Introduction
Sick leave due to mental disorders poses a relevant societal and economic burden. Additional to high individual burden and loss in quality of life (Comer et al., Reference Comer, Blanco, Hasin, Liu, Grant, Turner and Olfson2010), mental disorders are associated with long-term sick leave (Henderson, Harvey, Øverland, Mykletun, & Hotopf, Reference Henderson, Harvey, Øverland, Mykletun and Hotopf2011; Knudsen, Harvey, Mykletun, & Øverland, Reference Knudsen, Harvey, Mykletun and Øverland2013; Plana-Ripoll et al., Reference Plana-Ripoll, Weye, Knudsen, Hakulinen, Madsen, Christensen and McGrath2023) and high costs due to absenteeism and presenteeism (Evans-Lacko & Knapp, Reference Evans-Lacko and Knapp2016). The Organization for Economic Cooperation and Development (OECD) estimates average OECD countries to spend 1.9% of their gross domestic product on sickness and disability benefits, or about 10% of public social spendings (OECD, 2010). For several countries, it is estimated that 20–30% of all costs due to sick leave are caused by mental disorders (OECD, 2012, 2015). In the USA, costs due to depression alone were estimated to accumulate to 326 billion USD in 2018, with around 61% of workplace related costs, and to have risen by 38% since 2010 (Greenberg et al., Reference Greenberg, Fournier, Sisitsky, Simes, Berman, Koenigsberg and Kessler2021).
Meta-analyses on the effect of different psychological and work-focused interventions for common mental disorders and depression on sick leave report small effects yet emphasize a need for further studies (Nieuwenhuijsen et al., Reference Nieuwenhuijsen, Verbeek, Neumeyer-Gromen, Verhoeven, Bültmann and Faber2020; Nigatu et al., Reference Nigatu, Liu, Uppal, McKinney, Rao, Gillis and Wang2016; Salomonsson, Hedman-Lagerlöf, & Öst, Reference Salomonsson, Hedman-Lagerlöf and Öst2018). In the included studies, most interventions consisted of work-related interventions focusing on return-to-work or behavioral therapy (BT). To our knowledge, only few studies exist on the effects of psychodynamic therapy (PDT) on sick leave (Burnand, Andreoli, Kolatte, Venturini, & Rosset, Reference Burnand, Andreoli, Kolatte, Venturini and Rosset2002; Epping, de Zwaan, & Geyer, Reference Epping, de Zwaan and Geyer2018; Knekt, Lindfors, Sares-Jäske, Virtala, & Härkänen, Reference Knekt, Lindfors, Sares-Jäske, Virtala and Härkänen2013).
Several randomized controlled trials (RCT) showed similar positive treatment effects in terms of symptom reduction as well as on other health factors for short-term outpatient BT and PDT (Abbass et al., Reference Abbass, Town, Holmes, Luyten, Cooper, Russell and Kisley2020; Driessen et al., Reference Driessen, Hegelmaier, Abbass, Barber, Dekker, Van and Cuijpers2015; Leichsenring et al., Reference Leichsenring, Luyten, Hilsenroth, Abbass, Barber, Keefe and Steinert2015; Steinert, Munder, Rabung, Hoyer, & Leichsenring, Reference Steinert, Munder, Rabung, Hoyer and Leichsenring2017). Sick leave is discussed to be associated with symptom severity and to serve as an indicator of (mental) health and functioning (Volz et al., Reference Volz, Bartečků, Bartova, Bessa, De Berardis, Dragasek and Kasper2022). Hence, sick leave duration might be affected similarly by both treatment approaches as well.
Claims data pose a relevant and economically assessable data source and can be used to identify and estimate effects of single psychotherapeutic approaches on sick leave. This study aims to compare sick leave days over the course of outpatient short-term treatments in BT and PDT using a large database of health care claims data. Based on results of RCT studies, our null-hypothesis is an equal reduction in sick leave days between BT and PDT from before to after treatment.
Methods
The study follows a study protocol pre-registered and uploaded to the Open Science Framework (https://osf.io/xf6vb/).
Data source
This study was conducted based on the InGef research database, an anonymized health care claims database with longitudinal data from approximately nine million Germans insured in one of 52 German statutory health insurances (SHI). The database showed good agreement with nationwide demographics and morbidity and mortality measures in 2019 (Ludwig, Enders, Basedow, Walker, & Jacob, Reference Ludwig, Enders, Basedow, Walker and Jacob2022).
In brief, the InGef research database includes the following information: demographic data (e.g. age, sex), inpatient and outpatient services and diagnoses, drug prescription and dispensing data, as well as sick leave data and diagnoses. All diagnoses in the database are coded in accordance with the German modification of the 10th revision of the International Classification of Diseases (ICD-10-GM). Information on single services and procedures are coded via the Uniform Value Scale (or doctor's fee schedule; ‘Einheitlicher Bewertungsmaßstab’; EBM) for outpatient and operation and procedural codes (‘Operationen- und Prozedurenschlüssel’; OPS) for inpatient treatments (Ludwig et al., Reference Ludwig, Enders, Basedow, Walker and Jacob2022). All patient-level data in the InGef database are de-identified to comply with German data protection regulations.
Study population
We conducted a cohort study with patients who received a short-term outpatient BT or PDT. The complete study period spans from 01 January 2014 to 31 December 2019. The period from 01 January 2015 to 31 December 2018 was used as the observation period to identify patients beginning and ending treatment. Patients were followed from one year before the beginning of treatment (baseline period) for up to one year after the end of treatment (follow-up period).
Selection criteria
Short-term psychotherapy was defined as a series of at least 10 and no more than 25 sessions of outpatient BT or PDT by one single therapist followed by a period of 180 days without a session of psychotherapy. Beginning and end of psychotherapy were defined as the first and last session of such a series, respectively. Psychotherapy is subject to application at a patients' SHI in Germany, whereas application-free sessions which are mainly intended for psychodiagnosis can be conducted before treatment. We demanded at least one application-free session within three months preceding the beginning of treatment. To prevent ambiguity in exposure definition (i.e. which treatment was received), we also demanded a period ‘free of therapy’ of one year before the first billed session of psychotherapy in 2015 to 2018 without outpatient psychotherapy, still allowing patients to switch between therapists. Patients had to be aged ⩾19 at the beginning of treatment and aged ⩽65 years at the end of treatment to refer to possibly working individuals and assess reasonable information on sick leave. To refer to outpatient treatments only, we excluded patients who showed inpatient psychiatric treatment stays in one year preceding the beginning through 180 days after the end of treatment. The whole selection process and used criteria are displayed in Fig. 1. The used procedure codes, computational order, and criteria rationales are described in the supplementary information (online Supplementary Tables S1 and S2).
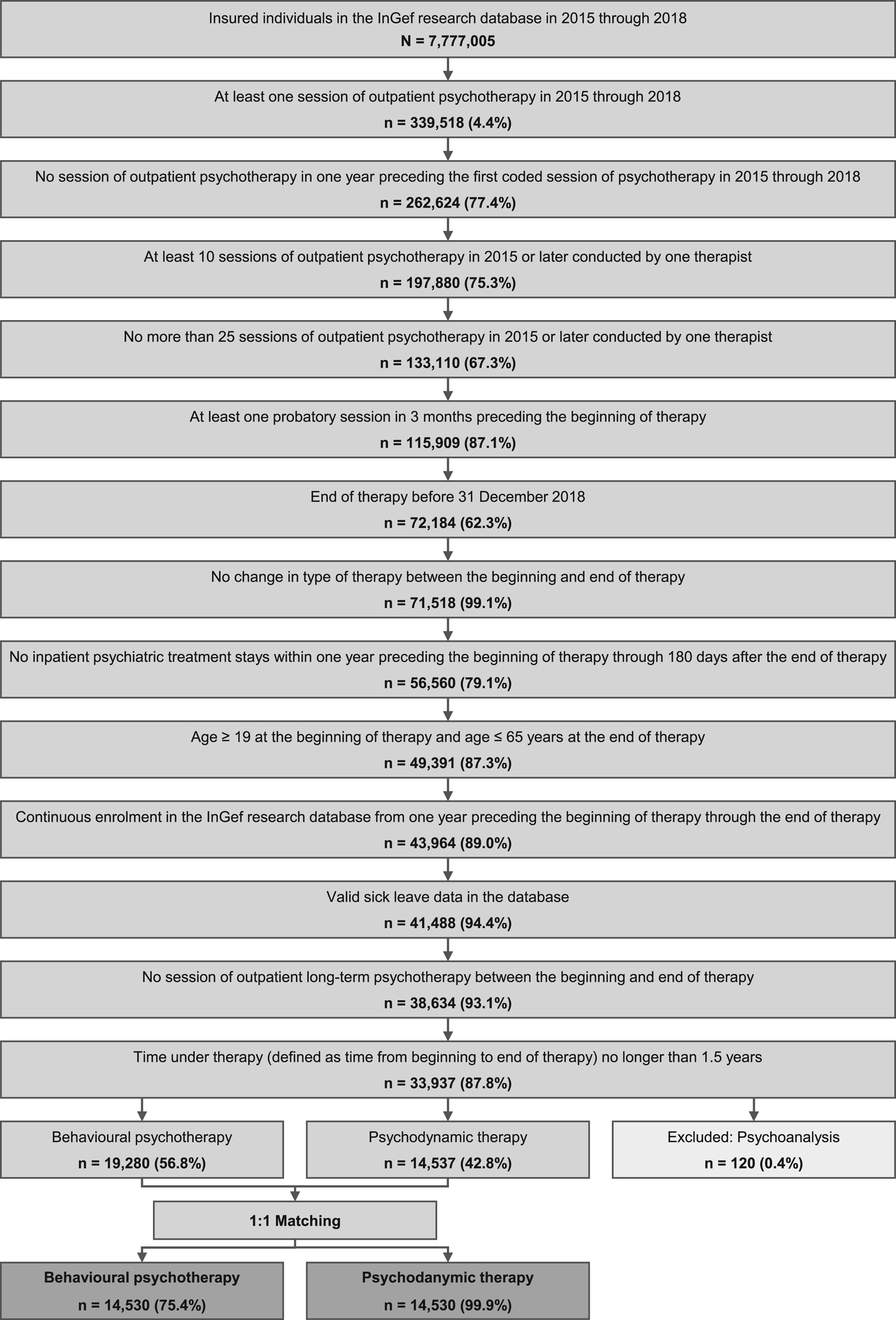
Figure 1. Flowchart of the sample identification process.
Baseline period started one year before cohort entry. Cohort entry was defined as the beginning of psychotherapy. Cohort exit was defined as one year after the end of treatment, end of continuous insurance period, or death, whatever comes first.
Outcomes
Outcome of interest were sick leave days determined for three periods: (1) within one year preceding the beginning of treatment (before therapy), (2) from the beginning to the end of treatment (during therapy), and (3) within one year following the end of treatment (after therapy). Days in hospital were considered as sick leave days, too. The primary outcome was the difference in duration of sick leave from (1) before the beginning to (3) after the end of psychotherapy. As a secondary outcome, the difference in duration of sick leave from before to during therapy was determined. As additional secondary outcomes, duration of sick leave with coded mental disorders (ICD-10-GM codes beginning with ‘F’) and total direct health care costs were determined following the same approach as for the duration of sick leave. Direct health care costs were attained as the sum of costs for outpatient and inpatient procedures as well as dispensed medication costs from a health care provider perspective. Costs for psychotherapy were assessed as all outpatient treatments with billed codes for psychotherapy or application-free sessions (online Supplementary Table S2). We additionally assessed the indication for psychotherapy as the ICD-10-GM chapter ‘mental and behavioral disorders’ (F00–F99) diagnoses billed by the clinical practitioner at the end of psychotherapy.
Statistical analysis
We conducted a propensity score (PS) matching to balance psychotherapy groups (Austin, Reference Austin2011). The PS was estimated by a logistic regression model and was defined as the probability of a psychodynamic therapy conditional on sociodemographic (age, sex) and clinical variables such as severe mental illnesses (SMI; Schneider, Erhart, Hewer, Loeffler, and Jacobi, Reference Schneider, Erhart, Hewer, Loeffler and Jacobi2019), physical illness (cancer; Charlson comorbidity index [CCI]; Sundararajan et al., Reference Sundararajan, Henderson, Perry, Muggivan, Quan and Ghali2004), and use of psycholeptic and psychoanaleptic drugs (see online Supplementary Table S3 for a detailed description) in the baseline period. A 1:1 matching was performed using the nearest-neighbor approach with a caliper of 0.2 × logit(PS) without replacement, where patients were matched from highest to lowest PS. The balance of patient characteristics between psychotherapy groups was analyzed using standardized mean differences (s.m.d.). An s.m.d. of less than 0.1 was considered a negligible difference.
For the analyses on duration of sick leave, the number of sick leave days were divided by the total person time (in years) to obtain the sick leave rates for all respective observation periods. Rate-differences were calculated for comparisons between both groups for each period, respectively, as well as for comparisons over time with the baseline period as reference. The difference in sick leave rate-differences (DiD) between both treatments over time (from before the beginning to after the end of psychotherapy) was calculated as the primary outcome measure. 95% confidence intervals (CI) for rates, rate differences, and DiDs in the unmatched samples were calculated by the bootstrap method with 1000 replications (Efron & Tibshirani, Reference Efron and Tibshirani1993). For the matched pairs, an adaption of the bootstrap of Austin and Small (Reference Austin and Small2014) was used. The same approach was followed for all secondary outcomes.
Sensitivity analyses
As a sensitivity analysis, all outcomes were analyzed stratified by age and sex, for the unmatched samples, and in subgroups defined by the profession of the respective therapist categorized as psychological, psychiatric, or other medical professions via practitioner-specific medical specialization numbers (also see online Supplementary Table S3).
Results
The study population after the selection process comprised n = 33 937 patients with short-term outpatient psychotherapy. Of these, n = 120 patients were excluded who received psychoanalysis, leading to a final study sample of n = 19 280 patients who received BT and n = 14 537 with PDT. The sample selection process is displayed in the flowchart in Fig. 1.
Sociodemographic and clinical characteristics before and after application of the PS matching are displayed in Table 1. s.m.d.s before matching were small in all variables used for covariate adjustment (s.m.d. = −0.070 to 0.061). After matching, a final sample of n = 14 530 patients in each group remained. s.m.d.s in the variables used for covariate adjustment reduced to −0.005 to 0.030. Sex and age were almost similar after matching, i.e., 68.1 and 68.0% were females and the mean age was 42.6 and 42.8 years (s.d. = 11.5/11.5) in patients who received BT and PDT, respectively. Severe major depression and cancer were the most prevalent clinical conditions with 10.6/10.9% and 5.9/6.3% (BT/PDT), respectively, whilst all other disorders and illnesses showed prevalence rates below 2%. Mean CCI was 0.5 (s.d. = 1.1) and 0.6 (s.d. = 1.1) in BT and PDT, respectively, indicating an overall low comorbidity status. Patients who received BT showed fewer treatment sessions (mean = 18.0 v. 18.7 for BT v. PDT, s.m.d. = 0.143) whilst having a longer time under therapy (292.2 v. 282.1 days for BT v. PDT, s.m.d. = −0.136). Both groups showed a mean of 4.6 (s.d. = 1.9/2.0) application-free sessions before treatment. The profession of therapist differed in terms of a greater share of psychological therapists in BT patients (92.2 v. 46.4% for BT v. PDT, s.m.d. = −1.144) and more psychiatric (27.6%) and other therapists (26.1%) who conducted PDT. In both groups, most psychotherapies were conducted for affective (ICD-10-GM F30-F39: 46.6/50.5% for BT/PDT) or neurotic, stress-related, and somatoform disorders (ICD-10-GM F40-F48: 61.4/60.1% for BT/PDT; see online Supplementary Table S4).
Table 1. Baseline characteristics and balance before and after matching of patients who received behavioral psychotherapy (BT) and psychodynamic therapy (PDT)
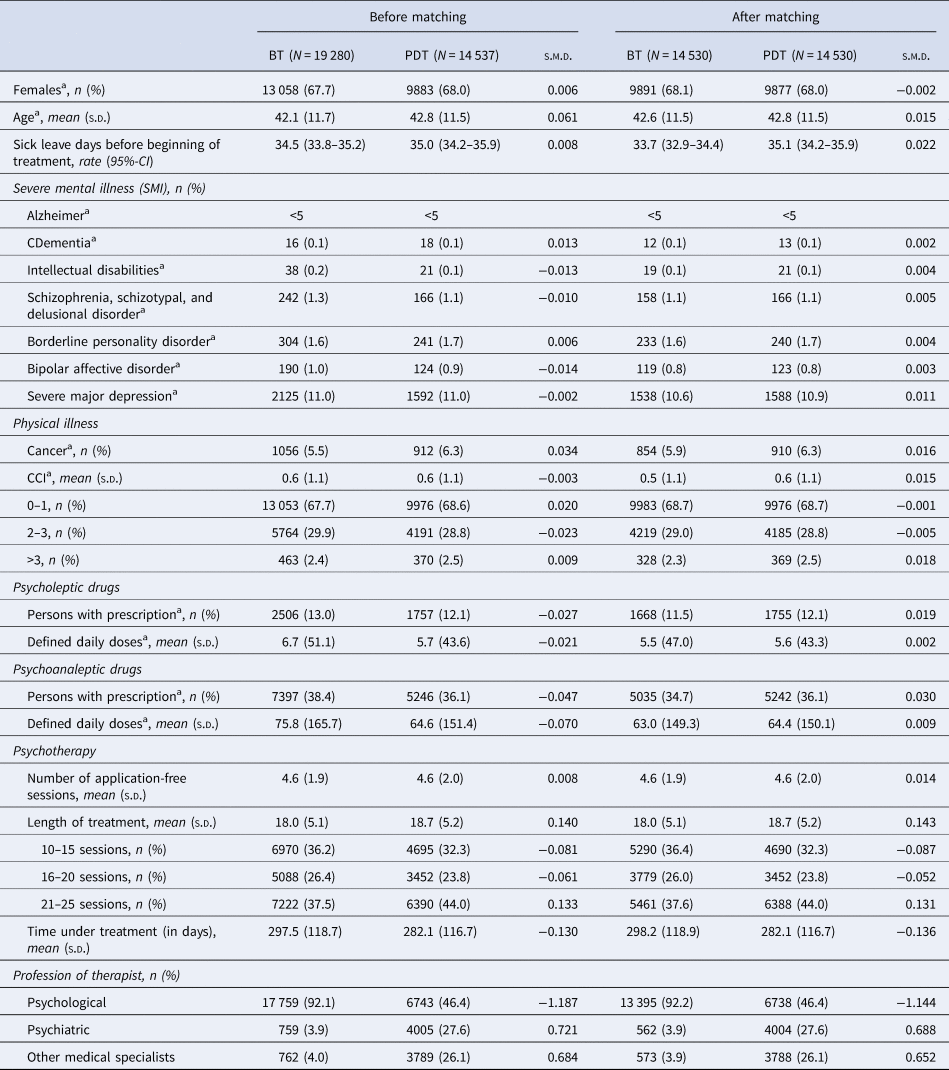
BT, Behavioral psychotherapy; PDT, Psychodynamic therapy; s.d., Standard deviation; s.m.d., Standardized mean difference; rate, sum of sick leave days divided by person-time in years; 95%-CI, 95% confidence interval calculated by the bootstrap method; CCI, Charlson comorbidity index.
a Variables marked with an a were included in the propensity score matching.
Sick leave
Results on primary and secondary outcomes are presented in Table 2. We found no difference between patients who received BT and PDT in rate-differences of sick leave days over time from before to after treatment (DiD = −0.48, 95%-CI −1.61 to 0.68). Both patients who received BT and PDT showed reductions in sick leave days in terms of rate-differences of −13.63 (95%-CI −14.49 to −12.80) and −14.11 (95%-CI −14.99 to −13.30) from before to after treatment, respectively. Patients who received BT showed smaller rates of sick leave days per year compared to PDT in one year before therapy (33.66/35.05 for BT/PDT; rate-difference = 1.39, 95%-CI 0.31–2.47), during therapy (35.99/39.74 for BT/PDT; rate-difference = 3.75, 95%-CI 2.36–5.08), as well as one year after therapy (20.03/20.95 for BT/PDT; rate-difference = 0.92, 95%-CI 0.11–1.70). Compared to before therapy, patients who received PDT showed a greater rise in sick leave days from before to during therapy (2.33/4.69 for BT/PDT; DiD = 2.36, 95%-CI 1.14–3.52). All trends remained stable regardless of age and sex, except for overall higher sick leave days and costs in older persons and males (see online Supplementary Tables S5–S9). A sensitivity analysis for the unmatched samples (online Supplementary Table S10) showed similar results in most time periods and comparisons.
Table 2. Sick leave days (overall and with coded mental disorders) and health care costs before, during, and after treatment in comparison between patients who received behavioral psychotherapy (BT) and psychodynamic therapy (PDT) as well as comparison over time for the matched samples
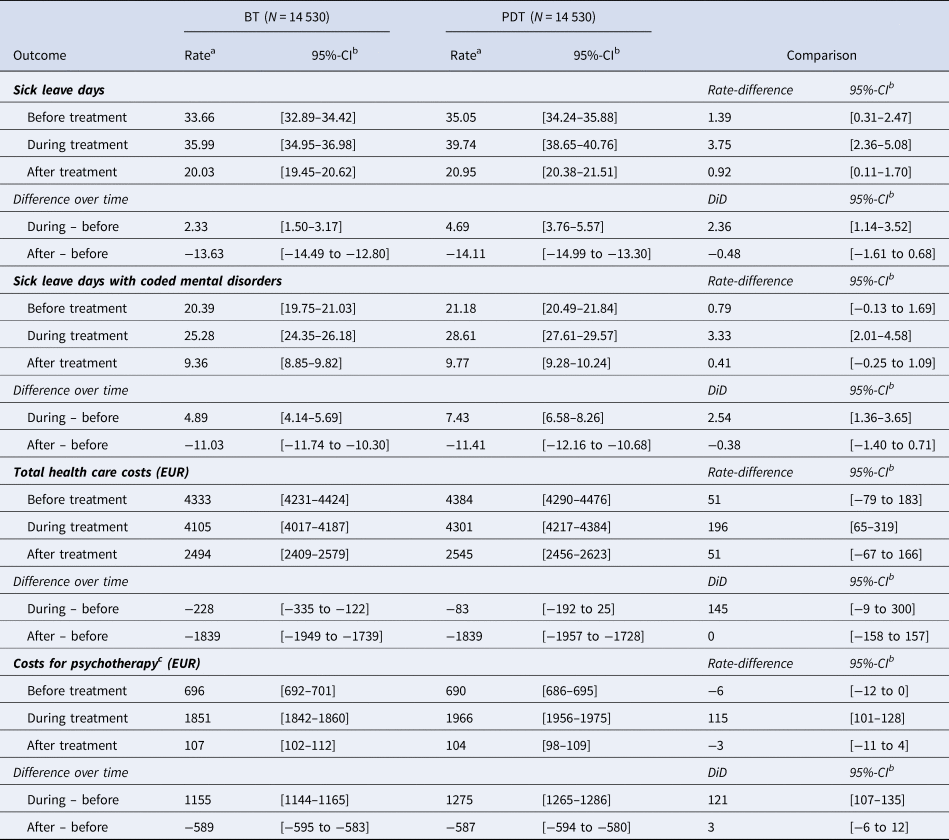
BT, Behavioral psychotherapy; PDT, Psychodynamic therapy; DiD, Difference in rate-differences over time.
a Rates were calculated by dividing the sum of a respective outcome over the total person time in years.
b 95%-Confidence intervals were calculated by the bootstrap method for matched samples (Austin & Small, Reference Austin and Small2014) with 1000 replications.
c Costs for outpatient psychotherapy services were assessed as all outpatient cases with codes billed for psychotherapy or application-free diagnostic sessions. A full list of the referenced codes is reported in online Supplementary Table S2.
Sick leave with coded mental disorders
Same trends as in total sick leave days can be seen in sick leave days with coded mental disorders, except for negligent differences between groups before and after treatment (rate-differences = 0.79 and 0.41). Patients with BT/PDT showed sick leave rates with coded mental disorders of 20.39/21.18 days before, 25.28/28.61 days during, and 9.36/9.77 days after psychotherapy, respectively, indicating a stable level of roughly 10–14 days of sick leave for other conditions (Table 2).
Direct health care and psychotherapy costs
Patients who received BT showed similar direct health care costs as patients who received PDT before (4333/4384 EUR for BT/PDT) and after therapy (2494/2545 EUR for BT/PDT). During therapy, costs were lower in patients who received BT (4105/4301 EUR for BT/PDT; rate-difference = 196 EUR, 95%-CI 65–319 EUR). In comparison from before to after therapy, both BT and PDT groups showed similar reductions in costs of −1839 EUR (DiD = 0 EUR, 95%-CI −158 to 157 EUR). Costs reduced from before to during therapy in both groups as well, but to a lesser extent (−228/−83 EUR for BT/PDT; rate-difference = 145 EUR, 95%-CI −9 to 300 EUR; Table 2).
Of the total direct costs, the costs for outpatient psychotherapeutic services accounted for roughly 16% before, 45% during, and 4% after treatment. There was no difference between groups before and after treatment, whereas costs for psychotherapy were slightly higher in patients who received PDT during treatment compared to BT (1851/1966 EUR for BT/PDT; rate-difference = 115 EUR, 95%-CI 101 to 128 EUR).
Sensitivity analyses by profession of therapist
Sensitivity analyses depending on the profession of the conducting therapist showed same trends in both treatment groups over time with only partly diverging extents (online Supplementary Tables S11–S13). Sick leave rates were overall highest in patients who were treated by psychiatric therapists (online Supplementary Table S12), especially during therapy compared to the whole study population (48.25 v. 35.99 for BT, 44.26 v. 39.74 for PDT). Accordingly, there was a greater increase in sick leave days from before to during therapy in patients who received BT compared to PDT by a psychiatric therapist (DiD = −6.63, 95%-CI −11.64 to −1.22), whereas the decrease from before to after was similar in both groups (DiD = 1.58, 95%-CI −2.90 to 6.44). Patients who were treated by other therapists (online Supplementary Table S13) showed higher sick leave rates and health care costs for PDT before and during therapy, resulting in a stronger decline in sick leave days in patients who received PDT from before to after therapy (DiD = −5.44, 95%-CI −9.61 to −1.23).
Discussion
Interpretation of results
This study sought to analyze the change in sick leave over a patient journey from one year preceding the beginning through one year after the end of outpatient short-term BT and PDT. Both patients who received BT and PDT showed a reduction of 13.63 and 14.11 sick leave days per year, respectively, or roughly 40%, from before to after therapy, with a non-significant DiD of −0.48 (CI −1.61 to 0.68) between groups. Similarity in sick leave differences over time between both treatments is consistent with findings from primary research and RCT studies which support similar treatment effects in outpatient short-term psychotherapies for both BT and PDT (Abbass et al., Reference Abbass, Town, Holmes, Luyten, Cooper, Russell and Kisley2020; Driessen et al., Reference Driessen, Hegelmaier, Abbass, Barber, Dekker, Van and Cuijpers2015; Leichsenring et al., Reference Leichsenring, Luyten, Hilsenroth, Abbass, Barber, Keefe and Steinert2015; Steinert et al., Reference Steinert, Munder, Rabung, Hoyer and Leichsenring2017). Of note, BT was found to be slightly more effective than PDT in RCT studies for some disorders, e.g., stronger short-term effects of BT in social anxiety disorders (Leichsenring et al., Reference Leichsenring, Salzer, Beutel, Herpertz, Hiller, Hoyer and Leibing2013) or obsessive compulsive disorders without evidence for PDT (Leichsenring & Steinert, Reference Leichsenring and Steinert2016). The extent of reductions in sick leave is in accordance with results from a previous study on sick leave using claims data (Epping et al., Reference Epping, de Zwaan and Geyer2018). Compared to meta-analyses (Nieuwenhuijsen et al., Reference Nieuwenhuijsen, Verbeek, Neumeyer-Gromen, Verhoeven, Bültmann and Faber2020; Nigatu et al., Reference Nigatu, Liu, Uppal, McKinney, Rao, Gillis and Wang2016; Salomonsson et al., Reference Salomonsson, Hedman-Lagerlöf and Öst2018), our results suggest stronger reductions in sick leave and, thus, possibly more positive effects for psychotherapies. Despite positive trends, psychotherapeutic interventions may be further improved by the implementation of modules focused on return-to-work (Kröger et al., Reference Kröger, Bode, Wunsch, Kliem, Grocholewski and Finger2015; Lagerveld, Blonk, Brenninkmeijer, Wijngaards-de Meij, & Schaufeli, Reference Lagerveld, Blonk, Brenninkmeijer, Wijngaards-de Meij and Schaufeli2012).
Sick leave rates of 33.66 and 35.05 days per year before the beginning of treatment for patients who received BT and PDT, respectively, are in accordance with a mean of 34 yearly days of sick leave in German patients with mental disorders (Bundespsychotherapeutenkammer, 2015). In both groups, patients showed roughly 20 sick leave days with coded mental disorders before treatment. These baseline sick leave rates indicate a considerable mental health burden preceding psychotherapy. Sick leave rates increased from before to during therapy in both groups (2.33/4.69 days for BT/PDT), whilst more in patients who received PDT (DiD = 2.36). This increase could be explained by adverse treatment effects (Bystedt, Rozental, Andersson, Boettcher, & Carlbring, Reference Bystedt, Rozental, Andersson, Boettcher and Carlbring2014; Duggan, Parry, McMurran, Davidson, & Dennis, Reference Duggan, Parry, McMurran, Davidson and Dennis2014), the higher share of psychological therapists in patients who received BT which cannot directly ascertain sick leave certificates due to legal prerequisite in Germany in contrast to psychiatrists or other physicians, or symptom worsening while waiting for treatment. Due to high demand, patients seeking psychotherapy in Germany have to wait roughly 20 weeks from first contact until the first session of psychotherapy (Nübling et al., Reference Nübling, Bär, Jeschke, Ochs, Sarubin and Schmidt2014). Untreated mental illness during this waiting time, which falls within the baseline period before therapy, could result in symptom worsening and, thus, also higher sick leave rates after the beginning of treatment (Alonso, Marco, & Andani, Reference Alonso, Marco and Andani2018; Marco, Alonso, & Andani, Reference Marco, Alonso and Andani2020). Reducing the time to treatment may reduce sick leave and benefit treatment outcomes (Reichert & Jacobs, Reference Reichert and Jacobs2018).
In total direct health care costs, patients who received both BT and PDT showed 1839 EUR, or roughly 40%, lower costs after treatment compared to before. The costs for psychotherapeutic services accounted for roughly 45% during and 16% before therapy, the latter mostly attributable to application-free diagnostic sessions. Considering a possibly strong association between sick leave and health care utilization and resulting costs, the equivalent trend in direct costs and sick leave is not surprising and further supports a similarity in treatment effects for both BT and PDT. These results are also in accordance with cost-effectiveness analyses of short-term outpatient psychotherapies and health economic studies on mental disorders (Bode, Götz von Olenhusen, Wunsch, Kliem, & Kröger, Reference Bode, Götz von Olenhusen, Wunsch, Kliem and Kröger2017; Bothe, Jacob, Kröger, & Walker, Reference Bothe, Jacob, Kröger and Walker2020; Mukuria et al., Reference Mukuria, Brazier, Barkham, Connell, Hardy, Hutten and Parry2013; Radhakrishnan et al., Reference Radhakrishnan, Hammond, Jones, Watson, McMillan-Shields and Lafortune2013; Yonatan-Leus, Strauss, & Cooper-Kazaz, Reference Yonatan-Leus, Strauss and Cooper-Kazaz2021). Contrarily to increasing sick leave days from before to during treatment, patients who received PDT showed similar (4383 v. 4301 EUR) and patients who received BT slightly lower costs (4333 v. 4105 EUR) during therapy compared to before. Before treatment beginning, most health care costs (84%) accounted for non-psychological and non-psychiatric treatments, while during therapy, a large share of costs (45%) is accounted for by outpatient psychotherapy. This suggests more health care utilizations not targeting the relevant mental illness before therapy and a reduction in the need for unspecific treatments while receiving psychotherapy.
The largest share (92%) of patients who received BT were treated by psychotherapists whereas PDT was less often conducted by psychotherapists (46%), followed by psychiatrists (28%) and other medical specialists (26%). This can be interpreted as a strong dominance of BT in psychology and more interest in PDT in the medical field. Sensitivity analyses depending on the profession of therapists showed overall similar developments of sick leave days over time in all groups while sick leave rates were overall highest in psychiatric therapists. We could hypothesize that several factors are responsible for differences between groups, e.g., different mental illnesses, patients' choices for a certain type of treatment, professional choices in patient selection, and medical specialists' legal prerequisite to ascertain sick leave certificates. Interpretability of these results is limited due to small and diverging sample sizes and, thus, further research is necessary.
Limitations
Several limitations of this study must be taken into account. First, we cannot include information on symptom severity, symptom reduction, or remission as a treatment effect in this study but only assess sick leave rates as a surrogate parameter of overall health. Considering sick leave to be economically assessable via claims data in large samples and sick leave being associated with overall health and functioning in mental disorders (Volz et al., Reference Volz, Bartečků, Bartova, Bessa, De Berardis, Dragasek and Kasper2022), we argue that this study offers valuable information and indicators of a patient's journey regarding their sick leave and health. Second, we cannot assume differences in sick leave days over time, i.e., strong reductions from before to after therapy, to be a direct effect of BT or PDT. The design of this study restricts interpretability to group differences and description of differences over time. Third, residual confounding due to disease severity or factors interfering with patients' or practitioners' choices for a certain type of psychotherapy cannot be ruled out. We tried to take these factors into account by using a PS matching including available information on severe physical and mental illness in order to adjust for confounding. Fourth, we assessed data only from the InGef research database and limited generalizability cannot be ruled out. No information on early retirement, socio-economic background, and employment status are available in the data which could not be considered in the PS matching nor the group comparisons. Additionally, we could only assess sick leave reported to SHIs which probably do not cover short-term incapacities to work so that overall sick leave is probably underestimated. Fifth, we only addressed patients who fulfilled conservative selection criteria depicting patients who received outpatient short-term psychotherapy in an ideal setting. The design of the study includes only patients who did not develop further treatment need after a maximum of 25 sessions nor suffered possible following relapse within 180 days after the end of therapy. We did so to enhance external validity of this study's results and comparability to RCT studies. Our findings cannot be generalized to other patient groups receiving inpatient, long-term, or other treatments without further research. Additionally, the chosen in- and exclusion criteria were first developed and used in this study and have not been validated elsewhere yet. To corroborate our approach, we pre-specified and discussed the selection criteria with three psychotherapists before the start of the study to find an agreeable depiction of clinical criteria within claims data. Still, more research on patients receiving treatments for mental illness using claims data is necessary and an implementation of registries could fundamentally improve research on mental illness.
Conclusion
We conducted a cohort study on sick leave before, during, and after treatment on patients who received outpatient short-term behavioral (BT, N = 14 530) or psychodynamic psychotherapy (PDT, N = 14 530). We defined complex selection criteria to assess individuals who received treatments representing a real-world clinical setting, focused on short-term outpatient treatments for external validity, and used a PS matching procedure for confounder adjustment. The results support the little existing evidence of similar reductions in sick leave days in BT and PDT treated patients of roughly 14 days, or 40%, per year as well as reduced direct health care costs from before to after therapy. Sick leave and health economic aspects may pose a crucial and important endpoint in the evaluation of RCT studies and should receive more attention in clinical research. Further research should use a claims-based approach on sick leave for other treatment modalities, e.g., inpatient and long-term treatments, and should strive to identify similar patients without treatment for causal inferential estimations of treatment effects in claims data.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291723003094
Acknowledgements
We greatly thank Martin Holst, Corinna Hartling, and Katharin Meyer for their valuable support in discussing the study design and the chosen in- and exclusion criteria.
Author's contributions
TB, DE, FB, and CK conceptualized and designed the study and study protocol. FB, DE, and TB carried out the data analysis. The manuscript was initially drafted by TB. All authors contributed to data interpretation, critical review, and revision of the manuscript and approved the decision to submit for publication. FB, DE, and TB have accessed and verified the study data. DE oversaw the statistical analysis and all authors vouch for the fidelity of this report to the study protocol and statistical analysis plan. All authors have read and approved the manuscript.
Funding statement
This research was partly funded by the German Federal Ministry for Economic Affairs and Climate Action (FB, DE: project AIR_PTE; funding code 01MJ 20 001B). The funding source was not involved in designing the study, conducting the analyses, interpreting the results, or writing of this manuscript.
Competing interests
CK is a trained behavioral therapist and state-licensed supervisor for psychotherapy. TB is a candidate applicant for behavioral therapy. FB and DE declare no conflicts of interests.
Data availability statement
The data used in this study cannot be made available in the manuscript, the supplementary files, or in a public repository due to German data protection laws (Bundesdatenschutzgesetz). To facilitate the replication of results, the used data will be stored on a secure drive at InGef - Institute for Applied Health Research Berlin. Access to the raw data used in this study can only be provided to external parties under the conditions of a cooperation contract and can be accessed upon request, after written approval ([email protected]), if required.






