Introduction
Posttraumatic stress disorder (PTSD) is a prevalent condition with a chronic course if untreated (Kessler et al., Reference Kessler, Aguilar-Gaxiola, Alonso, Benjet, Bromet and Cardoso2017; Morina, Wicherts, Lobbrecht, & Priebe, Reference Morina, Wicherts, Lobbrecht and Priebe2014). Several psychological interventions have been developed to treat this disorder and a large amount of clinical trials has investigated their efficacy. Meta-analytic reviews have concluded that psychological interventions for adult PTSD produce large effect sizes (e.g. Bisson, Roberts, Andrew, Cooper, & Lewis, Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016). However, there is lack of knowledge about the association of study quality and treatment efficacy. Literature on the efficacy of treatments for depression indicates that trials with low study quality have overestimated treatment efficacy for both psychopharmacology (Kirsch et al., Reference Kirsch, Deacon, Huedo-Medina, Scoboria, Moore and Johnson2008; Turner, Matthews, Linardatos, Tell, & Rosenthal, Reference Turner, Matthews, Linardatos, Tell and Rosenthal2008) as well as psychological treatment (Cuijpers, van Straten, Bohlmeijer, Hollon, & Andersson, Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010; Gellatly et al., Reference Gellatly, Bower, Hennessy, Richards, Gilbody and Lovell2007; Klein, Jacobs, & Reinecke, Reference Klein, Jacobs and Reinecke2007; Weisz, McCarty, & Valeri, Reference Weisz, McCarty and Valeri2006). Following a thorough examination of the relationship between study quality and treatment efficacy, Cuijpers et al. (Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010) concluded that the efficacy of psychological interventions for adult depression has been overestimated in the past. In this study, the authors assessed eight characteristics of study quality that were based on the criteria for assessing the quality of treatment delivery originally recommended by Chambless and Hollon (Reference Chambless and Hollon1998) as well as on the criteria proposed by the Cochrane Collaboration to assess the methodological validity of a study (Higgins & Green, Reference Higgins and Green2009). These criteria dictate that primary complaints were assessed with a valid diagnostic interview, a treatment manual was used, therapists were trained, treatment integrity was assessed, intent-to-treat (ITT) analyses were conducted, at least 50 participants were treated in the active and control group, an independent party conducted randomization, and assessors were blinded. Cuijpers et al. (Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010) concluded that only 11 out of 115 randomized clinical trials for depression were of high quality and that these trials had a significantly lower mean effect size than the other trials (d = 0.22 and 0.74, respectively). The small effect size of 0.22 found in high-quality trials for depression is alarming and calls for a thorough investigation of the role of trial quality in treatment efficacy. Prior to that, two meta-analyses on the efficacy of psychological interventions for pediatric depression had also found evidence that the effects of psychotherapy for depression have been overestimated (Klein et al., Reference Klein, Jacobs and Reinecke2007; Weisz et al., Reference Weisz, McCarty and Valeri2006).
Meta-analytic reviews of treatment efficacy for PTSD have applied different criteria to assess potential risks of bias and have generally concluded that methodological quality varied considerably across the trials and that risk of bias was high or unclear in a large proportion of older studies (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016). Gerger, Munder, and Barth (Reference Gerger, Munder and Barth2014) meta-analyzed 18 trials comparing the efficacy of specific v. unspecific psychological interventions for adult PTSD and concluded that high-quality trials (k = 4) did not significantly differ from lower-quality trials (k = 14). However, these results are limited by the low number of included trials and the low number of applied criteria to assess study quality (i.e. concealment of treatment allocation, adequacy of statistical analyses, and adequacy of outcome assessment).
We still lack a thorough analysis of the relationship between study quality and treatment efficacy for adult PTSD. Therefore, we aimed at providing a quantitative, meta-analytic review of the efficacy of interventions for adults suffering from PTSD and at investigating the relationship between study quality and treatment efficacy. For this purpose, we reviewed randomized controlled trials (RCTs) that compared the efficacy of psychological interventions relative to active control conditions (ACC) or passive control conditions (PCC). We first tested the hypothesis that psychological interventions can effectively reduce symptoms of PTSD. To this end, we examined the efficacy of active treatment conditions relative to PCC and ACC at posttreatment and at follow-up. Furthermore, we expected study quality to be negatively associated with treatment efficacy. We assessed the potential association between study quality and effect sizes by (1) comparing effect-sizes of high-quality v. lower-quality trials, (2) by examining study quality as a continuous predictor of effect sizes, and (3) by examining the relationship between the eight individual quality criteria and effect sizes. We defined the main structured research question describing the Population, Intervention, Comparison, Outcome, and Study design in accordance with the recommendations by the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) group (Moher, Liberati, Tetzlaff, & Altman, Reference Moher, Liberati, Tetzlaff and Altman2009). The question was ‘In patients with PTSD (P), does psychological treatment (I), compared to control conditions (C), improve PTSD (O) in randomized controlled trials (S)?’
Method
The aims and methods of this meta-analysis were registered with the PROSPERO database (CRD42018094698, http://www.crd.york.ac.uk/prospero).
Identification and selection of studies
The current systematic review was first based on the literature included in the meta-analysis by Bisson et al. (Reference Bisson, Roberts, Andrew, Cooper and Lewis2013). Then, we conducted a systematic search in the databases PsycINFO and Medline for the period between 1 January 2013 and 22 September 2020. Finally, we reviewed the relevant meta-analyses on the efficacy of psychological interventions for adult PTSD published since 2013 (Asmundson et al., Reference Asmundson, Thorisdottir, Roden-Foreman, Baird, Witcraft, Stein and Powers2019; Barawi, Lewis, Simon, & Bisson, Reference Barawi, Lewis, Simon and Bisson2020; Bisson, van Gelderen, Roberts, & Lewis, Reference Bisson, van Gelderen, Roberts and Lewis2020; Carpenter et al., Reference Carpenter, Andrews, Witcraft, Powers, Smits and Hofmann2018; Cipriani et al., Reference Cipriani, Williams, Nikolakopoulou, Salanti, Chaimani, Ipser and Stein2018; Coventry et al., Reference Coventry, Meader, Melton, Temple, Dale and Wright2020; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016; Gallegos, Crean, Pigeon, & Heffner, Reference Gallegos, Crean, Pigeon and Heffner2017; Gerger et al., Reference Gerger, Munder and Barth2014; Grasser & Javanbakht, Reference Grasser and Javanbakht2019; Hegberg, Hayes, & Hayes, Reference Hegberg, Hayes and Hayes2019; Hopwood & Schutte, Reference Hopwood and Schutte2017; Karatzias et al., Reference Karatzias, Murphy, Cloitre, Bisson, Roberts, Shevlin and Hutton2019; Khan et al., Reference Khan, Dar, Ahmed, Bachu, Adnan and Kotapati2018; Kline, Cooper, Rytwinksi, & Feeny, Reference Kline, Cooper, Rytwinksi and Feeny2018; Kuester, Niemeyer, & Knaevelsrud, Reference Kuester, Niemeyer and Knaevelsrud2016; Lenz, Haktanir, & Callender, Reference Lenz, Haktanir and Callender2017; Lewis, Roberts, Andrew, Starling, & Bisson, Reference Lewis, Roberts, Andrew, Starling and Bisson2020a; Lewis, Roberts, Bethell, Robertson, & Bisson, Reference Lewis, Roberts, Bethell, Robertson and Bisson2018; Lewis, Roberts, Gibson, & Bisson, Reference Lewis, Roberts, Gibson and Bisson2020b; Mahoney, Karatzias, & Hutton, Reference Mahoney, Karatzias and Hutton2019; Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Stockton, Meiser-Stedman and Pilling2020; Montero-Marin, Garcia-Campayo, López-Montoyo, Zabaleta-Del-Olmo, & Cuijpers, Reference Montero-Marin, Garcia-Campayo, López-Montoyo, Zabaleta-Del-Olmo and Cuijpers2018; Morina, Malek, Nickerson, & Bryant, Reference Morina, Malek, Nickerson and Bryant2017a; Niles et al., Reference Niles, Mori, Polizzi, Pless Kaiser, Weinstein, Gershkovich and Wang2018; Schwartze, Barkowski, Strauss, Knaevelsrud, & Rosendahl, Reference Schwartze, Barkowski, Strauss, Knaevelsrud and Rosendahl2019; Springer, Levy, & Tolin, Reference Springer, Levy and Tolin2018; Tran & Gregor, Reference Tran and Gregor2016; Van Dis et al., Reference Van Dis, van Veen, Hagenaars, Batelaan, Bockting, van den Heuvel and Engelhard2020; Wilson et al., Reference Wilson, Farrell, Barron, Hutchins, Whybrow and Kiernan2018). Inclusion criteria for the meta-analysis were: (1) RCT, (2) treatment targets primarily chronic PTSD, (3) participants older than 17 years, (4) at least ten participants per condition at post-assessment, and (5) at least 70% of the sample was diagnosed with PTSD by means of a structured interview (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013). There were no restrictions on language. Trials on comorbid PTSD and substance use disorders or traumatic brain injury were excluded. Other forms of comorbidity were allowed, yet PTSD needed to be the primary diagnosis.
We conducted multi-field searches (in titles, abstracts, and key concepts) using the following terms (Morina, Koerssen, & Pollet, Reference Morina, Koerssen and Pollet2016): Posttraumatic Stress Disorder (Posttraumatic stress OR post-traumatic stress OR Posttraumatic syndrome* OR PTSD OR PTSS), and Treatment (treatment* OR intervention* OR therapy OR psychotherapy OR exposure OR trial OR counselling). Two independent investigators first inspected the title and abstract of all hits and then read full texts of the hits that seemed to meet the aforementioned inclusion criteria.
Quality assessment
To code for the quality of included studies, we applied the eight quality criteria used by Cuijpers et al. (Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010): (1) participants met diagnostic criteria for PTSD identified with a diagnostic interview, (2) use of a treatment manual, (3) training of therapists, (4) assessment of treatment integrity, (5) report of ITT analyses, (6) at least 50 patients were included in a comparison, (7) independent randomization, and (8) blinded assessors. The criteria were coded categorically with ‘1’ if the criterion was fulfilled or ‘0’ if the criterion was not met or not reported (Cuijpers et al., Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010). Accordingly, a trial receiving eight points was rated as being of high quality. The second and third authors coded the quality criteria independently and discrepancies were resolved in joint discussions with the first author.
Coding of trial characteristics
Two independent investigators coded and extracted from each study: comparison group(s), number of participants, type of outcome measure, intervention format (individual or group), number and length of sessions, length of follow-up, age of participants, percentage of participants with a diagnosis of PTSD at pretreatment, female gender, type of intervention, country where the trial was conducted, type of traumatic event, and outcome scores (mean and standard deviation). If a publication reported more than one outcome measure of PTSD, we prioritized clinician-based PTSD measures (e.g. Blake et al., Reference Blake, Weathers, Nagy, Kaloupek, Gusman, Charney and Keane1995) over self-reports. Furthermore, publications that exclusively reported a comparison between two active interventions belonging to the same treatment family (e.g. Acierno et al., Reference Acierno, Knapp, Tuerk, Gilmore, Lejuez, Ruggiero and Foa2017) were not included. The follow-up period was divided into follow-up 1 (FU1) assessed up to 20 weeks after posttreatment and follow-up 2 (FU2) assessed more than 20 weeks after posttreatment. In line with previous meta-analyses on interventions for PTSD (Morina et al., Reference Morina, Koerssen and Pollet2016; Morina, Malek, Nickerson, & Bryant, Reference Morina, Malek, Nickerson and Bryant2017b), treatment interventions were first coded as either active treatment or control group. The active treatment group was then subdivided into trauma-focused cognitive-behavior therapy (TF-CBT), eye movement desensitization and reprocessing (EMDR), or other active treatment conditions (i.e. interpersonal psychotherapy, imagery rescripting, present centered therapy, meta-cognitive therapy, emotion focused supportive psychotherapy, dialogical exposure therapy, dialectical behaviour therapy, and mindfulness-based interventions). The control groups were subdivided into PCC, consisting of waitlist, single session psychoeducation, minimal attention, and self-administered relaxation interventions, and ACC, consisting of supportive counseling, treatment as usual, medical placebo, active listening, guided psychoeducation, stress inoculation training, self-help booklets, and guided relaxation training.
Statistical analysis
Data from ITT samples were used when available (72 publications) and completer samples were utilized if ITT samples were not provided (52 publications). To calculate an effect size, the control group mean was subtracted from the treatment group mean at posttreatment or follow-up, respectively, and divided by the pooled standard deviation. Subsequently, the outcome was multiplied by a sample size correction factor J = 1 − (3/(4df − 1)) to obtain the effect size Hedges' g (Lipsey & Wilson, Reference Lipsey and Wilson2009). Subgroup analyses were conducted if a specific group of interventions consisted of at least four comparisons (Morina et al., Reference Morina, Koerssen and Pollet2016). Analyses were completed with the metafor package (v.1.9.8) in R 3.5. using random-effect models given the heterogeneity of the studies (R Core Team, 2015; Viechtbauer, Reference Viechtbauer2010). Effect sizes may be conservatively interpreted with Cohen's convention of small (0.2), medium (0.5), and large (0.8) effects (Cohen, Reference Cohen2013). To examine heterogeneity of effect sizes, we calculated the Q-statistic and the I 2-statistic that is an indicator of heterogeneity in percentages, with higher percentages indicating high heterogeneity. The variance of true effect (τ 2) was assessed. To consider potential inequality in effect sizes, prediction intervals (PIs) were calculated using τ 2. PIs estimate an interval within which the estimate is expected to be (IntHout, Ioannidis, Rovers, & Goeman, Reference IntHout, Ioannidis, Rovers and Goeman2016; Riley, Higgins, & Deeks, Reference Riley, Higgins and Deeks2011). We also calculated the numbers needed to treat (NNT), which inform about the numbers of patients needed to be treated to prevent one adverse event and is more easily interpretable from a clinical perspective (Kraemer & Kupfer, Reference Kraemer and Kupfer2006). Unlike Cuijpers et al. (Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010) who applied a p value of 0.10 as the threshold for statistical significance, we utilized the more conservative p value of 0.05.
Potential publication bias was assessed through visual inspection of funnel plots for the primary outcome measures and analyses including more than nine comparisons (Sterne et al., Reference Sterne, Sutton, Ioannidis, Terrin, Jones, Lau and Higgins2011). Furthermore, we calculated the likely number of missing studies using the trim and fill procedure, which yields an estimate of the effect size after publication bias has been taken into account (Duval & Tweedie, Reference Duval and Tweedie2000). The association between quality criterion and treatment efficacy was examined by factorial subgroup analyses, whereas the overall influence of quality was investigated with mixed-effect models. If outliers emerged, we repeated the respective analysis without the outliers. We defined an effect size as an outlier when it was at least 3.3 standard deviations below or above the pooled mean effect size (Hunter & Schmidt, Reference Hunter and Schmidt2007; Tabachnick & Fidell, Reference Tabachnick and Fidell2013).
Results
Selection and characteristics of included studies
Figure 1 displays a PRISMA (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009) flow diagram of the publication selection process. After examining 22 029 abstracts, 1026 full text publications were reviewed. The final review resulted in 136 clinical trials with 8978 participants in total (5695 in an active treatment condition and 3283 in a PCC or ACC).

Fig. 1. Flowchart of study selection.
Relevant characteristics of the 136 trials are summarized in the online Supplementary material (Appendix A & B). All publications were journal articles in English, 119 of the trials were conducted in a Western country (four with refugees), while 17 were conducted in non-Western countries (four with refugees). The mean age of participants was 40.04 years (s.d. = 8.60) and 54.67% of them were female. Participants entered treatment on the basis of PTSD symptoms resulting from different traumatic events, with 65 publication including participants with diverse trauma backgrounds and combat being the most common form of specific traumatic experience. Individual treatment was applied in 73.53% of the trials (see Appendix A).
Appendix D in the online Supplementary material describes the number of active treatment and control conditions being examined in the included studies. Relevant follow-up data (i.e. at least one relevant group comparison available) were reported for 64 active treatment conditions. Some publications did not provide controlled follow-up data (e.g. Asukai, Saito, Tsuruta, Kishimoto, and Nishikawa, Reference Asukai, Saito, Tsuruta, Kishimoto and Nishikawa2010) and two trials (Neuner et al. Reference Neuner, Kurreck, Ruf, Odenwald, Elbert and Schauer2010; Orang et al. Reference Orang, Ayoughi, Moran, Ghaffari, Mostafavi, Rasoulian and Elbert2018) did not report controlled posttreatment data. In one trial, the subgroup sample size was above 9 only for the follow-up measures and this trial was included only in follow-up comparison (Krupnick et al., Reference Krupnick, Green, Stockton, Miranda, Krause and Mete2008).
Treatment efficacy
In total, 65 and 53 publications reported on the efficacy of 77 and 59 active treatment conditions compared to PCC and ACC at posttreatment, respectively. The pooled effect sizes of these comparisons were significantly larger (p < 0.001) when using PCC (g = 1.08) than using ACC (g = 0.47; see Table 1). Yet, overall the results demonstrate that psychological interventions are significantly more effective in reducing PTSD symptoms than both PCC and ACC. Heterogeneity was large for comparisons to both PCC and ACC at posttreatment, respectively (I 2 = 81.22; Q = 318.12, p < 0.001 and I 2 = 57.23; Q = 133.37, p < 0.001), indicating substantial heterogeneity in effect sizes between studies. Four trials comparing active treatment conditions to PCC were considered as outliers (Paunović, Reference Paunović2011; Sloan, Marx, Bovin, Feinstein, & Gallagher, Reference Sloan, Marx, Bovin, Feinstein and Gallagher2012; Wells, Walton, Lovell, & Proctor, Reference Wells, Walton, Lovell and Proctor2015; Zang, Hunt, & Cox, Reference Zang, Hunt and Cox2014) and when these were excluded, active conditions (i.e. k = 73) still reached an effect size of g = 0.99 [95% confidence interval (CI) = 0.86–1.13]. The comparison of active treatment conditions to ACC did not reveal any outliers. As can be seen in Table 1, active treatment conditions produced medium-to-large effect sizes when compared to PCC both up to 20 weeks (i.e. FU1) as well as more than 20 weeks following treatment (i.e. FU2).
Table 1. Efficacy of psychological interventions

ACC, active control conditions; k, number of trials included in the analysis for the given comparison; n.a., number of trials too small (k < 4) to conduct analysis; EMDR, eye movement desensitization and reprocessing; FU, follow-up; OAC, other active conditions; PCC, passive control conditions; PI, prediction interval; TF-CBT, trauma-focused Cognitive behavior therapy; WL, waitlist. For outlier- and asymmetry-adjustments see Appendix D.
*p < 0.05, **p < 0.01, ***p < 0.001.
Subgroup analyses at posttreatment revealed that TF-CBT interventions produced large and medium effect sizes when compared to PCC and ACC (see Table 1). Similar effect sizes were also found for EMDR when compared to PCC and ACC. Other active treatment conditions (i.e. excluding TF-CBT and EMDR) also produced large and medium effect sizes when compared to PCC and ACC. A comparison of TF-CBT to other active treatment conditions (excluding EMDR) and to EMDR revealed nonsignificant effect sizes.
Publication bias
With respect to comparisons with PCC, the visual inspection of the funnel plot and Egger's test pointed at significant asymmetry of the funnel plot (p < 0.001), but Duval and Tweedie's trim and fill procedure did not indicate missing trials. With regard to comparisons with ACC, the visual inspection of the funnel plot and Egger's test also indicated significant asymmetry of the funnel plot (p = 0.001). Duval and Tweedie's trim and fill procedure indicated four missing trials and the adjusted effect size was g = 0.42, 95% CI = 0.30–0.54. Note that this represents a small change in effect size (i.e. from 0.47 to 0.42).
Study quality
Intraclass correlation coefficient of the total score for all studies combined among the two raters of study quality was 0.79, 95% CI = 0.76–0.81, indicating good inter-rater reliability. Overall, study quality was moderate with a mean of 5.82 (s.d. = 1.48). The vast majority of trials (91.91%) received at least half of the quality scores. A total of 14 trials (10.29%) met all eight quality criteria (Acarturk et al., Reference Acarturk, Konuk, Cetinkaya, Senay, Sijbrandij, Gulen and Cuijpers2016; Bohus et al., Reference Bohus, Kleindienst, Hahn, Müller-Engelmann, Ludäscher, Steil and Priebe2020; Cloitre et al., Reference Cloitre, Stovall-McClough, Nooner, Zorbas, Cherry, Jackson and Petkova2010; Ehlers et al., Reference Ehlers, Hackmann, Grey, Wild, Liness, Albert and Clark2014; Foa et al., Reference Foa, McLean, Zang, Rosenfield, Yadin, Yarvis and Peterson2018; Galovski, Blain, Mott, Elwood, & Houle, Reference Galovski, Blain, Mott, Elwood and Houle2012; Ivarsson et al., Reference Ivarsson, Blom, Hesser, Carlbring, Enderby, Nordberg and Andersson2014; Jacob, Neuner, Maedl, Schaal, & Elbert, Reference Jacob, Neuner, Maedl, Schaal and Elbert2014; Langkaas et al., Reference Langkaas, Hoffart, Øktedalen, Ulvenes, Hembree and Smucker2017; Pacella et al., Reference Pacella, Armelie, Boarts, Wagner, Jones, Feeny and Delahanty2012; Reger et al., Reference Reger, Koenen-Woods, Zetocha, Smolenski, Holloway, Rothbaum and Gahm2016; Sloan, Unger, Lee, & Beck, Reference Sloan, Unger, Lee and Beck2018; Van den Berg et al., Reference Van den Berg, de Bont, van der Vleugel, de Roos, de Jongh, van Minnen and van der Gaag2015; Van Dis et al., Reference Van Dis, van Veen, Hagenaars, Batelaan, Bockting, van den Heuvel and Engelhard2007). Eight of these trials compared a total of 12 active treatment conditions to passive control groups and this comparison produced an effect size of g = 0.87 (see Fig. 2), which was not significantly smaller than the effect size of the 65 trials with lower quality (g = 1.14; see Table 2). Four of the high-quality trials compared active treatment conditions to PCC at FU1 and produced an effect size of g = 0.78, CI 0.22–1.33; NNT = 2.40. Only two of the high-quality trials provided FU2 data. Heterogeneity was large for both high- and low-quality trials. Three high-quality trials compared active treatment conditions to ACC (Cloitre et al., Reference Cloitre, Stovall-McClough, Nooner, Zorbas, Cherry, Jackson and Petkova2010; Ivarsson et al., Reference Ivarsson, Blom, Hesser, Carlbring, Enderby, Nordberg and Andersson2014; Van der Kolk et al., Reference Van der Kolk, Spinazzola, Blaustein, Hopper, Hopper, Korn and Simpson2007) and three high-quality trials compared different active treatments (Bohus et al., Reference Bohus, Kleindienst, Hahn, Müller-Engelmann, Ludäscher, Steil and Priebe2020; Langkaas et al., Reference Langkaas, Hoffart, Øktedalen, Ulvenes, Hembree and Smucker2017; Sloan et al., Reference Sloan, Unger, Lee and Beck2018), precluding meta-analytic review due to small number of available trials.

Fig. 2. Effect sizes of high-quality trials on treatments for PTSD compared to passive control conditions at post-test.
Table 2. Comparison of high-quality (HQ) and lower-quality trials (Other) when compared to passive control conditions at posttreatment
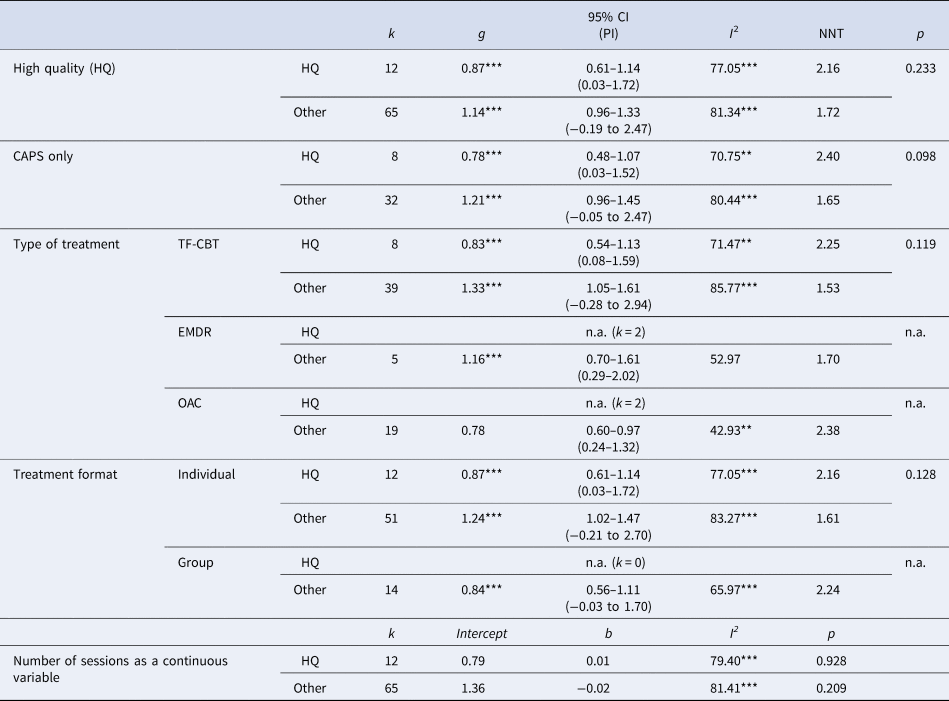
CAPS, clinician-administered PTSD scale; k, number of trials included in the analysis for the given comparison; n.a., not applicable [i.e. number of trials too small (k < 4) to conduct analysis]; OAC, other active conditions; PCC, passive control conditions; PI, prediction interval; TF-CBT, trauma-focused cognitive behavior therapy. p values refer to the comparison of high quality v. other studies and to the significance level of b. For outlier adjustments see Appendix E.
*p < 0.05; **p < 0.01 ***p < 0.001.
We further conducted a series of subgroup analyses to examine whether the following factors were associated with study quality: use of the Clinician-Administered PTSD Scale for DSM (Blake et al., Reference Blake, Weathers, Nagy, Kaloupek, Gusman, Charney and Keane1995) as treatment outcome, type of treatment (TF-CBT v. other), treatment format (individual v. group), type of control (PCC v. ACC), and total treatment duration in minutes (as a continuous variable). As shown in Table 2, none of the analyses revealed significant results. We also excluded outliers if indicated, however, the results remained non-significant.
Relationship between effect size and quality criteria
In a series of subgroup analyses we examined the relationship between treatment efficacy and single quality criteria (see Table 3). Use of a treatment manual was a significant predictor of effect size. However, this analysis included four outliers and their exclusion produced non-significant results (p = 0.224). None of the other seven criteria was significantly associated with treatment efficacy. The examination of the relationship between study quality as a continuous variable including all eight items and treatment efficacy also produced non-significant results. Altogether, the findings are contrary to our hypothesis and indicate that high-quality trials produced similar treatment effects as lower-quality trials.
Table 3. Associations between quality criteria and effect sizes when compared to passive control conditions at posttreatment
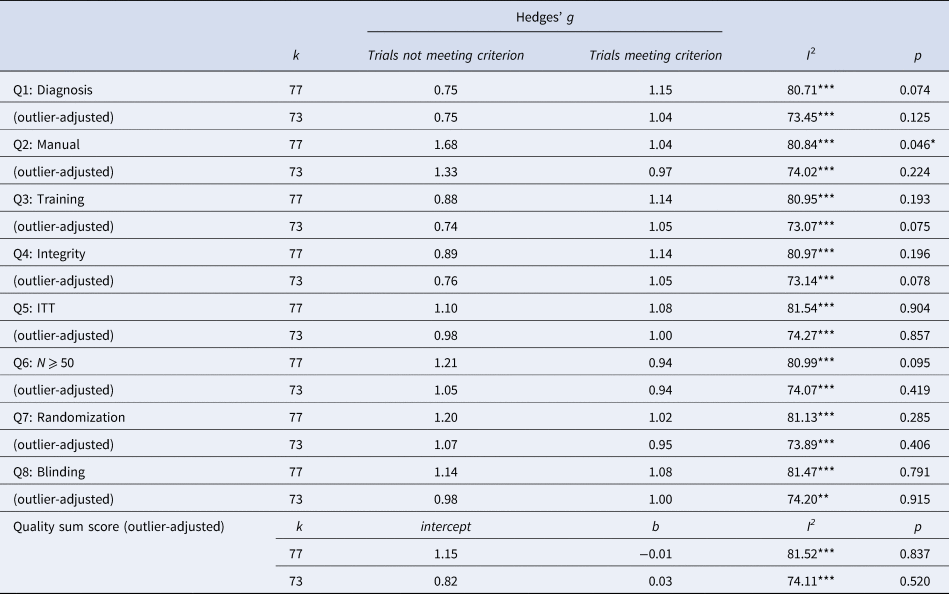
ITT, analyses conducted on an intent-to-treat basis (as opposed to completer basis); k, number of trials included in the analysis for the given comparison; p values refer to the comparison of trials meeting v. not meeting the quality criterion or the continuous moderator analyzed.
*p < 0.05, **p < 0.01, ***p < 0.001.
Discussion
We aimed at providing a quantitative review of the efficacy of interventions for adults suffering from PTSD and at investigating the relationship between study quality and treatment efficacy. The results of 136 RCTs suggest that psychological interventions can effectively reduce PTSD symptoms. Our findings further indicate that study quality is not significantly associated with treatment efficacy.
Consistent with previous meta-analyses (e.g. Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016), our findings demonstrate the efficacy of psychological interventions for PTSD relative to PCC and ACC. This applies in particular to TF-CBT that produced medium-to-large effect sizes when compared to PCC and ACC at both posttreatment and follow-up. EMDR, too, produced medium-to-large effect sizes when compared to PCC and ACC. However, too few trials have examined the long-term efficacy of EMDR relative to control conditions. The comparison on TF-CBT produced nonsignificant effect sizes when compared to EMDR and when compared to other psychological treatments. Altogether, TF-CBT and EMDR have been most researched and appear to be effective at sustaining the reduction of symptoms of PTSD beyond treatment endpoint. These findings help inform which psychological interventions have strongest evidence of effect and should therefore be prioritized for clinical use when available. It is important to note, however, that 88% of the trials were conducted in Western countries, limiting the informative value for non-Western countries.
Our meta-analysis suggests that psychological interventions can produce large treatment effects irrespective of study quality. Contrary to findings from research on treatment for depression (Cuijpers et al., Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010), comparisons of high-quality trials with lower-quality trials produced only non-significant results as did the investigation of the single quality criteria. Two findings in particular strengthen the conclusion that psychological interventions for PTSD are efficacious. First, overall study quality was moderate with a mean of 5.82 on a scale from 0 to 8. Second, the finding that high-quality trials too produced large effect sizes further strengthens this conclusion. It remains unclear why our findings are different from those reported by Cuijpers et al. The comparison to the findings by Cuijpers et al. seems relevant as in both meta-analyses a similar number of trials was included (i.e. 136 in our meta-analysis v. 116 in Cuijpers et al.). Furthermore, the number of trials meeting all measured study quality criteria comprised about 10% of trials in both meta-analyses. One explanation may relate to overall study quality in each meta-analysis. In the current meta-analysis, 92% of the trials received at least half of the quality scores, which indicates that trial quality in general was not that poor. However, Cuijpers et al. only reported that 11 trials met all criteria and did not further report on the overall quality. Other relevant factors may be attributed to the heterogeneity in the diagnosis and overall effect sizes. Overall, depression is a much more heterogeneous disorder than PTSD and might be more difficult to treat. In fact, the overall treatment effects were larger in the current meta-analysis than in the one by Cuijpers et al. Our results are in line with a recent meta-analysis on the association between study quality and treatment efficacy for pediatric PTSD (Hoppen & Morina, Reference Hoppen and Morina2020), which found that neither overall quality of the trials nor specific quality criteria were associated with effect sizes. Nonetheless, we must acknowledge that the number of high-quality trials is very small and therefore more high-quality trials need to be conducted to more rigorously examine treatment efficacy for PTSD. This applies in particular to other treatment forms than TF-CBT. Furthermore, many sub-analyses of long-term effects were limited by the low number of trials providing follow-up data. Accordingly, future research needs to investigate long-term effects of psychological interventions.
Strengths and limitations
This work represents the first thorough examination of the association between study quality and treatment efficacy for PTSD. The inclusion of a total of 136 trials strengthens the validity of our findings. However, we also note some limitations. First, 45% of the trials reported treatment completer data and the remainder ITT data, which raises difficulties in interpretation of results. Second, some specific quality criteria, such as the criterion of having included at least 50 patients, may be criticized as rather arbitrary. Although we explicitly aimed at applying the criteria examined in relation to treatment of depression (Cuijpers et al., Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010), future research needs to use other quality measures. Recall, however, that the quality criteria that we applied here are based on the criteria for assessing the quality of treatment delivery originally recommended by Chambless and Hollon (Reference Chambless and Hollon1998) as well as the Cochrane Collaboration to assess trial quality (Higgins & Green, Reference Higgins and Green2009). These two sets of criteria have played a decisive role in our understanding of what constitutes valid clinical trials that should inform empirically supported clinical work. Third, our ratings were based on the information reported in the specific publication, which may have resulted in rating some criterion as absent because the authors failed to report it. Finally, most of the included trials examined TF-CBT and the results mostly relate to this family of interventions.
Conclusion
In sum, current published research indicates that trauma-focused treatments produce large treatment effects. This is in line with current treatment guidelines recommending trauma-focused treatments as first line interventions (Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016). A substantial increase in the number of trials published in recent years resulted in a greater level of confidence in these findings, yet, more trials with follow-up assessments are needed. Treatment efficacy was not associated with study quality, which further supports the assumption that psychological interventions for PTSD are efficacious.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721001641 .
Author contributions
NM and THH designed the study and wrote the protocol. THH and AK conducted the analyses. NM wrote the first draft of the manuscript, and all authors contributed to and have approved the final manuscript.
Financial support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sector.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical standards
All presented data are publicly accessible and ethical approval was not required for this meta-analysis.








