Breast-feeding is the optimal nutrition for infants and is recommended as an exclusive diet for the first months with subsequent partial breast-feeding along with age-appropriate complementary food(1–Reference Koletzko, Bauer and Brönstrup3).
Advantages of breast-feeding are manifold for infants, mothers and the society. Being breastfed protects against infant mortality and morbidity from infectious diseases such as diarrhoea and pneumonia(Reference Horta and Victora4) and may decrease the risk for overweight and diabetes later in life(Reference Victora, Bahl and Barros5,Reference Horta, Loret de Mola and Victora6) . Breast-feeding also decreases the mother’s risk of developing breast and ovarian cancer(Reference Victora, Bahl and Barros5,Reference Babic, Sasamoto and Rosner7) .
Breast-feeding offers economic and environmental benefits to society through reduced costs of preventable diseases(Reference Walters, Phan and Mathisen8,Reference Rollins, Bhandari and Hajeebhoy9) and a lower carbon footprint compared to breastmilk substitutes(Reference Karlsson, Garnett and Rollins10). Breast-feeding is convenient and cost-efficient.
Thus, protection, promotion and support of breast-feeding is an impetus worldwide(Reference Agostoni, Braegger and Decsi2,11,12) . To get breast-feeding started successfully, WHO and UNICEF initiated the programme of the ‘Ten Steps to Successful Breastfeeding’ in 1989(13,14) . The Baby-friendly Hospital Initiative (BFHI) is based on the adherence to the Ten Steps and has been shown to be effective at improving breast-feeding outcomes globally(Reference Pérez-Escamilla, Martinez and Segura-Pérez15). To measure breast-feeding promotion and support on infant feeding practices within and among countries, indicators were suggested referring to initiation, exclusivity and duration of breast-feeding(16,17) . Based on these international recommendations, the German National Breastfeeding Committee (NSK) developed recommendations for breast-feeding promotion in hospitals in 1998(18) as well as definitions of breast-feeding status adapted to conditions in Germany in 1999(19), both updated in 2007(18,19) .
A European action plan, presented in 2004 and updated in 2008, called for standardised breast-feeding monitoring, defined as the systematic assessment of current, comprehensive and precise data on breast-feeding rates and behaviour at a national and regional level(20). Subsequently, in Germany, the NSK presented an integrative concept of breast-feeding monitoring comprising different levels of structured assessments of breast-feeding as a basis for quality assurance of promoting activities for breast-feeding(21,Reference Sievers, Weikert and Weißenborn22) .
To systematically collect data on breast-feeding promotion in hospitals providing maternity services and on subsequent breast-feeding rates, two nationwide surveys named ‘SuSe’ (an abbreviation for ‘Stillen und Säuglingsernährung in Deutschland’ to be translated as breast-feeding and infant nutrition in Germany) were conducted in Germany 20 years apart with SuSe I 1997–1998(Reference Kersting and Dulon23,Reference Dulon, Kersting and Bender24) and SuSe II 2017–2019(Reference Kersting, Hockamp and Burak25). The specific study design was essentially maintained and WHO/UNICEF and NSK definitions were applied in both surveys, allowing comparisons of study results.
The objective of this work is therefore to provide an insight into the development of breast-feeding in Germany over a period of 20 years.
Methods
Study structures
The SuSe study design is a combination of a cross-sectional survey on breast-feeding promotion and support in hospitals providing maternity services and a subsequent prospective survey of breast-feeding and infant nutrition during the first year of life in mother–infant pairs who were recruited in the participating hospitals. In SuSe I (1997–1998) and SuSe II (2017–2019), a similar design has been applied. The methodological approach and assessment details were retained as far as possible. However, some modifications had to be made in SuSe II.
The basic population in both studies was the total number of hospitals providing maternity services in Germany, hereinafter referred to as hospitals. The basic population from which the mother–infant samples were drawn were mothers who delivered in the participating hospitals during a pre-defined 2-week period. The mother–infant samples were prospectively followed up from birth for the first year of life with five (SuSe II) or six (SuSe I) assessments on breast-feeding and infant nutrition during the first year of life.
The change in communication modes particularly in the young parent population between the two studies suggested a switch from paper and pencil postal questionnaires and phone calls in SuSe I to web-based questionnaires in SuSe II. The web-based assessment tool was developed and applied by the Fraunhofer Institute for Software and Systems Engineering ISST, Dortmund.
SuSe I was carried out at the former Research Institute of Child Nutrition in Dortmund (Germany), SuSe II at the successor institution, the Research Department of Child Nutrition of the Pediatric Clinic at the University of Bochum (Germany). Obligatory for participation in both studies was the written informed consent of hospitals and mothers.
Recruitment
Hospitals
In SuSe I, a random sample of 360 hospitals was invited from the total of German hospitals (n 1120) in a randomised sequence, while all hospitals (n 712) were invited in SuSe II. In both studies, the chief physicians were invited by postal letter. In case of missing feedback, hospitals were reminded with phone calls (SuSe I + II) and additionally by fax and a video invitation from the study head (SuSe II).
In both studies, the ward staff filled out a ‘hospital’ questionnaire about their breast-feeding promotion and support practices and supported the recruitment of mothers for the follow-up survey. The chief physicians were requested to name a responsible person at the maternity ward as contact person for the study team. Within a 3-month window (SuSe I: March–May 1997, SuSe II: January–March 2018), each participating hospital was allocated to a pre-specified 2-week period for recruitment of mothers and parallel questionnaire completion.
As a recognition of their participation, hospitals in SuSe I received brochures on breast-feeding and infant nutrition published by the Research Institute of Child Nutrition. In SuSe II, they were offered an in-house training on infant feeding or on pregnancy lifestyle provided by the German ‘Healthy Start – Young Family Network’ at the Federal Centre for Nutrition (BZfE)(26).
Mother–infant pairs
During the recruitment period, the hospital ward staff was requested to document selected basic information of all births consecutively with documentation forms (SuSe I: n 4352; SuSe II: n 3810). Inclusion criteria were a healthy, full-term newborn (birth weight ≥ 2500 g, gestational age ≥ 37 weeks, no admittance to a neonatal intensive care unit) and sufficient maternal knowledge of the German language as assessed by the staff, the existence of a telephone (SuSe I) and internet access as well as an email address (SuSe II). Written study information including a consent form was handed out to mothers meeting the inclusion criteria on the ward (SuSe I: n 3294; SuSe II: n 2831). Written consents were collected by the staff and sent to the study team or sent by the mothers after they left the hospital (SuSe I: n 1851; SuSe II: n 1168). As a reward for their participation, mothers in SuSe I received a brochure with recommendations for child nutrition. They were not informed about this reward in advance but received the information with a letter of thanks upon receipt of the last questionnaire 12 months postpartum (pp). Mothers in SuSe II received health messages via email during the first year of life, a financial compensation of 30 euros and a brochure with recommendations for child nutrition at the end of the survey. Mothers in SuSe II were informed at the time of recruitment about these rewards to appeal in particular to mothers difficult to motivate for participation in trials.
Data collection
Questionnaires
The hospital questionnaire mainly inquired about breast-feeding support practices based on the WHO and UNICEF Ten Step programme, modified for Germany(13,14,18) . The steps were not directly named in the questions, for example, ‘Do you have policies for breast-feeding promotion on the ward?’ (answer options: yes/no), ‘In what form do the policies on breast-feeding promotion exist?’ (answer options: written policies/verbal agreements). For several steps, specifications were modified in SuSe II to increase the actual relevance of the answers (see results). In addition, characteristics of the hospital, for example, numbers of births in the last year, certified as ‘baby-friendly’ by the WHO/UNICEF BFHI were collected from hospitals.
The survey tools for hospitals (hospital questionnaire, documentation form) were tested in both studies in a pilot study in large local hospitals.
During the follow-up survey in both studies, mothers were asked at the infant’s age of 2 weeks and 2, 4, 6 and 12 months and in addition at the age of 9 months in SuSe I. In SuSe I, the 2-week assessment was carried out by phone 12 to 16 d pp and the following five assessments by 1-page postal dietary records with a deadline of 2 weeks (± 2 to 4 d). In SuSe II, assessments were web-based, that is, questionnaires were sent by email. Within the first 2 weeks, an additional phone call was planned to motivate the mothers to participate; about 200 mothers were reached by phone. The mothers had a time frame of 4 weeks to answer the first four questionnaires (2 weeks, and 2, 4 and 6 months). In both studies, the 2-week questionnaire assessed the infant feeding practices retrospectively during hospital stay and at discharge and the infant’s diet at present. Additionally, maternal characteristics were assessed at this point. The four follow-up questionnaires on current infant nutrition after the age of 2 weeks were the same until the age of 12 months. For answering the last questionnaire, a general deadline was set 3 weeks after the last questionnaire was sent. A more detailed assessment of infant feeding except breast-feeding was possible with the web-based version of the SuSe II tool. In case, the breast-feeding status had changed since the previous questionnaire by adding other fluids or food, mothers were asked in a separate short ‘weaning’ questionnaire about their reasons for additional feeding other than breast-feeding and about the total duration of exclusive and total breast-feeding. The dietary reporting referred to the current nutrition, for example, ‘How many breastmilk feedings does your child receive?’ (answer options: during the day/night: none, 1, 2, 3, 4 or more), ‘Does your child receive additional liquids (juice, water, tea, other)?’ (answer options: yes/no).
The maternal questionnaires were tested in local pilot studies with mothers recruited in a paediatric practice in SuSe I and in hospitals in SuSe II. In SuSe I, each incoming questionnaire was checked for completeness, and implausible or missing information was clarified by telephone inquiries. In SuSe II, the pilot study focused on testing the functioning of the online tool, since the comprehensibility of the questions had already been tested in SuSe I.
Assessment of breast-feeding
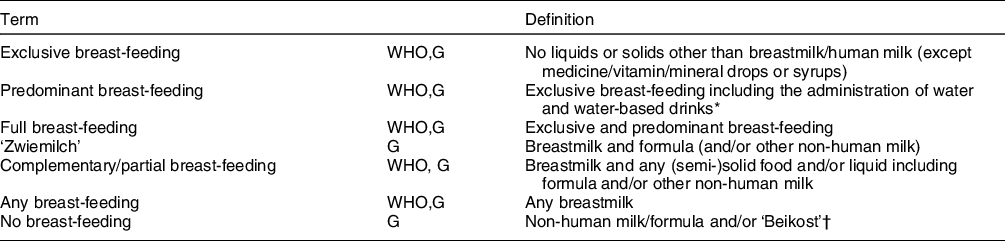
For the dietary questions, mostly pre-specified answers had to be selected. Initially, mothers reported the number of meals at daytime and nighttime for breastmilk, allowing for defining breast-feeding ‘yes’ or ‘no’. Subsequently, other milk feedings (e.g. formula and cow’s milk), non-milk fluids (e.g. water, tea, and juice) and other liquids (e.g. plant drinks) or (semi-)solids (complementary feeding, ‘Beikost’) given to the infant had to be indicated. These specifications allowed to define the infant feeding category according to the definitions given by WHO(16,17) and for Germany(19) (Table 1).
Data presentation
Data analysis was performed using the IBM® SPSS® Statistics Version 25.0 software package for Windows 2016 (IBM Corp.). Percentages for categorical variables or frequencies for continuous variables were used for data description. To determine differences between characteristics of participants, the exact test according to Fisher for categorical data and the Mann–Whitney U test for non-normally distributed continuous data were used. P-values <0·05 (two-sided) were considered to be significant. Continuous data were tested for normal distribution using the Kolmogorov–Smirnov test.
Results
Recruitment of hospitals and mother–infant pairs
An overview of the recruitment and the samples of hospitals and mothers in both studies is shown in Fig. 1. In 2017 (SuSe II), not only was the number of hospitals in Germany smaller, but also the participation rate of the hospitals was lower than in 1997 (SuSe I) (15·8 % v. 51·3 %) and less deliveries were recorded during the recruitment periods. In both studies, about half of the reasons for exclusion concerning the infant (birth weight < 2500 g, gestational age < 37 weeks and admittance to a newborn intensive care unit) and the other half concerned the mother (no sufficient knowledge of the German language, no telephone (SuSe I + II), no internet access and no email address (SuSe II)). In SuSe I, 1·7 % of mother–infant pairs could not be enrolled in the study due to a delayed arrival of their consent forms at the study centre. The participation rate of the mothers was lower in SuSe II compared to SuSe I (34·0 % v. 52·1 %), but in both studies, about 90 % of participating mothers attended the follow-up until the last survey 12 months pp.
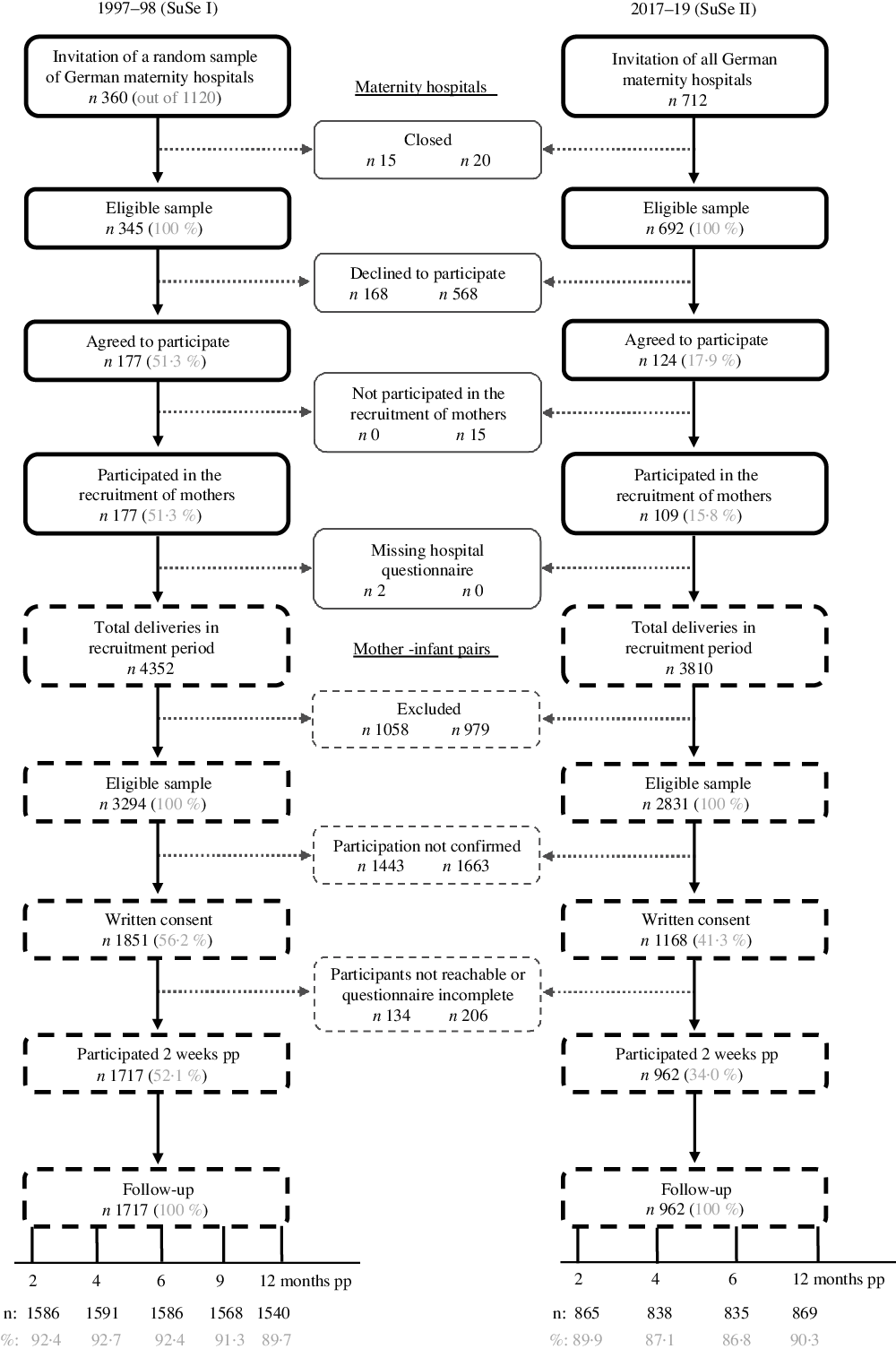
Fig. 1 Flowchart of recruitment and participation in 1997–1998 (SuSe I) and 2017–2019 (SuSe II); pp, postpartum
Hospitals
Hospital characteristics
The majority of hospitals in SuSe II were academic, while most hospitals in SuSe I were operated by public institutions (Table 2). The mean number of births per hospital per year and the percentage of caesarean sections were almost twice as high in SuSe II compared to SuSe I. In both studies, a similar number of maternity beds were available on the ward, but the average hospital stay was 2 d shorter in SuSe II. The number of hospitals certified as ‘baby-friendly’ and the availability of lactation consultants on the wards increased considerably over the last 20 years, while the availability of midwives was similar in both studies. In comparison with the respective reference group of all German hospitals, both study samples did not differ with regard to the annual birth rate(27,28) and regional distribution between the former politically separated parts of Eastern and Western Germany.
Table 2 Hospital characteristics in 1997–1998 (SuSe I) and 2017–2019 (SuSe II)
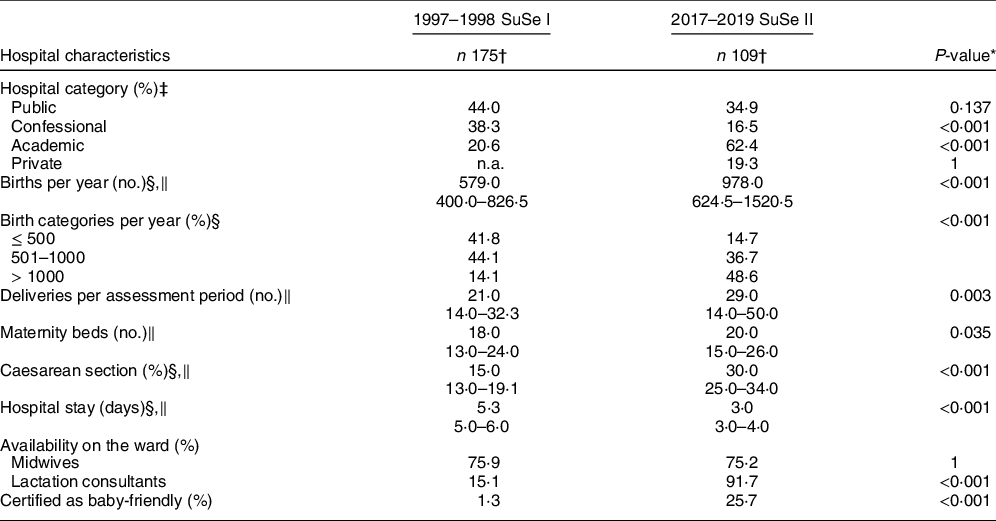
n.a., not asked.
* Fisher’s exact test for categorical variables, Mann–Whitney U test for non-normally distributed continuous variables; P values <0·05 were considered to be significant.
† SuSe I: n 177 for births/birth categories per year; n 174 for deliveries per assessment period; n 171 for number of maternity beds; n 170 for days of hospital stay; n 166 for caesarean section; n 174 (172) for the availability of midwives (lactation consultant) on the ward; SuSe II: n 107 for deliveries per assessment period.
‡ Multiple answers possible.
§ In 1996 for SuSe I; in 2016 for SuSe II.
‖ Median and 25th–75th interquartile range.
Breast-feeding promotion and support in hospitals
The recommendations of the Ten Steps were implemented to a varying extent by the hospitals in both studies (Table 3), ranging between 9·7 and 96·0 % of hospitals in SuSe I and 47·7 and 98·2 % in SuSe II. In SuSe II, more than 90 % of the hospitals gave mothers breast-feeding instructions and documented them (Step 5), stated that most mothers practised 24-h rooming-in (Step 7) and encouraged breast-feeding on demand or at least 8–10 times within 24 h without a fixed schedule (Step 8). Hospitals in SuSe II implemented seven steps to a greater extent than hospitals in SuSe I. Great improvements in the last 20 years were mainly observed in structural characteristics such as Step 1 (written breast-feeding policy (and breast-feeding coordinator)), Step 2 (regular training of health care staff), Step 5 (breast-feeding instruction and documentation) and Step 9 (alternative feeding methods). There was a deterioration compared to SuSe I in Step 3 (breast-feeding information) and Step 4 (first initiation of breast-feeding). Step 10 (breast-feeding support group) remained at a similar level. The response options for Step 1 and 8 were updated to the recent German recommendations. For Step 1, in addition to the written breast-feeding policies in SuSe I, a breast-feeding coordinator on the ward had to be present in SuSe II. For Step 8 (breast-feeding on demand), additional options (at least 8/10 times per 24 h without a fixed schedule) were provided. For Steps 3 and 7, hospitals in SuSe II had a single answer option in contrast to multiple choices in SuSe I. Initiation of breast-feeding (Step 4) was asked separately by type of delivery in SuSe II and uniform in SuSe I. Hospitals in SuSe II received a positive rating only if they enabled initiation within the first hour of life for both types of deliveries.
Table 3 Breast-feeding promotion and support in hospitals according to WHO(13,14) and German (G)(18) recommendations and as applied in the SuSe studies
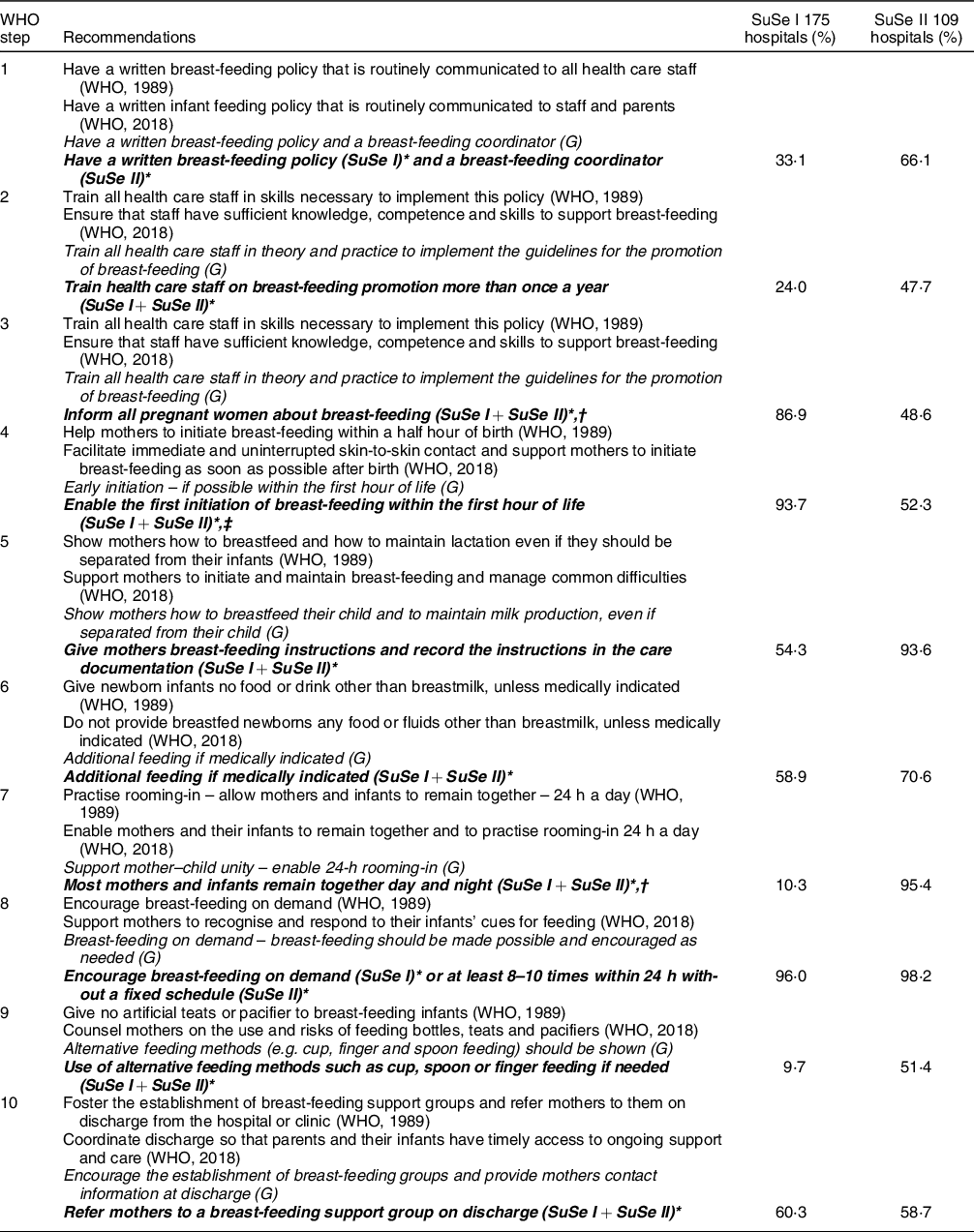
Italic: Breast-feeding promotion and support in hospitals according to German recommendations. Bold italic: Breast-feeding promotion and support in hospitals applied in the SuSe studies.
* SuSe I: assessment in 1997; SuSe II: assessment in 2018.
† Multiple answers possible in SuSe I, single choice in SuSe II.
‡ Not separated by type of delivery in SuSe I, separated by type of delivery in SuSe II and positive rated, if fulfilled for both.
Mother–infant pairs
Characteristics
Characteristics of participating mother–infant pairs of both studies are presented in Table 4. Mothers in the recent study were on average older and better educated than mothers in the previous study. With regard to the mode of delivery, the rate of caesarean section approximately doubled; the average length of hospital stay, however, was about 2 d shorter. There were no differences in the infant characteristics gender and birth weight. Compared to mothers eligible to participate, actual participating mothers in both studies were older, had a higher school education and were more often German citizens. Compared to national statistics, study participants (SuSe II) were older (35–39 years: 29·1 % v. 20·2 %) and better educated (higher secondary education: 65·5 % v. 43·5 %), and their postnatal stay in the hospital was longer (3–6 d: 81·5 % v. 67·6 %), but the rate of caesarean section was higher (31·3 % v. 24·7 %)(29,30) .
Table 4 Characteristics of mother–infant pairs in 1997–1998 (SuSe I) and 2017–2019 (SuSe II)
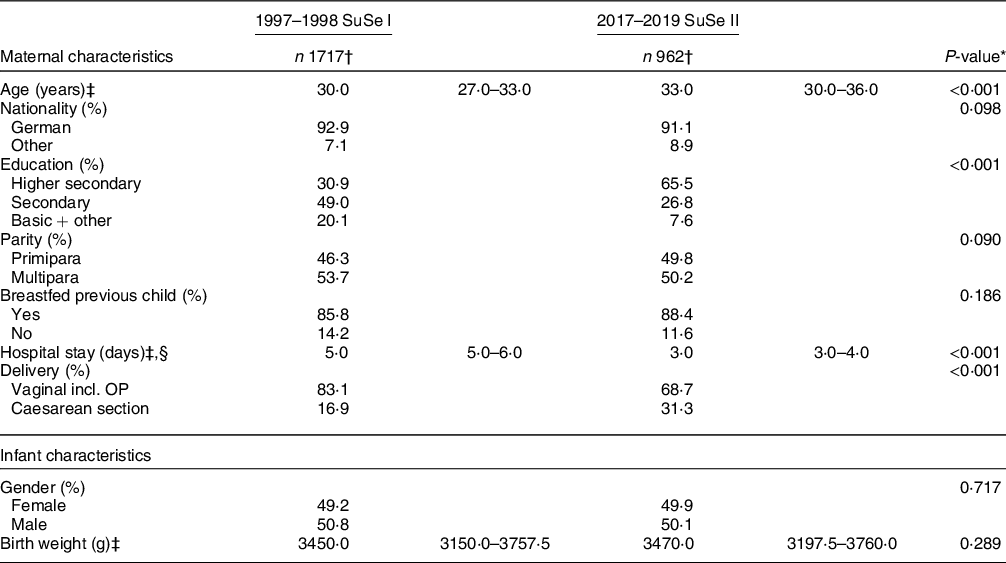
* Fisher’s exact test for categorical variables, Mann–Whitney U test for non-normally distributed continuous variables; P values <0·05 were considered to be significant.
† SuSe I: n 1715 for nationality, n 1706 for school education, n 1716 for parity, n 920 for breastfed previous child and n 1665 for hospital stay (days); SuSe II: n 959 for age, n 955 for school education, n 483 for breastfed previous child and n 940 for hospital stay (days).
‡ Median and 25th–75th interquartile range.
§ Outpatient births excluded.
Breast-feeding prevalence
In SuSe II, 96·6 % of mothers tried to breastfeed after birth, while 90·8 % of mothers tried in SuSe I (data not shown). The rates for exclusive breast-feeding at discharge were similar in both study samples, but thereafter higher in SuSe II than in SuSe I until 6 months pp (Table 5). In the second half of the first year of life, more mothers continued breast-feeding in the recent study with 78 % (41 %) for any breast-feeding at 6 (12) months pp compared to 48 % (13 %) in the previous study. Predominant breast-feeding (breastmilk plus water, tea or fruit juice) played a subordinate role in SuSe II, but breast-feeding plus non-human milk (‘Zwiemilch’) was practised more frequently. With the introduction of complementary foods after the end of the fourth month pp, exclusive or full breast-feeding was replaced by partial breast-feeding in both studies. The rate of mothers who did not breastfeed was about half as high during the first year of life in SuSe II compared to SuSe I.
Table 5 Breast-feeding prevalence for different feeding categories during the first year of life in 1997–1998 (SuSe I) and 2017–2019 (SuSe II) (% of all infants*)
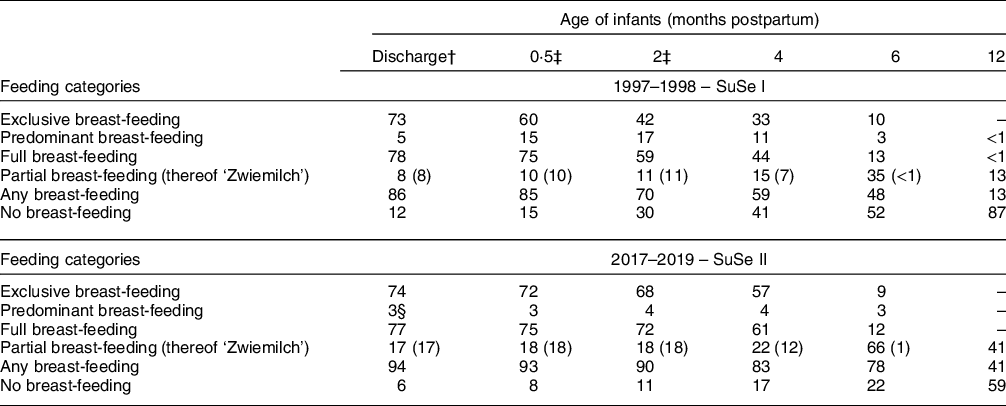
* 1997–1998: n 1717 at discharge and 0.5 months; n 1540–1717 2, 4, 6 and 12 months pp; 2017–2019: n 962 at discharge and 0.5 months; n 835–869 at 2, 4, 6 and 12 months pp.
† Median: 1997–1998: 5 d after birth, 2 % missing (outpatient birth); 2017–2019: 3 d after birth, 0.8 % missing (outpatient birth).
‡ Deviations in SuSe II due to rounding.
§ Breastmilk and other liquids including formula.
Discussion
The two breast-feeding studies, SuSe I and SuSe II, point to an improvement in breast-feeding in Germany over the last 20 years. Since the participation rates of hospitals and mothers were lower in SuSe II compared to SuSe I, it is not possible to distinguish between the potential roles of sample selection or breast-feeding promotion activities for the overall favourable development.
Study design
SuSe I was the first nationwide survey collecting data on breast-feeding promotion in hospitals and prospectively assessing breast-feeding and infant nutrition in the first year of life in Germany. The repetition using a similar study design 20 years later provided an insight into the development of breast-feeding over time. By starting data collection at birth, the breast-feeding continuum from hospital care to family practice was covered. Combined with data on maternal characteristics and attitudes, determinants of breast-feeding could be identified which can serve as a starting point for a tailored breast-feeding support.
The surveys are based on international definitions and recommendations(13,14,16,17) , enabling a comparison of results on an international level. The long-term participation rate of about 90 % in both studies indicates sustained high interest of mothers and the suitability of the study design. The prospective assessment minimised recall bias. In SuSe II, the online approach enabled mothers to answer questionnaires within about 15 min, bypassing the postal mail and eliminating the risk of interviewer bias that might have existed during the phone interviews in SuSe I. On the other hand, no queries could be asked during the online survey in case of problems in understanding the questions. In addition, the study design did not allow for verification of the information provided by mothers and hospital staff.
Participation
A weakness of both studies, in particular of SuSe II, is the low response rate of hospitals and mothers. In both studies, better educated mothers known to be more likely to initiate and maintain breast-feeding were overrepresented(Reference Cohen, Alexander and Krebs31). The hospital sample in the SuSe II study comprised relatively more baby-friendly hospitals (25·7 % v. approx. 15 % currently in Germany)(32). Therefore, the risk of a selection bias towards an overestimation of the breast-feeding friendliness in Germany cannot be excluded.
For hospitals, the additional workload of recruiting mothers could have been a main reason for the low participation rate. The additional work was limited to 2 weeks, working hours remained without compensation to the hospitals. In SuSe II, increased time and budget constrains in hospitals may have further tightened the options to participate in a research study(33).
For mothers, a reason for the lower participation rate in SuSe II could be the shortened hospital stay from 5 d (SuSe I) to 3 d (SuSe II). Due to the intense documentation and information requirements as part of routine care, there may not have been enough time for mothers to think thoroughly about their participation in the study. Whether the incentives for mothers in SuSe II increased their willingness to participate could not be analysed with the available data.
The decline in the response rate in the mother–infant cohorts from 52·1 % in SuSe I (1997–1998) to 34·0 % in SuSe II (2017–2019) is comparable to the German nationwide survey on the health of children and adolescents (KiGGS) with a response rate of 66·6 % in the baseline survey (2003–2006) and 38·8 % and 40·1 % in waves 1 (2009–2012) and 2 (2014–2017), respectively(Reference Kamtsiuris, Lange and Schaffrath Rosario34–Reference Hoffmann, Lange and Butschalowsky36). In two regional studies in Ulm (Germany), response rates also declined from of 67 % (2000–2001) to 49 % (2012–2013)(Reference Logan, Zittel and Striebel37). The Norwegian Mother and Child Cohort Study (1999–2006) and the Swiss Infant Feeding Study (2014) with 43·5 % and 40 % had similar response rates as our study(Reference Nilsen, Vollset and Gjessing38,Reference Gross, Späth and Dratva39) . Thus, the SuSe studies seem to reflect the general decline in willingness to participate in health-related surveys over the past decades(Reference Mindell, Giampaoli and Goesswald40,Reference Galea and Tracy41) .
Breast-feeding promotion and support in hospitals
Hospitals in SuSe II implemented 7 of the 10 Steps of the WHO breast-feeding promotion to a greater extent than hospitals in SuSe I (Steps 1, 2, 5, 6, 7, 8 and 9). The lower figures in SuSe II for Steps 3 and 4 are due to modified response options in the questionnaire. For Step 3 (breast-feeding information), the response mode was changed from multiple answers to a single one to reduce the probability of a socially desired answer. In Step 4 (first initiation of breast-feeding), the requirements for a positive evaluation had to be met for both types of delivery. In addition, the rate of deliveries by caesarean section was higher in SuSe II (30·0 % v. 15·0 %) and theses deliveries are usually associated with later initiation of breast-feeding(Reference Prior, Santhakumaran and Gale42). Steps 5 (breast-feeding instruction and documentation), 7 (24-h rooming-in) and 8 (breast-feeding on demand) were the best implemented steps in SuSe II, similar to a small hospital survey in the USA published in 2012(Reference Taylor, Nickel and Labbok43).
Even though only 25·7 % of participating hospitals in SuSe II were certified as baby-friendly, the implementation rate of the respective recommendations was relatively high in our total sample. Positive effects of WHO/UNICEF certification on breast-feeding outcomes were shown in a systematic review(Reference Pérez-Escamilla, Martinez and Segura-Pérez15) but may differ in individual studies(Reference Robert, Michaud-Létourneau and Dramaix-Wilmet44,Reference Hawkins, Stern and Baum45) . A described dose–response relationship between the number of steps to which women remembered being exposed to and the probability of improved breast-feeding outcomes(Reference Pérez-Escamilla, Martinez and Segura-Pérez15) suggests that even non-certified hospitals with a high level of commitment can provide good breast-feeding promotion, as seems to be the case in the SuSe studies.
Breast-feeding prevalence
With more than 90 %, the rates of mothers in the SuSe studies who tried to breastfeed are in the upper range for breast-feeding initiation in national (72–97 %) and European (56–98 %) comparison(Reference Weissenborn, Abou-Dakn and Bergmann46,Reference Theurich, Davanzo and Busck-Rasmussen47) . However, we cannot rule out the possibility that mothers not willing to breastfeed were left out in the recruitment by the hospital staff. The prospective comparison between the SuSe studies showed higher rates of exclusive breast-feeding and ‘Zwiemilch’ feeding (breast-feeding + non-human milk) until the end of the fourth month pp and any breast-feeding throughout the first year of life in SuSe II.
In a systematic review on breast-feeding data in Germany including 35 single, heterogeneous studies on births between 1990 and 2012, it was not possible to identify clear trends(Reference Weissenborn, Abou-Dakn and Bergmann46). The SuSe II data range in the upper and middle fields for any breast-feeding between 2 and 6 months and were lower for full breast-feeding 6 months pp compared to the review(Reference Weissenborn, Abou-Dakn and Bergmann46). A significant decline in breast-feeding rates within the first 2 months of life described in the review(Reference Weissenborn, Abou-Dakn and Bergmann46) was also observed in SuSe I but diminished in SuSe II.
Slight increases in the percentage of women who partially breastfed or breastfed at all at 6 months were observed in two local studies during 1990–2013(Reference Libuda, Bolzenius and Alexy48) and 2001–2013(Reference Logan, Zittel and Striebel37). In contrast, between 2001–2014, the retrospective nationwide KiGGS study showed a tendency towards a stabilisation of the duration of any and full breast-feeding and a decrease in full breast-feeding duration between 2009/2010–2013/2014(Reference Brettschneider, von der Lippe and Lange49). In the latest KiGGS assessment 2013/2014(Reference Brettschneider, von der Lippe and Lange49), any breast-feeding rates at 6 months (55·9 %) and 12 months (20·3 %) were lower than in SuSe II (78 % and 41 %, respectively). No breast-feeding data closer to the SuSe II period are available in Germany.
Among eleven selected European countries, the rates for any breast-feeding in the SuSe II study range among the high level countries, for example, the rates for any breast-feeding until 6 months pp were 71 % in Norway, 61 % in Sweden and 52 % in Switzerland(Reference Theurich, Davanzo and Busck-Rasmussen47). In contrast, the rate for exclusive breast-feeding at 6 months in the SuSe II study is even lower than in general in the WHO European region (9 % and 25 %, respectively)(50). The decline of exclusive breast-feeding rates between 4 and 6 months pp in SuSe I and II can be explained by the introduction of complementary foods between 4 and 6 months after birth which has been recommended in Germany for more than 20 years(Reference Kersting51).
General interpretation
The comparison of the SuSe studies points to an improvement of breast-feeding promotion and support in hospitals and breast-feeding prevalence during the last 20 years. Slight positive trends, as described in other repeated studies in Germany(Reference Logan, Zittel and Striebel37,Reference Weissenborn, Abou-Dakn and Bergmann46,Reference Libuda, Bolzenius and Alexy48) within almost the same time period, may have become particularly clear in SuSe II as the most recent study.
Hospital environment
Between 2001 and 2017, the number of certified baby-friendly hospitals increased from 6 to 108 in Germany(32) but is still lower than in neighbouring Switzerland (approx. 15 % v. 30 %, respectively)(52). While in SuSe I only 15 % of the hospitals had lactation consultants on the ward, the proportion in SuSe II was over 90 %. In addition to their medical qualification, lactation consultants receive a comprehensive training on breast-feeding and are represented almost nationwide in Germany(53). Structural efforts, for example, in staff training, support the hypothesis that recent changes in the hospital landscape towards more specialisation and quality improvement might have made hospitals more breast-feeding-friendly over time, although certain structural everyday conditions such as documentation requirements and shorter hospital stays might still hamper effective breast-feeding promotion.
Structural innovations
New federal regulations on parental benefits and parental leave as well as on maternity protection became effective between 2015 and 2017(54,55) , and all of them are discussed to be positively associated with breast-feeding duration(Reference Smith, O’B Hourihane and Kenny56–Reference Hawkins, Griffiths and Dezateux58). In parallel, regulations targeting the support of families with low income and in stressful family situations started in 2007(59).
Information campaigns
The long-established free distribution of leaflets with practical breast-feeding recommendations for mothers and hospital staff by the NSK has recently been strengthened by the multimedia information campaigns of the ‘Healthy Start – Young Family Network’, launched by the German Federal Ministry of Food and Agriculture and the Federal Ministry of Health in 2009, disseminating easy-to-understand recommendations on infant feeding with a special focus on breast-feeding(60).
Since the SuSe studies were conducted 20 years apart, it is neither possible to determine when the increase in breast-feeding friendliness occurred within the 20 years period nor can the positive effects on breast-feeding be attributed to individual direct or indirect measures of increased breast-feeding friendliness.
Perspective
There is still a considerable potential to improve breast-feeding in Germany. In the international research project ‘Becoming Breastfeeding Friendly’(Reference Pérez-Escamilla, Hromi-Fiedler and Bauermann Gubert61,Reference Hromi-Fiedler, dos Santos Buccini and Bauermann Gubert62) , which systematically evaluated breast-feeding promotion in Germany in 2017–2019(Reference Flothkötter, Kunath and Lücke63), a moderate score was achieved (1·7 out of 3·0 points)(64). The conclusions of the project strengthen the need of a multilevel breast-feeding monitoring system in Germany(65). Prospective studies like SuSe are urgently warranted. To ensure comparisons of the results over time, the design and the use of the international definitions should be maintained but complemented by other study designs that could help to better cover the social diversity of the population. To fulfil the monitoring requirements and allow a timely reaction in breast-feeding promotion measures, the repetitions should be scheduled in shorter intervals(11,65) .
Conclusion
SuSe II shows an improvement of breast-feeding promotion in hospitals and of breast-feeding prevalence during the first year of life in Germany compared to the SuSe I study 20 years earlier. Since the participation rates of hospitals and mothers were lower in SuSe II compared to SuSe I, it is not possible to disentangle the potential roles of sample selection or breast-feeding promotion activities for the overall favourable development. In the future, the comprehensive SuSe survey design should be complemented by other approaches to better reflect the diversity of hospitals and mothers for targeted breast-feeding promotion, including increased resources for researchers and hospitals for effective maternal recruitment, particularly given today’s short stay on maternity wards.
Acknowledgements
Acknowledgements: The authors kindly thank the scientific advisory board of the SuSe II study for their valued advice: Prof. Dr Nicola Bauer (Hochschule für Gesundheit), Dr Burkhard Lawrenz, (Berufsverband der Kinder- und Jugendärzte), PD Dr Erika Sievers (MPH, Ärztin für Kinder- und Jugendmedizin, Neonatologie), Aleyd von Gartzen (Deutscher Hebammenverband), PD Dr Cornelia Weikert (Bundesinstitut für Risikobewertung), Prof. Dr Klaus Vetter (Deutsche Gesellschaft für Perinatale Medizin). The authors kindly thank the participating families for answering the questionnaires conscientiously and patiently. The authors express their gratitude to all participating hospitals of both SuSe studies, especially for the much appreciated support in the recruitment of mother–infant participants. In particular, the authors would like to thank the hospitals of the SuSe II study: St. Joseph Krankenhaus, Berlin-Tempelhof; Diakonissen-Stiftungs-Krankenhaus, Speyer; St. Vincenz Krankenhaus/St. Louise, Paderborn; Sozialstiftung Bamberg Klinikum, Bamberg; Krankenhaus Landshut-Achdorf, Landshut-Achdorf; Krankenhaus St. Elisabeth und St. Barbara, Halle (Saale); Klinikum Dortmund, Dortmund; Universitätsklinikum Düsseldorf, Düsseldorf; Städtisches Krankenhaus Kiel, Kiel; Universitätsklinikum Würzburg, Würzburg; Vinzenz-Pallotti-Hospital, Bergisch Gladbach-Bensberg; Klinikum rechts der Isar, München; DRK Krankenhaus Chemnitz-Rabenstein, Chemnitz; St. Josefskrankenhaus, Freiburg; Klinikum Mannheim, Mannheim; Maria Heimsuchung Caritas-Klinik Pankow, Berlin; Universitätsklinikum des Saarlandes, Homburg/Saar; Mainz-Kinzig-Kliniken, Gelnhausen; Sana Kliniken Duisburg, Duisburg; Universitätsklinikum Freiburg, Freiburg; Marienhospital Osnabrück, Osnabrück; Ev. Diakoniekrankenhaus, Breisgau; Klinikum St. Georg, Leipzig; Klinikum Leverkusen, Leverkusen; Klinikum Osnabrück, Osnabrück; Vivantes Auguste-Viktoria-Klinikum, Berlin; Universitätsklinikum Gießen und Marburg, Marburg; Klinikum Itzehoe, Itzehoe; St.-Johannes-Hospital, Dortmund; Universitätsklinikum Münster, Münster; Regio Kliniken, Pinneberg; Städt. Klinikum Solingen, Solingen; Krankenhaus Herrenberg, Herrenberg; Ev. Amalie Sieveking Krankenhaus, Hamburg; Kath. Klinikum Oberhausen, Oberhausen; Kath. Klinikum Bochum, Bochum; Hegau-Bodensee-Klinik, Singen; Kliniken des Main-Taunus-Kreises, Bad Soden; Diakonissenkrankenhaus Mannheim, Mannheim; Ev. Krankenhaus, Lippstadt; Siloah St. Trudpert Klinikum, Pforzheim; Ubbo-Emmius-Klinik, Aurich; St. Marien-Krankenhaus Siegen, Siegen; Oberschwabenklinik, Krankenhaus St. Elisabeth, Ravensburg; Vivantes Humboldt-Klinikum, Berlin; Klinikum Coburg, Coburg; Medizin Campus Bodensee, Friedrichshafen; Carl-Thiem-Klinikum Cottbus, Cottbus; Caritas-Krankenhaus Bad Mergentheim, Bad Mergentheim; St. Vinzenz Krankenhaus Hanau, Hanau; Klinikum Oberberg, Gummersbach; Agaplesion Diakoniekrankenhaus, Rotenburg (Wümme); DRK Krankenhaus Kirchen, Kirchen; Alfried Krupp Krankenhaus Rüttenscheid, Essen; Thüringen-Kliniken ‘Georgius Agricola’, Saalfeld; imland Klinik Rendsburg, Rendsburg; Dietrich-Bonhoeffer-Klinikum, Neubrandenburg; Helios Amper-Klinikum Dachau, Dachau; St. Johannisstift, Paderborn; Heidekreis-Klinikum, Walsrode; St. Josef Krankenhaus Moers, Moers; St. Rochus-Hospital, Castrop-Rauxel; Klinikum Landsberg, Landsberg am Lech; Augusta-Kranken-Anstalt, Bochum; Städt. Klinikum Görlitz, Görlitz; HELIOS Klinik Sangerhausen, Sangerhausen; St. Barbara-Klinik, Hamm-Heesen; Johanniter-Krankenhaus Geesthacht, Geesthacht; Krankenhaus Winsen, Winsen (Luhe); Hospital zum Heiligen Geist, Kempen; Herz-Jesu-Krankenhaus Hiltrup, Münster-Hiltrup; Kreiskrankenhaus Ehingen, Ehingen; Südharz Klinikum Nordhausen, Nordhausen; Ev. Krankenhaus Paul Gerhardt Stift, Lutherstadt Wittenberg; Klinikum Kulmbach, Kulmbach; Harzklinikum Dorothea Christiane Erxleben, Wernigerode; Klinikum Landkreis Erding, Erding; Ev. Diakonie-Krankenhaus, Bremen; Sana Hanse-Klinikum, Wismar; Städt. Klinikum Dresden, Dresden; Kreisklinik Ebersberg, Ebersberg; Kreiskrankenhaus Dormagen, Dormagen; Marienhospital Brühl, Brühl; Marien Hospital Papenburg Aschendorf, Papenburg; Marienhaus Klinikum Eifel, Bitburg; St. Martinus Krankenhaus, Langenfeld; SHG: Klinikum Merzig, Merzig; Sana Krankenhaus Gerresheim, Düsseldorf; St. Anna Krankenhaus, Sulzbach-Rosenberg; Immanuel Klinikum Bernau, Bernau; SRH Krankenhaus Bad Saulgau, Bad Salgau; St. Marien-Krankenhaus, Ratingen; CURA Kath. Krankenhaus im Siebengebirge, Bad Honnef; Muldentalkliniken – Krankenhaus Wurzen, Würzen; Marien Hospital Herne, Herne; Marienkrankenhaus St. Wendel, St. Wendel; Hunsrück Klinik kreuznacher diakonie, Simmern; Ev. Krankenhaus Bethesda Mönchengladbach, Mönchengladbach; Kaiserin-Auguste-Victoria-Krankenhaus, Ehringshausen; Alb-Donau Klinikum Blaubeuren, Blaubeuren; OsteMed Kliniken und Pflege, Bremervörde; KMG Klinikum Sondershausen, Sondershausen; St. Sixtus-Hospital Haltern am See, Haltern am See; KMG Klinikum Sömmerda, Sömmerda; SRH Klinikum Naumburg, Naumburg; Kreiskrankenhaus Delitzsch, Klinik Eilenburg, Eilenburg; MEDINOS Kliniken des Landkreises Sonneberg, Sonneberg; DRK Krankenhaus Mecklenburg-Strelitz, Neustrelitz; Kreisklinik Hofgeismar, Hofgeismar. Financial support: SuSe I (1997–98) was supported by the Federal Ministry of Health (Grant number 423-7620-0/127); SuSe II (2017–19) was supported by the Federal Ministry of Food and Agriculture and the German Nutrition Society (Grant number 123-02.05-20.0321/16-II-E). Conflict of interest: All authors declare no conflict of interest; M.K. and E.S. are members of the German National Breastfeeding Committee since 1994 (M.K.) and 2008 (E.S.); S.R. is member of the Nutrition Committee of the German Society of Pediatrics and Adolescent Medicine. Authorship: N.H. conducted data analysis and drafted the manuscript; C.B. was responsible for survey management in SuSe II; E.S. gave advice on items covered by the questionnaire, data analysis and interpretation; S.R. gave advice on human milk research; A.B. developed and applied the web-based assessment tool; M.T. and J.Z. assisted in participant recruitment and data preparation; T.L. supervised SuSe II; M.K. conceived and supervised both SuSe studies. All authors critically reviewed the manuscript as submitted. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the International Scientific Committee of the Research Institute for Child Nutrition for SuSe I (1997–1998) and by the Ethics Committee of the Medical Faculty of the Ruhr University Bochum for SuSe II (2017–2019). Written informed consents were obtained from all maternity hospitals and mothers.