Given the time trends of the obesity epidemic, public health systems are clearly involved in more effective management and prevention policies. Weight excess is responsible for several chronic degenerative disorders, which in turn negatively affect the patient's outcome. Accumulation of total and abdominal fat has been independently associated with overall-cause and disease-specific mortality, thus making body weight reduction and long-term maintenance of weight loss a clinical imperative(Reference Whitlock and Lewington1–4). Body weight excess is associated not only with increased mortality(Reference Whitlock and Lewington1, Reference Pischon, Boeing and Hoffmann2) but also with a broad range of complications, such as diabetes, hypertension and CVD(Reference Calza, Decarli and Ferraroni5).
In Italy, the prevalence of overweight and obesity in the adult population (>18 years of age) has recently been estimated to be 33·4 % and 9·1 %, respectively(4). Accordingly, these data translate into an increasing prevalence of chronic diseases among weight excess categories(Reference Calza, Decarli and Ferraroni5). A similar epidemic has also been observed in children (overweight 20 %; obese 4 %)(Reference Cattaneo, Monasta and Stamatakis6). It has been speculated that the misperception of weight status among adults has important implications in the prevention of obesity since childhood(Reference Harnack, Lytle and Himes7).
With a perspective to both cure and prevent weight excess, governments have been investing a lot of money in the design of resolution programmes, and Task Forces and Working Groups have been constituted by clinicians(8–10). The main purpose is to increase the knowledge and awareness about weight status. These issues would theoretically result in better weight management and in a significant reduction of health-care costs as a consequence of cardiometabolic risk prevention(10).
Community-wide educational initiatives are heterogeneous. These could be addressed not only to schoolchildren but also to the adult population as well as to health-care professionals. Unfortunately, the effects of these programmes and how these interventions translate into population awareness and management have been scantily evaluated. It could be hypothesized that some information on these issues could be useful to improve current policies, as it cannot be excluded that current trends towards higher prevalence of overweight are also due to ineffective programmes.
To investigate current knowledge and awareness about weight status and management among Italian adults, we designed the present 1 d cross-sectional survey.
Methods
Obesity Day initiative
In 2001, the Italian Dietetic Association (ADI) designed the 1 d sensitization campaign ‘Obesity Day’. Since then, this initiative has been taking place in Italian hospitals on 10th October every year. About 1 week before the initiative, people started being informed about the upcoming event in different ways: posters were hung near the centres involved and spots were included in national newspapers and television news.
On the day of the campaign, the nutrition teams (clinical nutritionists, dietitians and nurses) belonging to the ADI-associated Clinical Nutrition or Endocrinology and Metabolic Disorders Units or Services were involved in the free-of-charge evaluation of nutritional status. No new staff were recruited. Gazebos or stands were set up outside the heath facilities and patients were recruited on an open-label basis. Accordingly, all those (out-patients or visitors) interested in gathering information on personal weight status and spontaneously presenting to the nutrition teams were evaluated. In some cases, individuals were directly invited or approached by the staff independent of apparent nutritional status. Basic nutritional assessment included the following measurements: height, body weight, BMI and waist circumference. Therefore, explanation on data collected and counselling for a healthy lifestyle were provided to achieve a possible improvement in nutritional status.
Study design and assessments
During the 2008 edition, in the northern Italian region of Lombardy, along with the basic assessment it was planned to investigate current awareness about and knowledge on weight status and management through the use of a self-administered questionnaire to be completed before any assessment or counselling. The questionnaire was initially drafted by a selected Scientific Committee (the authors of the manuscript) on the basis of literature review. Thereafter, an open discussion with the other investigators of the ADI Lombardia Study Group was planned for the improvement. An introductory section was considered to gather data on common covariates: age, sex, menopause, smoking status, years of education, physical activity and comorbidities (hypertension, diabetes, dyslipidaemia, depression, previous history of CVD). Along with this, simple questions were developed (see online Supplementary Material) to obtain information on the purposed issues.
All adults aged >18 years were eligible for study inclusion. Keeping the participants dressed in only light clothes and without shoes, body weight (to the nearest 0·1 kg) was recorded after subtracting 1 kg from the weight measured by a portable calibrated flat scale. Height (to the nearest 0·5 cm) was measured using a portable stadiometer or by using the same weighing scale provided in a telescopic vertical steel stadiometer. BMI was calculated as weight in kilograms divided by the square of height in metres (kg/m2) and categorized into four levels: normal weight (<25·0 kg/m2), overweight (25·0–29·9 kg/m2), mild obesity (30·0–34·9 kg/m2) and moderate/severe obesity (≥35·0 kg/m2)(11). Participants were also asked to report their weight.
Physical activity was quantified (h/week) by summing the duration of leisure time and the time spent playing sport in the last year. Accordingly, patients were asked to report the frequency (times per week) and duration (in min) of physical activity in a normal week. Occupational physical activity was not considered because of difficulties in standardization.
Comorbidities were assessed as follows: hypertension as recurrent blood pressure measurements ≥140/90 mmHg or the reported use of antihypertensive medications; diabetes as determined by at least two blood glucose measurements ≥126 mg/dl or current antidiabetic treatment; dyslipidaemia as high total cholesterol (>200 mg/dl) and/or TAG (>150 mg/dl) values or the use of any lipid-lowering medications; depression as reported diagnosis by a specialist practitioner or by the use of appropriate medications; and CVD as reported history of myocardial infarction and/or angina and/or stroke. Comorbidities were also ascertained through direct recall by a doctor.
Nineteen centres (ten Hospital Clinical Nutrition Units, two hospital Endocrinology and Metabolic Disorders Units, three Clinical Nutrition and Dietetics Services with territorial activity, three rehabilitation care-associated Clinical Nutrition Units and/or Dietetics Services, two University Clinical Nutrition Departments) were involved in the recruitment phase. The survey was conducted in agreement with the principles of the Declaration of Helsinki and the protocol was approved by the local ethics committees. Written informed consent was obtained from every patient.
Statistical analysis
Each recruiting centre produced an electronic archive that was then sent to the coordinating centre (Istituti Clinici di Perfezionamento, Milano, Italy). Data were first checked for completeness and then analysed using the Statistical Package for the Social Sciences statistical software package for Windows version 17·0 (SPSS Institute Inc., Chicago, IL, USA). The level of significance was established as a two-sided P value <0·05.
Data were reported as mean and sd (continuous variables) or as number and percentage (categorical variables). They were compared with the results of the Student t test (two-group comparison), the ANOVA analysis (multiple-group comparison) or Fisher's exact test.
Given the low prevalence of participants with severe obesity (BMI ≥ 40·0 kg/m2; 3·4 % of the total study sample), this obese class was combined with class II obesity (35·0–39·9 kg/m2) into one category.
OR and their 95 % CI, for the factors associated with the issues investigated, were computed by means of multivariable logistic regression models. The covariates included were: gender (female = 0 and male = 1), age (fitted as a continuous variable (1-year increase)), education (entered as <5, 5–8, 9–13 and >13 years), physical activity (categorized as none, 1–3, 4–7 and >7 h/week) and BMI (categorized as normal weight (<25·0 kg/m2), overweight (25·0–29·9 kg/m2), mild obesity (30·0–34·9 kg/m2) and moderate/severe obesity (≥35·0 kg/m2)). Other adjusting variables were: menopause (absent = 0 and present = 1), smoking habits (categorized as none = 0, former = 1 or current = 2) and comorbidities (entered independently with a 0–1 coding).
Results
Study sample
In total, 929 participants (612 female and 317 male) were evaluated. The refusal rate to participate in the survey was not systematically recorded but it was estimated to be approximately 1–2 %. All those attending the initiative agreed to complete the questionnaire. Complete data were available for 914 participants (605 female and 309 male). The features of the population according to gender and nutritional status are presented in Tables 1 and 2, respectively. The prevalence rates of overweight, mild and moderate/severe obesity were 34·8 %, 24·2 % and 13·1 %, respectively. Male participants were a little older, had a higher level of education and were more physically active than female participants. In contrast to these features, we observed a higher prevalence of overweight and obesity in male participants. As expected, nutritional status was negatively correlated with education and physical activity and positively associated with the prevalence of type 2 diabetes (P < 0·001), dyslipidaemia (P = 0·002), hypertension (P < 0·001), CVD (P = 0·016) and depression (P < 0·001) (Fig. 1).
Table 1 Personal features of the study population stratified by gender: adults attending the Obesity Day initiative, Lombardy, Italy, 2008
PA, physical activity; WL, weight loss.
*Data are reported as mean and sd, and compared with Student's t test.
†Data are reported as n and %, and compared with Fisher's exact test.
‡Waist circumference data were available for a smaller subgroup (n 600: female, n 417; male, n 183).
Percentages are calculated within single groups with the exception of the following cases:
§After excluding those on a WL diet (n 158).
∥After excluding those who have never been on a WL diet (n 384: female, n 220; male, n 164).
Table 2 Features of the whole population according to weight status (BMI categories): adults attending the Obesity Day initiative, Lombardy, Italy, 2008
PA, physical activity; WL, weight loss.
Comparisons for continuous and categorical variables were performed by ANOVA analysis and Fisher's exact test, respectively.
*Waist circumference data were available for a smaller subgroup (n 600; female, n 417 and male, n 183).
Percentages are calculated within single groups with the exception of the following cases:
†After excluding those on a WL diet (n 158).
‡After excluding those who have never been on a WL diet (n 384: BMI < 25·0 kg/m2, n 159; 25·0–29·9 kg/m2, n 153; 30·0–34·9 kg/m2, n 60; ≥35·0 kg/m2, n 12).
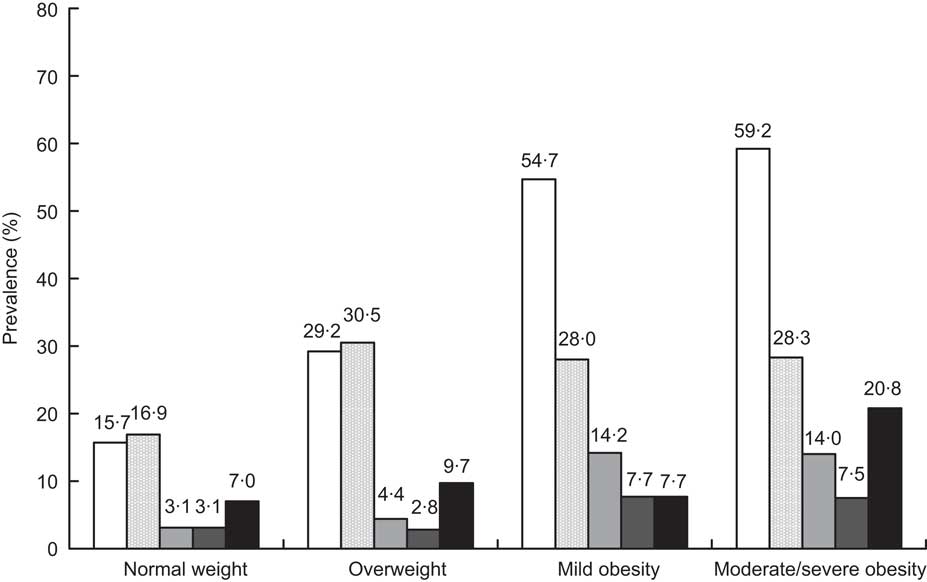
Fig. 1 Prevalence of comorbidities among weight categories (□, hypertension; ![]() , dyslipidaemia;
, dyslipidaemia; ![]() , type 2 diabetes;
, type 2 diabetes; ![]() , CVD; ▪, depression): adults attending the Obesity Day initiative, Lombardy, Italy, 2008
, CVD; ▪, depression): adults attending the Obesity Day initiative, Lombardy, Italy, 2008
Awareness about body weight and nutritional status
Most of the participants (83·5 %) considered obesity as a disease. Misperception of weight status was also frequent (38·5 %). Particularly, 38·8 % of normal-weight adults believed themselves to be overweight, whereas 71·1 % and 37·5 % of classes I and II/III obese individuals classified themselves as overweight and mildly obese, respectively. However, most of the overweight (90·2 %), mildly (96·8 %) and moderately/severely obese adults (99·1 %) recognized the need to lose weight. Female participants were less likely to underestimate body weight, although we found no difference between sexes in misreporting weight status. Multivariable logistic regression (Table 3) revealed that, with increasing age, adults were more likely to misreport their weight and not consider obesity a disease. A low education appeared to contribute to this behaviour. Participants with higher BMI were more likely to underestimate weight and misperceive weight status. However, the need to lose weight was positively associated with body weight excess. Finally, participants practising physical activity were less likely to report the need to lose weight.
Table 3 OR and 95 % CI for the factors associated with the awareness about and knowledge on weight status and management: adults attending the Obesity Day initiative, Lombardy, Italy, 2008
PA, physical activity; WL, weight loss.
OR and 95 % CI are computed by multivariable models of analysis including each answer to the questions as dependent variable.
The independent variables entered in the models were: gender (female = 0 and male = 1), age (fitted as a continuous variable (1-year increase)), menopause (absent = 0 and present = 1), smoking habits (categorized as current = 2, former = 1 or none = 0) and comorbidities (entered independently with a 0–1 coding), education (entered as <5, 5–8, 9–13 and >13 years), PA (categorized as none, 1–3, 4–7 and >7 h/week) and BMI (categorized as normal weight (<25·0 kg/m2), overweight (25·0–29·9 kg/m2), mild obesity (30·0–34·9 kg/m2) and moderate/severe obesity (≥35·0 kg/m2)). For categorical variables with more than two categories (BMI, education and PA) the OR provided is for every class increase, taking the first as reference; accordingly, the P values were calculated by test for trend (Wald's test) based on models including the variable as linear term.
OR is calculated for the overall population with the exception of the following cases:
*After excluding those on a WL diet (n 158).
†After excluding those who have never been on a WL diet (n 384: BMI < 25·0 kg/m2, n 159; 25·0–29·9 kg/m2, n 153; 30·0–34·9 kg/m2, n 60; ≥35·0 kg/m2, n 12).
Management of body weight
The role of physical activity in weight management was consistently underestimated (37·8 %), although a good proportion of participants appeared to be aware about the best way to lose weight: slowly (88 %) and through a combination of diet and physical activity (76 %). Of overweight, mildly and moderately/severely obese participants, 50·5 %, 70·6 % and 90·0 % had been on a weight loss diet. However, only 17·2 % of these ‘dieters’ declared being advised to follow a diet by their doctor. Female participants declared themselves to have been on a weight loss diet more frequently, mainly for aesthetic purposes. Male participants were more likely to diet for health reasons and showed greater expectations from weight loss programmes. The use of weight loss drugs was reported by a limited number of participants, whereas that of other over-the-counter products was slightly higher. The putative role of both drugs and other weight loss ‘adjuvants’ was better recognized by female participants.
In multivariable logistic regression analyses (Table 3), age and education appeared to significantly affect the correct management of body weight: older participants and those with lower education were less aware about the best way to regulate body weight and obtain weight loss through a diet. The role of physical activity in weight management appeared to be recognized mainly by those practising it and, interestingly, only by those on a diet. Previous dieting seemed unrelated to the importance of physical activity in weight management. BMI was positively associated with greater expectations from weight loss programmes, with overweight and obese participants aiming to achieve consistent results in a shorter time frame. In agreement with this finding, BMI was positively associated with the use of drugs and other products for weight loss.
It was also investigated whether having been on a diet has played a role in the knowledge about weight loss management. Accordingly, the variable ‘former diet’ was also included. Participants who had previously been on a diet were less acquainted with the correct practices: how many kilograms do you think could be lost in the first 2 months? (up to 5 kg, OR = 0·56, 95 % CI 0·38, 0·83; P = 0·004); which is the best way to achieve weight loss? (eat moderately and engage in physical activity, OR = 0·67, 95 % CI 0·46, 0·97; P = 0·034); how should weight loss be? (slow and gradual, OR = 0·66, 95 % CI 0·52, 0·93; P = 0·005). The associations found for the other variables were also confirmed.
Finally, attention was focused on the reasons for weight loss in current and/or previous ‘dieters’ (subgroup sample size, n 530). Aesthetic purposes were less common in male participants, in those constantly practising physical activity and in those overweight/obese. Overweight, obesity and ageing were the most important factors for being suggested to lose weight by a doctor. No association was found with the proposal for a better health status, nor with BMI, age or education. Finally, in the ‘dieter’ subgroup (current and/or former), current and former diets were positively associated with diabetes (OR = 2·44, 95 % CI 1·36, 4·35; P = 0·003 and OR = 3·22, 95 % CI 1·59, 6·49; P = 0·001, respectively). Among diabetic patients (n 70), 82·9 % reported a history of dieting but only one out of three (n 22; 31·4 %) was suggested doing so by a doctor. No association was detected between current and/or former dieting and the other diseases.
Discussion
Population-tailored educational/behavioural programmes have shown efficacy in preventing weight gain and complications, as well as in achieving weight loss(Reference Knowler, Barrett-Connor and Fowler12–Reference West, Raczynski and Phillips16). Within a perspective of prevention, previous investigators have more frequently focused on the parents’ perception of the weight status of their children. These studies most frequently reported a low awareness, thus pointing out the importance of tailored education and the role of primary care(Reference Harnack, Lytle and Himes7, Reference Huang, Becerra and Oda17–Reference Towns and D'Auria20). The self-perception of weight status among adults has been partly addressed by previous research(Reference Gillum and Sempos21–Reference Paeratakul, White and Williamson24). However, information on how individuals think weight excess should be managed has never been provided.
Awareness about body weight and nutritional status
According to the present study, obesity is recognized as a disease. Perhaps not everyone will agree that this is correct but it represents a milestone for the patient's decision making. It is not surprising that the need to lose weight is largely recognized by overweight and obese individuals. However, this seems to be the consequence of the patient's self-perception and not of objective assessments and/or appropriate education. A recent Italian study has reported that body image dissatisfaction is common in treatment-seeking patients with obesity(Reference Dalle Grave, Cuzzolaro and Calugi25). Participants did not appear to be able to classify their nutritional status and those obese were more likely to underestimate their body weight. Unfortunately, it was not assessed whether individuals know how to calculate their BMI, what its threshold values are and the rated implications for health. Probably, these issues could allow a better interpretation of how knowledge and awareness translate into practice for weight management. Poor ability to recognize their own weight status may result in ignoring health messages and in lack of motivation to reduce weight or prevent weight gain(Reference Paeratakul, White and Williamson24). Moreover, it seems likely that some recommended practices for the management of body weight are far from desirable standards(8–10). Expert panels and clinical guidelines underline the importance of a systematic and constant monitoring of body weight for its maintenance(8, 9). Unfortunately, participants were not asked whether they were used to checking their weight and how often they did so. With the increase in BMI we observed a wider tendency to underestimate body weight. Previous studies have suggested that among the explanations of this bias should be included the lack of recent body weight measurements recorded at home or taken by health-care professionals(Reference Gillum and Sempos21, Reference Kuczmarski, Kuczmarski and Najjar22). Finally, although the rationale of the Obesity Day initiative was to focus on weight excess, the elevated prevalence (∼40 %) of normal-weight adults believing themselves to be overweight should also be highlighted. Various studies have suggested that sociocultural pressures are currently responsible for an increase in dissatisfaction with body image, which in turn can be associated with the engagement in body change behaviours(Reference McCabe, Ricciardelli and Holt26, Reference Xu, Mellor and Kiehne27).
Management of body weight
In agreement with this last finding, it is not surprising that female participants reported a higher frequency of dieting and level of physical activity than male participants. However, the present study revealed that current practices for body weight management are far from desirable. Education appeared to be an important determinant of this picture. Particularly, lower education was related to greater expectations of weight loss in the first months and the desire for faster results, apparently through inappropriate weight loss programmes. Adequate knowledge about weight management should theoretically result in weight loss and long-term maintenance of nutritional status. Particularly, people should be made aware of the potential outcomes, advantages in the quality of life and health benefits derived from some programmes compared with others. Weight loss should be gradual, induced by appropriate energy restriction and physical activity. Accordingly, long-term adherence to moderate energy restriction may be feasible and will result in less decrease in the BMR, which is believed to be a determinant of weight regain(Reference Schwartz and Doucet28). The individuals recruited appeared more likely to reduce body weight through self-prescribed diets than through tailored programmes. This seems to be supported by several observations. First, the role of physical activity was recognized mainly by those who practised it. Interestingly, these participants reported less need to lose weight. Second, a significant association between previous dieting and less knowledge on the best way to achieve weight loss was detected. It would be expected that experience with programmes with little success leads to better knowledge. Thus, it is not surprising that patients with a higher BMI also have greater weight loss expectations, a finding that has already been reported in the Italian obese population(Reference Dalle Grave, Calugi and Magri29).
The level of knowledge detected in the present study has also a counterpart in the motivation found in the present study population. In agreement with the poor awareness about and interest in current body weight and nutritional status, participants reported to adhere more frequently to weight loss programmes in view of aesthetic goals rather than because of benefits to health. Some may argue that the quest for health is more likely to be sustained by the need of treating diseases rather than by their prevention. However, no association was found between dieting and obesity-related complications with the exception of diabetes.
In the approach to weight loss management, a contribution could also be ascribable to the attitude of health-care professionals. It was surprising that only approximately 22 % and 27 % of overweight and obese participants, respectively, were advised to lose weight by health-care professionals. However, 82·9 % of diabetic patients reported to be or to have been on a diet. In agreement with the evidence-based recommendations reviewed by the American Diabetic Association(Reference Franz, Bantle and Beebe30), the importance of diet and weight loss appeared to be well recognized. Unfortunately, only few diabetic patients reported being driven to dieting by a doctor. Knowledge on the issue ‘diet and diabetes’ is more likely to be the result of other educational initiatives than of a reasoned medical approach.
When the role of doctors in the management of body weight was investigated, a limited use of weight loss drugs was also observed. The US Food and Drug Administration (http://www.fda.gov) recommends that drug-based interventions should be considered only when diet and physical activity are clearly ineffective(8, Reference Lucchin, D'Amicis and Gentile31). In the present study, only 23·5 % of those who had been on multiple diets reported the prescription of a weight loss drug. This observation suggests a limited application of treatment guidelines.
Study limitations
The present study has limitations. It was a cross-sectional study and not an intervention trial aiming to assess the effectiveness of a tailored educational programme. Moreover, we do not have a previous study to compare with. It could reflect the Italian picture only in part. Some educational initiatives have already been prompted in Italy. The present results seem to reflect a time trend, as increased age and low education appeared to be associated with poor knowledge about desirable practices for weight management.
This was not a well-designed population study and findings cannot be generalized. Participants were recruited from only one of the twenty Italian regions and geographical factors have been shown to affect the prevalence and risk of nutrition-related complications(Reference Lucchin, D'Amicis and Gentile31). Inclusion was not performed on a random basis. Although some methodological strengths can be recognized (high participation rate; appropriate equipment and trained staff for anthropometric assessment), it is reasonable that the adults attending the initiative were those more concerned about weight excess and looking for counselling. This is suggested by the higher prevalence of female and obese participants. The prevalence rates of overweight and obesity in Italy are significantly lower than those of the present study. However, the level of education of age-matched groups is also lower(4, Reference Calza, Decarli and Ferraroni5). Taken together, these findings clearly underscore that current practices of weight management are still poor and educational messages are not understood and/or not adequately translated into practice. Finally, dealing with data generalizability, it cannot be excluded that some of the participants in the present study have been involved in the previous editions of the Obesity Day initiative.
Conclusion
In conclusion, the present study suggests that in Italy knowledge about weight management should be improved not only in the general population but also among health-care professionals. To confirm this finding, there is now the rationale for a nationally representative survey. Besides, the present study allows further improvement of the questionnaire developed. New educational programmes could be designed on the basis of the information collected. The efficacy of such programmes should be also addressed by high-quality intervention trials.
Acknowledgements
The present study was supported by the Italian Dietetic Association (Associazione Italiana di Dietetica e Nutrizione Clinica – ADI). The authors have no conflict of interest to declare. E.C., A.E.M., M.B. and G.F. designed the study; the ADI Lombardia Study Group collected the data; E.C. analysed the data; E.C., A.E.M. and M.B. interpreted the data; E.C. and A.E.M drafted the manuscript; E.C., A.E.M., M.B. and G.F contributed to critical revision of the manuscript. All authors contributed significantly to the work, and read and approved the final version of the manuscript. All authors, external and internal, had full access to all data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. The authors thank Miss Cecilia Magris for assistance in drafting the manuscript.
ADI Lombardia Study Group Investigators are: Baldo Cinzia, RD (Ospedale Buzzi – Istituti Clinici di Perfezionamento, Milano); Bianchi Maria Antonietta, MD (Direzione Sanitaria Dipartimento di Prevenzione Medico – Servizio Igiene Alimenti e Nutrizione, ASL di Varese, Varese); Riccardo Caccialanza, MD (Nutrition and Dietetics Service, Fondazione IRCCS Policlinico San Matteo, Pavia); Cassani Erica, MD and Cecilia Biazzi, RD (Servizio di Dietetica e Nutrizione Clinica – Istituti Clinici di Perfezionamento, Milano); Cazzato Narciso, MD and Donghi Emanuela, RD (Servizio Igiene Alimenti e Nutrizione, ASL di Lecco, Lecco); Cereda Emanuele, MD, PhD (International Center for the Assessment of Nutritional Status (ICANS) – Dipartimento di Scienze e Tecnologie Alimentari e Microbiologiche (DISTAM), Università degli Studi di Milano); Colzani Milena, MD (Centro per la Diagnosi e la Cura dell'Obesità, Azienda Ospedaliera di Busto Arsizio-Saronno-Tradate, Saronno, Varese); Cortinovis Fiorenzo, MD (U.O. di Dietetica e Nutrizione Clinica, Azienda Ospedaliera Ospedali Riuniti di Bergamo, Bergamo); Di Battista Roberto, MD (U.O di Medicina, Ambulatorio di Dietologia, Azienda Ospedaliera ‘G. Salvini’, Rho, Milano); Fatati Giuseppe MD (U.O. di Dietetica e Nutrizione Clinica, Azienda Ospedaliera ‘S.Maria’, Terni); Garnerone Laura, BioD (Scuola di Specializzazione in Scienze dell'Alimentazione, Università degli Studi di Milano, U.O. di Diabetologia e Malattie Metaboliche, IRCCS Policlinico San Donato, San Donato Milanese); La Russa Antonio, MD (Azienda Ospedaliera ‘Istituti Ospitalieri di Cremona’, Cremona); Macca Claudio, MD (U.O. di Dietetica e Nutrizione Clinica, Dipartimento di Medicina Interna, Spedali Civili di Brescia, Brescia); Malavazos Alexis Elias, MD and Lelio Morricone Elias, MD (U.O. di Diabetologia e Malattie Metaboliche, IRCCS Policlinico San Donato, San Donato Milanese); Muzio Fulvio, MD (U.O. di Dietologia e Nutrizione Clinica Azienda Ospedaliera – Polo Universitario Luigi Sacco, Milano); Noli Francesca, BioD (Ospedale Valduce, Como); Oggionni Sabrina, RD (Humanitas Gavazzeni, Bergamo); Pasqualinotto Lucia, MD (Unità di Malattie Metaboliche e Diabetologia, IRCCS San Michele, Istituto Auxologico Italiano, Milano); Rondanelli Mariangela, MD (Ambulatorio di Dietologia, Centro Interdipartimentale di Studi e Ricerche sulla Nutrizione Umana e i Disturbi del Comportamento Alimentare – Università degli Studi di Pavia); Sabbatini Annarita, RD (U.O. di Dietetica e Nutrizione Clinica, Istituto Europeo di Oncologia, Milano); Sileo Fulvio, MD (U.O. di Dietetica e Nutrizione Clinica, Azienda Ospedaliera Ospedali Riuniti di Bergamo, Bergamo); Turbini Chiara, MD (Servizio di Riabilitazione Nutrizionale e psico-motoria dell'Obesità, Casa di Cura ‘Villa Esperia’, Salice Terme, Pavia); Vigna Luisella, MD (Ambulatorio Obesità e Lavoro, Dipartimento Di Medicina Preventiva, Del Lavoro e Dell'Ambiente, Fondazione I.R.C.C.S. Ospedale Maggiore Policlinico, Mangiagalli e Regina Elena, Milano).






