In 2000, world leaders committed their nations to a new global partnership to reduce extreme poverty in its many dimensions and set out concrete, time-bound targets to be achieved by 2015: the Millennium Development Goals (MDG)( 1 ). While accomplishments exist, progress has been uneven and in some cases slow across both countries and MDG. There is an urgent need to support countries as they design, implement and monitor effective public health strategies( 2 ).
The burden of disease from vitamin and mineral malnutrition is high, compromising maternal and child health and well-being. It is estimated that 7 % of infant deaths and 10 % of the total disease burden worldwide are caused by the combined effects of deficiencies of iron, vitamin A and zinc, suboptimal breast-feeding and childhood underweight( 3 ). In low-income countries, preventable nutritional deficiencies can prevent one in thirty-eight newborns from reaching 5 years of age( 3 ). Other important vitamin and mineral deficiencies preventing optimal maternal and child health and nutrition include those of calcium, folate, vitamin B12, iodine and vitamin D. Various vitamin and mineral interventions targeting women, children and the entire population have been proposed for integration into public health programmes( Reference Horton, Shekar and McDonald 4 , Reference Pena-Rosas, De-Regil and Rogers 5 ). The interventions include oral supplementation for women and children, point-of-use fortification of foods consumed by children, fortification of staple foods and bio-fortification of staple crops. Support of breast-feeding practices and consumption of micronutrient-rich foods also contribute to improve micronutrient status and health. All of these interventions are considered feasible to scale up and likely to reduce death, disease and prevent the irreversible harm attributable to micronutrient deficiencies, thus contributing to the achievement of various MDG( Reference Horton, Shekar and McDonald 4 ).
Nutrition interventions are more likely to be effective if they are ‘owned’ by stakeholders in each country. They should also be built into existing health strategies based on a clear understanding of how the micronutrient intervention will contribute to achieving public health goals. Promoting and strengthening national ownership and leadership for development is itself a key determinant of progress in achieving the MDG( 6 ). This requires that stakeholders not only select effective interventions, but also understand the potential impact, the programme components and the activities required to implement the programme, the resources available and the context where an intervention will be implemented. Traditionally this has been achieved using, for example, protocols, lists, flow charts or logical frameworks. A logic model is a valuable tool to increase stakeholders’ understanding of these issues and their interrelationships.
A logic model is a visual representation of the programme that maps the expected relationships among the resources invested, the activities taking place, the direct results of programme activities and the benefits or changes that are expected to occur among intervention participants over time( Reference Frechtling 7 , Reference Renger and Titcomb 8 ). In other words, a logic model is a description of the programme logic which explains the expected changes from multiple and synchronized actions( 9 ), and ideally should first be developed as a part of the initial programme description. Logic models are often presented on one page and read from left to right showing how each step is expected to lead to the next; however, they do not need to be limited to one page nor laid out in a linear manner left to right if other schemes (e.g. laying out top to bottom, or circles) better describe the expected programme logic.
Methods
The Department of Nutrition for Health and Development from the WHO and the International Micronutrient Malnutrition Prevention and Control Program from the US Centers for Disease Control and Prevention (CDC) established in 2009 a working group to develop a generic logic model and a tool to standardize indicators that could be adopted and adapted for the design, implementation and monitoring of micronutrient interventions. Similar types of generic logic models have been developed for other programmatic areas( 10 , Reference Reed, Jordan and Mortensen 11 ) and the relevance of this idea was confirmed after a short scoping session with stakeholders held during the same year at the International Nutrition Congress in Bangkok, Thailand.
The structure of the model was founded in programme evaluation, public health theory and programmatic experience gained in flour fortification( Reference Pena-Rosas, Parvanta and van der Haar 12 , 13 ). Three logic models were initially developed taking into consideration the main delivery systems for micronutrient interventions: market, institutional settings and community activities. Some of these initial logic models were piloted and adapted to existing programmes in countries.
In January 2010, a two-day workshop was convened by CDC and WHO in Atlanta, USA with representatives from organizations that are currently supporting or implementing vitamin and mineral interventions worldwide and who would be potential users of this tool, including UN and international donor agencies, international non-governmental organizations, research institutions and universities. The consultation served to discuss and validate the structure of the logic model by building on partners’ experiences developing and implementing interventions. The group-oriented discussions suggested merging the initial three logic models into a single generic one and improving its structure to better depict real-life programmes and feasibility of measurement. The logic model was then subjected to an iterative review process with the workshop group and other experts in programme evaluation, which included testing the ability to adapt the logic model to various:
-
• delivery systems, such as Ministry of Health facility-based, community volunteer-based and market-based distribution systems;
-
• vitamin and mineral interventions, including mass food fortification, point-of-use fortification with micronutrient powders, supplementation, and breast-feeding support and counselling; and
-
• intervention approaches targeted at individuals, policy and environmental changes, and mass communication strategies.
Results
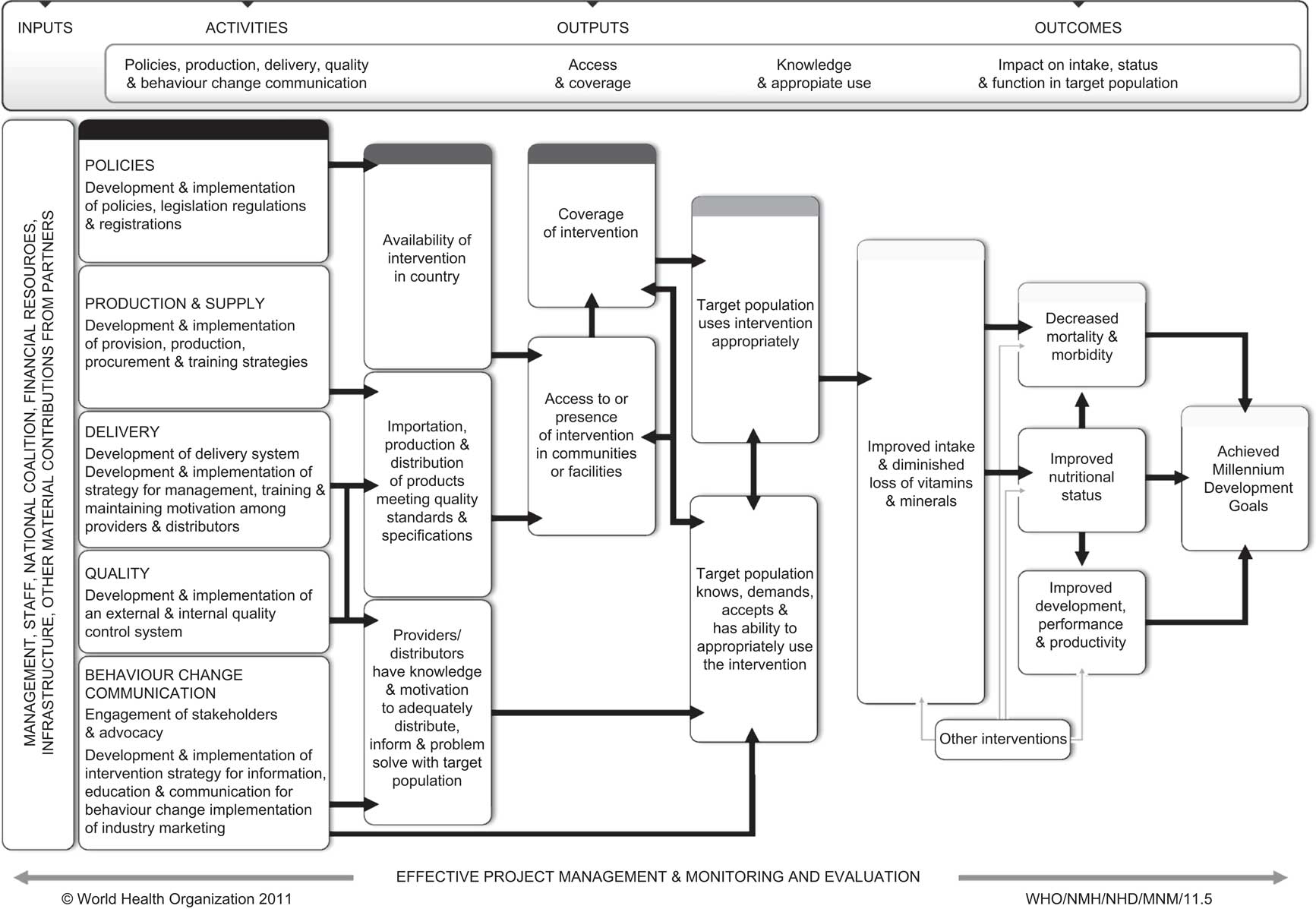
The WHO/CDC logic model for micronutrient interventions in public health (Fig. 1) is a tool intended to assist countries describe their micronutrient programmes focused on achieving public health goals. The logic model aims to provide a common framework and understanding among stakeholders from different contexts and with different needs (e.g. those involved in programme operations and partners such as government staff, donors, coalitions and intervention staff; as well as those served or affected by the intervention such as professional associations, advocacy groups, elected officials, academics, community members/organizations and participants). Ideally, it is first developed as part of the initial programme description and its use can support the planning, implementation, monitoring and evaluation of micronutrient programmes in order to improve their effectiveness. It does not provide explicit guidance on the selection of indicators as they are programme-specific, but the visualization of expected intervention processes facilitates the identification of indicators for each box. The logic model also serves to communicate and advocate for the actions that are required to reach public health goals and objectives.
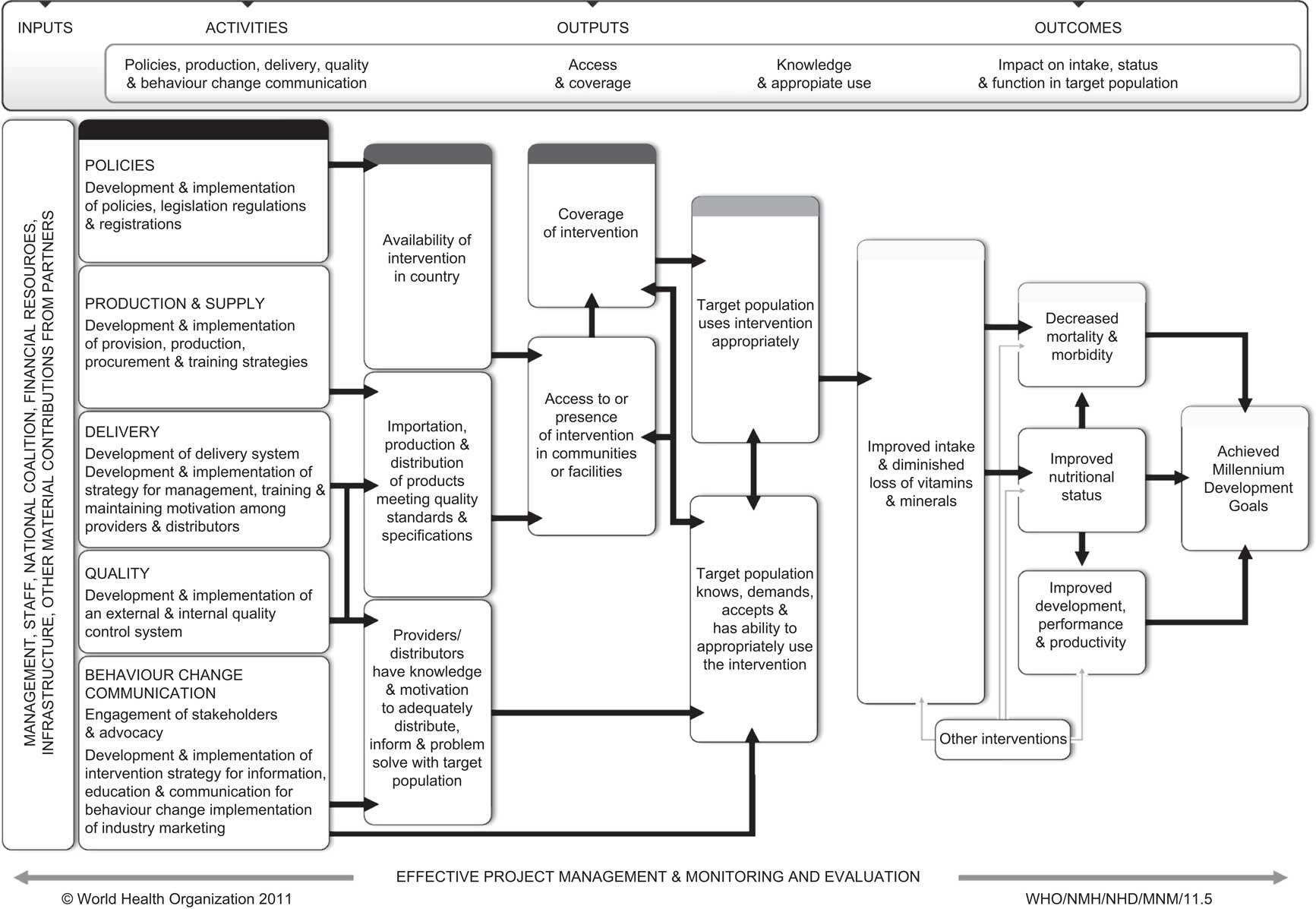
Fig. 1 WHO/CDC logic model for micronutrient interventions in public health
The logic model is organized according to four main hierarchical categories: inputs, activities, outputs and outcomes.
-
1. Inputs are the resources invested in the intervention, including personnel (paid and voluntary), equipment, materials, partnerships, and direct and indirect support from organizations and communities.
-
2. Activities are the actions, events and processes of programme implementation; for example, developing protocols, passing legislation, designing supply delivery systems and engaging stakeholders. The WHO/CDC logic model includes five main categories of activities from different spheres that together with the inputs are instrumental to initiate and sustain a programme with a single or multiple interventions: (i) policy; (ii) products and supply; (iii) delivery systems; (iv) quality control; and (v) planning of a behaviour change communication strategy.
-
3. Outputs are the direct effects or products of activities, such as: the procurement of annual supplies and availability of the supply in the country; staff trained to deliver and counsel participants on the intervention; or availability of the intervention in communities or markets.
-
4. Outcomes are the benefits or changes among intervention participants during or after the intervention. Outcomes could include changes in: behaviours, knowledge, skills, motivations or decision making related to an intervention; or intake of micronutrients, nutritional status, health conditions or functions. It is important to recognize that outcomes may be intended or unintended, positive, negative or neutral. In some logic models ‘impacts’ are listed as a separate category from ‘outcomes’, but in the WHO/CDC logic model ‘impact’ is a type (subset) of outcomes.
The WHO/CDC logic model lays out the presumed connections between inputs, activities, outputs and outcomes from left to right and the use of boxes and arrows might make the relationships appear unidirectional or static in the model figure; however, they can be dynamic and interact with each other (Fig. 1). The focus should be on describing the programme logic in a way that makes sense and is useful for a given intervention. For example, in the proposed logic model the coverage of an intervention reflects the convergence of the intervention delivery at community level and the receipt and demand of the intervention among participants. For some interventions, coverage may best fit as an output and for others as an outcome; the best location for coverage in a specific intervention is context-specific, but regardless of the location it should be included in the logic model pathway.
Typically, the activities and outputs reflect the work and are under control of those involved in the implementation of interventions (i.e. programme staff). Depending on the intervention, the activities and outputs might also involve the work of non-programme staff, such as food producers in the case of mass fortification interventions. The outcomes are distinct in that they represent the expected effects among the participants and are not under the control of the programme staff but are reasonably expected to be influenced by the intervention. Inputs define the scope and breadth of the activities and outputs, as well as the expected outcomes. Lastly, the influence of additional interventions to achieve outcomes is also acknowledged with an ‘other interventions’ box in the logic model, as the existence of these interventions may also influence the ability to carry out activities and achieve outcomes if they are not considered. Because they are not the main focus of the intervention reflected in the logic model and occur independently from the intervention, the arrows for the ‘other interventions’ are shown in grey.
Discussion
When the WHO/CDC generic logic model is used, it inevitably requires adaptation at the local, regional or national levels through discussion between government authorities and their stakeholders.
The logic model is based on the assumption that no major unexpected cultural, political, economic, social or technological factors or unforeseen contextual issues will influence the intervention (e.g. sudden war or changes in financial resources). Programme staff are expected to monitor any known contextual or moderating factors that could support or limit the effectiveness of the intervention and the achievement of programme goals; although these are outside the direct control of the programme, monitoring allows for the timely recognition of changes that could influence the intervention and identify whether programme adjustments are warranted( 14 ).
There are assumptions and expectations that either consciously or unconsciously influence decision making when developing a logic model for micronutrient interventions and it is useful to make them as explicit as possible to increase use, understanding and ownership of the intervention and logic model. For example, stakeholders may hold different ideas about how an integrated intervention package with multiple components will function in real life compared with what is anticipated in the programme theory described on paper. Stakeholders might recognize the complexity associated with integrating multiple components with fidelity and different stakeholders might prioritize some components over others, for example. Another example of an assumption is that intervention delivery staff will be motivated to participate in training and deliver the intervention. Discussing assumptions and expectations helps improve communication among programme staff and stakeholders through the assessment of whether these assumptions and expectations are reasonable or adjustments are needed.
An additional consideration is that inputs, activities and outputs are programme-specific and depend on the stage of development of a programme and the intervention. During the intervention development stage, if they do not already exist then it may be necessary to create national coalitions that advocate, support and promote national policy decisions and strategic plans; a stakeholder coordinating body to oversee the development and implementation of the intervention; and delivery channels to implement an intervention. In later stages of programme maturity, there may be several national coalitions already developed, a stakeholder coordinating body in place, and delivery channels implemented and available. The logic model should be periodically reviewed and revised, if needed, in order for it to continue to serve as a useful tool for planning, implementation, monitoring and evaluation. Stakeholders can revise the logic model as the programme transitions through different stages of the project life cycle (e.g. development, implementation, scale-up and maintenance). In addition, some vitamin and mineral interventions stand alone while others are a part of broader public health programmes. In some cases it might be useful to develop a logic model focused on just one component of an integrated programme.
When adapting the logic model, stakeholders and users might prefer the content in each of the boxes to remain at a higher level, such as proposed in Fig. 1. Alternatively, it can also be useful to include very specific details in each box or disaggregate boxes with multiple concepts into several boxes with fewer concepts per box in order to provide finer detail of the expected programme processes. As described in Fig. 1, the logic model does not necessarily make explicit all of the important factors that operate within and between the boxes. If a higher level of specification is needed, then a logic model that does not necessarily fit on one page might be preferred, or a companion document that provides this detail might be required. The decision of how general or specific to write the contents of each box depends on the use, as well as stakeholder needs and interests, and thus is programme-specific. During the adaptation, changing the boxes may require an adjustment in the direction or orientation of arrows in order to accurately reflect the expected connections between boxes ultimately leading to the desired outcomes. The logic model (the boxes, arrows and content) can be adapted to each context and it is likely that an adapted logic model will look different from the generic logic model. An example of how this model can be adapted for an integrated infant and young child feeding and micronutrient powders project will soon be published( 14 ).
The format of the logic model is a strength because it explicitly outlines the different programme components and how they relate to each other leading to the expected outcomes. Because of this ability to use the logic model boxes to identify indicators tied to expected intervention processes, the WHO/CDC logic model will be a key component of the forthcoming WHO/CDC Indicator eCatalogue, a repository of vitamin and mineral intervention indicators. For stakeholders, a strength of the logic model format is that it allows for easy visualization and review of the expected programme theory against actual monitoring results, which supports stakeholder understanding, coordination and ownership.
Conclusion
The generic WHO/CDC logic model for micronutrient interventions in public health simplifies the process of developing a logic model by providing a tool (template) that has already identified and highlighted the high priority areas and concepts that apply to virtually all public health micronutrient interventions. During its development, it was tested with multiple delivery systems, interventions and approaches, and adapted to existing interventions in countries in order to ensure that the content and structure worked for almost any public health micronutrient intervention. This logic model is easy to adapt according to the country context, intervention and maturity of the programme and its use helps support programme planning, implementation, monitoring and evaluation of micronutrient interventions in public health. Its availability in the six official languages of WHO – Arabic, Chinese, English, French, Russian and Spanish – is expected to make it both more equitable and effective by reaching larger audiences. This logic model also facilitates a common understanding among stakeholders of expected intervention processes and actions that are required to reach the goals and objectives of a programme and serves as a complement or alternative to the narrative description of the overall programme. When combined with other resources and tools, the WHO/CDC logic model provides a foundation for effective programme planning, implementation, monitoring and evaluation of micronutrient interventions in public health practice.
Acknowledgements
Source of funding: This work received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Ethics: Ethical approval was not required. Conflicts of interest: The authors report no conflicts of interest. Authors’ contributions: L.M.D.-R., J.P.P.-R. and M.E.d.S.J. conceived of the original idea and wrote the first draft. All authors contributed to the interpretation and approved the final document. L.M.D.-R. and J.P.P.-R. are WHO staff members. These authors alone are responsible for the views expressed in this publication, which do not necessarily represent the decisions or policies of the WHO. R.F.-A. and M.E.d.S.J. are staff members of the CDC. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC. Acknowledgements: The authors would like to thank Cria Perrine, Tom Chapel, the technical consultation participants and the country stakeholders. They are grateful for their feedback in the development of the generic logic model.