Rising rates of diet-related chronic disease, attributed in part to greater consumption of convenience foods and less frequent cooking at home, have prompted increasing interest in cooking interventions as a means of improving diet quality, especially among socioeconomically disadvantaged populations which carry a disproportionate burden of chronic disease(Reference Wolfson, Frattaroli and Bleich1). Food insecurity is a mediator in the relationship between poverty and poor health outcomes in children and adults(Reference Pérez-Escamilla and Vianna2,Reference Seligman, Laraia and Kushel3) .Cooking skills can help to mitigate risks associated with food insecurity through improved ability to prepare nutritious meals from low-cost ingredients and better management of food resources(Reference Pooler, Morgan and Wong4,Reference Reicks, Kocher and Reeder5) . Emerging frameworks, including Food Agency, conceptualise cooking skills not as discrete manual tasks but as a comprehensive set of knowledge, skills and behaviours, acknowledging the complex environmental factors that influence food provisioning and cooking behaviours(Reference Wolfson, Bostic and Lahne6). Community health centres (CHC) have emerged as an important venue to address food insecurity and other barriers to consumption of a healthy diet along the socio-ecological continuum through interventions such as onsite farmers markets, produce prescription programmes, teaching kitchens and cooking classes(7–Reference Alvarez, Lantz and Sharac11). This paper describes the development and pilot evaluation of a CHC located, Food Agency-focused cooking intervention to improve diet quality, mitigate food insecurity risk, and reduce food waste.
While more frequent home cooking is associated with better diet quality and is generally perceived to be healthier and more affordable, low-income and food insecure households still face multiple barriers to preparing healthy meals(Reference Daniel12–Reference Tiwari, Aggarwal and Tang17). Common barriers to healthy cooking among low-income households include lack of time and limited affordability of and access to fresh ingredients(Reference Wolfson, Bleich and Smith18). Perceived risk of wasting food also plays a significant role in shopping and cooking decisions in low-income households. Low-income parents are less likely to purchase unfamiliar foods compared with high-income parents, due to fear of wasting money on foods that their children would not like(Reference Daniel12). Similarly, Supplemental Nutrition Assistance Program-eligible adults describe concerns about food waste as a barrier to purchasing fresh foods and experimenting with new ingredients(Reference Gosliner and Shah19). Cooking skills can help address the barriers faced by low-income households in multiple ways: through more efficient meal preparation, ability to prepare tasty meals from low-cost ingredients and make recipe substitutions and strategies to utilise and preserve perishable foods(Reference Engler-Stringer20,Reference Engler-Stringer, Stringer and Haines21) . While there is some evidence that cooking skills are associated with reduced household food waste, literature on this subject is limited(Reference Lavelle, Spence and Hollywood22,Reference Schanes, Dobernig and Gözet23) . Schanes et al.(Reference Schanes, Dobernig and Gözet23) explain that cooking-related behaviours including ‘planning, shopping, storing, cooking, eating and managing leftovers play a decisive role in food provisioning but also in food waste generation’ and that reducing food waste ‘requires time, knowledge and cooking skills to better utilise foods creatively’. However, cooking skills are rarely conceptualised to include this broad range of cooking-related behaviours; therefore, cooking programmes often focus solely on discrete manual tasks and specific recipes(Reference Wolfson, Bostic and Lahne6). Furthermore, evaluations of cooking interventions typically do not assess outcomes related to food waste(Reference Reicks, Kocher and Reeder5,Reference Reicks, Trofholz and Stang24) .
Programmes to increase cooking at home are associated with favourable changes in multiple domains including diet, health status, cooking confidence, cooking knowledge and food security(Reference Pooler, Morgan and Wong4,Reference Reicks, Kocher and Reeder5,Reference Rees, Hinds and Dickson25) . Despite the prevalence of cooking interventions, programmes are rarely focused exclusively on cooking skills, are rarely informed by theory and rigorous evaluation is generally lacking(Reference Reicks, Kocher and Reeder5,Reference Wolfson, Bostic and Lahne6) . There is increasing recognition of the complex environmental factors that influence nutrition and cooking behaviours. The Food Agency framework posits that cooking requires a ‘complex set of deliberate procurement, budgeting, organizational, conceptual, and decision-making skills’ that are ‘specific to an individual’s context and environment’(Reference Wolfson, Bostic and Lahne6). A Food Agency-based pedagogy integrates cognitive abilities like planning and decision-making with manual cooking skills, preparing learners to navigate the complex factors that influence provisioning and preparing nutritious meals in a way that is adaptable to individual contexts(Reference Trubek, Carabello and Morgan26). Decisions about meal preparation occur within complex individual, social and physical contexts. Community-tailored cooking interventions incorporate these approaches by addressing community-specific barriers to cooking and including information that is most relevant to participants. Thus, there is a need to assess the feasibility and effectiveness of Food Agency-focused cooking education programmes that are tailored to specific communities. CHC situated in underserved communities provide an opportunity to engage low-resource populations in cooking education as part of a holistic, culturally sensitive approach to improving food security and diet quality.
CHC are engaged in a variety of interventions to improve diet quality and food security, with increasing interest in integrated services that go beyond traditional nutrition education and counselling to address food access, nutrition literacy and cultural barriers(7). CHC located farmers markets, produce prescription programmes and cooking demonstrations have been associated with increased food security, increased fruit and vegetable intake and improved glycemic controls(Reference Freedman, Choi and Hurley9,Reference Bryce, Guajardo and Ilarraza10,Reference Castañeda, Giacinto and Medeiros27,Reference Van Name, Camp and Magenheimer28) . In a 2017 survey from the National Association of Community Health Centers, 16 health centres reported having ‘cooking/kitchen programmes’(7) but published evaluation of these programmes is limited. Given that CHC have limited time, space and resources to implement cooking education programmes(Reference MkNelly, Nishio and Peshek8), more research is needed to assess the feasibility and effectiveness of these interventions.
In this academic-community research partnership, we developed, piloted and evaluated a Food Agency-based cooking skills intervention. We used focus groups with patients at the CHC to inform the content and format of the intervention which was developed with the collaboration and guidance of a community steering committee(Reference Strong, Israel and Schulz29). The objectives of this study were to (1) develop and implement a community-tailored, Food Agency-based cooking programme at a CHC and to (2) evaluate the effect of the intervention on cooking confidence and food waste.
Methods
Study design
We used an exploratory sequential mixed methods design(Reference Creswell and Plano Clark30) and principles of community-based participatory research (CBPR) to guide this research(Reference Strong, Israel and Schulz29,Reference Wallerstein and Duran31) . First, we used focus groups to explore cooking and shopping behaviour, food access and utilisation of existing food and cooking programmes among patients at a CHC. Findings from the focus groups and input from the health centre steering committee informed the development and pilot testing of a hands-on cooking intervention in the health centre’s teaching kitchen. We evaluated the intervention using pre/post surveys immediately before and after the classes and qualitative interviews 2–4 months after the intervention.
Focus group participant recruitment
Clients at a CHC that is a Federally Qualified Health Center in Detroit, MI, were recruited to participate in focus groups using paper flyers and advertisements on the CHC’s Facebook page. Inclusion criterion was being age 18 years or older; individuals did not have to be patients at the CHC to participate in the study. Participants were required to register for the focus group by calling or signing up in person at the CHC. Registration was first come first served and was capped at twelve participants per group. Participants received a reminder call 1 or 2 days prior to the focus group.
Focus group procedures
Four focus groups (two in English and two in Spanish) were held in a private meeting room at the CHC. Focus groups were approximately 90 min, were audio recorded and were moderated by J.A.W. T.G. took notes and co-moderated the Spanish groups. Participants completed a brief demographic survey at the beginning of the focus group. In the survey, participants were also asked ‘in an average week, how many days do you, or someone in your house cook food for dinner or supper at home?’ Refreshments were provided, and participants received a $30 gift card to a local supermarket as compensation for their time.
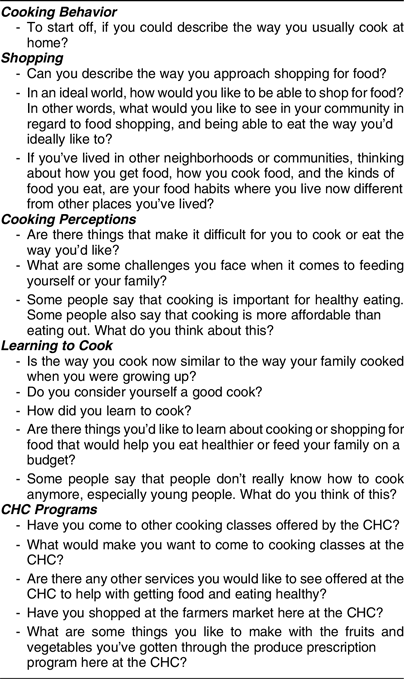
A discussion guide was developed by the research team in collaboration with the CHC steering committee (see Appendix A). The first set of focus group questions was designed to elicit information about cooking and shopping habits, including attitudes and challenges related to these activities, perceptions of food access and cooking in the community and associations between cooking and health. The second set of focus group questions focused on how participants learned to cook and what they would like to learn in a cooking class. The last set of questions was about satisfaction with food and nutrition programming at the CHC and what would motivate participants to attend a cooking class. The questions were open ended to encourage discussion among participants.
Focus group analysis
Audio recordings from the focus group were transcribed verbatim by a professional service. Spanish transcripts were translated into English prior to analysis. Transcripts were coded using a codebook developed a priori by the research team. All transcripts were double coded by two members of the research team. Coding proceeded iteratively, and transcripts were revisited as new codes were identified and added to the codebook(Reference Saldaña32). Throughout coding, the research team met to discuss coding and interpretation of codes. The Dedoose online qualitative data analysis platform was used to facilitate coding and analysis. After initial line by line coding was complete, codes were aggregated into broader themes, and code memos were produced for each theme and code grouping(Reference Birks, Chapman and Francis33).
Cooking intervention recruitment
Recruitment was conducted by the CHC staff. Priority was given to people who participated in a focus group; they received a phone call from a community health worker inviting them to a cooking class. The classes were then advertised to the broader community using flyers in the CHC waiting area, advertisements on the CHC Facebook page and referrals from providers, community health workers and the nutrition coordinator. Participants were required to register for the classes by calling or signing up in-person at the CHC. Registration for each class was capped at fifteen participants. Participants were not allowed to attend more than one class. Participants received a reminder call 1 or 2 days prior to the class.
To incentivise attendance and encourage participants to continue practicing the skills learned in class, each participant received a reusable tote bag with a recipe book, a strainer, three stainless steel prep bowls, a vegetable peeler, a certificate of completion and some ingredients from the recipes prepared in the class. In addition, all participants were entered in a raffle to win an instant pot or a vacuum sealer. These incentive items were chosen based on information gleaned during the focus groups and input from the steering committee.
The cooking skills intervention
We developed a hands-on cooking class curriculum informed by findings from the focus groups and input from the steering committee at the CHC. After discussing findings from the focus groups with the steering committee, we selected ingredients and recipes based on what focus group participants were interested in learning about (i.e. eggplant and vegetarian cooking) and what types of food participants were already familiar with (i.e. Mexican cuisine and chicken). We also considered which foods were available at the CHC’s weekly farmer’s market and organised the classes around themes that the steering committee thought would be relevant to the CHC patient population, such as anti-inflammatory cooking, vegetarian cooking and seasonal ingredients. The classes were promoted using those themes, rather than using a ‘healthy cooking’ framing. In order to incorporate a Food Agency approach and to illustrate strategies for reducing food waste, we selected recipes that demonstrated multiple methods of preparing the same ingredients (e.g. sautéed v. roasted v. quick pickled) and that could be easily adapted to substitute different vegetables or different seasonings. Throughout the class, the instructor emphasised how recipes could be adapted for substitute ingredients. The objectives of the intervention were fourfold: (i) build Food Agency (with particular emphasis on mise en place and self-efficacy adapting recipes), (ii) increase knowledge about multiple uses and food preservation techniques for different ingredients to mitigate food insecurity and prevent food waste, (iii) increase cooking confidence and enjoyment among participants and (iv) increase awareness and use of the CHC onsite farmers market among participants.
The classes were conducted in either English or Spanish and were centred on three themes: Mexican-inspired vegetarian cooking (English and Spanish), anti-inflammatory cooking (English only) and seasonal cooking (English and Spanish). A total of six classes were offered on weekdays in the CHC teaching kitchen on either Tuesday evenings 17.30–19.30 or Thursdays from 10:30 to 12:30. Each 2-h class consisted of 20 min of instruction, 1 h and 20 min of active cooking in small groups and 20 min of tasting and group discussion. Classes were led by members of the research team with assistance from the CHW and Nutrition Coordinator at the CHC.
In the first part of the class, the instructor introduced the theme, discussed and demonstrated basic cooking skills and concepts including mise en place, basic knife skills and strategies for reducing food waste, such as quick pickling and how to store different types of produce. During this instructional component, participants were encouraged to share their own knowledge and experiences, setting the stage for a flexible and collaborative learning environment. Participants were then divided into small groups, assigned one of two recipes and instructed to gather their ingredients and begin cooking, following a recipe handout. The two recipes used the same basic ingredients to demonstrate the versatility of the ingredients and the utility of different cooking methods and seasonings. The recipes also left several decisions about exact amounts of ingredients or components of the meal up to the participants to encourage using their own preferences regarding ingredients and taste to drive decision-making during cooking. The instructors circulated throughout the classroom to answer questions, provide tips, encourage equitable participation, coordinate use of the oven and stove top and monitor food safety. A variety of herbs, spices and vegetables were provided, and participants were encouraged to experiment with different flavour combinations, while following the basic contours of the recipe provided.
At the end of class, participants sat down to a meal of the food they had prepared and were able to taste and compare the food prepared by each team. The instructor facilitated discussion among the participants about their experience preparing the different recipes, what was new or surprising about the recipes, differences between the dishes prepared by each team and what changes they might make if they cooked the same dish at home.
Evaluation instruments
We assessed changes in cooking confidence and related outcomes using a survey pre- and post-class. In the survey, participants were asked to indicate their agreement with twelve statements about cooking attitudes and confidence in various cooking skills. The post-class survey included six additional questions about enjoyment, learning and confidence reducing food waste. Food insecurity was assessed using a validated two-item food insecurity screening tool(Reference Hager, Quigg and Black34).
Post-class interviews were conducted over the phone 2–4 months after the class with a subset of participants. Interviews lasted approximately 15 min and followed a semi-structured interview guide. Participants were called in a random order until three participants from each class had been interviewed. Individuals who completed the interview received a $30 gift card to a local supermarket.
Survey analysis
Agreement with each statement was coded on a score of one to five, with one indicating ‘Strongly Agree’ and five indicating ‘Strongly Disagree’. Data were pooled across all six classes. Differences between pre and post scores for each item were assessed using paired t tests. Analysis was conducted in 2020 using Stata, version 15.
Follow-up interview analysis
Audio recordings from the phone interviews were transcribed verbatim by a professional service. Spanish transcripts were translated into English prior to analysis. The interviews were coded using an inductive, iterative process to define codes based on a line by line reading of the data, and transcripts were revisited as new codes were added. The Dedoose online qualitative data analysis platform was used to facilitate coding and analysis.
Results
Focus group participants
A total of thirty-eight individuals participated in the focus groups, twenty two participated in the two Spanish groups and sixteen participated in the two English groups. Characteristics of the focus group participants are presented in Table 1. The mean age of participants was 48·3 ± 15·8; however, English speakers tended to be older (62·6 ± 14·5) compared with the Spanish speakers (mean age= 39·3 ± 8·9). English speakers also tended to be more highly educated than Spanish speakers (69 % of English speakers had at least some college compared with 18 % of Spanish speakers). Overall, 66 % of participants identified as Hispanic/Latino, 13 % were white and 8 % were black. The majority of participants were female (84 % overall, 91 % among Spanish speakers and 75 % among English speakers). None of the English speakers had children under 18 in their household, compared with 73 % of Spanish speakers. Among English speakers, 31 % reported cooking dinner 5–7 times a week, compared with 86 % of Spanish speakers.
Table 1 Focus group participant demographics

CHASS, Community Health and Social Services Center.
Focus group results
Participants identified barriers to shopping for food and cooking healthy meals, especially trade-offs between quality, cost and convenience of food, presented in Table 2. Other prominent challenges included chronic disease management, difficulty satisfying preferences of family members and lack of time and interest. Many participants self-identified as ‘good cooks’ but lacked confidence preparing unfamiliar foods. Participants expressed great enthusiasm for more cooking and nutrition programming for patients at the CHC and offered numerous ideas for cooking class themes/content.
Table 2 Focus group themes and key quotations.
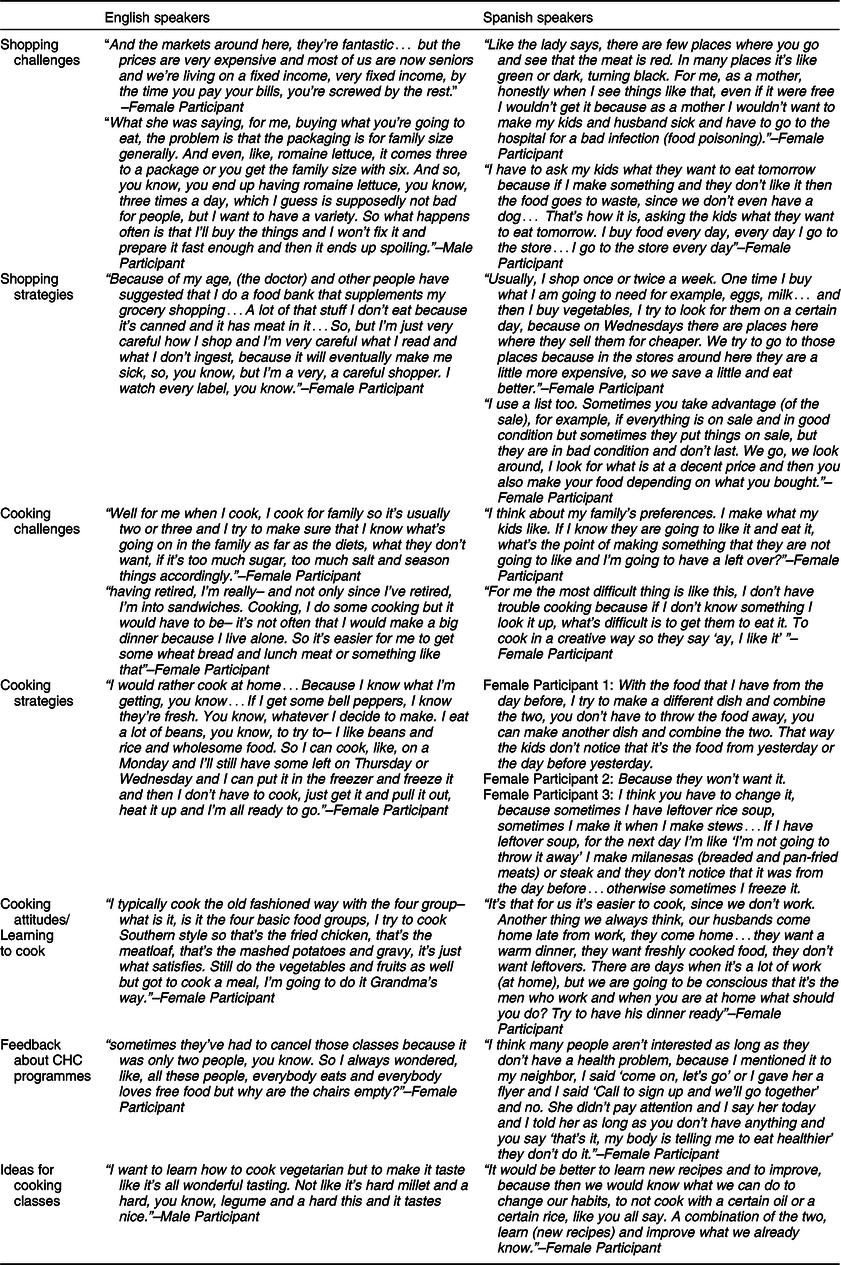
CHC, community health centre.
While both the English- and Spanish-speaking participants expressed that they needed to learn more about healthy cooking, there were also clear differences in the way the Spanish-speaking participants approached food shopping and cooking compared with the English-speaking participants. For example, the Spanish-speaking participants tended to cook and shop frequently and generally considered themselves good cooks. However, they were more comfortable cooking familiar dishes and focused on cooking traditional foods that they knew their children would like. Spanish-speaking participants tended to cook for their children and spouses, making family preferences and health concerns a top priority in food decisions. Lack of time for cooking or difficulty preparing food due to health conditions were more common challenges among the English-speaking participants. English-speaking participants tended to live alone or with an adult sibling and were more interested in strategies to more efficiently prepare meals for just one or two people. Both groups valued traditional cooking and homecook expertise, describing traditional Mexican cuisine, ‘grandma’s way’ and ‘Southernstyle’ cooking.
While Spanish speakers tended to shop more at local supermarkets, whereas English speakers shopped at chain supermarkets, both groups discussed food access issues including distance to chain supermarkets and high prices and/or low quality of produce and meat in local supermarkets and convenience stores. Both groups agreed that healthy ingredients were more expensive and that money-saving strategies such as buying foods on sale or in bulk often resulted in wasted food. Another common challenge was reading nutrition labels and applying nutrition recommendations – especially recommendations related to chronic disease management – in shopping and food preparation.
Cooking class participants
A total of forty-five individuals participated in the cooking classes, 24 participated in a class taught in Spanish and 21 participated in a class taught in English (Table 3). Characteristics of the cooking class participants are presented in Table 3. The mean age of participants was 48·8 ± 15·0, and age distribution was similar between English groups (47·8 ± 18·0) and Spanish groups (49·8 ± 11·9). Overall, 69 % of participants identified as Hispanic/Latino, 24 % were black and 7 % were white. The majority (87 %) of participants were female; 19 % of English speakers had children under 18 in their household, compared with 88 % of Spanish speakers. Thirty-seven percent of participants reported an annual household income <$10 000. Over half of participants (54 %) were food insecure and 14 % were receiving Supplemental Nutrition Assistance Program benefits.
Table 3 Cooking class intervention participant demographics.
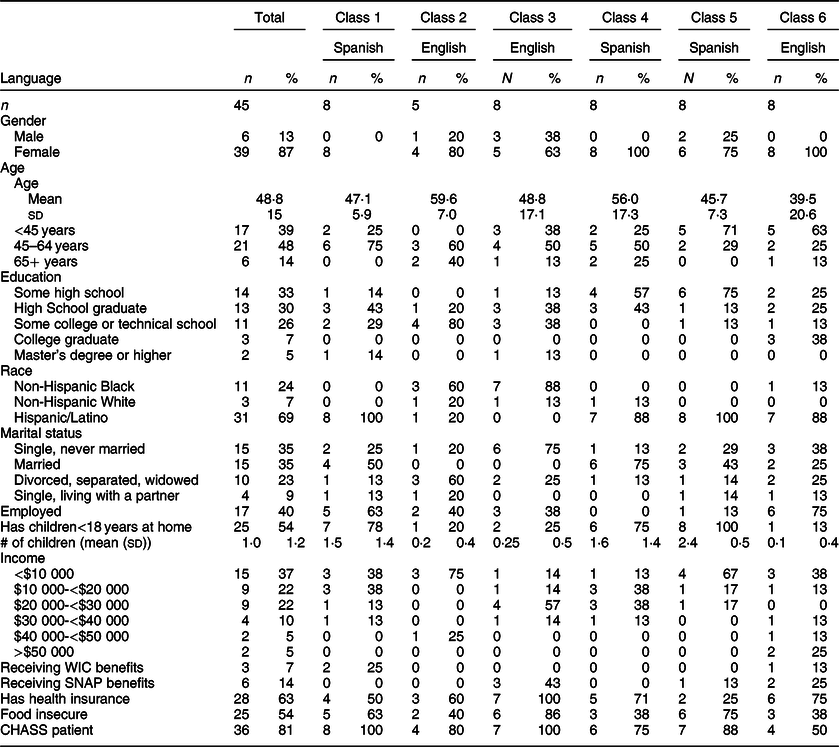
SNAP, Supplemental Nutrition Assistance Program; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; CHASS, Community Health and Social Services Center.
Survey and interview results
Mean baseline scores for a number of cooking confidence measures were high (Table 4). However, participants indicated improved confidence in cooking (P 0·004), experimenting with new ingredients (P 0·006) and knowing how to make use of food before it goes bad (P 0·017).
Table 4 Cooking class intervention results.
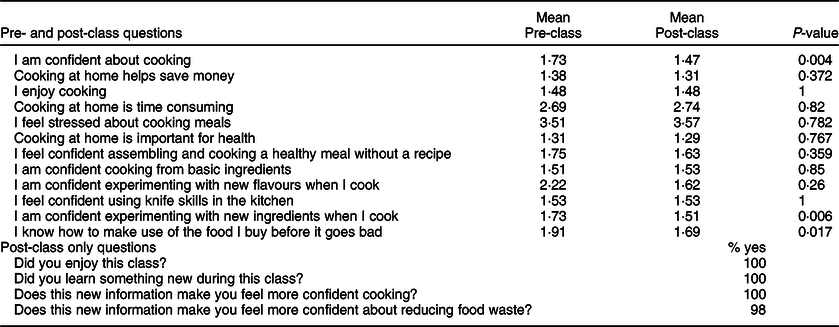
Note: Analyses based on two-sided paired t tests.
In post-class interviews, participants identified that they valued the participatory format and fellowship with classmates and that they had used the recipes and cooking techniques at home. They enjoyed the hands-on component of the class because it was engaging and gave them the opportunity to practice new skills and experiment with new ingredients, with guidance from the instructor. Participants valued the social interaction and sense of community in the class; they enjoyed working together with classmates, discussing different ideas and variations to the recipe while cooking, and sitting down to eat a meal together at the end of class. Managing diet-related chronic diseases for self or family members was the most common motivator for attending the class. Another motivator was learning how to prepare healthier meals in general.
“Oh yes, I mean pickling and I tell you that seasoning and how to put it in the oven, don’t fry it, you know what I mean, instead of frying. Yeah, I learned a lot of things, Because of vegetables like with the market, it was so convenient because I could get the vegetables regular, you know and then try another recipe, make something different and it would help me …”–Female Participant, Class 2, English
“I loved it…I even made it last Thursday, I make it once a week. My kids loved it, my son loved the Tofu tacos, which I didn’t even know…The soy that I know and I’ve always known is the one that is dry. And my kids loved them, they tell me, ‘Mommy, make those tacos because I loved them,’ and I’m like ‘Okay!’ He loved them and my husband too, I bought two boxes because one is not enough. ”–Female Participant, Class 1, Spanish
Discussion
This study demonstrated the feasibility of developing and implementing a community-tailored, Food Agency-based cooking skills intervention at a CHC. Participants valued the participatory format and opportunity for social interaction, highlighting community building as a potentially important secondary outcome of cooking programmes. Furthermore, we characterised multiple barriers to cooking in a low-income, urban community, contributing to a growing body of research on cooking as a health behaviour important not only for diet quality, but for addressing food insecurity as well. Findings from this study demonstrate an important role that CHC located cooking interventions can play in addressing known barriers to healthy eating among their patient populations.
This study highlights the opportunity to use a hands-on cooking programme as an effective way to engage patients at a CHC while also encouraging healthy eating and providing skills to mitigate food insecurity. The short, pilot intervention resulted in significant improvements in cooking confidence in multiple domains and was an effective way to engage patients at the CHC. CHC are typically located in underserved, low-income neighbourhoods and specialise in providing culturally sensitive, community-based services. As of March 2020, CHC served over 29 million patients in the USA, 68 % of whom were at or below the National Poverty Level(35). Food insecurity is prevalent among CHC patients and is associated with poorer health status compared with that of food secure CHC patients(Reference Alvarez, Lantz and Sharac11). While some CHC facilitate enrollment in federal nutrition assistance programmes, not all food insecure clients are eligible for these programmes and for those who are eligible, benefits received may be insufficient to ensure consistent access to safe, nutritious, culturally acceptable foods(Reference Alvarez, Lantz and Sharac11,Reference Andreyeva, Tripp and Schwartz36) .
Findings from our formative focus groups were consistent with previous studies showing heterogeneity in cooking attitudes and behaviour across and between socio-demographic groups(Reference Wolfson, Bleich and Smith18). In this study, Hispanic participants tended to be married mothers who enjoyed cooking and considered themselves to be good cooks but found it challenging to prepare healthy meals that met the preferences of their children and spouses. English-speaking participants tended to be unmarried seniors on a fixed income who did not enjoy cooking as much and found it difficult to shop and cook efficiently when preparing meals for one person. Both groups described issues related to food access, food waste, understanding nutrition labels and applying nutrition recommendations for chronic disease management in meal preparation. These findings support an emerging body of literature demonstrating that facilitators and barriers to home cooking are complex and highly dependent on individual, social, cultural and geographical contexts. Focus groups were an effective way to understand community-specific barriers to cooking and to inform programme development.
We found that a community-tailored cooking intervention was feasible to develop and implement using a CBPR approach. While CBPR is a recognised and increasingly utilized tool for programme development at CHC and other settings(Reference Freedman, Choi and Hurley9,Reference Castañeda, Giacinto and Medeiros27,Reference Wallerstein and Duran31) , literature on CHC located cooking interventions is limited. CHC cooking programmes tend to be supplementary activities, for example, as part of cancer prevention, nutrition education or diabetes management programmes(Reference MkNelly, Nishio and Peshek8,Reference Castañeda, Giacinto and Medeiros27,Reference Liebman, Heffernan and Sarvela37) and thus programme theory rarely focuses on cooking-specific elements. Castañeda et al(Reference Castañeda, Giacinto and Medeiros27) used a CBPR approach to develop and evaluate the acceptability, feasibility and health behaviour impacts of a community-tailored cooking intervention as part of a breast cancer-focused health literacy programme at a CHC. The intervention, which included cooking demonstrations, was feasible to implement and acceptable to participants, and participants valued the social aspect of the programme. Social support and culturally appropriate materials were also highlighted as contributors to successful implementation of Supplemental Nutrition Assistance Program Education, sometimes including a cooking-related component, at twelve Federally Qualified Health Centers in California(Reference MkNelly, Nishio and Peshek8). Our findings are consistent with these prior studies and contribute to a growing body of literature demonstrating the utility of CBPR in programme development, the importance of community-tailored approaches to cooking education, the value of social support in cooking interventions and the appropriateness of CHCs as a venue for cooking education.
The Food Agency-based approach with a focus on active participation, flexible recipes, experimentation with taste and flavours and emphasis on organisation or mise en place is a unique approach that should be replicated in larger studies with control groups and longer term follow-up periods. Participants in this intervention, as is common with numerous cooking skills interventions(Reference Pooler, Morgan and Wong4,Reference Reicks, Trofholz and Stang24) , were already confident cooks who enjoyed cooking and were interested in learning new skills. The Food Agency approach was successful at engaging these individuals and still provided them valuable new skills and approaches for more efficient, healthy cooking. The discussions throughout the course and during the shared meals at the end were valuable for allowing participants to consider how to apply the approaches emphasised during class in their daily lives and allowed them to learn from each other as well as from the expertise of the instructors.
The outcomes of our cooking intervention are consistent with a limited number of studies showing modest but significant improvements in cooking confidence. In a recent review, among seven studies that assessed cooking confidence as an outcome, cooking interventions were generally associated with improvements in self-reported cooking confidence immediately after the intervention and/or at 3–6 month follow-up(Reference Reicks, Kocher and Reeder5). However, specific outcome measures varied, not all results were statistically significant, and not all improvements were maintained after a longer follow-up period. A previous review also found that three studies demonstrated increased cooking confidence 1–6 months post-intervention(Reference Reicks, Trofholz and Stang24). Cooking interventions are generally challenging to compare due to substantial variation in programme design, target population and outcomes assessed and the majority of programmes lack a theoretical basis for design and evaluation(Reference Reicks, Kocher and Reeder5,Reference Wolfson, Bostic and Lahne6,Reference Reicks, Trofholz and Stang24) .
To our knowledge, ours is the first study to assess food waste as an outcome of a cooking intervention. Multiple cooking strategies for reducing food waste were introduced in the cooking class including quick pickling to extend storage of vegetables, flexible recipes to encourage use of available ingredients and discussion of storing produce to maximise shelf-life. We observed a significant improvement in ‘knowing how to make use of food before it goes bad’ immediately post-intervention. Even in programmes focused on food resource management, primarily the Cooking Matters curriculum, food resource management learning objectives are largely related to shopping, meal planning and general ability to ‘make low-cost meals’, not specific cooking strategies(Reference Pooler, Morgan and Wong4). Furthermore, although assessment of food resource management has been based on ‘frequency with which respondents engaged in behaviours to maximise food resources’ and self-confidence in these activities, outcomes related to food waste are not assessed. Given that food waste is known to be a significant concern among low-income and/or food insecure households, cooking programmes to improve food security should expand on the current teaching and assessment of food resource management to incorporate food waste reduction activities.
This study has several limitations. First, the study was conducted in a low-income, urban neighbourhood in Southwest Detroit with a large Hispanic population; therefore, generalisability, particularly to non-urban settings or to other ethnic populations, may be limited. Second, participants self-selected into the focus groups and cooking classes by responding to flyers or were specifically invited by providers or CHW. Participants targeted by CHW may have been engaged in other programming at the CHC that influenced their food and cooking behaviours and biased their perception of the CHC, such as nutrition counselling or regular primary care. While the flyers encouraged interest from anyone interested in learning about cooking, regardless of current cooking skills, most participants in the focus groups were interested in the topic, enjoyed cooking and considered themselves to be ‘good cooks’. Third, our evaluation lacked a control group or randomisation. Additionally, the sample size for the intervention component of the study was limited due to available funding and room capacity in the teaching kitchen. Due to a high number of confirmed participants who did not attend the cooking classes, sample size was further reduced which limited the statistical power of this study and contributes to potential self-selection bias. We did not follow-up with individuals who signed up for the classes, but then failed to attend the classes to determine whether there were differences between those who did and did not participate in the intervention. Future interventions may provide the opportunity to follow-up with no-show participants in order to understand why some individuals fail to attend the class and how to facilitate greater participation and retention. CHW called all participants to confirm attendance the day before the cooking class; however, future research or programming should incorporate additional strategies to maximise attendance. Fourth, exposure to the intervention was a single class, due to preferences expressed by the steering committee. Future iterations of this intervention could expand to offer a series of classes. Fifth, changes in cooking skills and behaviour were based on self-report, and the follow-up period was short. It is unclear whether improvements in cooking confidence indicated in the post-class survey were representative of lasting behaviour change, although participants did report modest behaviour change in the follow-up interviews 2–4 months post-intervention. Relying on self-reported outcomes may lead to social desirability bias, including bias from patients who are ‘loyal’ to the CHC and thus want to reflect positively on CHC programming. Further research with longer follow-up is needed to explore more objective methods of measuring cooking skills and confidence. Finally, although our intervention highlighted nutritious ingredients and healthier cooking methods, we did not assess outcomes related to diet quality in this study which is an important area for future research.
Conclusion
Findings from this study highlight the opportunity to engage CHC patients in cooking education as part of an integrated approach to improving food security and diet quality, as well as the challenge of developing CHC programmes that are inclusive and sensitive to the needs of a diverse patient population. Further research is needed to evaluate Food Agency-based approaches to cooking education in larger studies with control groups, longer follow-up periods and more comprehensive assessment of outcomes.
Acknowledgements
Acknowledgements: The authors would like to thank Martha Ruiz and Jesus Cohen for their contributions to the pilot intervention and follow-up interviews and Kimberly Fitzgerald, who contributed to the formative focus groups. Financial support: Funding for this study was provided by a Community-Academic Partnership Grant from the University of Michigan Poverty Solutions and the University of Michigan Detroit Urban Research Center. J.A.W. was also supported by the National Institutes of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (Award #K01DK119166). Conflict of interest: There are no conflicts of interest. Authorship: J.A.W., D.P., R.B., C.R. and T.G. contributed to the conception and design of this work. Data were collected by T.G., B.F. and J.A.W. and were analysed by J.A.W. and T.G. J.A.W., T.G., R.B. and D.P. contributed to the interpretation of the results. The first draft of the manuscript was written by T.G. and J.A.W., and all authors contributed to critical revision of the article and approved the final version to be published. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the University of Michigan Institutional Review Board. Written informed consent was obtained from all subjects/patients.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020003511.
Appendix A

Appendix Fig. 1 Study design
Appendix Table 1. Focus group discussion guide