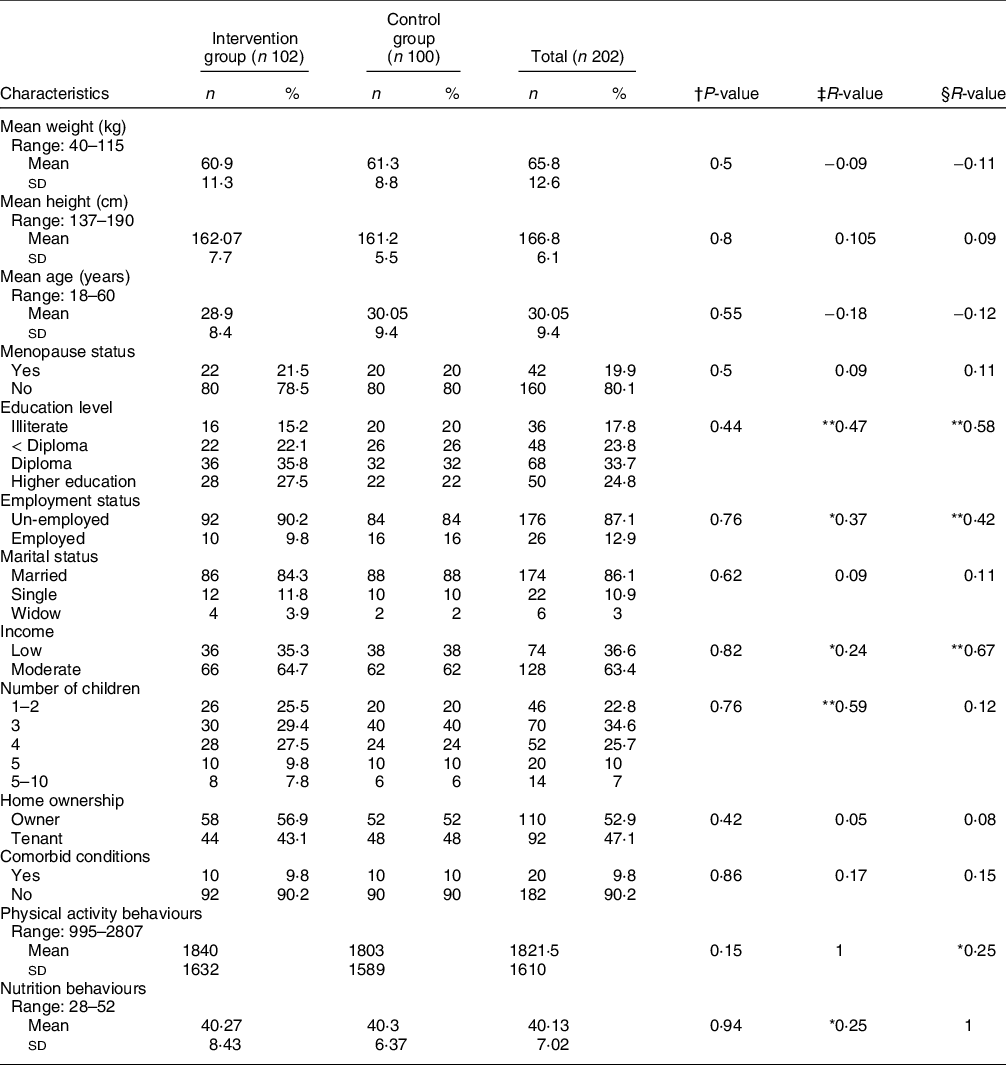
n, number of eligible participants.
* Correlation is significant at the 0·05 level.
† Testing significant change between control and experimental groups.
‡ Testing correlation between physical activities behaviours and demographic characteristics.
§ Testing correlation between nutrition behaviours and demographic characteristics.
** Correlation is significant at the 0·01 level.
At baseline, all of HPM’s constructs were homogeneous in intervention and control groups. The results related to the PA behaviours showed a significant difference (P < 0·05) in the change in all constructs of Pender’s HPM (except situational influences) in the intervention group compared with the control group at follow-up, and in change from baseline to follow-up in all scores. Our finding linked to nutrition behaviours showed the evidence of significant improvement (P < 0·05) in prior behaviours, self-efficacy, perceived barriers/benefits, commitment and behaviour outcomes in the intervention v. control groups at follow-up, and in change from baseline to follow-up. We found no evidence of any significant differences (P > 0·05) in the change in construct of Pender’s HPM, PA and nutrition behaviours in the control group at follow-up (Table 4). This result was synchronous with the regression models that showed significant interaction effects between time and groups. The results of this study showed that among the women in the intervention group compared with the control group, prior behaviours (P ≤ 0·001), self-efficacy (P ≤ 0·001), interpersonal influences (P ≤ 0·001), feeling (P = 0·001), perceived benefits and barriers (P = 0·002) and commitment to a plan of action (P ≤ 0·001) were significantly changed across time during baseline through follow-up (Table 5).
Table 4 Average scores for HPM’s constructs from baseline to follow-up for physical activity and nutrition behaviours

n, number of eligible participants.
* Testing significant change between control and intervention groups.
** Testing significant change from pre-intervention to 3-month follow-up.
Table 5 Interaction of intervention with time period for each HPM’s constructs

* Adjusted for number of children, employment status, income and level of education.
Discussion
We conducted this study to evaluate the effectiveness of Pender’s HPM on improving the PA and nutrition behaviours in Iranian women.
Prior-related behaviour is the main construct of the HPM model that influences individuals’ characteristics and experiences(Reference Heydari and Khorashadizadeh15,Reference Khazaee-Pool, Pashaei and Jahangiry31) . In the first session of intervention, the participants with low education (under diploma level) lack appropriate experience in health-promoting behaviours. These participants believed that they have low capabilities on their functioning to PA (low self-efficacy) and expressed they lack adequate knowledge in recognising healthy food groups, but a significant increase in the average score of individuals’ characteristics and experiences was observed in the intervention group in post-intervention and follow-up. This might be due to the increase in their knowledge and commitment to healthy behaviours. Specific findings from this study indicated that more than 77·1 % of the women in the intervention group had breakfast, used the five main healthy food groups, replaced consumption of sugar-sweetened beverages with water and reduced low-nutrition and energy-dense foods (snacks and fast food) after the intervention. Participants (65 %) engaged in PA, during the intervention, gradually increase the duration of appropriate PA that could be realistically fit into their particular lifestyle and daily schedule. This result was consistence with previous studies that found an increase in individual’s awareness that could be made to a higher stage of change and commitments to modify the level of PA(Reference Taymoori, Niknami and Berry30,Reference Stacey, James and Chapman32) and healthy nutrition behaviours(Reference Dehdari, Rahimi and Aryaeian24,Reference Rosário, Araújo and Padrão33) .
Similarly, in support of the study hypothesis, the participants in the intervention group reported high levels of agreement regarding perceptions and commitments about expected barriers and benefits of regular PA and eating habits, when compared with the control groups at the post-intervention and follow-up. The majority of participants (85 %) in our focus groups indicated that cultural and social barriers (e.g., their traditional role at home, particularly responsibility for their spouse and children, spouse opposition due to fear of harassment), employment status, religion and policy effects (Muslim religion, hijab bans) may have influenced their ability or willingness to participate in regular PA. Similarly, we discovered that PA was negatively and significantly correlated with the number of children and employment status, most likely due to having a high responsibility for childcare and working outside the home. Therefore, these participants lack adequate time and so take time out to do some PA. In the intervention group, most of the participants learn how to use replacement strategies to overcome perceived barriers, a commitment to be physically active and use the five main healthy food groups. Moreover, the intervention had significant effects on increasing positive feelings of healthy behaviours in the intervention group as compared with the control group. These findings support other HPM studies that identified the perceived barriers and benefits as the most influential factors to institutionalising behaviours in families(Reference Rosário, Araújo and Padrão33,Reference Benjamin and Donnelly34) .
In this study, the participants in the intervention group also reported a greater change in the mean score of perceived self-efficacy after the intervention, which was consistent with the results of other similar studies using the Pender’s HPM(Reference Khodaveisi, Omidi and Farokhi8,Reference Dehdari, Rahimi and Aryaeian24,Reference Vahedian-Shahroodi, Amin-Shokravi and Hidarnia35) . During the educational intervention, all participants learned how to set realistic goals to increase their commitment and time to perform appropriate PA per day or increase small changes that could be made to have healthier diets. Therefore, most of the participants in the intervention group have higher individual capability and self-confidence to perform appropriate behaviours regularly even in conflicting situations.
The mean score of interpersonal influences was significantly improved after intervention in the intervention group because they significantly developed their social networking and communication with their family members (brother, sister, husband and parents) and friends to share their attitudes towards nutrition and PA behaviours. Likewise, they had effectively convinced their families to support (encouragement) them to participate in regular PA or to follow a healthy diet. Several studies reported that people are more likely to perform healthy behaviours when they feel their relatives and friends encourage them frequently to perform those behaviours(Reference Hosseini, Ashk Torab and Taghdisi36–Reference Seo and Hah38). This finding highlighted the role of family members (particularly the parents and husband) and friends as influential people on healthy behaviours in terms of interpersonal modelling, which is in agreement with other health promotion studies using Pender’s model. Moreover, Fleury et al. suggested that, when designing health promotion programmes to modify the healthy behaviours of women, other family members should be encouraged to be positive role models by targeting their healthy behaviours(Reference Fleury and Lee39).
The present results demonstrated that the education intervention was able to increase the perception of situational influence in an experimental group after the intervention. However, this change was not significant in this work. This could be due to economic problems, cultural and social (policies and regulations) barriers. Findings showed that family income had a significant correlation with nutrition behaviours in the both groups. This result was confirmed by other educational studies that reported that a family’s income is an influential factor that can increase the frequency of healthy food consumption and food quality among women(Reference Khodaveisi, Omidi and Farokhi8,Reference Spence, Campbell and Crawford40) . Likewise, all participants addressed concerns about undertaking PA in the natural environment such as polluted weather, a lack of natural settings and exercise facilities, a lack of suitable streets and sidewalks, a great distance to travel to the gym and inadequate transportation. Thus, it is necessary to set an appropriate educational intervention for a better understanding of the barriers and facilitators that are needed for PA promotion among Iranian women.
Strengths of the study
This study is one of the first to test the effectiveness of educational intervention using all constructs of Pender’s model (HPM) on improving the PA and nutrition behaviours among a Muslim women population. Testing the application of the theoretical model in different populations is important in moving the theory forward and understanding the crucial components in successful interventions. Likewise, it is essential to test the mediator’s constructs to find out how they change behaviour outcomes and support people’s abilities to commit to behaviours. A unique aspect of the present research was that all of the positive effects of the HPM intervention were sustained at the 3-month follow-up, particularly on self-efficacy, perceived benefits, perceived barriers and interpersonal influences. This success of the HPM intervention may be related to useful theoretical mediator constructs (such as behaviour-specific cognitions and affect) or it may be due to specific behaviour change techniques such as setting out goals or having focus group discussions. Similarly, Van Sluijs et al. found positive effects of the HPM intervention on successful behaviour changes at a 3 or 6-month follow-up(Reference Taymoori, Niknami and Berry30,Reference Van Sluijs, Van Poppel and Twisk41) . This finding will provide a basis for future education interventions aimed at promoting healthy behaviours. In addition, this research is feasible and highly acceptable as it requires minimal investment and time by the training of health provider in healthcare centres; the PA nutritional training programme is simple enough that the health provider could be trained to perform it as well. In addition, the training programme is simple to adapt into the daily schedule of the women.
Limitations
The present study is subject to some limitations. Firstly, the results were assessed using a self-report questionnaire, which introduces the possibility of biased results. A second limitation is that mediator questions may not reflect all aspects of HPM’s constructs in a natural setting. However, we would not have expected this to affect our results because the test–retest reliability of these questionnaires was more than 0·9 in this study. The final limitation is that the mediator items may not have been sensitive enough to detect all changes over the 3-month intervention, particularly mediators of dietary change, due to the complexity and multiple dietary behaviours that were targeted in the intervention (vegetables, fruit, salt, fat, energy, meat consumption), and the lack of validated and brief items. Future research is still needed to use a behaviour promotion model to test their specific change constructs in different intervention programmes. Further studies should be conducted to sustain a positive behaviour change after the end of the intervention programme. As a fact, maintenance of behaviour change and identification of differences in mediators of behaviour change are part of a field that requires further interventions in the future.
Conclusion
In recent decades, international efforts towards change in policy indicated obesity requires attention among women, particularly in low-moderate socio-economic countries, and intervention strategies based on behaviour change theory are recommended to combat the ‘obesogenic’ environments. Therefore, we attempted to implement theory-based interventions aimed at promoting healthy eating habits and PA that had a significant impact on healthy behaviour promotion. Our finding highlighted the impact of intervention programmes based on HPM on strengthening PA and nutrition behaviours. A significant change was demonstrated in PA and nutrition behaviours in the intervention group that was also sustained at the 3-month follow-up. Likewise, the utility of Pender’s HPM constructs for promoting nutrition behaviour and PA was supported, since individuals in an intervention group moved to a higher stage of change if they had a greater perception of self-efficacy, benefits and barriers to healthy behaviours. It appears that the use of Pender’s HPM and its potential constructs could offer a promising way to develop critical techniques to behaviour change success. This has important implications for policy makers and researchers. Cultural and social policies (their traditional role at home, particularly responsibility for their spouse and children, spouse opposition due to fear of harassment), employment status, religious condition, number of children and economic problems have also been identified as major barriers affecting women’s ability or willingness to participate in regular PA and healthy dialysis. Therefore, to achieve a healthy lifestyle among women, appropriate training programmes must be systematically and formally implemented in healthcare facilities.
Acknowledgements
Acknowledgements: The authors wish to express their gratitude towards the vice president of research in Mashhad University of Medical Sciences. Financial support: The Mashhad University of Medical Sciences funded this project. Conflict of interest: The authors declare no conflict of interest. Authorship: All authors contributed to conceptualisation of the study. M.V. and M.T. interpreted the data, conducted quality appraisals and was involved in manuscript development; S.B.T.S., A.J. and Z.H.K. interpreted the data, conducted quality appraisals and drafted the manuscript; Z.H.K. conducted health education intervention among women population; H.E. analysed and interpreted the data, conducted quality appraisals. All authors have read and approved the manuscript. Ethics of human subject participation: This study was conducted after the approval and permission of Mashhad University of Medical Sciences Research Committee IR.MUMS.REC.1396.225 and was conducted with consideration of Helsinki Declaration in all phases of the study. Confidential data treatment was guaranteed. Written informed consent was obtained from the participants (trial registration: IRCT20160917029843N8).
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021002664










