COVID-19 vaccination has emerged as a key strategy to combat the global pandemic and vaccine acceptance is integral in this process (Laine, Cotton, & Moyer, Reference Laine, Cotton and Moyer2020). It is thus important to study the different factors influencing health behaviors and attitudes, to combat vaccine hesitancy effectively. In a study published in Psychological Medicine, Freeman et al. (Reference Freeman, Loe, Chadwick, Vaccari, Waite, Rosebrock and Lambe2020) showed that vaccine acceptance was related to the ‘recognition of collective importance’. Cultural tightness is an important factor that influences human behavior and the way different societies cope with collective threats (Gelfand et al., Reference Gelfand, Jackson, Pan, Nau, Pieper, Denison and Wang2021). At present, it is unclear if cultural tightness influenced COVID-19 vaccine acceptance. To address this gap in knowledge, we examined publicly available data on the global attitude toward COVID-19 vaccination, from Imperial College London YouGov COVID-19 Behavior Tracker Data Hub (Jones, Reference Jones2021). Respondents from 15 countries were surveyed between 30 December 2020 and 11 January 2021 on their willingness to receive the COVID-19 vaccine (Jones, Reference Jones2021). We then analyzed each country's vaccination willingness with their corresponding level of cultural tightness as defined by Gelfand et al. (Reference Gelfand, Jackson, Pan, Nau, Pieper, Denison and Wang2021) (12 out of 15 of the surveyed countries had a cultural tightness score).
Interestingly, we found that cultural tightness was negatively related to the willingness to receive the COVID-19 vaccine (r = −0.65, p = 0.02) (see Fig. 1). This finding seemed counterintuitive as the theory of cultural tightness and looseness suggested that societies with tighter cultures had greater self-regulation, which compelled individuals to be more cooperative in the face of crisis situations such as natural disasters and epidemics (Gelfand et al., Reference Gelfand, Jackson, Pan, Nau, Pieper, Denison and Wang2021). To understand our finding better, we further mined and analyzed data (Roser, Ritchie, Ortiz-Ospina, & Hasell, Reference Roser, Ritchie, Ortiz-Ospina and Hasell2020) of the average number of COVID-19 cases per million people per day in the 12 countries included in the Imperial College London YouGov survey (during the period of survey). Our analysis showed that the willingness to receive the COVID-19 vaccine was positively related to the prevailing degree of community transmission (r = 0.61, p = 0.015). With common concerns for the potential side effects and safety profile of a novel vaccine (Dodd et al., Reference Dodd, Pickles, Nickel, Cvejic, Ayre, Batcup and McCaffery2021), a low risk for contracting COVID-19 as perceived by people in countries where COVID-19 is well-controlled may have prompted them to decline and delay vaccination. It seemed possible that the success of cultural tightness in controlling COVID-19 cases and fatalities may be a confounding factor in COVID-19 vaccination willingness and acceptance.
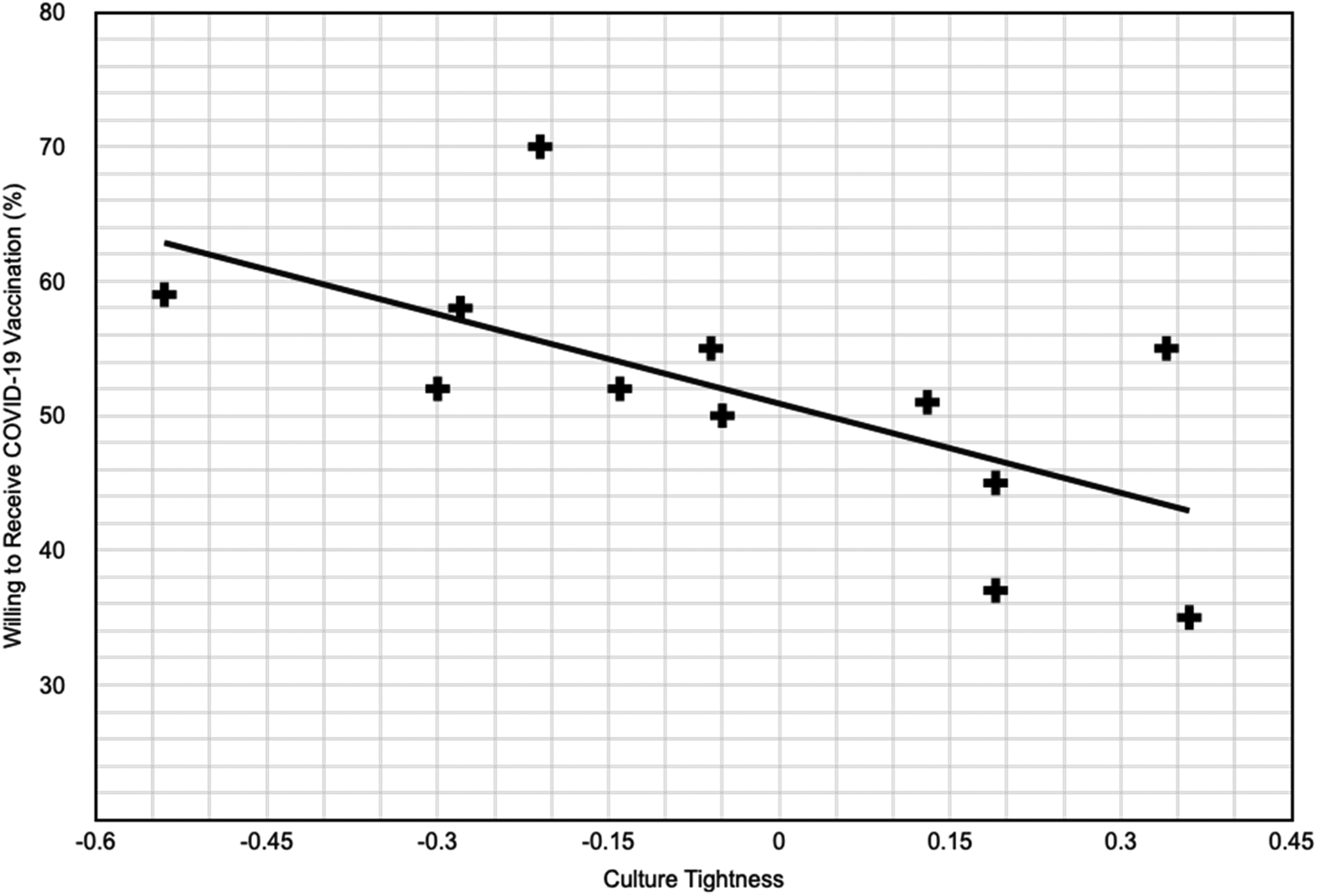
Fig. 1. Association of cultural tightness and willingness to receive vaccination.
Cultural tightness has been advantageous in helping communities overcome collective threats (Gelfand et al., Reference Gelfand, Jackson, Pan, Nau, Pieper, Denison and Wang2021). It is crucial for culturally-tight countries who have done well in the COVID-19 pandemic to avoid complacency and remain vigilant as this collective threat still exists. Public administrators and healthcare professionals in culturally-tight countries should tap on their intrinsic strengths of societal cooperation and coordination to portray COVID-19 vaccination as an important part of civic duty to improve vaccination willingness and acceptance. As societal cultures are multidimensional and increasingly dynamic and fluid (Kashima, Reference Kashima2014), it will be prudent to conduct further studies on the ways cultural tightness affects individual vaccine decisions and how cultural dynamics may be modified to allow societies and countries to better cope with the global pandemic.
Acknowledgements
We like to thank the National Medical Research Council, Singapore, for their support.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of interest
None.




