Introduction
Studies in Western Europe have found an increased incidence of psychotic disorders among various migrant and minority ethnic groups in Western Europe (e.g. Selten, van der Ven, & Termorshuizen, Reference Selten, van der Ven and Termorshuizen2020). The European Network of National Schizophrenia Networks Studying Gene-Environment Interaction (EU-GEI) study confirmed and extended this finding. During the period from 2010 to 2015, it compared the incidence of psychotic disorder between ethnic minorities and the reference population at sites in Spain, Italy, France, the UK, and the Netherlands. When the researchers categorized the participants according to their country of birth and the country of birth of their parents, the results showed higher incidence rate ratios (IRRs) for individuals with a Non-Western background (pooled, adjusted IRR = 2.12; 95% CI 1.88–2.40) than for those with a Western background (pooled, adjusted IRR = 1.09; 95% CI 0.91–1.32) (Termorshuizen et al., Reference Termorshuizen, van der Ven, Tarricone, Jongsma, Gayer-Anderson, Lasalvia and Selten2022). (For the definition of ‘Western’ and ‘Non-Western’ used in the study, see Methods below.) It is worthwhile to note that many, but not all members of minority ethnic groups are first- and second-generation migrants.
Most researchers assume an important role in social stressors (e.g. Dykxhoorn and Kirkbride, Reference Dykxhoorn and Kirkbride2019; Morgan, Knowles, and Hutchinson, Reference Morgan, Knowles and Hutchinson2019; Selten and Cantor-Graae, Reference Selten and Cantor-Graae2005; Selten and Ormel, Reference Selten and Ormel2023), but no study has examined whether the variation in psychosis risk might be explained by cannabis use, another important environmental risk factor for psychosis (e.g. Gage, Hickman, and Zammit, Reference Gage, Hickman and Zammit2016). To the best of our knowledge, five studies have compared the frequency of cannabis use among migrants to that for the reference population (Kortas et al., Reference Kortas, Abrahão, Malbergier, Fidalgo, Moura, de Andrade and Castaldelli-Maia2022), Two studies from Spain (Marsiglia, Kulis, Luengo, Nieri, & Villar, Reference Marsiglia, Kulis, Luengo, Nieri and Villar2008; Sarasa-Renedo et al., Reference Sarasa-Renedo, Sordo, Pulido, Guitart, González-González, Hoyos and Barrio2015) and one from Norway (Abebe, Hafstad, Brunborg, Kumar, & Lien, Reference Abebe, Hafstad, Brunborg, Kumar and Lien2015) reported lower cannabis use in migrants. A third study from Spain reported a relationship with length of stay: lower levels of cannabis use for migrants who had stayed for less than 10 years and increased rates for subjects from some regions (South-American Cone and Western-Europe) who had stayed for a longer period of time (Sordo et al., Reference Sordo, Indave, Vallejo, Belza, Sanz-Barbero, Rosales-Statkus and Barrio2015). A study from France reported increased rates of cannabis use for non-European migrants aged 11 to 14 years and a younger age at first use (Chau, Baumann, Kabuth, & Chau, Reference Chau, Baumann, Kabuth and Chau2012).
Two psychosis incidence studies examined the frequency of cannabis use during the year before first contact with a helping agency and found no strong differences between migrants and the reference population (Cantwell et al., Reference Cantwell, Brewin, Glazebrook, Dalkin, Fox, Medley and Harrison1999; Veen et al., Reference Veen, Selten, Hoek, Feller, van der Graaf and Kahn2002). However, these studies did not include control groups from the general population. In sum, there is sufficient reason to examine if, and to what extent the association between ethnic minority status and risk of psychotic disorder is explained by the use of cannabis.
The case-control part of the EU-GEI-study collected information on drug use from incident cases and controls, and reported increased odds ratios (ORs) of psychotic disorder, compared with never users, for daily cannabis users (adjusted OR = 3.2; 95% CI 2.2–4.1) and for daily users of high-potency cannabis (adjusted OR = 4.8; 2.5–6.3) (Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson and Quigley2019). The study has also found strong differences in the risk of psychosis by migrant status and ethnicity (Jongsma et al., Reference Jongsma, Gayer-Anderson, Tarricone, Velthorst, van der Ven, Quattrone and Kirkbride2021). Here we examined (i) whether controls who belong to a Western or Non-Western minority reported a greater frequency of cannabis use than controls from the reference population; (ii) the extent to which ORs of psychotic disorder for Non-Western minorities (versus the reference population) changed after adjustment for variables reflecting cannabis use.
Methods
Participants
Between May 1, 2010 and April 1, 2015, researchers at 17 sites in Italy, Spain, France, Brazil, the UK, and the Netherlands approached patients and controls for participation in the EU-GEI study. They asked for informed consent from all patients aged 18–64 years who presented with a first-episode of psychosis (ICD-10 criteria: F20-F33) to local psychiatric services. Patients were excluded if they met criteria for organic psychosis or for psychotic symptoms resulting from an acute intoxication. Patients who refused participation were counted as cases in the incidence study but did not participate in the present case-control study. Using the Operational Criteria Checklist algorithm (McGuffin, Farmer, & Harvey, Reference McGuffin, Farmer and Harvey1991) all patients interviewed received a research-based diagnosis.
To select a sample of controls broadly representative of local populations in relation to age, sex, and ethnicity, a mixture of random and quota sampling was used. Local demographic data were used to set quotas for controls. Quotas were then filled using a variety of recruitment methods, including random sampling, stratified random sampling, and ad hoc approaches. Controls were not matched to cases (for more details, see Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020). In London, individuals of Black African and Black-Caribbean ethnicity were over-sampled to enable subsequent sub-group analyses. Sampling weights were created to account for this in the analysis (see below). Controls were excluded if they had received a diagnosis of or treatment for psychotic disorder. Details have been provided in previous publications (Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020; Jongsma et al., Reference Jongsma, Gayer-Anderson, Lasalvia, Quattrone, Mulè and Szöke2018).
All participants provided informed, written consent. Ethical approval was provided by research ethics committees at each site.
Measures of cannabis use
The cases and controls who consented to participate were interviewed using an updated version of the modified Cannabis Experience Questionnaire (CEQEU−GEI), which gathers a detailed history of the use of cannabis and other drugs (Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson and Quigley2019). Participants were asked whether they had ever used cannabis in their lifetime and whether they used cannabis now. If the answer to the first question was yes, four more questions were asked to ascertain the pattern of use that described the ‘most’ how each participant used over the period of use: (1) age at first use, (2) frequency of use, (3) money spent weekly, and (4) type of cannabis used. In answer to the latter question, participants reported the name of the type used in their native language. Later work categorized the type of cannabis used into low potency (Δ9-tetrahydrocannabinol (THC) <10%) or high potency (⩾10%). These two categories were derived using official data available from each of the study countries (for references: see online Supplementary Material) and from the EMCDDA 2016 (European Monitoring Centre for Drugs & Drug Addiction, 2016). For more details, see Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson and Quigley2019.
In the earlier EU-GEI analysis, the frequency of use and the potency of cannabis used were combined into a seventh variable because these two variables showed the highest ORs of psychosis and their combination showed a dose-response relationship (Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson and Quigley2019).
Region of origin/ethnicity
The Medical Research Council Socio-Demographic Schedule was used to collect information on the birth place of each individual and their parents and on the individual's self-reported ethnicity (Mallett, Leff, Bhugra, Pang, & Zhao, Reference Mallett, Leff, Bhugra, Pang and Zhao2002). Subjects with one or two foreign-born parents were considered subjects with an ethnic minority status. On the basis of the country of origin we distinguished between subjects with a Western background (‘Western’ embraces Europe, the USA, Canada, Australia, New Zealand, and countries of the former Soviet Union with a predominantly Christian religion) and those with a “Non-Western” background (all other countries). The concepts of Western and non-Western, developed by Statistics Netherlands, are primarily intended to reflect cultural properties, but they overlap with concepts like race, ethnicity, religion, and levels of economic and industrial development. Within the group of subjects from Non-Western countries we distinguished between minorities from (i) the Middle-East (includes also Turkey, Israel, Egypt), (ii) the Maghreb, (iii) sub-Saharan Africa, (iv) Asia (including states of former Soviet Union with a predominant Islamic population), (v) Latin-America, and (vi) Caribbean islands, Surinam, Guyana, and French Guyana. Thus, most non-Western individuals were born in developing countries or were raised by parents born in such countries. Native-born participants, the parents of whom were also without a migration history, were placed in the reference category. The seven minority groups and the reference population add up to eight groups in the present study.
Statistical analysis
The site of Maison-Blanche, Paris, had to be excluded from the analysis because it did not recruit controls. The site in Brazil (Ribeirão Preto) was excluded given its very different context with regard to migration and ethnicity. Puy-de-Dôme had to be excluded owing to missing data on ethnicity, Verona due to some quality issues with regard to cannabis data. This resulted in an analysis based on information from 13 sites. Due to the relatively small numbers of cases and controls at each site in Spain (Madrid, Barcelona, Valencia, Santiago, Oviedo, and Cuenca) and Italy (Bologna, Palermo), we collapsed them into two recruitment areas: Spain and Italy. Thus, we report on results obtained at 13 sites and distinguished in our analyses seven recruitment areas: Spain, Italy, Créteil, Southeast London, Cambridgeshire, Amsterdam, Gouda, and Voorhout.
Since the sites of Santiago, Oviedo, Valencia, and Cuenca had at least 10% of data missing on the measures of cannabis use or on one or more of the confounding variables, we also conducted analyses based on information obtained from 9 sites (13 minus 4).
Use of cannabis by ethnic background among controls
To examine whether controls who belong to a western or non-western minority use more cannabis than controls from the reference population do, we conducted 13 logistic regression analyses. The outcome variables of the first seven analyses were lifetime use, current use, first use before age 15, daily use, amount of money spent weekly of more than 20 Euros, use of high-potency cannabis and daily use of high-potency cannabis, all dichotomized in yes v. no. As for individuals with a lifetime history of use, it is conceivable that the pattern of use differs between members of Western or Non-Western minorities and those of the reference population. Consequently, we conducted six additional analyses, restricted to individuals who had ever used cannabis in their lifetime. The outcome variables of these analyses were current use, first use before age 15, daily use, amount of money spent weekly of more than 20 Euros, use of high-potency cannabis and daily use of high-potency cannabis.
Odds ratio of psychotic disorder for ethnic minorities compared with reference population, cases v. controls
To examine whether the ORs of psychotic disorder for Non-Western minorities, compared to the reference population, change after adjustment for variables reflecting cannabis use, we conducted multivariable logistic regression analyses, with and without adjustment for each of the seven measures of cannabis use. The participant's status as case or control was the outcome variable in this analysis. Cases were compared to controls with respect to two important variables: ethnic minority status and cannabis use.
Ideally, the group of controls is representative in terms of age, sex, and region of origin of the source population from which the cases originate. However, migrants from Africa and the Caribbean were intentionally over-sampled in London to facilitate sub-group comparisons. Since the distribution of the aforementioned characteristics deviated also at some other sites, we calculated weighting factors to adjust for these deviations (see e-Methods in online Supplement). In all logistic regression analyses, a statement for inclusion of these weighting factors was included (‘weights = weightfactor’).
In the first analysis, the logistic model included ethnic minority status (categorized into reference population, Western and Non-Western minority), age, sex, and the seven areas of recruitment. The next part of this analysis consisted of seven separate models; each one of them included the abovementioned variables and one of the seven indicators of cannabis use.
In the second analysis, we repeated these analyses (that is, without and with adjustment for a cannabis measure), with ethnic minority status categorized into eight groups (see above).
In the third analysis, the ORs for minorities (Western and Non-Western v. reference population) were estimated for each of the five recruitment countries (Spain, Italy, France, United Kingdom, and the Netherlands) separately, without and with adjustment for a cannabis measure. This was done in a model with age, sex, minority ethnic group, recruitment area, and with terms for the interaction between minority status and recruitment area.
If there was information on cannabis use for at least 10 cases and at least 10 controls from a minority group at a given site, we conducted both parts of the analysis (without and with adjustment for cannabis use) for this particular group (fourth analysis). The results were analyzed in separate models for each group at a given recruitment site; all models included the pertinent minority versus the local reference population, age, and sex.
Since it is conceivable that the results are influenced by the use of other substances that can cause psychotic disorder, in particular stimulants and cocaine (Chen et al., Reference Chen, Lin, Sham, Ball, Loh, Hsiao and Murray2003; Roncero et al., Reference Roncero, Daigre, Grau-López, Barral, Pérez-Pazos, Martínez-Luna and Casas2014), we repeated the second, third, and fourth analysis in the following way. First, we adjusted the ORs of psychotic disorder for the lifetime use of stimulants or cocaine using a model that also included age, sex, and site. Second, we examined whether an additional adjustment for lifetime use of cannabis, daily use of cannabis, or daily use of high-potency THC during the period of use, influenced the results.
Finally, we repeated the first, second, and third analyses for the nine sites with <10% of missing data on cannabis variables. Data preparation, record linkage, and estimation of the weighting factors were performed using SPSS version 22.0. The logistic regression analyses were performed in R, version 4.2.1.
Results
As for all the 17 sites that participated in the EU-GEI study 1519 cases were approached for participation and 1130 were recruited (Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020). The number of cases who refused to participate was 356 (23.4%). An additional 33 cases had to be excluded due to language barriers or because they did not meet the age criteria (Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson and Quigley2019; online Supplement). After exclusion of cases from Maison-Blanche, Brazil, Verona, Puy-de-Dôme, and cases with insufficient information on country of birth, the final sample for our study included 825 cases and 1026 controls.
Table 1 provides information on cases and controls with regard to demographics, levels of education, and types of employment. Online Supplementary Table 1 provides additional information on race/ethnicity by recruitment area. Table 2 shows the figures for reported substance use; cases and controls were further divided into individuals from the reference population and those from western or non-western countries. The results show that cases are younger than controls, are more often men, and more often use cannabis.
Table 1. Socio-demographic characteristics by case-control status
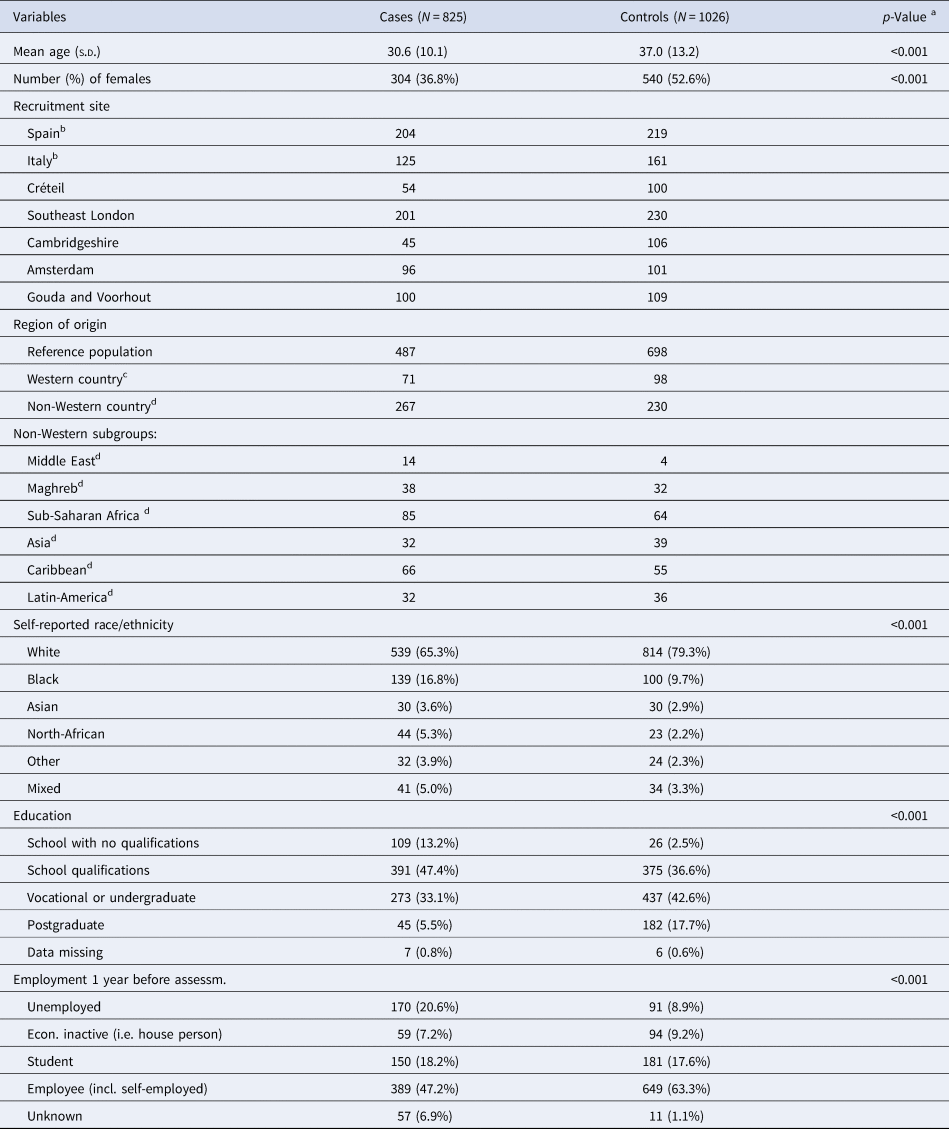
a P-values belonging to χ2-test (categorical variables) or Kruskal–Wallis test (continuous variables).
b Spain: Madrid, Barcelona, Valencia, Cuenca, Oviedo, Santiago. Italy: Bologna, and Palermo.
c Country of birth (or parental country of birth): Europe, USA, Canada, Australia, New Zealand, and countries of former Soviet Union with a predominantly Christian religion.
d Non-Western: all other countries. Middle East: includes also Egypt, Israel and Turkey. Maghreb: North-African countries except Egypt. Asia: including states of the former Soviet Union with a predominant Islamic religion; Caribbean includes the Caribbean islands, Surinam, Guyana, and French Guyana.
Table 2. Substance use reported by cases and controls, by country of birth or parental country of birth
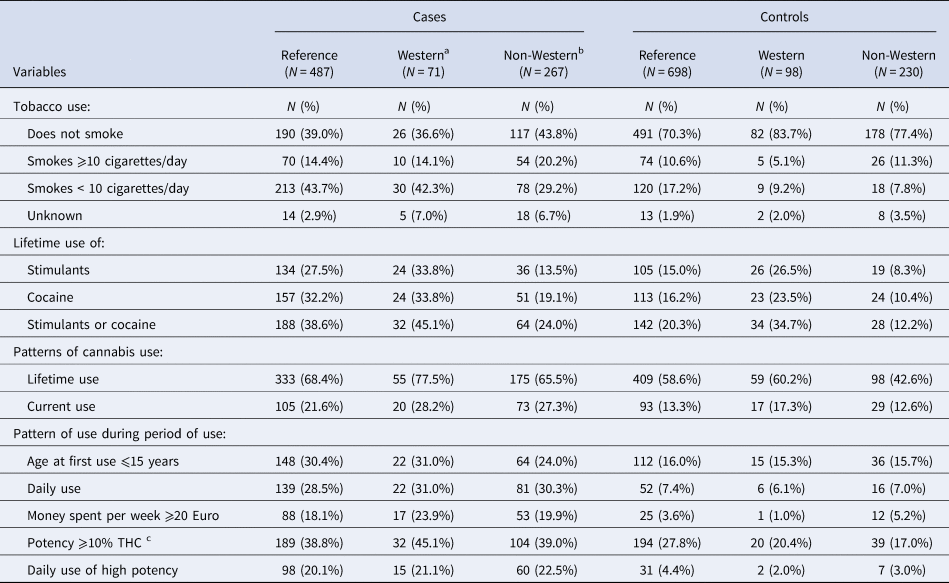
a Country of birth (or parental country of birth): Europe, USA, Canada, Australia, New Zealand, and countries of former Soviet Union with a predominantly Christian religion.
b Non-Western: all other countries.
c Δ9-tetrahydrocannabinol.
Use of cannabis by ethnic background among controls
Table 3 shows that the odds of lifetime use of cannabis were about 48% lower for controls with a Non-Western background compared with the reference population (OR, adjusted for age and sex = 0.52; 95% confidence interval [95% CI] = 0.38–0.73). On the other hand, among those who had ever used cannabis, the proportions of subjects who were current users, daily users, younger than 15 years at their first use, or who spent at least 20 Euros per week were somewhat higher within the group of Non-Western controls.
Table 3. Measures of cannabis use among controls, by region of origin; odds ratios of several aspects of cannabis use for western and non-western controls, versus controls from the reference population
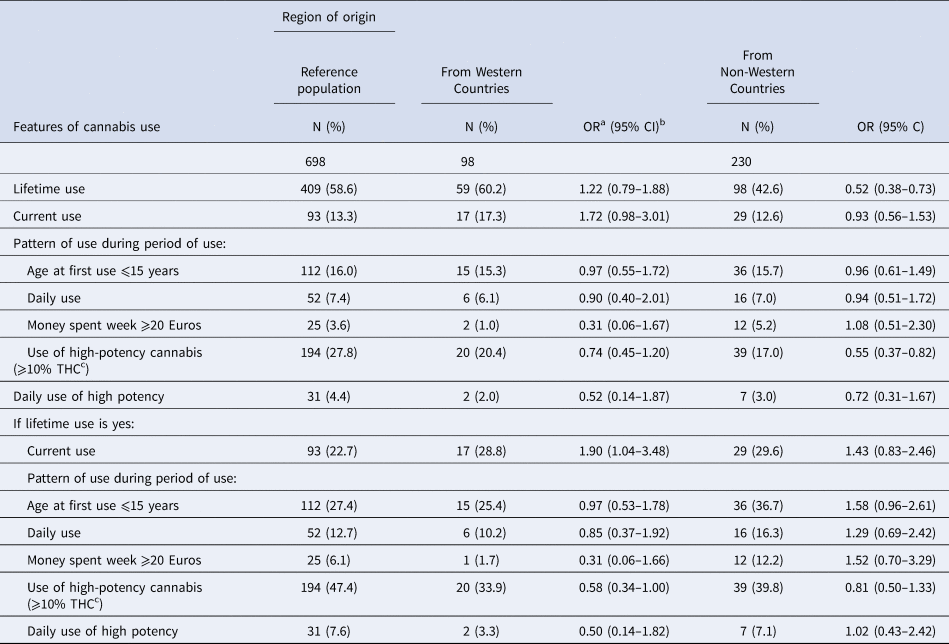
a Odds ratio adjusted for age and sex.
b 95% Confidence Interval.
c Δ9-tetrahydrocannabinol.
Odds ratios of psychotic disorder for ethnic minorities, cases v. controls
The OR of psychotic disorder for Non-Western minorities, adjusted for age, sex, and area of recruitment, was 1.80 (95% CI 1.39–2.33). Further adjustment for any of the seven cannabis use variables had a minimal effect on this OR, which remained significantly increased (Table 4).
Table 4. Odds ratios of psychotic disorder for subjects from all non-western countries and for subjects from sub-groups of non-western countries, before and after adjustment for several measures of cannabis use
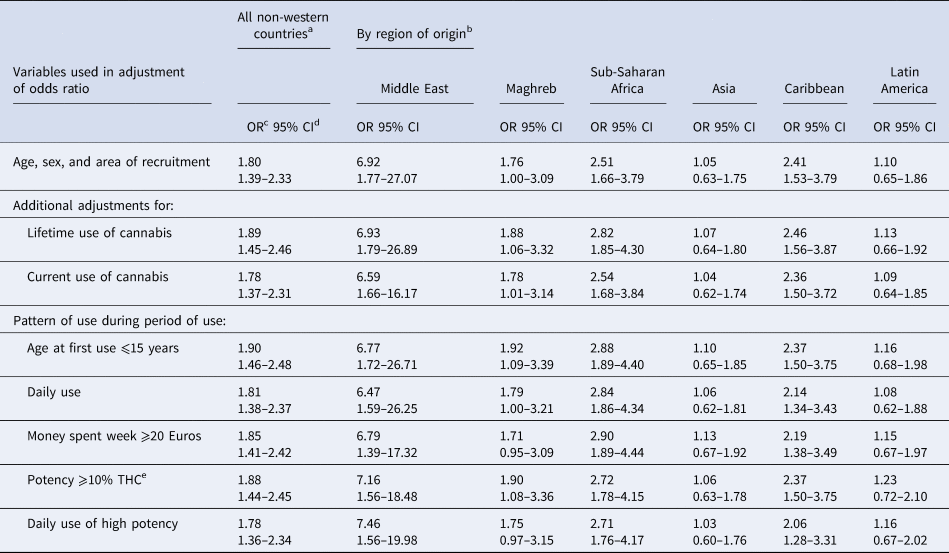
a The statistical model included region of origin (non-western, western, reference), recruitment area (seven areas), age, and sex.
b The statistical model included region of origin (six non-western regions, western, reference), recruitment area (seven areas), age, and sex.
c Odds ratio.
d 95% Confidence Interval.
e Δ9-tetrahydrocannabinol.
In an additional model with terms of interaction for {ethnic origin × cannabis use}, the effect of cannabis on the risk of psychotic disorder appeared to be stronger for individuals from non-Western countries than for the reference population. This was explored for cannabis measures 1 (lifetime use), 4 (daily use), and 7 (daily use of high-potency THC) Thus, the lack of effect of adjustment for cannabis use variables on the association between non-Western minority status and risk of psychotic disorder was not due to a lack of an association between cannabis use and this risk for non-Western minorities (data available on request).
We found negligible effects of cannabis use on the association between ethnic minority status and odds of psychosis in analyses using our more detailed region of origin variable (Middle East, the Maghreb, sub-Saharan Africa, Asia, the Caribbean, Latin America, and Western countries; see Table 4 and online Supplementary Table 2).
Odds ratios for Non-Western minorities by country and site of recruitment
The results showed that adjustments for measures of cannabis use had a minimal effect in each country (online Supplementary Table 3). An exception is the OR for subjects from non-western countries in the Netherlands, where adjustment for daily use during the period of use led to a decrease in the OR from 1.58 (95% CI 0.98–2.55) to 1.35 (95% CI 0.82–2.23) and to 1.36 (95% CI 0.82–2.26) after adjustment for daily use of high-potency cannabis, during the period of use.
In southeast London, there were at least 10 cases and at least 10 controls from Asia, sub-Saharan Africa, and the Caribbean. In Créteil and Amsterdam this applied to subjects from the Maghreb and from Surinam and the Netherlands Antilles, respectively (see online Supplementary Table 5 for numbers of cases and controls; information on their replies to questions on the use of cannabis is available upon request).
In London, there was little evidence that adjustment for any cannabis variable modified the OR of psychosis in participants of Asian or sub-Saharan African heritage. However, adjustment for daily use of high-potency cannabis (during the period of use) substantially decreased the OR for individuals of Caribbean origin (Table 5). In Amsterdam, adjustment for daily use of cannabis use (during the period of use) resulted also in a substantial decrease of the OR for those of origin from Surinam and the Netherlands Antilles (Table 5). For subjects from the Maghreb in Créteil, however, there was no evidence that adjustments for measures of cannabis had meaningful effects on the OR of psychosis.
Table 5. Odds ratios of psychotic disorder for certain minorities by recruitment area (versus local reference population), before, and after adjustment for measures of cannabis use
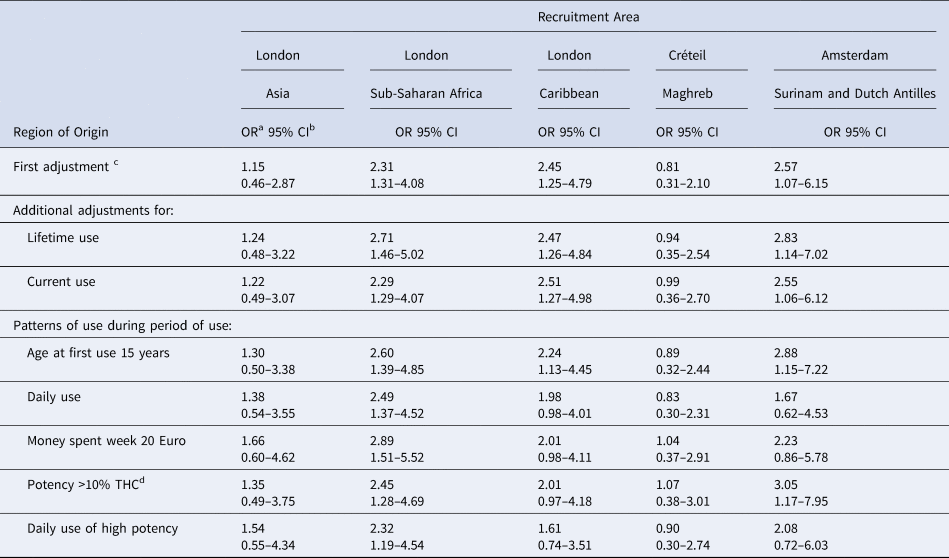
a Odds ratio.
b 95% Confidence interval.
c Separate logistic regression models for each minority at a given site. Each model included age and sex.
d Δ9-tetrahydrocannabinol.
Analyses without weighting factors yielded only minor differences. The age- and sex-adjusted OR of psychotic disorder for African-Caribbeans in London, computed without these factors, was 2.23 (95% CI 1.15–4.32). After adjustment for daily use of high-potency cannabis, this value decreased to 1.42 (95% CI 0.68–2.98). As for the Surinamese and Dutch Antilleans in Amsterdam, the age- and sex-adjusted OR computed without weighting factors was 2.89 (95% CI 1.23–6.76); after adjustment for frequency of use, the OR came to 1.84 (95% CI 0.69–4.89).
We repeated the analyses for Non-Western minorities at all sites combined and at each separate site without weighting factors and examined the impact of adjustment for frequency of use and for daily use of high-potency cannabis. The results were similar to those obtained with weighting factors (data available upon request).
The analyses that took into account the use of stimulants or cocaine yielded the following results. First, adjustment for the lifetime use of stimulants or cocaine almost always resulted in an increase of the OR of psychotic disorder, not a decrease. Second, an additional adjustment for each of the three selected variables reflecting cannabis use had, again, no major influence on the OR. The exceptions were, again, the substantial reductions in the OR of psychotic disorder for African-Caribbeans in London (after adjustment for daily use of high potency THC during the period of use) and for Suriname and Dutch Antilleans in Amsterdam (after adjustment for daily use during the period of use). See online Supplementary Tables 6, 7, and 8.
Finally, repeat of the first, second, and third analyses after the exclusion of four Spanish sites resulted in minimal differences with the previous analyses (online Supplementary Tables 9, 10, and 11). The exception was a change in the OR of psychotic disorder for subjects from non-western countries in Spain. The OR of 1.09 (95% CI 0.59–2.02), adjusted for age and sex but not for cannabis use, decreased to an OR of 0.57 (95% CI 0.22–1.45) after the exclusion of four Spanish sites. Again, the adjustments for variables related to cannabis use had a minimal effect.
Discussion
The main findings of this study are: (i) Non-Western controls as a whole do not report more use of cannabis than controls from the reference population; (ii) adjustments for measures of cannabis use have a very small effect on the ORs of psychotic disorder; and (iii) exceptions are Black Caribbeans in London and the Surinamese and Dutch Antilleans in Amsterdam; their ORs decreased by more than 20% and lost their statistical significance after adjustment for frequency of cannabis use (both groups) and for frequency of use of high-potency cannabis (Caribbeans in London); and (iv) adjustments for the lifetime use of stimulants or cocaine generally resulted in an increase of the ORs of psychotic disorder for non-western immigrants, not in a decrease.
Strength and limitations
This is the largest study of its kind. Cases and controls were thoroughly interviewed about their use of cannabis and other illicit substances, using a structured questionnaire. The diagnoses of a psychotic disorder were based on semi-structured diagnostic interviews, clinical, and collateral information. The analyses took into account a possible confounding effect of stimulants or cocaine. However, there were also some limitations. About one-quarter of the approached cases refused to be interviewed and the numbers of cases and controls of some groups by site and ethnic origin were very small. Further, data on cannabis use were not validated by biological measures. However, it is difficult to test for use over previous years by such means. One can use hair analysis for this purpose, but hair is not always long enough and some participants decline to yield hair (Selten et al., Reference Selten, Bosman, de Boer, Veen, van der Graaf, Maes and Kahn2002). Importantly, studies with laboratory data and self-reported information have shown that cannabis users reliably report the type of cannabis used (Freeman et al., Reference Freeman, Morgan, Hindocha, Schafer, Das and Curran2014; Meijer et al., Reference Meijer, Dekker, Koeter, Quee, van Beveren and Meijer2012). It is also important to note that we cannot exclude the possibility of differential reporting of cannabis use by ethnicity. Previous studies have found that some minority ethnic groups may be more likely to under-report substance use for several reasons, including concerns over privacy, discrimination, or potential prosecution (Johnson, Reference Johnson2014; Johnson & Bowman, Reference Johnson and Bowman2003).
We conducted a number of subgroup analyses (n = 35; Table 5) when controlling for seven different cannabis use variables in models stratified by site and ethnicity, where smaller sample sizes also increased uncertainty in the precision of our estimates. We cannot exclude the possibility that the two observed reductions in psychosis odds reported above were chance findings due to multiple testing. However, since our main conclusion is that there is no effect of adjustment for cannabis, adjustment for multiple testing would make this conclusion stronger, not weaker. We mentioned the two observed substantial reductions to allow for possible exceptions.
Finally, it is important to note that the data do not allow us to distinguish between the different mechanisms that can be responsible for an effect of cannabis.
Interpretation
The results of this study do not support the hypothesis that the use of cannabis (or stimulants or cocaine) explains a large part of the excess incidence of psychotic disorders among Non-Western minorities in Europe. An important alternative explanation is exposure to social stressors (Jongsma et al., Reference Jongsma, Gayer-Anderson, Tarricone, Velthorst, van der Ven, Quattrone and Kirkbride2021; Kirkbride et al., Reference Kirkbride, Anglin, Colman, Dykxhoorn, Jones, Patalay and Griffiths2024; Morgan et al., Reference Morgan, Knowles and Hutchinson2019; Selten & Ormel, Reference Selten and Ormel2023; Tarricone et al., Reference Tarricone, D'Andrea, Jongsma, Tosato, Gayer-Anderson, Stilo and Morgan2022).
The possible exceptions to this are those of Black Caribbean ethnicity in London and Amsterdam and the Surinamese in Amsterdam, but our results require independent replication in larger samples. The findings suggest that a non-negligible proportion of the excess risk of psychosis in these populations may be explained by daily use of high-potency cannabis. The use of cannabis may act as a confounder of the association between ethnic background and risk of psychosis, as a mediator in the causal pathway between ethnic background and psychosis, or as both.
Given the findings in Spain (Sordo et al., Reference Sordo, Indave, Vallejo, Belza, Sanz-Barbero, Rosales-Statkus and Barrio2015) it is worthwhile to note that the use of cannabis in some minority ethnic groups may increase with the length of their stay in Western Europe. On the other hand, the results of a recent study that examined the incidence of psychotic disorder and the possible link with cannabis use in Nigeria, India, and Trinidad suggested that a problematic use of cannabis among Caribbeans is not necessarily a consequence of migration. The results showed not only a higher incidence of psychotic disorder in Trinidad, but also a greater frequency of cannabis use than in the two other countries (Pow et al., Reference Pow, Donald, Di Forti, Roberts, Weiss, Ayinde and Hutchinson2023; see also Atkinson, Abel, & Whitehorne-Smith, Reference Atkinson, Abel and Whitehorne-Smith2015).
Conclusion
While the consumption of cannabis may contribute to the excess risk of psychotic disorder for some ethnic minorities in some specific settings, we have found no evidence that it contributes to the overall excess risk of psychoses in ethnic minorities
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724001004.
Funding statement
The EU-GEI Project is funded by the European Community's Seventh Framework Programme under grant agreement No. HEALTH-F2-2010-241909 (Project EU-GEI). The funder was not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript and decision to submit the manuscript for publication.
Dr Arango was supported by the Spanish Ministry of Science and Innovation, Instituto de Salud Carlos III (ISCIII), co-financed by the European Union, ERDF Funds from the European Commission, ‘A way of making Europe’, financed by the European Union - NextGenerationEU (PMP21/00051), PI19/01024. CIBERSAM, Madrid Regional Government (B2017/BMD-3740 AGES-CM-2), European Union Structural Funds, European Union Seventh Framework Program, European Union H2020 Program under the Innovative Medicines Initiative 2 Joint Undertaking: Project PRISM-2 (Grant agreement No.101034377), Project AIMS-2-TRIALS (Grant agreement No 777394), Horizon Europe, the National Institute of Mental Health of the National Institutes of Health under Award Number 1U01MH124639-01 (Project ProNET) and Award Number 5P50MH115846-03 (project FEP-CAUSAL), Fundación Familia Alonso, and Fundación Alicia Koplowitz.
Competing interests
Dr Arango has been a consultant to or has received honoraria or grants from Acadia, Angelini, Biogen, Boehringer, Gedeon Richter, Janssen Cilag, Lundbeck, Medscape, Menarini, Minerva, Otsuka, Pfizer, Roche, Sage, Servier, Shire, Schering Plough, Sumitomo Dainippon Pharma, Sunovion, and Takeda.








