Over the past 20 years, the incidence of non-communicable diseases (NCD) and especially CVD has changed, with a significant decline in industrialized countries and a rise in developing countries including those in the Eastern Mediterranean region(1). Iran is an Eastern Mediterranean country in which the population has adopted a more Westernized lifestyle with respect to nutrition habits, smoking and physical inactivity. This adoption has led to a higher prevalence of CVD risk factors among the Iranian population(Reference Sarraf-Zadegan, Boshtam and Rafiei2). CVD has emerged as the leading cause of mortality in Iran over the last decade(Reference Sarraf-Zadegan, Boshtam, Malekafzali, Bashardoost, Sayed-Tabatabaei, Rafiei, Khalili, Mostafavi, Khami and Hassanvand3). Several effective and successful intervention programmes in industrialized countries, targeting CVD risk factors, have resulted in decreasing prevalence of CVD events(Reference Puska, Salonen and Nissinen4–Reference Ornish, Brown and Sherwitz6). These have been rare in developing countries.
The Isfahan Healthy Heart Programme (IHHP) – a long-term, community-based intervention programme for health promotion through the reduction of CVD risk factors and hence CVD-induced morbidity and mortality – was conducted in two intervention cities (Isfahan and Najaf-Abad) and one reference city (Arak)(Reference Sarraf-Zadegan, Sadri and Malek Afzali7) in Iran. One of the main objectives of the IHHP was to improve health behaviours, such as dietary behaviour, of the general population, and so dietary patterns were assessed annually in both the intervention and the reference areas(Reference Sarraf-Zadegan, Sadri and Malek Afzali7) to assess achievement of this aim.
In recent years, major works on dietary assessment have measured diet quality from diverse perspectives and in a comprehensive method. Many studies suggest that measuring diet complexity is the preferred choice to use of a single nutrient from foods to measure diet quality(Reference Kant8, Reference Gerber9). Overall diet scores have been associated with diet-related plasma biomarkers(Reference Hann, Rock, King and Drewnowski10) and are more strongly associated with risk of disease than are single nutrients(Reference Kant, Schatzkin and Ziegler11).
Several such overall diet scores have been developed, including the Diet Quality Index(Reference Patterson, Haines and Popkin12), the Healthy Eating Index(Reference Hann, Rock, King and Drewnowski10) and the Global Dietary Index(Reference Huot, Paradis and Ledoux13). The present paper reports the results of the impact evaluation of the IHHP interventions on adults’ dietary behaviours after four years of the programme. Also, we test the hypothesis that change in dietary behaviour will vary based on settlement (rural and urban) and gender.
Methods and materials
Brief description of the programme
The IHHP long-term objectives are to decrease the incidence, disability and mortality of NCD. The short-term objectives are to improve knowledge, attitude and practice in the general population and health professionals about the causes and outcomes of NCD, improving their skills to control risk factors. The IHHP objectives are described in more detail elsewhere(Reference Sarraf-Zadegan, Sadri and Malek Afzali7).
The study was done in two intervention areas (Isfahan and Najaf-Abad, a city neighbouring Isfahan) and one reference area (Arak), all located in central Iran. According to the National Census in 2000, the population was 1895856 and 275084 in Isfahan and Najaf-Abad, respectively. Arak, located 375km north-west of Isfahan with 668531 population, was selected as reference area because of the similarity of its socio-economic, demographic and health profile with the intervention areas and good co-operation(Reference Sarraf-Zadegan, Sadri and Malek Afzali7). A major baseline cross-sectional survey was conducted in 12514 randomly selected adults aged ≥19 years and equally in both the intervention and the reference areas based on sex, age and settlement distributions in each community. About 5–10% of households in these clusters were randomly selected. One person aged ≥19 years per household was randomly selected if Iranian and mentally competent and if not pregnant for women(Reference Sarraf-Zadegan, Sadri and Malek Afzali7).
After the survey in 2001, a five-year intervention programme was started in August 2002 in urban and rural areas of Isfahan and Najaf-Abad. The interventions continued until 2006. Multistage random sampling and age-based Countrywide Integrated Non-communicable Disease Intervention (CINDI) protocol sampling methods(Reference Sarrafzadegan, Baghaei and Sadri14) were used for the baseline and subsequent annual surveys in both intervention and reference areas. Arak was evaluated as a reference area without any intervention.
The intervention activities
After analysing the results of the initial primary survey, we assessed the priorities and needs, and defined our objectives. Then, existing human and economic resources were used and set projects and strategies to emphasize tobacco control, healthy diet, physical activity and stress management based on different target groups. IHHP strategies have integrated activities in different fields of the health sector such as health promotion, disease prevention, treatment and rehabilitation. Key strategies for the interventional activities include public education through mass media, intersectional co-operation and collaboration, health professional education and involvement, marketing and organizational development, legislation and coordination, policy making, research and evaluation. Specific interventional activities are described elsewhere(Reference Sarraf-Zadegan, Sadri and Malek Afzali7). The IHHP targeted healthy nutrition, increased physical activity, tobacco control and stress management.
The programme includes ten distinct projects with different target groups, including: the Women’s Healthy Heart Project, Heart Health Promotion in Children, the Health Professional Education Project, the Youth Healthy Heart Project, the Worksite Intervention Project, Healthy Lifestyles for High Risk Groups, Healthy Food for Healthy Communities, Isfahan Exercise and Air Pollution Control Project, Non Governmental Organizations (NGOs) and Volunteer Intervention Project, and Healthy Lifestyle for Cardiac Patients. Each project is managed by a directors committee including academics, health professionals, stakeholders and policy makers, and are involved in planning, implementing and evaluating their projects. An underlying principle in all ten projects is to develop and maintain close contact with representatives of relevant community organizations. IHHP teams work intensively and closely with representatives of the mass media, health professionals, business and market leaders (food industry, groceries, bakeries, fast-food shops), key NGO staff, and local political decision makers. The Mayor, Governor and Governor General of Isfahan and Najaf-Abad are involved in IHHP and the Isfahan Governor General is the honorary president of the IHHP. Among the nutrition activities, the population has learned to: (i) substitute hydrogenated oil and ghee with liquid oil and olive oil to minimize consumption of trans fatty acids; (ii) increase consumption of fruit and vegetables, fish and soya protein; (iii) decrease consumption of sausages, animal fat, sweets and soft drinks; and (iv) consume low-fat dairy products. Details of the interventions are described elsewhere(Reference Sarraf-Zadegan, Sadri and Malek Afzali7).
Evaluation design
The IHHP was conducted as an action-oriented, quasi-experimental demonstration programme with ongoing evaluation. This programme included three phases: pre, during and post intervention, all of which have been described previously(Reference Sarraf-Zadegan, Sadri and Malek Afzali7).
The IHHP impact evaluation was done with four annual independent sample surveys and a 10-year longitudinal cohort sample survey, to compare the levels of modifiable risk factors for NCD in the intervention and reference areas before, during and after the implementation of the interventions. To our knowledge, there is no evidence of a similar comprehensive, integrated, community-based intervention NCD prevention programme in a developing country which used a quasi-experimental design and with different levels of evaluation.
Data on physical and biochemical measurements were collected in the intervention and reference areas in the same studies on independent samples in the post intervention phase in 2006(Reference Sarraf-Zadegan, Sadri and Malek Afzali7).
Short-term impacts of IHHP interventions on knowledge, attitudes and practices were evaluated in a series of independent sample surveys in 2002, 2003, 2004 and 2005, beginning in October every year(Reference Sarrafzadegan, Baghaei and Sadri14).
In the present paper we report only the short-term impacts of IHHP interventions on nutrition behaviour in the repeated cross-sectional study design in the intervention areas v. the reference area during these years, but because of some financial difficulties the fourth evaluation in 2005 was not done in the reference community.
Dietary assessment
Dietary behaviours were assessed with a validated, qualitative, forty-eight-item FFQ. As the present study is an intervention programme like the CINDI programme, the FFQ was adapted from the CINDI programme questionnaire(Reference Leparki and Nussel15). Frequency responses could be scored as 2, 1 or 0 depending on nutritional value, with a higher score indicating higher total and saturated fat intakes. For example, for the question ‘How many times a week do you usually eat meat, egg or whole dairy products?’, a score of 0 was given to none or once per week, a score of 1 was given to two or three times weekly and a score of 2 was given for a frequency of four or more times weekly. A total score was calculated by summing the responses to individual questions. Score attribution was based on the cholesterol–saturated fat index, atherogenicity index for a specific food(Reference Connor, Gustafson, Artaud-Wild, Flavell, Classick-Kohn, Hatcher and Connor16), as well as the American Heart Association recommendations and the National Cholesterol Education Program(17).
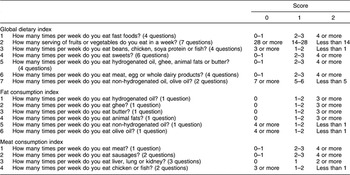
In the study, a global dietary index (GDI) of diet quality was calculated, representing the average of the mean of twenty-nine frequency questions in seven categories. A smaller GDI indicates better behaviour. The GDI was expected to decrease after the intervention activities. In addition to the GDI, two consumption indices were calculated for specific food groups: major sources of fat and meat products. These indices represent the mean of scores given to items from specific food groups. The fat consumption index (FCI) represents the mean of five frequency questions in five categories related to fat intake and the meat products consumption index (MCI) represents the mean of eight frequency questions in four categories related to meat intake. Table 1 shows how the GDI, FCI and MCI were calculated.
Table 1 Calculation of the global dietary index, fat consumption index and meat consumption index scores
The FFQ of CINDI was translated into Persian by a nutritionist. Foods that were not consumed in Iran were excluded and some typical Iranian foods, judged to be important contributors to total and saturated fat intake, were added. Face-content validity and translation of the questionnaire were assessed by an expert panel consisting of five nutritionists. The FFQ was pre-tested for clarity among 200 adults aged 19–69 years who were not subjects in the main study samples; they completed the questionnaire twice at a 2-week interval to assess the test–retest reliability (r = 0·8). Criterion-related validity was assessed in 2400 subjects of the baseline sample by comparing the GDI score with a single 24 h diet recall. Subjects were visited at home by trained interviewers to complete a 24 h diet recall. Correlation coefficients of the GDI with energy intake from total fat and saturated fat were 0·39 and 0·45, respectively.
Statistical analyses
Mean differences in BMI, age, FCI, MCI and GDI between the intervention and reference areas in each year were studied by the t test. Analysis of covariance was conducted to compare variables of interest in each area during these years by considering other variables such as age, BMI, educational level and smoking status in the models to control confounding effects. Univariate ANOVA was conducted to evaluate the impact of the IHHP on dietary behaviours by analysing the interaction between year and group based on sex and settlement (urban or rural). The SPSS statistical software package version 15 (SPSS Inc., Chicago, IL, USA) was used to analyse the data. P values less than 0·05 were considered significant.
Results
The total number of subjects studied comprised 12 512 individuals in 2001, and 5891, 4793 and 6083 individuals in 2002, 2003 and 2004, respectively. Because of financial limitations, the fourth evaluation study in 2005 was done only in the intervention communities, on a population of 3010 individuals. Table 2 shows the population frequency of basic characteristics (sex, settlement, educational level and smoking status) in the intervention and reference areas. Figure 1 shows the secular trend of mean GDI in the total population. Mean GDI was reduced significantly in the intervention areas compared with the reference area, based on a significant year × group interaction coefficient (P < 0·001).
Table 2 Basic characteristics of the samples in the intervention (experimental) and reference (control) areas, 2001–2005: Isfahan Healthy Heart Programme, Iran
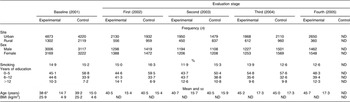
ND, not determined.
Mean values were significantly different from those of the control group in the same evaluation stage: * P< 0·05.
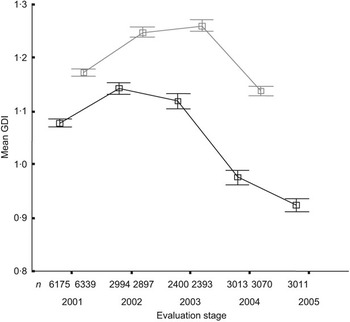
Fig. 1 Comparison of the trend in global dietary index (GDI) between the intervention (—□—) and reference (![]() ) areas, 2001–2005: Isfahan Healthy Heart Programme, Iran. Values are means with standard deviation represented by vertical bars
) areas, 2001–2005: Isfahan Healthy Heart Programme, Iran. Values are means with standard deviation represented by vertical bars
As Table 3 shows, mean GDI was significantly lower in the intervention areas than in the reference community based on gender and settlement in each year. Mean GDI also showed a significant increase from baseline to the first evaluation (P < 0·001); a mild increase in the reference area (P < 0·05) but a decrease in the intervention areas from the first to the second evaluation; and in the third evaluation study, despite the decrease in both areas, this decline was more in the intervention communities (P < 0·001).
Table 3 Comparison of mean scores on the global dietary index between the intervention (experimental) and reference (control) areas based on sex and site, 2001–2005: Isfahan Healthy Heart Programme, Iran
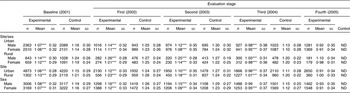
ND, not determined.
Mean values were significantly different from those of the control group in the same evaluation stage: ***P < 0·001.
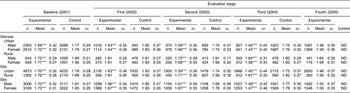
According to the significant year × group interaction coefficient for mean FCI in the total population, there was a significant improvement in FCI in the intervention areas v. the reference area (P < 0·001; Fig. 2).
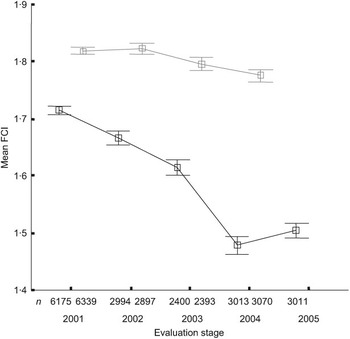
Fig. 2 Comparison of the trend in fat consumption index (FCI) between the intervention (—□—) and reference (![]() ) areas, 2001–2005: Isfahan Healthy Heart Programme, Iran. Values are means with standard deviation represented by vertical bars
) areas, 2001–2005: Isfahan Healthy Heart Programme, Iran. Values are means with standard deviation represented by vertical bars
Table 4 shows that the mean FCI was lower in the intervention areas than the reference area in each year (P < 0·001); however, it showed a significant decrease in each area during these years (P < 0·001). Although mean FCI appeared to reach a plateau from the third and the fourth evaluation study in the intervention areas, the difference between the intervention and the reference areas was not significant.
Table 4 Comparison of mean scores on the fat consumption index between the intervention (experimental) and reference (control) areas based on sex and site, 2001–2005: Isfahan Healthy Heart Programme, Iran
ND, not determined.
Mean values were significantly different from those of the control group in the same evaluation stage: ***P < 0·001.
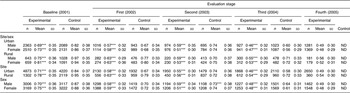
Figure 3 shows that the improvement in mean MCI was significantly more in the intervention areas than in the reference area (P < 0·001). As Table 5 shows, although the trend of mean MCI decreased significantly in both areas, for each year it was lower in the intervention areas.
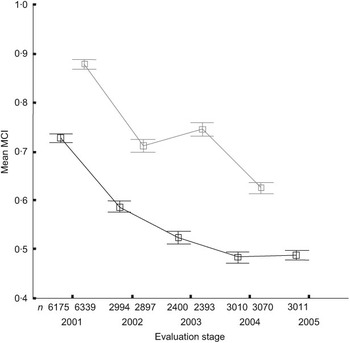
Fig. 3 Comparison of the trend in meat consumption index (MCI) between the intervention (—□—) and reference (![]() ) areas, 2001–2005: Isfahan Healthy Heart Programme, Iran. Values are means with standard deviation represented by vertical bars
) areas, 2001–2005: Isfahan Healthy Heart Programme, Iran. Values are means with standard deviation represented by vertical bars
Table 5 Comparison of mean scores on the meat consumption index between the intervention (experimental) and reference (control) areas based on sex and site, 2001–2005: Isfahan Healthy Heart Programme, Iran
ND, not determined.
Mean values were significantly different from those of the control group in the same evaluation stage: ***P < 0·001.
Discussion
The IHHP was effective in improving dietary behaviours as reflected in the GDI and consumption indices, especially the FCI. The programme had a local design and an impact on dietary behaviours, the same as previous heart health promotion programmes(Reference Fortmann, Taylor, Flora and Winkleby18–Reference Tudor-Smith, Nutbeam, Moore and Catford21). Compared with the North Karelia Project, which showed a reduction in SFA of 20 % in men and 24 % in women(Reference Pietinen, Nissinen, Vartiainen, Tuomilehto, Uusitalo, Ketola, Moisio and Puska22), other programmes have shown lower population-wide changes(Reference Fortmann, Taylor, Flora and Winkleby18–Reference Tudor-Smith, Nutbeam, Moore and Catford21). Joint analysis of the combined evaluation data of the Stanford Project, the Minnesota Heart Health Program and the Pawtucket Heart Health Program did not show any global acceptable impact on the main dietary variables, suggesting that statistical power was not an issue in the evaluation of the individual programmes(Reference Winkleby, Feldman and Murray23). In addition, a Quebec 4-year community-based programme could not show any impact on high-fat/junk food consumption(Reference O’Loughlin, Paradis, Gray-Donald and Renaud24).
At baseline in our study, GDI, FCI and MCI values in the intervention areas were significantly lower than those in the reference community. This can be considered a result of the small cultural difference between the intervention and reference areas, although we tried to choose similar communities. However, as the changes in GDI, FCI and MCI were compared during the years, our results were not confused. A significant secular trend was found in FCI, GDI and MCI, which revealed an improvement in fat consumption, overall diet and meat consumption, respectively. Trans fatty acid intake is the most important dietary factor in CVD incidence and hydrogenated oil is the main dietary source of this fatty acid(Reference Mozafarian, Katan, Ascherio, Stampfer and Willett25). Based on a previous study, hydrogenated oils produced in Iran contain 30–40 % trans fatty acids and also 89 % of the Iranian population consumes hydrogenated oil(Reference Bahrami and Mirzaeei26); so a reduction in trans fatty acid consumption was defined as the main nutritional objective in the IHHP(Reference Sarraf-Zadegan, Sadri and Malek Afzali7). To implement this objective, some intervention activities were conducted, including co-operation with the Isfahan Commerce Office to substitute hydrogenated oil distribution with liquid oil by coupon; educating people to not use hydrogenated oil by mass media and health professionals; and co-operation with oil factories in order to help them produce liquid oil instead of hydrogenated oil or to decrease the trans fatty acid content of the oils made. As IHHP intervention activities were not done in the reference area, the trend of FCI was a plateau in this community; therefore the significant decrease in FCI in the intervention areas showed the acceptable effect of the IHHP intervention activities on dietary fat consumption.
The trends in MCI showed that intervention activities can improve meat, poultry and fish consumption, i.e. they can increase fish and poultry consumption and decrease meat consumption frequency. As meat consumption in the Iranian population is not generally high, we focused on meat less than on oil in the IHHP; however, one of our intervention activities was increasing fish consumption. The high decrease in MCI in the reference area might be caused by a concurrent national health programme, including public education by mass media such as television, magazines and newsletters, independent from IHHP activities.
The GDI increased after one year of intervention in 2002, and it also improved after the second year of intervention; so the GDI might need more time to improve. Although the results showed a significant improvement in GDI and consumption indices in the intervention areas, the secular trend had the same direction in both areas, likely a result of other intervention activities that were in progress in the whole country parallel to the IHHP. The country-wide intervention activities were focused mainly on public education by mass media.
Strong secular trends towards in fat reduction have been shown in North America since the beginning of the North Karelia Project in 1970. Canadian adults decreased their dietary fat intake from 40% to 30% during 1970–8(Reference Gray-Donald, Jacobs-Starkey and Johnson-Down27). In Quebec, nutrition assessments have shown that men aged 35–49 years reduced their fat intake from 37·0% to 34·0% and women from 37·5% to 33·4%, during 1970–90(Reference Huot, Paradis and Ledoux13). Also, SFA intakes decreased from 15·2% to 12·9% in men and from 15·4% to 12·2% in women(Reference Huot, Paradis and Ledoux13).
Study limitations and strengths
Cross-sectional, independent samples were used in the present study despite the fact that a cohort sample shows greater statistical significance(Reference Diehr, Martin, Koepsell, Cheadle, Psaty and Wagner28). The FFQ is subject to bias due to the limited food list, the choice of frequency categories and the difficulty in remembering foods eaten in the past(Reference Willett29); moreover, as the FFQ employed was qualitative, the estimation of dietary intake was not exact. In addition to these limits, dietary behaviours are subject to recall or report bias(Reference Hebert, Clemow, Pbert, Ockene and Ockene30). On the other hand, the longitudinal nature of the data and the novelty of the data and the programme in a developing country are the main strengths of the present study. Although we tried to choose the intervention and reference areas to be similar in health profile, there was a small difference between these two areas; however, as we compared their dietary behaviour changes during the years, this limitation did not confuse the results.
Conclusion
The IHHP interventions were effective in improving dietary behaviours at the population level. The greatest effectiveness was seen for the FCI, as a representation of fat consumption. Since these simple and integrated interventions were effective, they can be disseminated in other communities.
Acknowledgements
We have no conflicts of interest. N.M. wrote the paper and co-operated in designing and managing the studies, and conducting the intervention activities and evaluation studies; R.K. co-operated in designing the study and writing the paper; M.S. co-operated in conducting the intervention activities; N.S. co-operated in designing and managing the study; F.S. co-operated in conducting the intervention activities and evaluation studies; G.H.S. co-operated in designing and managing the study; M.M. co-operated in conducting the intervention activities and evaluation studies; H.A. co-operated in conducting the intervention activities and evaluation studies; S.H. co-operated in conducting the evaluation studies; F.S. co-operated in conducting the intervention activities. The Organization of Planning and Management, the Deputy for Health of the Iranian Ministry of Health, Treatment, and Medical Education, and the Isfahan Cardiovascular Research Center funded the study. We thank Isfahan Provincial Health Center and Arak Health Center who helped us in performing the study and Miss Hengameh Nouri for her help with statistical analysis.










