Midlife mortality rates in the United States are increasing (Woolf & Schoomaker, Reference Woolf and Schoomaker2019). This increase has been largely attributed to ‘deaths of despair’–including deaths from suicide, drug poisonings, and alcohol-related diseases (Case & Deaton, Reference Case and Deaton2015) – and to a stagnation and subsequent increase in previously declining mortality rates from cardiometabolic conditions (Harris, Majmundar, & Becker, Reference Harris, Majmundar and Becker2021; Shah et al., Reference Shah, Lloyd-Jones, Kandula, Huffman, Capewell, O'Flaherty and Khan2020). These trends have generally been described separately, but they may be driven by similar mechanisms (National Academy of Medicine, 2022; Sterling & Platt, Reference Sterling and Platt2022). Here, we used data from a prospective, nationally representative cohort to characterize the co-occurrence of midlife diseases of despair and cardiometabolic risk and to test adolescent psychopathology as a common precursor to these outcomes.
Diseases of despair comprise interrelated maladies (suicidality, substance misuse, pain, and sleep problems) that increase the risk of death from despair (Brennan et al., Reference Brennan, Moffitt, Ambler, Harrington, Hogan, Houts and Caspi2023). Cardiometabolic risk factors include a cluster of conditions (e.g. hypertension, hyperlipidemia, and high-risk waist circumference) that antedate premature mortality from cardiometabolic diseases. There are reasons to anticipate that these conditions may co-occur in midlife. Both despair-related diseases and cardiometabolic problems are increasing among middle-aged individuals (Case & Deaton, Reference Case and Deaton2022; Drozdz et al., Reference Drozdz, Alvarez-Pitti, Wójcik, Borghi, Gabbianelli, Mazur and Wühl2021; Gaydosh et al., Reference Gaydosh, Hummer, Hargrove, Halpern, Hussey, Whitsel and Harris2019; O'Hearn, Lauren, Wong, Kim, & Mozaffarian, Reference O'Hearn, Lauren, Wong, Kim and Mozaffarian2022). Further, they can have interactive effects: sleep problems, pain, and substance misuse increase cardiometabolic risk, and cardiometabolic problems such as obesity can lead to more pain, sleep, and mental-health difficulties (Abdul-Rahman, Card, Grainge, & Fleming, Reference Abdul-Rahman, Card, Grainge and Fleming2018; Beccuti & Pannain, Reference Beccuti and Pannain2011; Deste & Lombardi, Reference Deste and Lombardi2023; Fayaz, Ayis, Panesar, Langford, & Donaldson, Reference Fayaz, Ayis, Panesar, Langford and Donaldson2016; Gan et al., Reference Gan, Buxton, Scheuermeyer, Palis, Zhao, Desai and Slaunwhite2021; Ge et al., Reference Ge, Guyatt, Tian, Pan, Chang, Chen and Yang2019; Michal & Beutel, Reference Michal and Beutel2021; Vgontzas et al., Reference Vgontzas, Bixler, Tan, Kantner, Martin and Kales1998). Although the literature supports the hypothesis that midlife diseases of despair and cardiometabolic risk may co-occur, their degree of co-occurrence has not been empirically tested in a general-population sample.
Adolescent psychopathology is an under-investigated origin of adult health that may contribute to both midlife diseases of despair and cardiometabolic risk (Beseran et al., Reference Beseran, Pericàs, Cash-Gibson, Ventura-Cots, Porter and Benach2022; Brennan et al., Reference Brennan, Moffitt, Ambler, Harrington, Hogan, Houts and Caspi2023). Recent findings in a New Zealand cohort suggest that adolescents who experience psychopathology are at elevated risk for a syndrome of despair-related problems in midlife (Brennan et al., Reference Brennan, Moffitt, Ambler, Harrington, Hogan, Houts and Caspi2023). In addition, young people with mental-health problems tend to have poorer physical health and higher mortality in middle adulthood (Bourassa et al., Reference Bourassa, Moffitt, Ambler, Hariri, Harrington, Houts and Caspi2022; Ploubidis, Batty, Patalay, Bann, & Goodman, Reference Ploubidis, Batty, Patalay, Bann and Goodman2021), and adolescent psychological distress may increase the risk for midlife cardiometabolic conditions (Boehm, Qureshi, & Kubzansky, Reference Boehm, Qureshi and Kubzansky2022; Goldstein & Korczak, Reference Goldstein and Korczak2020). However, to our knowledge, there has been no prospective study of the association of adolescent psychopathology with despair-related diseases in the United States, where deaths of despair are most prevalent. It also remains unclear to what extent adolescent psychopathology may serve as a common contributor to both midlife despair-related diseases and cardiometabolic risk. Further, little is known about the mechanisms that may link adolescent psychopathology to midlife morbidity.
The primary aims of this study were to use a U.S. nationally representative sample to test (1) whether adolescent psychopathology is a common antecedent of midlife despair-related diseases and cardiometabolic risk, (2) whether truncated education partially accounts for associations of adolescent psychopathology with midlife morbidity, (3) the extent to which despair-related diseases and cardiometabolic risk co-occur in middle adulthood, and (4) the extent to which any co-occurrence is accounted for by adolescent psychopathology. Because early-life socioeconomic circumstances and cognitive ability shape risk for both despair-related diseases and cardiometabolic problems (Beseran et al., Reference Beseran, Pericàs, Cash-Gibson, Ventura-Cots, Porter and Benach2022; Gottfredson, Reference Gottfredson2004; Phelan, Link, Diez-Roux, Kawachi, & Levin, Reference Phelan, Link, Diez-Roux, Kawachi and Levin2004; Wang et al., Reference Wang, Ye, Kong, Zheng, Xu, Xu and Wang2023b; Wang, Li, & Zheng, Reference Wang, Li and Zheng2023a), our analyses adjusted for adolescent socioeconomic status (SES) and cognitive ability. To provide a benchmark for adolescent psychopathology's associations with midlife morbidity, we also tested associations of adolescent physical health with midlife diseases of despair and cardiometabolic risk.
First, we hypothesized that adolescents who experienced psychopathology would have more midlife indicators of despair-related diseases and cardiometabolic risk. Second, we hypothesized that low education would mediate associations of adolescent psychopathology with midlife morbidity (Case & Deaton, Reference Case and Deaton2015, Reference Case and Deaton2022; Kessler, Avenevoli, & Ries Merikangas, Reference Kessler, Avenevoli and Ries Merikangas2001). Despair-related diseases and deaths are concentrated among Americans with low education (Case & Deaton, Reference Case and Deaton2015; Copeland et al., Reference Copeland, Gaydosh, Hill, Godwin, Harris, Costello and Shanahan2020), and psychopathology may impede adolescents' ability to engage with schooling, adversely impacting role transitions and placing them on a trajectory toward poor midlife outcomes (Case & Deaton, Reference Case and Deaton2022; Kessler et al., Reference Kessler, Avenevoli and Ries Merikangas2001). Finally, we hypothesized that midlife diseases of despair and cardiometabolic risk would co-occur, with adolescent psychopathology accounting for a portion of this co-occurrence.
If adolescent psychopathology precipitates midlife diseases of despair and cardiometabolic risk, it would be an important prevention target. In addition, identifying adolescent psychopathology as a common contributor to these outcomes could help to identify shared mechanisms underlying rising midlife mortality. Even if the association is not causal, establishing a prospective link would identify adolescent psychopathology as an early-warning sign for poor midlife health and premature death.
Methods
Participants
Participants were drawn from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative cohort of adolescents, grades 7–12, in the United States who were recruited in 1994–1995 (N = 20 745) and followed to middle adulthood. Add Health has followed participants across five assessment waves, most recently at ages 33–43 years (response rate = 71.8%). Detailed information about the Add Health study has been previously reported (Harris et al., Reference Harris, Halpern, Whitsel, Hussey, Killeya-Jones, Tabor and Dean2019; Harris & Halpern, Reference Harris and Halpern2022).
Study outcomes included indicators assessed within the Wave V biomarker sample (n = 5381). Our analytic sample therefore included individuals who were in the biomarker sample and who had information on study variables (n = 4578).
Measures
Detailed information concerning measure definitions is provided in online Supplemental Table S1. The assessment schedule is shown in Fig. 1.
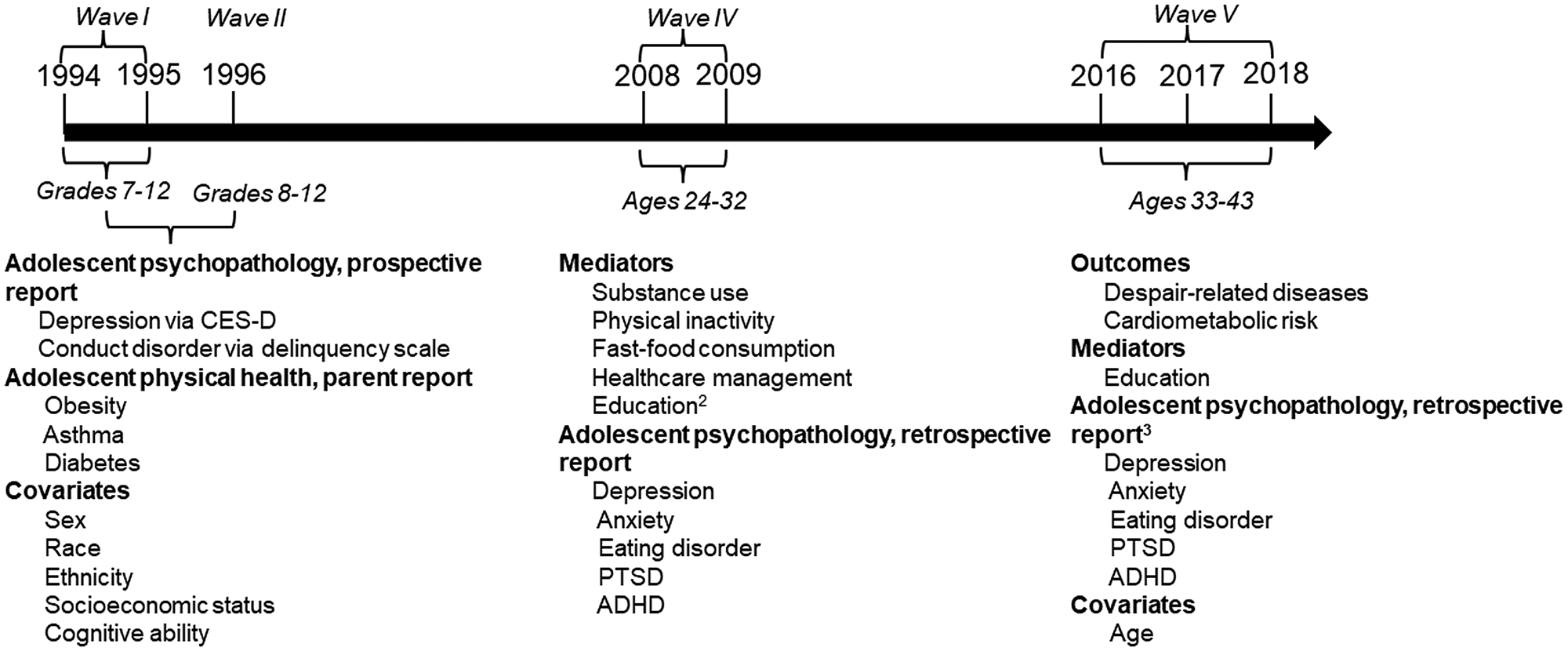
Figure 1. Measures and corresponding waves from the National Longitudinal Study of Adolescent to Adult Health.1
1 Only waves from which data were drawn are shown.
2 Education information from Wave IV was only used if Wave V information was unavailable.
3 Retrospective reports of adolescent psychopathology from Wave V were only used if Wave IV information was unavailable.
Adolescent psychopathology
We assessed internalizing and externalizing conditions occurring between ages 11 and 18 years. Prospective assessments were used when available and were supplemented with retrospective reports. Depression and conduct disorder were assessed prospectively at Waves I and II, using the Center for Epidemiological Studies Depression Scale (CES-D) (Blodgett et al., Reference Blodgett, Lachance, Stubbs, Co, Wu, Prina and Cosco2021) and an 11-item delinquency scale corresponding to DSM-IV criteria, respectively (Miles, van den Bree, & Pickens, Reference Miles, van den Bree and Pickens2002). CES-D scores were pro-rated to 20 items and standard depression cut-offs of 22 and 24 were used to identify depression in males and females, respectively (Roberts, Lewinsohn, & Seeley, Reference Roberts, Lewinsohn and Seeley1991). Consistent with DSM-IV criteria, adolescents with three or more conduct-disorder indicators were classified as having conduct disorder. Retrospective reports of depression, anxiety, PTSD, eating disorders, and ADHD were ascertained at Waves IV and V. To reduce risk of retrospective-reporting bias, Wave V assessments were used only if Wave IV data were unavailable. Retrospective reports of psychopathology were assessed using the question, ‘Has a doctor, nurse, or other health care provider ever told you that you have or had X condition?’ We limited to diagnoses made between ages 11 and 18 using the question, ‘How old were you when you were diagnosed by a doctor, nurse, or other health care provider with X condition?’
We created indicators for any adolescent psychopathology, any internalizing psychopathology (depression, anxiety, PTSD, and eating disorder), and any externalizing psychopathology (conduct disorder, ADHD). A sum score of the number of adolescent mental-health conditions was also created.
Adolescent physical health
We focused on adolescent physical-health problems that, like mental-health conditions, are potentially treatable or manageable. These included obesity, diabetes, and asthma. Parent reports of physical-health conditions at Wave I were used if available; otherwise, retrospective self-reports at Wave IV or V were used. An indicator for any adolescent physical-health problem and a sum score of the number of physical-health problems were created.
Midlife diseases of despair
At Wave V, when participants were 33–43 years old, we assessed eight indicators of despair-related diseases across four domains including suicidality, substance misuse, sleep problems, and pain (Brennan et al., Reference Brennan, Moffitt, Ambler, Harrington, Hogan, Houts and Caspi2023). Suicide-related indicators included self-reported (1) suicidal ideation and (2) suicide attempts in the past year. Substance-misuse indicators included (1) binge drinking 3 + times a week in the past 12 months, and (2) other illicit or prescribed drug misuse in the past 30 days. Sleep problems included (1) trouble falling asleep 5+ times per week in the past 4 weeks, and (2) typically sleeping less than 5 hours per night. Pain indicators were derived from past 4-week medication use: (1) narcotic use, and (2) non-steroidal anti-inflammatory drug use. Indicators were summed to create a score (possible range = 0–8). Participants had between 0 and 6 indicators of despair-related diseases. However, due to small counts, individuals with 4 or more despair indicators were collapsed into a single category.
Midlife cardiometabolic risk
We assessed five indicators of cardiometabolic risk at Wave V: hypertension, hyperlipidemia, high-risk waist circumference, diabetes, and any cardiovascular diagnosis (blood clots, heart disease, heart failure, stroke, or heart attack). Hypertension, diabetes, and hyperlipidemia were assessed across multiple modalities including biomarker data, medication use for the condition in the prior four weeks, and self-reported diagnoses. Participants with a high-risk waist circumference included females with a waist circumference greater than 88 cm and males with a waist circumference greater than 102 cm (‘Executive Summary of the Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults,’, 1998). Cardiometabolic-risk indicators were summed to create a score ranging from 0 to 5. Due to small counts, individuals with 4 or 5 indicators were collapsed into a single category.
Mediators
Low education was the primary, prespecified mediator of interest. We defined low education as a high-school education or less, as reported at Wave V (Case & Deaton, Reference Case and Deaton2015). Wave IV education information was used for those without Wave V information. We also assessed secondary mediators at Wave IV: early-adult substance use, physical inactivity, fast-food consumption (as a proxy for diet), and healthcare management.
Covariates
Covariates included sex, race, ethnicity, SES, and cognitive ability (all assessed at Wave I), and age (assessed at Wave V).
Statistical analysis
First, we tested associations of adolescent psychopathology and adolescent physical health with midlife outcomes. We estimated incidence rate ratios (IRRs) using negative-binomial regression models for despair-related diseases and Poisson regression models for cardiometabolic risk. Negative-binomial regression was used to account for over-dispersion of the sum score for despair-related diseases. Baseline models controlled for age, sex, race, and ethnicity. Adjusted models further controlled for adolescent SES and adolescent cognitive ability.
Second, we used mediation analysis to test whether associations of adolescent psychopathology with midlife outcomes were mediated by low education. Secondary analyses tested mediation by early-adult substance use, physical inactivity, fast-food consumption, and healthcare management (De, Sondhi, Bhattacharjee, & Joshi, Reference De, Sondhi, Bhattacharjee and Joshi2024; Goldstein & Korczak, Reference Goldstein and Korczak2020). Bootstrapped confidence intervals (500 iterations) were used. Mediation analyses were conducted on the full analytic sample (n = 4578) using Monte Carlo integration so that participants with missing information on mediators could be included in analyses.
Third, we used Poisson regression models to test the co-occurrence of midlife despair-related diseases with cardiometabolic risk. Despair-related disease was modeled as the exposure because (1) it was our primary construct of interest and (2) there is evidence that cardiometabolic problems may follow from despair-related problems such as substance misuse (Gan et al., Reference Gan, Buxton, Scheuermeyer, Palis, Zhao, Desai and Slaunwhite2021). We tested their co-occurrence before and after adjusting for adolescent psychopathology–independently, and together with adolescent SES and cognitive ability.
To generate nationally representative estimates, analyses accounted for the Add Health complex survey design including stratification, clustering, and sampling weights. Wave V biomarker-sample weights were used. SAS version 9.4 (SAS Institute Inc, 2016) and MPlus version 8 (Muthén & Muthén, Reference Muthén and Muthén1998–2017) were used for statistical analyses.
The analysis plan for this project was preregistered at https://sites.lsa.umich.edu/richmond-rakerd-lab/project-proposals/.
Results
Sample characteristics
The analytic cohort (n = 4578) was, on average, 37.2 (s.d. = 1.9) years old at Wave V. Of the analytic cohort, 49.3% were male, 73.2% were White, and 10.6% were Hispanic (Table 1). 30.3% of participants were identified as having adolescent psychopathology, and 18.1% had at least one physical-health problem in adolescence (Table 1).
Table 1. Weighted descriptive statistics for study variables
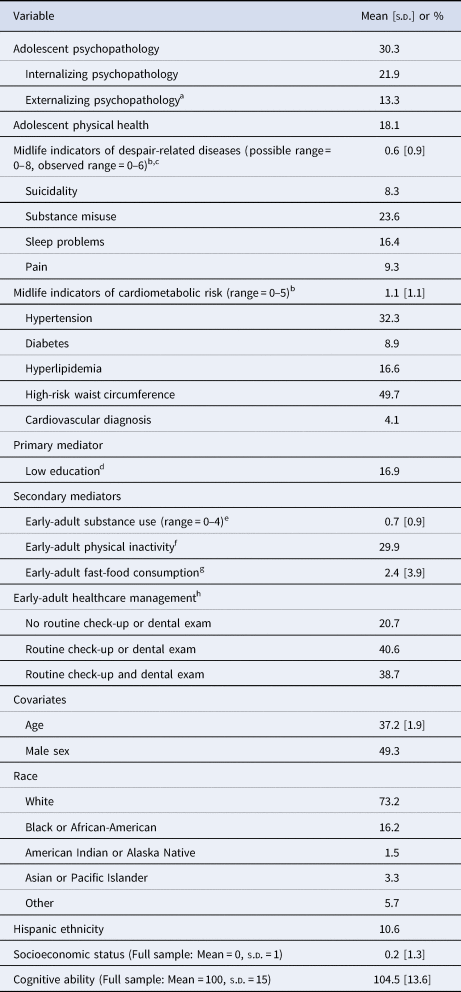
Weighted mean and standard deviation [s.d.] presented for continuous or count variables. Weighted prevalence presented for categorical variables. Analytic n = 4578, except where otherwise noted.
a Seven participants were missing information on externalizing mental-health conditions (analytic n = 4571).
bNon-collapsed versions of sum scores were used to calculate the mean and standard deviation.
cWeighted prevalence estimates for each domain of despair are reported. Prevalence estimates indicate the percentage of individuals with at least one (of two) indicators within the domain.
d One participant was missing information on education level (analytic n = 4577).
e 182 participants were missing information on substance use at Wave IV (analytic n = 4396).
f 185 participants were missing information on physical inactivity at Wave IV (analytic n = 4393).
g 187 participants were missing information on fast-food consumption at Wave IV (analytic n = 4391).
h 182 participants were missing information on healthcare management at Wave IV (analytic n = 4396).
Associations of adolescent psychopathology with midlife diseases of despair
Adolescents who experienced psychopathology tended to experience more despair-related diseases in middle adulthood, even after adjusting for demographics, adolescent SES, and adolescent cognitive ability (Fig. 2a). After accounting for covariates, adolescents with psychopathology had 1.67 [1.46–1.87] times the number of indicators of despair-related diseases than those without psychopathology. The magnitude of the association was similar for internalizing (IRR = 1.65 [1.45–1.86]) and externalizing (IRR = 1.62 [1.35–1.89]) conditions. In addition, after adjusting for covariates, adolescents who experienced more mental-health conditions tended to experience more midlife indicators of despair (IRR = 1.50 [1.38, 1.61]; Table 2). In supplemental analyses using all Wave V respondents (with information on study variables; n = 10342), associations of adolescent psychopathology with midlife despair-related diseases were modestly attenuated, but robust (online Supplemental Table S4). Associations remained evident when limiting to prospective measures of adolescent psychopathology (online Supplemental Table S5).
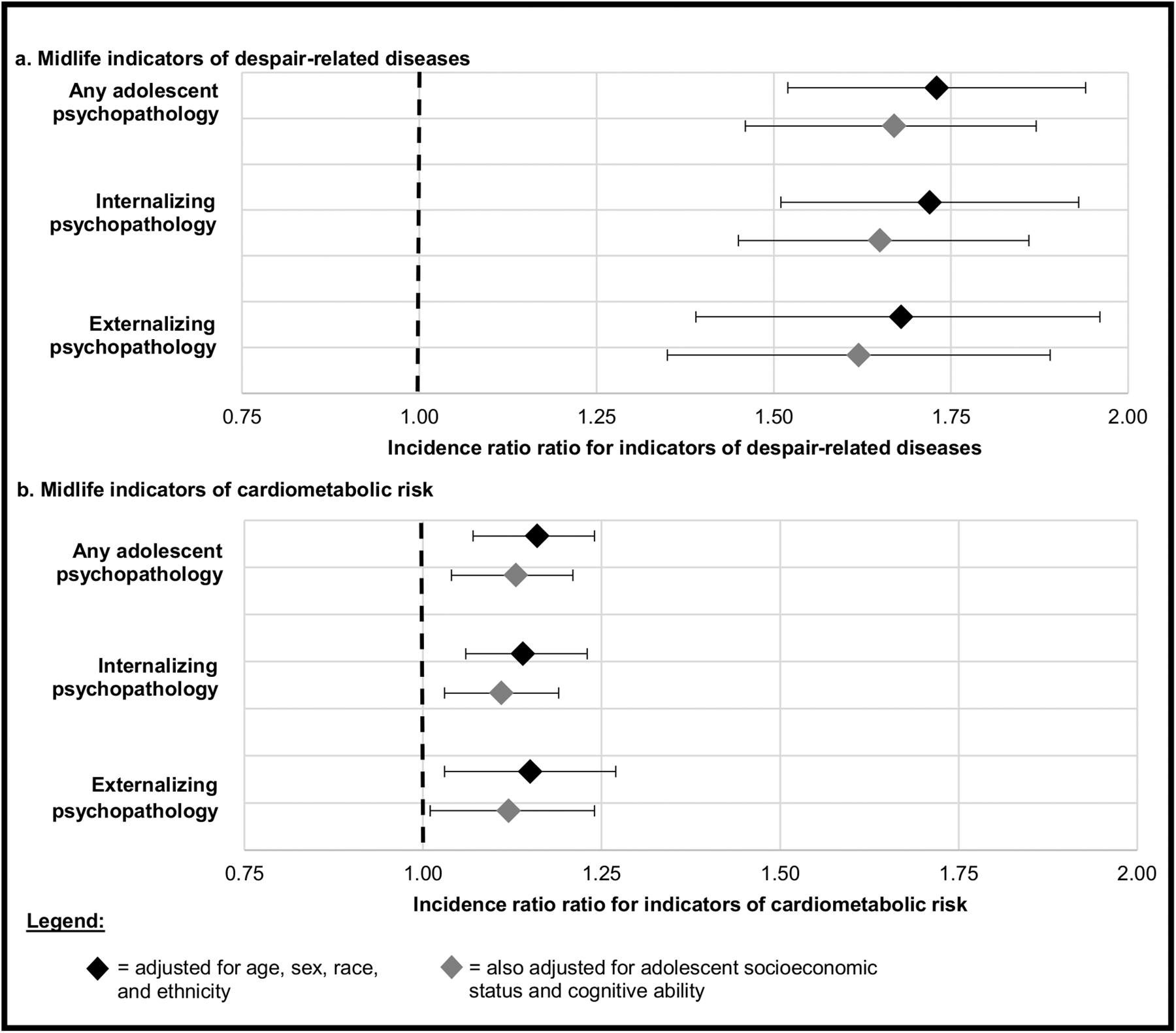
Figure 2. Incidence rate ratios and 95% confidence intervals for associations of adolescent psychopathology with midlife diseases of despair and cardiometabolic risk.
Table 2. Incidence rate ratios (and 95% confidence intervals) for associations of the number of adolescent mental-health conditions with midlife diseases of despair and cardiometabolic risk
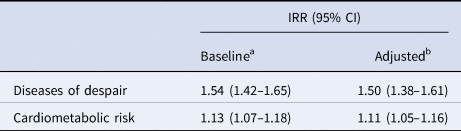
a Baseline models adjusted for demographic factors including age, sex, race, and ethnicity.
b Adjusted models also adjusted for adolescent socioeconomic status and adolescent cognitive ability.
Associations of adolescent psychopathology with midlife cardiometabolic risk
Adolescents who experienced psychopathology tended to experience more indicators of cardiometabolic risk at midlife; this association persisted even after adjustment for demographic factors, adolescent SES, and adolescent cognitive ability (Fig. 2b). After accounting for covariates, adolescents with psychopathology had 1.13 [1.04–1.21] times the number of indicators of cardiometabolic risk than those without psychopathology. The magnitude of the association was similar across internalizing (IRR = 1.11 [1.03–1.19]) and externalizing (IRR = 1.12 [1.01–1.24]) conditions. Adolescents who experienced more mental-health conditions tended to experience more midlife indicators of cardiometabolic risk (Table 2, adjusted IRR = 1.11 [1.05–1.16]). When limiting to only prospective measures of adolescent psychopathology, psychopathology's association with cardiometabolic risk was attenuated, and not statistically significant (online Supplemental Table S5, adjusted IRR = 1.06 [0.97–1.14]).
Associations of adolescent physical health with midlife diseases of despair and cardiometabolic risk
After accounting for demographics, adolescent SES, and adolescent cognitive ability, adolescents with a physical-health condition had more indicators of midlife cardiometabolic risk, but not diseases of despair (IRRs for cardiometabolic risk and diseases of despair = 1.47 [1.36–1.59] and 1.16 [0.98–1.33], respectively; online Supplemental Table S6). Adolescents who experienced more physical-health problems also tended to experience more midlife indicators of cardiometabolic risk (adjusted IRR = 1.44 [1.34–1.54]). In supplemental analyses using all Wave V respondents (n = 10 342), adolescent physical health was significantly associated with midlife despair-related diseases, with an effect size comparable to that in the biomarker sample (adjusted IRR = 1.20 [1.07–1.33]; online Supplemental Table S4).
Testing potential mechanisms linking adolescent psychopathology with midlife outcomes
In primary mediation tests, low education was a statistically significant mediator of adolescent psychopathology's association with despair-related diseases, but the effect size was modest: after accounting for demographic factors, adolescent SES, and adolescent cognitive ability, education mediated 2.1% of the association (online Supplemental Table S7). Low education was not a statistically significant mediator of the association with cardiometabolic risk (online Supplemental Table S8).
In secondary tests, that were not preregistered, we investigated four additional potential mediators, assessed in early adulthood: substance use, physical inactivity, fast-food consumption, and healthcare management (fast-food consumption and healthcare management were added in response to peer review). After accounting for covariates, early-adult substance use was a statistically significant mediator of the association of adolescent psychopathology with midlife despair-related diseases, explaining 21.5% of the association (online Supplemental Table S7). Mediation remained evident after removing substance-related indicators from the despair outcome (online Supplemental Table S7). Early-adult substance use did not mediate the association with cardiometabolic risk (online Supplemental Table S8). Early-adult physical inactivity, fast-food consumption, and healthcare management did not mediate associations of adolescent psychopathology with either midlife despair-related diseases or cardiometabolic risk (online Supplemental Tables 7, 8).
Co-occurrence of midlife diseases of despair and cardiometabolic risk
Despair-related diseases and cardiometabolic problems co-occurred at midlife (Table 3). For every additional indicator of despair-related disease, individuals had, on average, 1.12 [1.08–1.16] times the number of indicators of cardiometabolic risk. Adolescent psychopathology accounted for 8.3% of the association of despair-related diseases with cardiometabolic risk (adjusted IRR = 1.11 [1.07–1.15]; Table 3). Together, adolescent psychopathology, adolescent SES, and adolescent cognitive ability accounted for 16.7% of the association between despair-related diseases and cardiometabolic risk, but the association remained significant even after accounting for these factors (IRR = 1.10 [1.06–1.13]; Table 3).
Table 3. Incidence rate ratios (and 95% confidence intervals) for associations of indicators of midlife despair-related diseases with indicators of midlife cardiometabolic risk
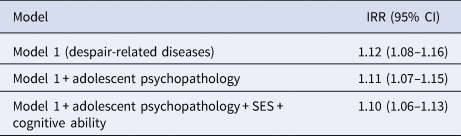
Note: All models were adjusted for age, sex, race, and ethnicity.
Discussion
In this longitudinal, nationally representative study of over 4500 participants, adolescents who experienced psychopathology went on to develop more diseases of despair and more indicators of cardiometabolic risk at midlife, even after accounting for demographic characteristics, adolescent SES, and adolescent cognitive ability. Adolescent psychopathology's association with midlife despair-related diseases was partly explained by early-adult substance use. In comparison, adolescents with physical-health problems went on to develop more midlife indicators of cardiometabolic risk, but not diseases of despair (in the Wave V biomarker sample). Diseases of despair and cardiometabolic risk also co-occurred; adolescent psychopathology accounted for a portion of this co-occurrence.
Associations of adolescent psychopathology with midlife diseases of despair and cardiometabolic risk were evident across both internalizing and externalizing conditions. Further, we observed dose–response associations, such that young people with more mental-health conditions went on to develop more indicators of despair-related diseases and cardiometabolic risk. Associations were robust to controls for adolescent SES and cognitive ability, suggesting that psychopathology in early life may be an independent contributor to multiple causes of morbidity in midlife. The current study extends prior work in a New Zealand cohort (Brennan et al., Reference Brennan, Moffitt, Ambler, Harrington, Hogan, Houts and Caspi2023) showing that adolescent psychopathology antedates midlife despair-related diseases. In addition to replicating the study's findings in a nationally representative United States sample, we show that adolescent psychopathology also antedates cardiometabolic risk. These findings join a growing body of literature indicating that early-life mental health forecasts not just later-life mental health, but also physical health (Bourassa et al., Reference Bourassa, Moffitt, Ambler, Hariri, Harrington, Houts and Caspi2022; Ploubidis et al., Reference Ploubidis, Batty, Patalay, Bann and Goodman2021; Richmond-Rakerd et al., Reference Richmond-Rakerd, Caspi, Ambler, d'Arbeloff, de Bruine, Elliott and Moffitt2021). If the associations identified here are causal, prevention and treatment of adolescent psychopathology could benefit population lifespan and healthspan.
Adolescents with physical-health conditions including obesity, diabetes, and asthma also tended to experience more indicators of midlife morbidity. As anticipated, the association of adolescent physical health with cardiometabolic risk was larger than that for diseases of despair. In addition, within the biomarker sample, the association with despair-related diseases was not statistically significant after controlling for adolescent SES and cognitive ability. This contrasts with adolescent psychopathology, for which both internalizing and externalizing conditions were associated with both midlife outcomes, even after accounting for potential confounders. This finding suggests that although adolescent physical health is an important contributor to midlife morbidity, interventions targeting adolescent psychopathology might confer broader effects. However, it should be noted that adolescent physical health's association with despair-related diseases was statistically significant in the full Wave V sample, with a comparable effect size to that observed in the biomarker sample. Thus, the lack of association in our analytic sample may in part reflect reduced statistical power.
It remains unclear exactly how adolescent psychopathology may confer risk for despair-related diseases and cardiometabolic risk. Only 2.1% of adolescent psychopathology's association with diseases of despair was explained by low education, and low education did not explain the association with cardiometabolic risk. In comparison, early-adult substance use explained 21.5% of the adolescent psychopathology's association with diseases of despair but did not mediate its association with cardiometabolic risk. Other health behaviors including early-adult physical inactivity, fast-food consumption, and healthcare management did not help to explain associations. Prior research has found that deaths of despair and cardiovascular mortality are elevated among individuals with low education (Case & Deaton, Reference Case and Deaton2015; Montano, Reference Montano2022), but our findings suggest that adolescent psychopathology does little to account for this observation. Instead, adolescent psychopathology may shape midlife morbidity through alternative mechanisms, such as substance use and other health behaviors (Ames, Leadbeater, & MacDonald, Reference Ames, Leadbeater and MacDonald2018; Hoare et al., Reference Hoare, Werneck, Stubbs, Firth, Collins, Corder and Van Sluijs2020). Although the health behaviors we considered did not significantly mediate associations, our measures were not comprehensive, limiting our ability to draw strong conclusions. In addition, midlife morbidity was assessed at ages 33–43, and the consequences of poor health behaviors may take more time to accumulate (Lachman, Teshale, & Agrigoroaei, Reference Lachman, Teshale and Agrigoroaei2015). Adolescent psychopathology may also shape midlife health via other mechanisms, such as limiting adolescents' acquisition of physical, cognitive, social, and economic resources, which are important for determining health trajectories (Patton et al., Reference Patton, Sawyer, Santelli, Ross, Afifi, Allen and Viner2016). To further investigate how adolescent psychopathology may confer risk for diseases of despair and cardiometabolic risk, future research should (1) incorporate more comprehensive assessments of health behaviors, (2) extend the follow-up period beyond early midlife, and (3) consider additional mediators including cognitive, social, and economic resources.
In middle adulthood, individuals with more diseases of despair also tended to experience more indicators of cardiometabolic risk. However, despite the associations of adolescent psychopathology with each outcome individually, adolescent psychopathology explained a somewhat modest degree (approximately eight percent) of their co-occurrence. As such, many adolescents with mental-health problems tended to develop either more indicators of despair-related diseases or cardiometabolic risk, but not both. Thus, in addition to some overlapping risk mechanisms, there may also be heterogeneity in the trajectories of midlife morbidity that follow from adolescent psychopathology (Hoare et al., Reference Hoare, Werneck, Stubbs, Firth, Collins, Corder and Van Sluijs2020). For instance, psychopathology may lead to more sedentary behavior for some adolescents, resulting in greater cardiometabolic risk (Raudsepp, Reference Raudsepp2016). Other young people may cope with mental-health problems by using substances (Copeland, Wolke, Shanahan, & Costello, Reference Copeland, Wolke, Shanahan and Costello2015), leading to more diseases of despair (Storr, Pacek, & Martins, Reference Storr, Pacek and Martins2012). Though adolescent psychopathology tends to increase the risk for midlife diseases of despair or cardiometabolic risk, once these problems develop, they may confer additional risk for each other. As such, treatment of adolescent psychopathology may still ultimately reduce the co-occurrence of these outcomes.
This study has additional clinical and theoretical implications. First, the co-occurrence we observed between diseases of despair and cardiometabolic risk has implications for clinical care in midlife. Our results suggest a need for greater integration of medical and mental-health treatment. For instance, providers treating patients for cardiometabolic problems should also consider screening for suicidality, substance misuse, sleep problems, and pain, which may exacerbate cardiometabolic conditions (Abdul-Rahman et al., Reference Abdul-Rahman, Card, Grainge and Fleming2018; Beccuti & Pannain, Reference Beccuti and Pannain2011; Deste & Lombardi, Reference Deste and Lombardi2023; Fayaz et al., Reference Fayaz, Ayis, Panesar, Langford and Donaldson2016; Gan et al., Reference Gan, Buxton, Scheuermeyer, Palis, Zhao, Desai and Slaunwhite2021; Ge et al., Reference Ge, Guyatt, Tian, Pan, Chang, Chen and Yang2019; Michal & Beutel, Reference Michal and Beutel2021; Vgontzas et al., Reference Vgontzas, Bixler, Tan, Kantner, Martin and Kales1998). Similarly, providers treating individuals for problems related to suicidal behavior, substance misuse, sleep problems, or pain should monitor patients' cardiometabolic health, providing psychoeducation and referring them to specialists when warranted. Second, our findings support the hypothesis that adolescent psychopathology is a causal contributor to midlife despair-related and cardiometabolic diseases. However, additional research is required to confirm this hypothesis. This includes clinical studies demonstrating that interventions targeting adolescent psychopathology reduce midlife despair-related and cardiometabolic morbidity, as well as epidemiologic evidence that individuals experiencing greater midlife morbidity also experienced more psychopathology as adolescents. To date, most research analyzing trends in the prevalence of mental-health conditions has focused on recent trends, which do not capture the adolescent period for those currently experiencing high midlife morbidity and mortality (Moreno-Agostino et al., Reference Moreno-Agostino, Wu, Daskalopoulou, Hasan, Huisman and Prina2021).
Our results raise the question of how adolescent psychopathology may fit into the deaths-of-despair framework. This framework argues that elevated mortality from overdose, suicide, and alcohol among individuals with less education is driven by an economy that fails to support the working middle class (Case & Deaton, Reference Case and Deaton2022). It is proposed that, as a result, individuals without a bachelor's degree have lost ‘job(s), status, and dignity,’ which leads to despair, increases in suicidality, and self-medication with substances (Case & Deaton, Reference Case and Deaton2022). Our findings suggest that adolescent psychopathology may have both direct and indirect effects on midlife despair. For some individuals, adolescent psychopathology may directly predispose them to midlife despair-related diseases, regardless of the economic advantages or disadvantages they receive. For others, adolescent psychopathology may increase their vulnerability to the social and psychological impacts of economic disadvantage, and their subsequent effects on midlife morbidity.
We acknowledge limitations. First, prospective assessments of psychopathology were not available for all mental-health conditions. Retrospective reports are subject to recall bias and underestimate prevalence relative to prospective reports (Moffitt et al., Reference Moffitt, Caspi, Taylor, Kokaua, Milne, Polanczyk and Poulton2010). In supplemental analyses, effect sizes were attenuated when only prospective psychopathology reports were used. However, this may reflect reduced statistical power rather than an impact of retrospective-reporting bias, as only two conditions (depression and conduct disorder) were assessed prospectively. Second, mental-health diagnoses were based on symptom scales and self-reported diagnoses rather than diagnostic interviews. Third, for retrospective reports, we used age-at-diagnosis to determine whether mental-health conditions occurred during adolescence. Mental-health conditions often onset before they are diagnosed; our ascertainment strategy did not capture adolescents with conditions that went undiagnosed or were not diagnosed until later in life. Despite these limitations, our prevalence estimate for adolescent psychopathology was within the range of those from other epidemiologic studies, including studies utilizing prospective mental-health assessments and diagnostic interviews (Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel and Moffitt2014; Jaffee, Harrington, Cohen, & Moffitt, Reference Jaffee, Harrington, Cohen and Moffitt2005; Merikangas et al., Reference Merikangas, He, Burstein, Swanson, Avenevoli, Cui and Swendsen2010). In addition, misclassifying some adolescents as undiagnosed means that our estimates of associations with adolescent psychopathology are likely conservative. Fourth, our measure of cognitive ability was limited to receptive vocabulary, which is not a comprehensive assessment of cognitive ability. However, verbal ability is typically found to contribute most strongly to the g-factor of general intelligence (Moore & Conway, Reference Moore and Conway2023; Wallbrown, Blaha, Wallbrown, & Engin, Reference Wallbrown, Blaha, Wallbrown and Engin1975). Fifth, our assessment of despair-related diseases was limited to the available data. Notably, pain was only assessed via pain-medication use; subjective measures were not available. Sixth, we assessed more adolescent mental-health than physical-health conditions, making it difficult to directly compare their associations with midlife outcomes. Seventh, there may be some temporal overlap in the assessment periods for adolescent psychopathology and low education, leaving open the potential for reverse-causation. Lastly, we assessed indicators of midlife morbidity, not mortality. Although research has linked diseases of despair and cardiometabolic risk to premature death (Di Angelantonio et al., Reference Di Angelantonio, Kaptoge, Wormser, Willeit, Butterworth, Bansal and Danesh2015; Glei & Preston, Reference Glei and Preston2020; Huyett, Siegel, & Bhattacharyya, Reference Huyett, Siegel and Bhattacharyya2021; Inoue, Ritz, & Arah, Reference Inoue, Ritz and Arah2022; Prabhakar et al., Reference Prabhakar, Peterson, Hu, Chawa, Rossom, Lynch and Ahmedani2021), we cannot confirm that our findings extend to deaths of despair and mortality from cardiometabolic diseases.
Conclusions
Psychopathology in adolescence antedates both diseases of despair and cardiometabolic risk in middle adulthood. Our results suggest that prevention and treatment of adolescent psychopathology might reduce multiple contributors to midlife morbidity, and extend population lifespan. The current findings also highlight several avenues for future research. First, clinical and epidemiologic studies are needed to provide evidence of adolescent psychopathology as a causal contributor to midlife morbidity. Second, research should explore the mechanisms by which adolescent psychopathology may lead to poor midlife health; areas of focus may include health behaviors and access to cognitive, social, and economic resources. Third, future work should investigate the co-occurrence and antecedents of despair-related diseases and cardiometabolic risk across the lifespan, into older adulthood.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724000916
Funding statement
This research uses data from Add Health, funded by grant P01 HD31921 (Harris) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Add Health is currently directed by Robert A. Hummer and funded by the National Institute on Aging (NIA) cooperative agreements U01 AG071448 (Hummer) and U01AG071450 (Aiello and Hummer) at the University of North Carolina at Chapel Hill. Add Health was designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill. Additional support was provided from the American Foundation for Suicide Prevention (LSR-R, PRG-1-153-20), the NIA (KRD, T32AG027708, PIs: Kobayashi and Park), and the Duke Aging Center Postdoctoral Research Training Grant (GMB, T32AG000029). This work's content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Competing interests
The authors declare no conflicts of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.








