Introduction
Background
Alexithymia, literally translated as ‘no words for emotions’, is a subclinical trait with an estimated prevalence of 10% in the general population (Berthoz & Wessa, Reference Berthoz, Pouga, Wessa, Decety and Cacioppo2011; Nemiah, Freyberger, & Sifneos, Reference Nemiah, Freyberger, Sifneos and Hill1976). The construct of alexithymia can be broken down into several facets, including: difficulties in identifying feelings (internally interpreting and differentiating emotions); difficulties in describing feelings (expressing emotions) and externally oriented thinking (focusing attention away from emotions; Bagby, Parker, and Taylor, Reference Bagby, Parker and Taylor1994).
Of note, individuals with high-alexithymic traits are reported to experience significantly more interpersonal difficulties and mental health problems than those with lower levels of alexithymia (Grabe, Spitzer, & Freyberger, Reference Grabe, Spitzer and Freyberger2004; Spitzer, Siebel-Jürges, Barnow, Grabe, & Freyberger, Reference Spitzer, Siebel-Jürges, Barnow, Grabe and Freyberger2005; Vanheule, Desmet, Meganck, & Bogaerts, Reference Vanheule, Desmet, Meganck and Bogaerts2007). Furthermore, alexithymia has been shown to be a significant barrier to intervention success across psychiatry and healthcare (Grabe et al., Reference Grabe, Frommer, Ankerhold, Ulrich, Groger, Franke and Spitzer2008; Ogrodniczuk, Piper, & Joyce, Reference Ogrodniczuk, Piper and Joyce2011). In light of these issues, poor self-knowledge of one's internal emotions (i.e. alexithymia) is now recognised as a transdiagnostic mechanism that modulates mental health outcomes in the general population (Fernandez, Jazaieri, & Gross, Reference Fernandez, Jazaieri and Gross2016; National Institute of Mental Health, 2019).
Alexithymia and social-communication difficulties in autism
Given its intrinsic role in social–emotional processing, it is unsurprising that elevated rates of alexithymia have been reported across a range of neurodevelopmental and neuropsychiatric conditions that affect social and/or emotion understanding (Berthoz, Pouga, & Wessa, Reference Berthoz, Pouga, Wessa, Decety and Cacioppo2011; Bird and Cook, Reference Bird and Cook2013). For example, current estimates suggest that at least 40–65% of autistic people experience severe alexithymia (Bird & Cook, Reference Bird and Cook2013; Hobson et al., Reference Hobson, Westwood, Conway, McEwen, Colvert, Catmur and Happé2020; Kinnaird, Stewart, & Tchanturia, Reference Kinnaird, Stewart and Tchanturia2019). Autism is one of the most common, lifelong neurodevelopmental conditions, with a prevalence of ~1.9% (Maenner et al., Reference Maenner, A, Baio, Washington, Patrick, DiRienzo and Dietz2020) – characterised by core traits of social-communication difficulties and restricted and repetitive behaviours (American Psychiatric Association, 2013). In addition, some autistic individuals experience difficulties with emotion awareness and processing. For instance, when recounting personal memories, individuals may tend to focus on objective events, rather than their feelings about those events (Hurlburt, Happé, & Frith, Reference Hurlburt, Happé and Frith1994). Similarly, when reflecting on internal emotions (e.g. when asked ‘how do you know when you are happy?’), some autistic individuals consider the observable features of emotions (‘because I am laughing’, ‘because it's my birthday’), over their subjective ‘feeling’ (Rieffe, Meerum Terwogt, & Kotronopoulou, Reference Rieffe, Meerum Terwogt and Kotronopoulou2007).
Since social-communication difficulties are a core feature of autism, most published studies have focused on associations between alexithymia and difficulties in perceiving and understanding the emotions of others. For example, autistic individuals with higher alexithymic traits experience more difficulties in recognising verbal and non-verbal emotional expressions, compared to those with lower levels of alexithymia (Cook, Brewer, Shah, & Bird, Reference Cook, Brewer, Shah and Bird2013; Heaton et al., Reference Heaton, Reichenbacher, Sauter, Allen, Scott and Hill2012; Oakley, Brewer, Bird, & Catmur, Reference Oakley, Brewer, Bird and Catmur2016) – and these difficulties are associated with everyday social functioning (Trevisan & Birmingham, Reference Trevisan and Birmingham2016).
Furthermore, alexithymia in autism has been shown to relate to reductions and/or differences in the production of emotion expressions (Trevisan, Bowering, & Birmingham, Reference Trevisan, Bowering and Birmingham2016; Wagner & Lee, Reference Wagner and Lee2008) and emotional empathy towards others (Bird et al., Reference Bird, Silani, Brindley, White, Frith and Singer2010). These skills are critical for accurately interpreting and appropriately responding to social cues and facilitating successful interpersonal relationships (Ekman, Reference Ekman, Dalgleish and Power1999) and may, therefore, contribute to increased difficulties in social interactions. Thus, findings to date imply that alexithymia may act as a modifier, exacerbating social-communication difficulties in autism (Mundy, Henderson, Inge, & Coman, Reference Mundy, Henderson, Inge and Coman2007).
Alexithymia and anxiety/depression symptoms in autism
However, far fewer studies have considered the role of alexithymia – particularly difficulties in perceiving one's own emotions – in explaining individual variability in anxiety and depression symptom severity in autism. This is despite evidence that difficulties with emotion awareness relate to mental health symptoms in the general population (Mattila et al., Reference Mattila, Kronholm, Jula, Salminen, Koivisto, Mielonen and Joukamaa2008), including young children (Rieffe, Oosterveld, Miers, Meerum Terwogt, & Ly, Reference Rieffe, Oosterveld, Miers, Meerum Terwogt and Ly2008). Moreover, at least 20–50% of autistic individuals experience co-occurring anxiety and/or depression – far higher rates than those observed in the general population (Hollocks, Lerh, Magiati, Meiser-Stedman, & Brugha, Reference Hollocks, Lerh, Magiati, Meiser-Stedman and Brugha2019; Simonoff et al., Reference Simonoff, Pickles, Charman, Chandler, Loucas and Baird2008). Hence, research on mechanisms associated with co-occurring anxiety and depression in autism has been declared a research priority (Autistica, 2017; Pellicano, Dinsmore, & Charman, Reference Pellicano, Dinsmore and Charman2014), for which alexithymia may provide a tractable treatment target.
Some recent studies indicate that there may be associations between alexithymia and anxiety/depression symptoms in autism. For instance, Milosavljevic et al. (Reference Milosavljevic, Carter Leno, Simonoff, Baird, Pickles, Jones and Happe2016) showed that adolescents with autism and elevated alexithymia self-reported significantly higher concurrent anxiety than those with autism only. Similarly, alexithymia has been found to partially mediate associations between core autism traits and anxiety and depression symptoms in autistic young adults (Maisel et al., Reference Maisel, Stephenson, South, Rodgers, Freeston and Gaigg2016; Morie, Jackson, Wei, Marc, & Dritschel, Reference Morie, Jackson, Wei, Marc and Dritschel2019). These findings imply that alexithymia may be a key contributing factor for mental health problems in autism, as in the general population.
Nevertheless, there is a considerable lack of longitudinal research examining the putative impact of alexithymia in autism (Kojima, Reference Kojima2012). Existing studies have been cross-sectional in nature and considered alexithymia as a unitary construct, when there may be subtle differences between its individual facets (e.g. difficulties in describing v. identifying emotions) and specific outcomes. As a result, the role of alexithymia (or its individual facets) in predicting the development of social-communication difficulties and/or mental health symptoms remains unclear.
For example, alexithymia may be a modifying factor that interacts with concurrent core autism traits and/or anxiety and depression symptoms, resulting in individual differences in outcome, or treatment response. Additionally, or alternatively, alexithymia may represent a precursor to later developing socio-emotional and mental health problems – potentially via difficulties with emotion perception/production (Brewer et al., Reference Brewer, Biotti, Catmur, Press, Happé, Cook and Bird2016a; Trevisan & Birmingham, Reference Trevisan and Birmingham2016), interoception (perception of internal bodily states; Garfinkel et al., Reference Garfinkel, Tiley, O'Keeffe, Harrison, Seth and Critchley2016) and/or emotion regulation (Maisel et al. Reference Maisel, Stephenson, South, Rodgers, Freeston and Gaigg2016; Morie et al. Reference Morie, Jackson, Wei, Marc and Dritschel2019). Finally, alexithymia may be a consequence of difficulties in understanding others' emotions (Carruthers, Reference Carruthers2009), or act as a compensatory buffer against aversive internalising problems (Kojima, Reference Kojima2012; Mor & Winquist, Reference Mor and Winquist2002). Overall, establishing longitudinal relationships between potential precursors (e.g. alexithymia) and outcomes over time (e.g. social functioning, anxiety and depression) is essential for informing early and effective interventions and support in autism.
The current study
Thus, our study first aimed to assess cross-sectional associations between alexithymia (including its individual facets), social-communication difficulties, anxiety and depression symptoms in a large, well-characterised cohort of autistic and non-autistic males and females, aged 12–30 years. Furthermore, we modelled longitudinal associations between earlier alexithymia and subsequent social-communication difficulties, anxiety and depression symptoms approximately 12–24 months later. Based on previous literature, we predicted that increasing alexithymia would be associated with elevated social-communication difficulties, anxiety and depression symptoms in the autism group, at a single timepoint and longitudinally.
Methods
Participants
The current study is based on data from the EU-AIMS Longitudinal European Autism Project (LEAP). A detailed description of the design and methodologies of LEAP are reported elsewhere (Loth et al., Reference Loth, Charman, Mason, Tillmann, Jones, Wooldridge and Buitelaar2017). Briefly, LEAP employed a case-control design whereby males and females aged 6–30 years, with and without a formal diagnosis of autism spectrum disorder (ASD), were recruited simultaneously across seven European study sites. Subsequently, the cohorts were followed up longitudinally, after approximately 12–24 months. Participants were initially recruited via existing databases, schools and flyers; and those with mild intellectual disability (IQ ⩽ 75) were additionally recruited through clinic contacts or support groups. Although individuals with IQ ⩽ 75 were recruited to both ASD and comparison groups, we note that few met these criteria, partly due to the reasonably demanding nature of the full LEAP protocol and because some individuals believed to have mild intellectual disability based on an initial screener scored above 75 on standardised IQ measures (see Loth et al., Reference Loth, Charman, Mason, Tillmann, Jones, Wooldridge and Buitelaar2017).
In total, 337 participants aged 12–30 years (ASD N = 179) with available alexithymia data were included in this study. Table 1 shows participants’ characteristics on entry to the study (timepoint one; T1). A total of 135 individuals (ASD N = 76) were able to be followed up approximately 12–24 months later (timepoint two; T2). T2 participant characteristics are shown in online Supplementary Table S2.
Table 1. Descriptives and group comparisons for participant characteristics and alexithymia at T1
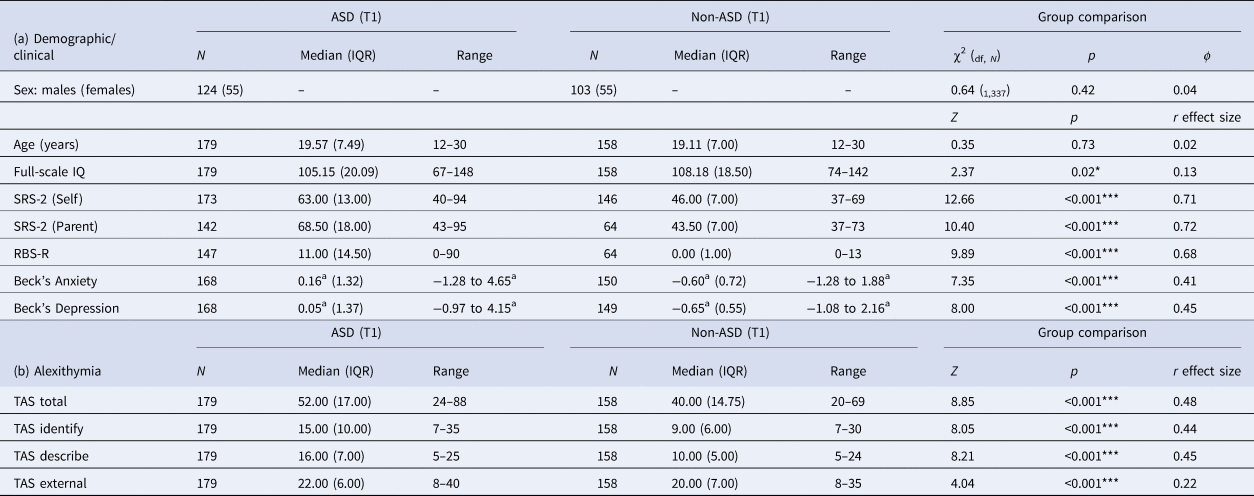
SRS-2, Social Responsiveness Scale-Second Edition; RBS-R, Repetitive Behaviour Scale-Revised; TAS, Toronto Alexithymia Scale; IQR, interquartile range; Z, statistic for Mann–Whitney comparison; χ2(df, N), χ2 test (degrees of freedom, number of participants); r, effect size (Z/√N).
a Scores z-transformed for comparability between youth and adult versions.
***p < 0.004 (significant after Bonferroni correction; p = 0.05/12).
On entry to the study, there were no significant differences between autistic and comparison individuals in age (p = 0.73, r effect size = 0.02) nor sex (p = 0.42, ϕ = 0.04). Autistic individuals had marginally lower average IQ than comparison individuals (p = 0.02, r = 0.13), although median scores were fairly comparable between groups (ASD median = 105.15, IQR = 20.09; comparison median = 108.18, IQR = 18.50). Autistic individuals had significantly more core autism traits (T1: p < 0.001; r ⩾ 0.68; T2: p < 0.001; r ⩾ 0.54) and higher mental health symptom severity (T1: p < 0.001; r ⩾ 0.41; T2: p < 0.001; r ⩾ 0.34) than comparison individuals across all measures, at both timepoints.
Participants who were able to be followed up at T2 did not significantly differ from non-returners on baseline age/sex (p ⩾ 0.14), alexithymia (p = 0.22), social-communication difficulties (p ⩾ 0.12), nor depression symptoms (p = 0.36). Returners had slightly higher IQ (p = 0.01) and lower anxiety (p = 0.05) and repetitive behaviours than non-returners (p = 0.02). Reasons for loss to follow-up included: participants returning at T2 but not completing the alexithymia measure; inability to make contact with participants; and personal circumstances that made participants unable to visit at T2.
Materials and procedures
Alexithymia
See online Supplementary Table S1 for a summary of all measures. To index alexithymia, we administered the 20-item self-report Toronto Alexithymia Scale (TAS-20; Bagby et al., Reference Bagby, Parker and Taylor1994), which has been previously validated for use in autism (Berthoz & Hill, Reference Berthoz and Hill2005). The TAS-20 results in a total score and three subscales: difficulties in identifying feelings (I am often puzzled by sensations in my body), difficulties in describing feelings (It is difficult for me to find the right words for my feelings) and externally oriented thinking (I prefer to analyse my problems rather than just describe them). As evident from these example items, one's awareness of their difficulties with emotions seems somewhat distinct from one's awareness that they are experiencing a positive or adverse emotional state.
Higher scores indicate higher alexithymia, with scores ⩾61 indicating ‘severe’ (i.e. clinically relevant) alexithymia (Parker, Taylor, & Bagby, Reference Parker, Taylor and Bagby2003). Alexithymia was weakly associated with verbal IQ – significant in the whole sample (r s = −0.24, p < 0.001) and marginal in the ASD group (r s = −0.16, p = 0.03), suggesting results were not wholly explained by difficulties in completing the TAS due to individual differences in verbal ability.
Core autism traits
The clinical characteristics of the full LEAP cohort are reported elsewhere (Charman et al., Reference Charman, Loth, Tillmann, Crawley, Wooldridge, Goyard and Buitelaar2017). In the current study, social-communication difficulties were measured using self- and parent-report versions of the Social Responsiveness Scale-2nd Edition (SRS-2; Constantino and Gruber, 2012). Higher scores (sex-specific T-norms) indicate more difficulties. Repetitive behaviours were measured using the parent-report Repetitive Behaviour Scale-Revised (RBS-R; Lam and Aman, Reference Lam and Aman2007), with higher scores indicating more repetitive behaviours.
Anxiety/depression symptoms
Beck's Anxiety and Depression Inventories (Beck, Beck, Jolly, & Steer, Reference Beck, Beck, Jolly and Steer2005; Beck, Epstein, Brown, & Steer, Reference Beck, Epstein, Brown and Steer1988; Beck, Steer, & Brown, Reference Beck, Steer and Brown2001) were used to capture self-reported anxiety and depression symptoms at two timepoints, ~12–24 months apart. Beck's Inventories were chosen on the basis of their fast administration time (reducing longitudinal participant burden) and ability to accurately screen for mental health problems in general population and autism samples (Cassidy, Bradley, Bowen, Wigham, & Rodgers, Reference Cassidy, Bradley, Bowen, Wigham and Rodgers2018; Leyfer, Ruberg, & Woodruff-Borden, Reference Leyfer, Ruberg and Woodruff-Borden2006). We administered a youth-version for ages 12–17 years and an adult-version for ages 18–30 years. Therefore, scores were z-transformed for comparability, with higher scores indicating more severe symptoms.
Statistical analyses
Analyses were performed using RStudio®. As some data violated the normality assumption, non-parametric analyses were used for group comparisons (Mann–Whitney) and correlations (Spearman's r s). For group comparisons, effect size r (calculated as Z/√N) is reported, with 0.10 denoting a small effect, 0.30 a moderate effect and 0.50 a large effect. Bonferroni correction was applied throughout. See Supplementary Table S3 for correlations between all T1 and T2 measures.
To investigate cross-sectional associations between alexithymia, and clinical features of social-communication difficulties, anxiety and depression symptoms, we first compared those who did v. did not meet cut-off (⩾61) for clinically relevant alexithymia – an approach that would also capture potentially non-linear relationships. Next, we investigated both cross-sectional and longitudinal relationships between alexithymia and clinical features in greater depth using linear (‘lm’) regression models. Dependent variables were, respectively, SRS-2-rated social-communication difficulties and Beck-rated anxiety/depression symptom. Independent variables across all models were age, IQ, sex and alexithymia (total/subscale scores).
Results
Alexithymia in the current sample
Autistic individuals reported, on average, significantly higher total alexithymia than comparison individuals, with a moderate effect size (p < 0.001, r = 0.48). Autistic individuals scored significantly higher than comparison individuals across TAS-20 subscales, particularly difficulties in identifying (p < 0.001, r = 0.44) and describing emotion (p < 0.001, r = 0.45; Table 1).
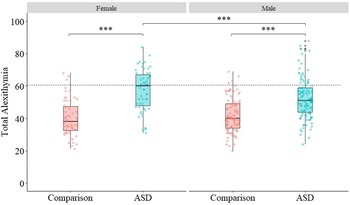
As demonstrated in Fig. 1, 29.1% (N = 52) of autistic individuals met cut-off for clinically relevant alexithymia (score ⩾61; Parker et al., Reference Parker, Taylor and Bagby2003), compared to 4.4% (N = 7) of comparison individuals. Autistic females were over-represented in the group who met cut-off (p = 0.001, χ2(1179) = 11.55, ϕ = 0.27). A total of 47.3% (N = 26) of autistic females met cut-off, compared to 21.0% (N = 26) of males. Autistic females in our sample also scored higher than males for self-reported social-communication difficulties (p = 0.01, r = 0.20). Conversely, there was no significant sex difference in alexithymia in the comparison group (p = 0.96, χ2(1158) = 0.003, ϕ = 0.04).
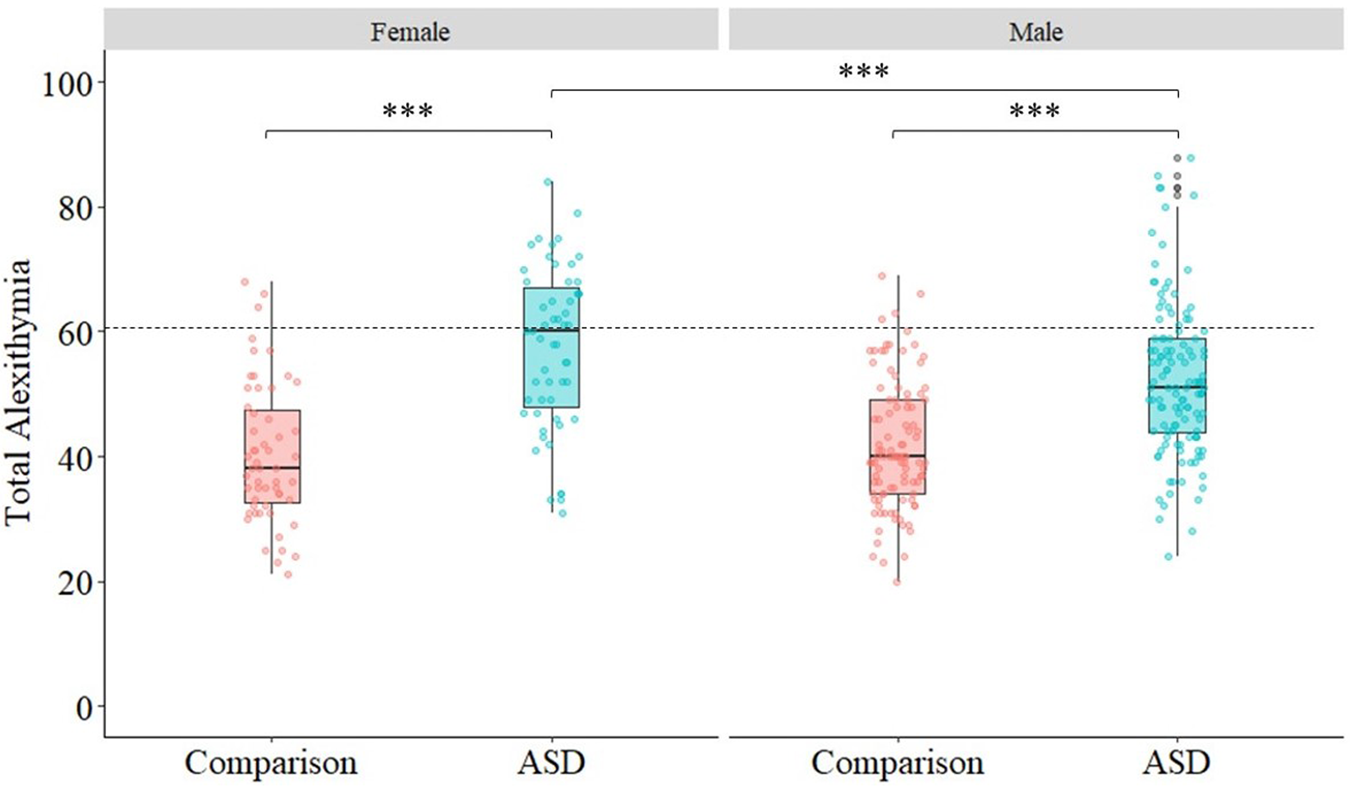
Fig. 1. Box plots showing median and IQR of total alexithymia in ASD and comparison groups, split by sex. Individual data plots are overlaid to demonstrate the variability of scores in both groups. Cut-off for severe alexithymia (⩾61) is indicated by the dashed line.
T1 associations between alexithymia and social-communication difficulties
First, we used a categorical approach to confirm that individuals with clinically relevant alexithymia scored higher for social-communication difficulties than those with lower levels of alexithymia (see online Supplementary Table S4). Overall, individuals who met cut-off for severe alexithymia had significantly higher SRS-2 self-reported social-communication difficulties (p < 0.001, r = 0.55) and, to a lesser degree, parent-reported social-communication difficulties (p < 0.001, r = 0.33) than those with lower levels of alexithymia. Similarly, in the ASD group, individuals with severe alexithymia scored high for SRS-2 self- (p < 0.001, r = 0.61) and parent-reported social-communication difficulties (p = 0.01, r = 0.22).
Next, we considered dimensional relationships between alexithymia (sub)scale scores and social-communication difficulties, controlling for potential confounds of age, IQ, sex and concurrent repetitive behaviours. In the whole sample, alexithymia remained significantly associated with SRS-2 self-reported social-communication difficulties, across all TAS-20 (sub)scales, with the strongest effect size for difficulties in describing feelings: total (p < 0.001, β = 0.62, 95% confidence interval (CI) 0.52–0.69), identify (p < 0.001, β = 0.53, 95% CI 0.40–0.59), describe (p < 0.001, β = 0.57, 95% CI 0.46–0.64) and external (p < 0.001, β = 0.28, 95% CI 0.16–0.38). Difficulty in describing feelings was also significantly related to SRS-2 parent-reported social-communication difficulties (p = 0.001, β = 0.19, 95% CI 0.08–0.29).
In the ASD group, alexithymia remained significantly associated with SRS-2 self- (but not parent-) reported social-communication difficulties, across all TAS-20 (sub)scales, with the strongest effect size for difficulties in describing feelings: total (p < 0.001, β = 0.64, 95% CI 0.51–0.73), identify (p < 0.001, β = 0.52, 95% CI 0.37–0.62), describe (p < 0.001, β = 0.57, 95% CI 0.44–0.67) and external (p = 0.001, β = 0.25, 95% CI 0.10–0.38).
T1 associations between alexithymia and anxiety/depression symptoms
Similar to the findings reported above, individuals who met cut-off for severe alexithymia had significantly higher T1 Beck-rated anxiety and depression symptom severity, as compared to those with lower levels of alexithymia – in the whole sample (p < 0.001, r ⩾ 0.42) and ASD group (p < 0.001, r ⩾ 0.46; online Supplementary Table S4).
Once again, we assessed dimensional relationships between alexithymia and anxiety/depression symptoms, controlling for potential confounds of age, IQ, sex and core autism traits. Based on findings from simple correlations (online Supplementary Table S3), we ran linear regression models for associations between all alexithymia (sub)scale scores, except for externally oriented thinking.
As shown in Table 2, difficulties in identifying feelings were significantly associated with anxiety symptom severity in the whole sample (p < 0.001, β = 0.54, 95% CI 0.41–0.69). Of note, when depression symptoms were also controlled for, the relationship between difficulties in identifying feelings and anxiety remained (p < 0.001, β = 0.28, 95% CI 0.15–0.40). The same pattern of effects was identified in the ASD group. Difficulties in identifying feelings accounted for significant variance in anxiety symptoms (p < 0.001, β = 0.54, 95% CI 0.41–0.77), even after controlling for depression (p = 0.001, β = 0.27, 95% CI 0.12–0.46).
Table 2. Regression coefficients and model fit statistics for T1 Beck-rated anxiety and depression symptom severity, regressed onto alexithymia scores, controlling for demographic factors and core autism traits in the: (a) whole sample; (b) ASD group
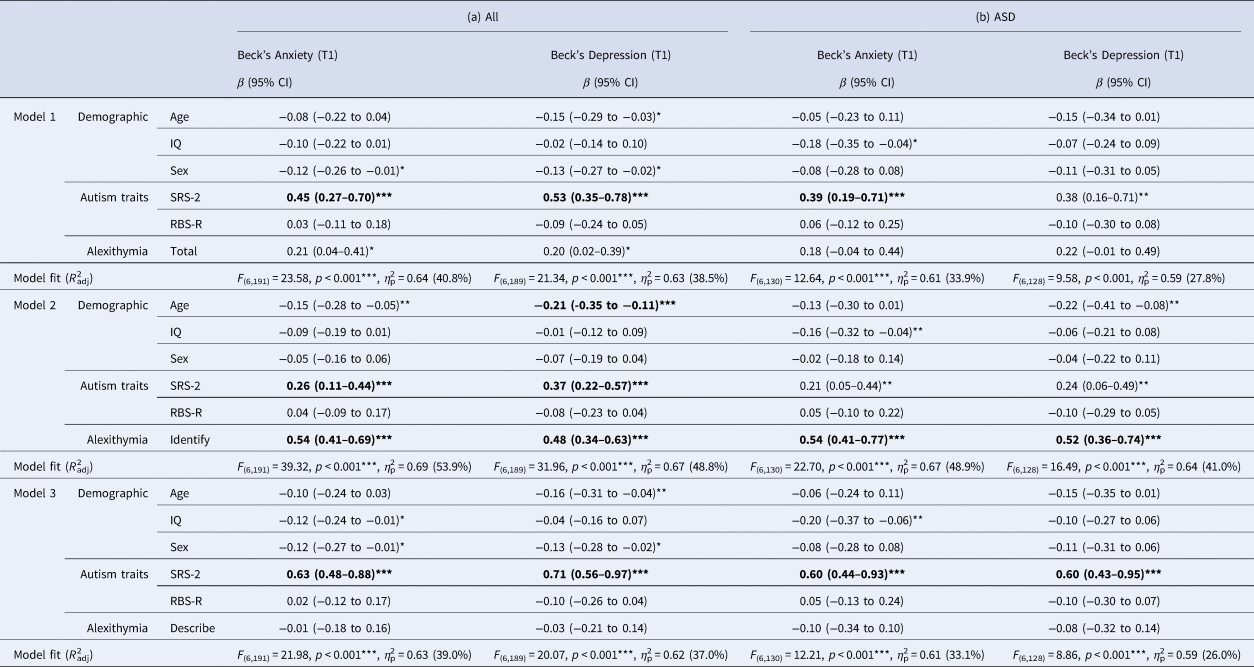
T1, timepoint 1; SRS-2, Social Responsiveness Scale-Second Edition (self-report); RBS-R, Repetitive Behaviour Scale-Revised; β (95% CI), regression coefficient with 95% confidence intervals.
*p < 0.05; **p < 0.01; ***p < 0.001 (significant after Bonferroni correction; p = 0.05/72).
In contrast, although difficulties in identifying feelings were also significantly associated with depression in the whole sample (p < 0.001, β = 0.48, 95% CI 0.34–0.63), this association fell to the marginal level for significance after controlling for anxiety (p = 0.04, β = 0.14, 95% CI 0.01–0.28). Similarly, in the ASD group, difficulties in identifying feelings were significantly associated with depression symptoms (p < 0.001, β = 0.52, 95% CI 0.36–0.74), but marginally after controlling for anxiety (p = 0.03, β = 0.19, 95% CI 0.02–0.38).
Post-hoc analysis using the ‘mediate’ function (10 000 iterations) showed that anxiety partly mediated associations between difficulties in identifying feelings and depression. a denotes the path from difficulty in identifying feelings to anxiety; b is the path from anxiety to depression symptoms and c′ is the direct path from difficulty in identifying feelings to depression. Although the direct path from difficulty in identifying feelings to depression remained (whole sample c′ = 0.04, s.e. = 0.01, p < 0.001; ASD c′ = 0.04, s.e. = 0.01, p < 0.001), anxiety was a significant, partial mediator of this relationship (whole sample a = 0.10, s.e. = 0.01, p < 0.001; b = 0.62, s.e. = 0.04, p < 0.001; ASD a = 0.10, s.e. = 0.01, p < 0.001; b = 0.58, s.e. = 0.06, p < 0.001).
Longitudinal associations between alexithymia, social-communication difficulties, anxiety and depression symptoms
Stability in measures over time
For those who participated at both timepoints, paired difference tests showed that, at the group level, alexithymia severity did not significantly change over time (p = 0.60, r = 0.05). Similarly, there was no significant change in self-reported social-communication difficulties (p = 0.17, r = 0.18), anxiety (p = 0.08, r = 0.15), nor depression symptoms (p = 0.10, r = 0.14).
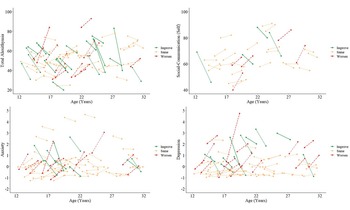
These effects were consistent when considering the ASD group only (alexithymia: p = 0.47, r = 0.08; social-communication: p = 0.22, r = 0.22; anxiety: p = 0.48, r = 0.08; depression: p = 0.20, r = 0.15; see Table 1 and online Supplementary Table S2 for descriptives). At the individual level, fewer than half of autistic participants exhibited a minimally clinically important change of >0.5 s.d. on any variable, between timepoints (see Norman, Sloan, and Wyrwich, Reference Norman, Sloan and Wyrwich2003). Individual longitudinal trajectories for alexithymia, social-communication difficulties, anxiety and depression are shown in Fig. 2.
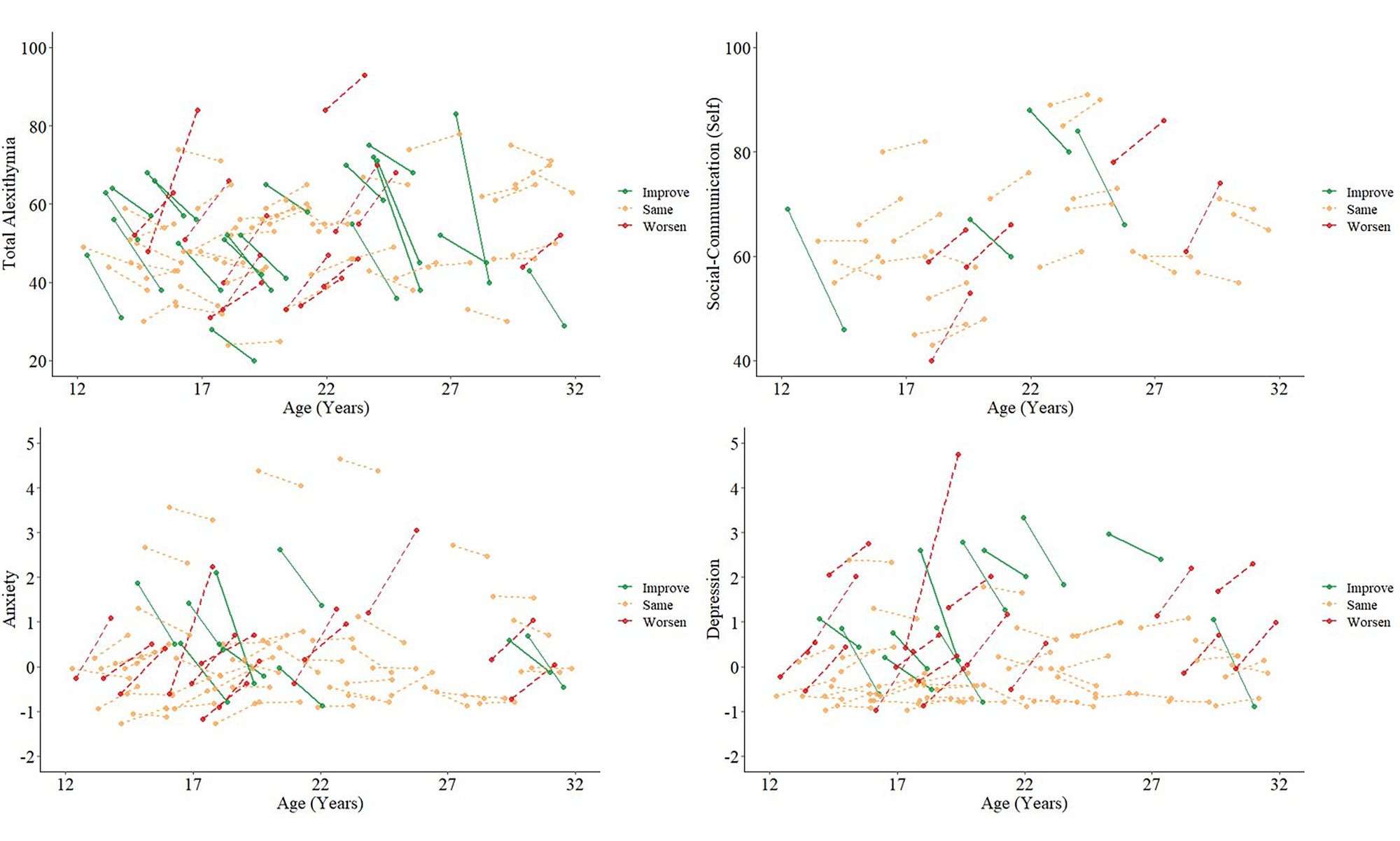
Fig. 2. Individual trajectories of alexithymia, self-reported social-communication difficulties, anxiety and depression from T1 to T2 for autistic individuals in our cohort. Few individuals experienced ‘minimally clinically important’ change (>0.5 s.d. from baseline score): total alexithymia N = 13 ‘worsen’, N = 20 ‘improve’, N = 43 ‘same’; self-reported social-communication difficulties N = 5 ‘worsen’, N = 4 ‘improve’, N = 22 ‘same’; anxiety N = 13 ‘worsen’, N = 9 ‘improve’, N = 48 ‘same’; depression N = 16 ‘worsen’, N = 11 ‘improve’, N = 44 ‘same’.
Social-communication difficulties
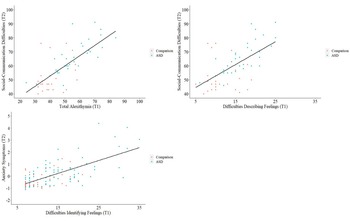
To ascertain whether earlier alexithymia was associated with later self-reported social-communication difficulties, anxiety and depression symptoms, over ~12–24 months, we conducted longitudinal regression analyses (Fig. 3).
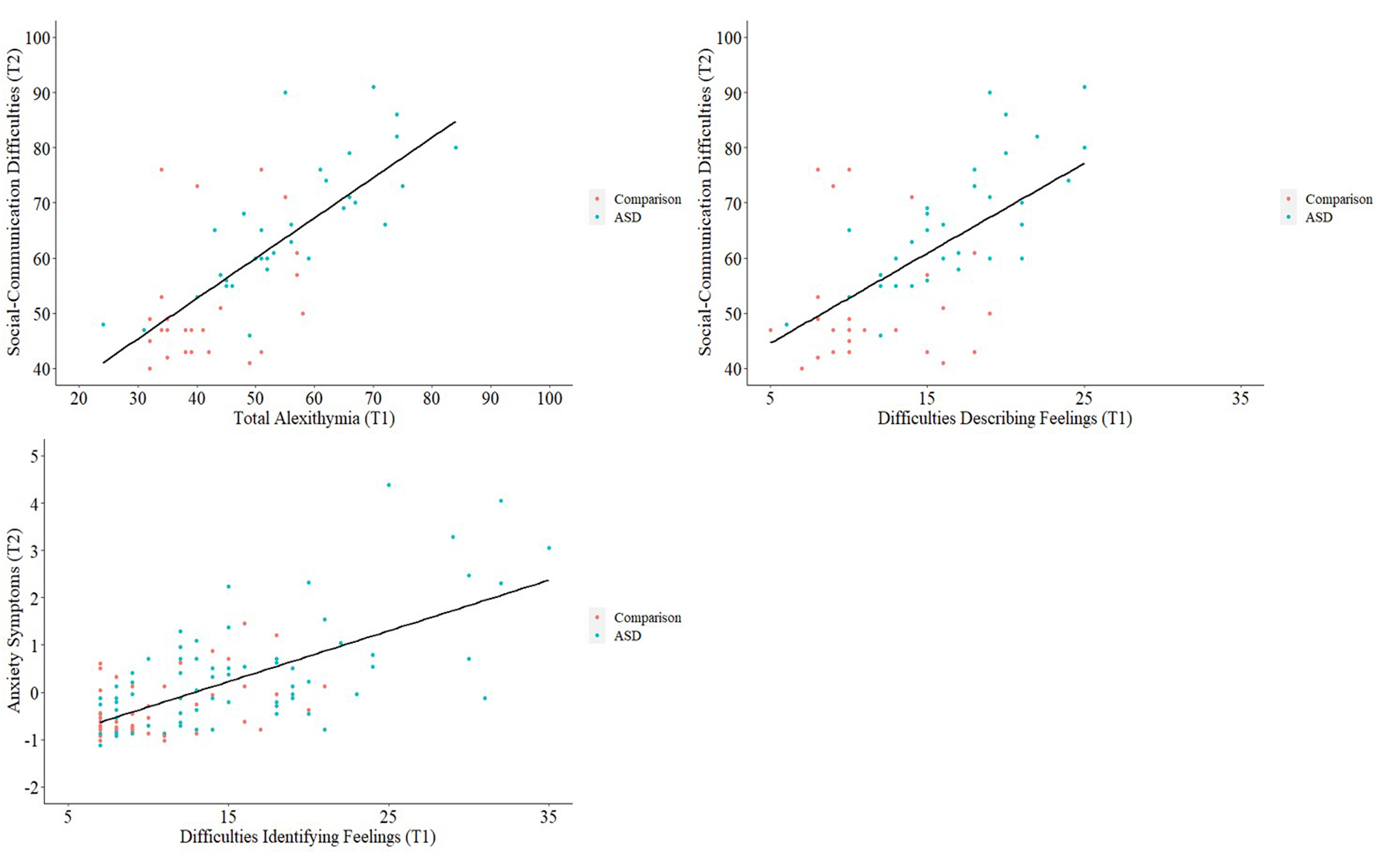
Fig. 3. Scatterplots with regression lines fitted, showing longitudinal relationships between T1 alexithymia and T2 self-reported social-communication difficulties and anxiety symptoms.
In the whole sample, no associations between alexithymia and social-communication difficulties were maintained longitudinally. Conversely, in the ASD group, T1 total alexithymia remained marginally associated with T2 self-reported social-communication difficulties, after controlling for age, IQ, sex, repetitive behaviours and T1 self-reported social-communication difficulties (p = 0.02, β = 0.52, 95% CI 0.09–0.92). The same was true for the association between T1 difficulties in describing feelings and T2 self-reported social-communication difficulties (p = 0.02, β = 0.43, 95% CI 0.07–0.82), although we caution that only N = 22 autistic individuals had sufficient longitudinal data. Overall both models were significant and accounted for over 59.0% of the variance in T2 self-reported social-communication difficulties in the ASD group (total F (6,22) = 8.01, p < 0.001, η p2 = 0.76, R 2adj = 60.0%; describe F (6,22) = 7.88, p < 0.001, η p2 = 0.76; R 2adj = 59.6%).
Anxiety/depression symptoms
T1 difficulty in identifying feelings remained associated with T2 anxiety symptoms in individuals with sufficient longitudinal data from both the whole sample (N = 76; p = 0.002, β = 0.32, 95% CI 0.12–0.52) and ASD group (N = 51; p = 0.01, β = 0.31, 95% CI 0.08–0.62), after accounting for demographic factors, core autism traits and T1 anxiety/depression symptoms. The overall model for this association was significant and accounted for over 69.0% of the variance in T2 anxiety symptom severity (whole sample F (8,76) = 26.43, p < 0.001, η p2 = 0.79 R 2adj = 70.8%; ASD F (8,51) = 17.86, p < 0.001, η p2 = 0.79 R 2adj = 69.6%).
No other longitudinal models showed significant associations between T1 alexithymia and T2 anxiety/depression symptoms, after controlling for other factors. Nevertheless, in simple correlations, T1 difficulties in identifying feelings remained associated with T2 depression (whole sample: r s = 0.47, p < 0.001; ASD: r s = 0.51, p < 0.001; Supplementary Table S3).
Discussion
Alexithymia and social-communication difficulties in autism
To our best knowledge, this is the most comprehensive study to date to assess cross-sectional – and the first to assess longitudinal – associations between alexithymia, social-communication difficulties, anxiety and depression symptoms in autistic males and females, during adolescence and early adulthood. First, we found that all facets of alexithymia (total severity, difficulties in identifying/describing feelings and externally oriented thinking) were significantly associated with concurrent self- (but not parent-) reported social-communication difficulties in autism. The strongest associations were between total alexithymia/difficulties in describing feelings and self-reported social-communication difficulties. Furthermore, associations between both total alexithymia and difficulties in describing feelings with self-reported social-communication difficulties were maintained longitudinally (albeit in a smaller subsample for whom data were available), and this was true even after controlling for age, IQ, sex, repetitive behaviours and earlier T1 social-communication difficulties.
This finding suggests that autistic individuals with lower emotional awareness, particularly those who find it challenging to describe their emotions, also perceive themselves to experience more interpersonal difficulties – although these difficulties may not be observed by others. This corresponds to previous findings from individuals with high alexithymia without autism (and analyses including the comparison group in this study), for whom difficulties with describing feelings are also the facet of alexithymia most strongly associated with interpersonal problems (Spitzer et al., Reference Spitzer, Siebel-Jürges, Barnow, Grabe and Freyberger2005).
One possible explanation for the observed associations between alexithymia and social-communication difficulties is that difficulties with emotion recognition and production disrupt everyday social interactions (Bothe, Palermo, Rhodes, Burton, & Jeffery, Reference Bothe, Palermo, Rhodes, Burton and Jeffery2019; Trevisan & Birmingham, Reference Trevisan and Birmingham2016). For instance, previous studies suggest some autistic individuals find it challenging to interpret others' facial emotion expressions; and non-autistic individuals experience difficulties in interpreting the expressions of autistic people (Brewer et al., Reference Brewer, Biotti, Catmur, Press, Happé, Cook and Bird2016a; Loth, Ahmad, Watson, Duff, & Duchaine, Reference Loth, Ahmad, Watson, Duff and Duchaine2018). Furthermore, given that difficulty in describing feelings was the alexithymia subscale most strongly related to social-communication difficulties, it is likely that broader (emotional) language impairments may be implicated (Lartseva, Dijkstra, & Buitelaar, Reference Lartseva, Dijkstra and Buitelaar2015). Indeed, in the current study, verbal ability was significantly (although weakly) associated with alexithymia in both the whole sample and autism group. In the wider literature, ‘acquired’ alexithymia has been reported following traumatic brain injury affecting language regions (Hobson et al., Reference Hobson, Brewer, Catmur, Gordon, Krueger, Chau and Grafman2018) and language delay/reduced depth of verbal expression are common in autism – observed from early development (Baird et al., Reference Baird, Simonoff, Pickles, Chandler, Loucas, Meldrum and Charman2006; Rieffe et al., Reference Rieffe, Meerum Terwogt and Kotronopoulou2007).
Nevertheless, since alexithymia was associated with self- but not parent-reported social difficulties in the autism group, it is also possible that some autistic individuals are highly aware of the impact of their emotional understanding on interpersonal relationships and experience low confidence in their social abilities. For example, difficulties in recognising the emotions and thoughts of others may lead to real-world negative social encounters or ‘catastrophising’ negative beliefs (e.g. ‘they must be upset with me’), which increase self-consciousness in future social interactions (Capriola, Maddox, & White, Reference Capriola, Maddox and White2017; Spain, Sin, & Freeman, Reference Spain, Sin and Freeman2016; van Roekel, Scholte, & Didden, Reference van Roekel, Scholte and Didden2010). Therefore, interventions for improving social communication in autism should not only focus on social skills, but also on emotional awareness. This may have wider benefits for improving subjective perceptions of social competence, reducing social anxieties and increasing confidence in social settings.
Difficulties in identifying feelings and anxiety/depression symptoms in autism
In addition, difficulties in identifying feelings were significantly and robustly associated with anxiety symptoms in autistic adolescents and adults – even after controlling for demographic factors, core autism traits and concurrent depression. Moreover, using longitudinal data, we ascertained that earlier difficulties in identifying feelings remained associated with anxiety symptoms approximately 12–24 months later, also after accounting for earlier T1 anxiety. Since alexithymia and anxiety were stable over time in over half of autistic individuals in this sample, findings suggest that the ability to accurately interpret one's own emotional state has a significant and persistent impact on mental health outcomes in autism. Overall, our findings lend support to the suggestion that, as progress is made in developing and modifying interventions for autistic people, the potentially primary role of emotional awareness must be considered (Conner et al., Reference Conner, White, Beck, Golt, Smith and Mazefsky2019).
The reported findings have wider implications for informing early intervention strategies to improve mental health outcomes in autism. Currently, cognitive behavioural therapy (CBT) is the most widely supported intervention for anxiety in autism (White et al., Reference White, Simmons, Gotham, Conner, Smith, Beck and Mazefsky2018). Similar to many psychological therapies, this approach requires individuals to reflect on and discuss emotions and their antecedents. Yet, paradoxically, autistic individuals with particularly low emotional awareness are the most likely to be referred for CBT (likely due to associated mental health problems; Roberts-Collins, Mahoney-Davies, Russell, Booth, and Loades, Reference Roberts-Collins, Mahoney-Davies, Russell, Booth and Loades2018). This raises several questions around the long-term effectiveness of current treatment approaches and highlights the stark need for additional research to develop and evaluate treatment modifications for managing mental health symptoms in autism (Walters, Loades, & Russell, Reference Walters, Loades and Russell2016). Notably, emotion recognition training is included in current guidance from the UK National Institute for Health and Care Excellence on the adaptation of CBT for autism (National Institute of Health & Care Excellence, 2013), for which this study provides empirical support.
A key direction for future research is, therefore, to assess whether incorporating techniques specifically targeting emotional awareness could improve therapeutic outcomes for autistic people. For instance, psychological interventions that specifically target, rather than passively measure, alexithymia have been found to be successful in reducing alexithymic traits and improving emotion regulation skills in neurotypical populations (Cameron, Ogrodniczuk, & Hadjipavlou, Reference Cameron, Ogrodniczuk and Hadjipavlou2014). Such methods have tended to focus on psychoeducation and stress-management. However, the efficacy of these techniques for improving outcome in autism, and other neurodevelopmental/neuropsychiatric conditions characterised by high rates of alexithymia, is yet to be confirmed (Cooper, Loades, & Russell, Reference Cooper, Loades and Russell2018).
Another outstanding issue for future research is to establish the mechanistic processes that connect emotional awareness and mental health outcomes (e.g. anxiety) over time. Emotion regulation difficulties are one candidate underpinning mechanism for mental health gaining increasing attention in the autism literature (Cai, Richdale, Uljarević, Dissanayake, & Samson, Reference Cai, Richdale, Uljarević, Dissanayake and Samson2018), with emotion awareness argued to be the first and most fundamental aspect of successful emotion regulation (Gross, Reference Gross2015). For instance, if the accurate identification of one's current emotion is impeded, this may hinder the implementation of adaptive emotion regulation strategies, including cognitive reappraisal (reinterpreting the emotion) and situation selection/modification (adjusting the environment; Gross and Thompson, Reference Gross, Thompson and Gross2007).
Adaptive emotion regulation may also be impeded by broader difficulties in interpreting internal bodily states (i.e. interoception) that indicate heightened arousal or anxiety, such as elevated heart and breathing rate (Garfinkel, Eccles, & Critchley, Reference Garfinkel, Eccles and Critchley2015; Müller et al., Reference Müller, Schulz, Andermann, Gäbel, Gescher, Spohn and Bertsch2015). Of note, the Beck's Anxiety Inventory indexes several physiological anxiety symptoms (heart/breathing rate and trembling) and some previous studies suggest that alexithymia is related to general interoceptive impairments, across affective and non-affective domains (Brewer, Cook, & Bird, Reference Brewer, Cook and Bird2016b; Murphy, Catmur, & Bird, Reference Murphy, Catmur and Bird2018). Furthermore, alongside alexithymia, autistic individuals have been shown to experience elevated interoception and emotion regulation difficulties – engaging in fewer ‘voluntary’ (e.g. cognitive reappraisal – reinterpreting emotional stimuli) and more ‘involuntary’ regulation strategies (e.g. rumination and arousal) than neurotypical individuals (Gross, Reference Gross2015; Mazefsky, Borue, Day, & Minshew, Reference Mazefsky, Borue, Day and Minshew2014; Samson, Hardan, Lee, Phillips, & Gross, Reference Samson, Hardan, Lee, Phillips and Gross2015). Thus, difficulties with emotional, and broader internal bodily, awareness may compromise ‘downstream’ emotion regulation processes, increasing vulnerability for mental health problems such as anxiety.
Finally, we note that while relationships between difficulties in identifying feelings and anxiety symptoms were robust, we identified a more complex pattern of results for depression. Difficulties in identifying feelings and depression were associated cross-sectionally, although associations fell to the marginal level for significance after also controlling for anxiety. In addition, after accounting for other factors, earlier difficulties in identifying feelings were not longitudinally associated with depression symptoms 12–24 months later, in the whole sample, nor the autism group. This may suggest that associations between alexithymia and depression symptoms are explained by wider shared factors, such as co-occurring anxiety (Milosavljevic et al., Reference Milosavljevic, Carter Leno, Simonoff, Baird, Pickles, Jones and Happe2016), or situational factors such as social withdrawal and loneliness (Hedley, Uljarević, Foley, Richdale, & Trollor, Reference Hedley, Uljarević, Foley, Richdale and Trollor2018). In support of this suggestion, a post-hoc mediation analysis showed that anxiety partly mediated cross-sectional associations between difficulties in identifying feelings and depression.
Strengths and limitations
A major strength of our study is the inclusion of a heterogeneous, well-characterised sample of autistic males and females, aged 12–30 years. By including females, we were able to ascertain that significantly more diagnosed autistic females than males report high alexithymia. This implies that observed sex differences in rates of co-occurring emotional symptoms in autism (i.e. higher rates of anxiety/depression in autistic females; Mandy et al., Reference Mandy, Chilvers, Chowdhury, Salter, Seigal and Skuse2012) may be explained by sex differences in their underpinning mechanisms. Furthermore, to our best knowledge, this is the first study to report longitudinal associations between alexithymia and social-communication difficulties, anxiety and depression symptoms in autism. We were thus able to confirm that alexithymia in our cohort was generally stable over a period of approximately 12–24 months, supporting the conceptualisation of alexithymia as a trait, rather than state (Salminen, Saarijärvi, Ääirelä, & Tamminen, Reference Salminen, Saarijärvi, Ääirelä and Tamminen1994). However, we also acknowledge several limitations.
First, although we report associations between alexithymia and anxiety/depression symptoms for the whole sample (including the comparison group), in addition to the autism group, these must be interpreted with some caution. This is because clinically relevant mental health symptoms were screened out in the comparison (but not ASD) group on recruitment. We chose to report findings including our comparison group to address questions pertaining to specificity. For instance, associations between alexithymia and concurrent social-communication difficulties, as well as between alexithymia and concurrent/later anxiety symptoms were consistent between the whole sample and autism group. This adds to literature suggesting that the role of alexithymia in relation to mental health outcomes is not specific to a single neurodevelopmental/neuropsychiatric condition (e.g. autism), but instead a broader, diagnostically cross-cutting mechanism for mental health (National Institute of Mental Health, 2019). Furthermore, our findings imply that there are likely significant ‘commonalities’ in the nature of underpinning risk factors for mental health symptoms between autistic and neurotypical individuals, however they may differ in frequency/intensity.
Second, due to the lack of availability of self-report alexithymia measures for children and individuals with intellectual disability (Griffin, Lombardo, & Auyeung, Reference Griffin, Lombardo and Auyeung2016; Loas, Braun, Delhaye, & Linkowski, Reference Loas, Braun, Delhaye and Linkowski2017), we were only able to include autistic individuals aged ⩾12 years, with IQ ⩾ 67. This prevented us from assessing whether associations between alexithymia and anxiety and depression symptoms were consistent across developmental stage and level and from generalising findings beyond the age range of 12–30 years. Indeed, a longitudinal period of 12–24 months is a reasonably short window for capturing traits that may have been established earlier in development. Therefore, a prospective longitudinal approach will be beneficial for further elucidating the mechanistic pathways linking alexithymia and outcomes in autism. In relation to this point, we were unable to assess the role of alexithymia in predicting change in social-communication difficulties, anxiety and depression symptoms between timepoints, due to the small number of participants who significantly changed on these features within the study period. It is still notable that we were able to include autistic individuals from age 12, since early adolescence is the developmental stage at which anxiety and depression symptoms most commonly emerge for both autistic and non-autistic individuals (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005; Simonoff et al., Reference Simonoff, Pickles, Charman, Chandler, Loucas and Baird2008). Nevertheless, the development and validation of tools for indexing alexithymia in under-represented groups is paramount (see Gaigg, Cornell, and Bird, Reference Gaigg, Cornell and Bird2016).
Conclusions
Alexithymia, and particularly difficulty in describing feelings, is significantly associated with greater self-reported social-communication difficulties in autism, both cross-sectionally and longitudinally. Furthermore, difficulty in identifying feelings is related to anxiety symptom severity, including over a longitudinal period of at least 12–24 months. Taken together, these findings show that the influence of alexithymia on social functioning and anxiety is both substantial and persistent for autistic people – and possibly for autistic girls and women in particular. This has notable implications for intervention, indicating that psychological therapies targeting emotional awareness may improve later outcomes for some individuals.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720003244
Acknowledgements
We thank all participants and their families for their time and effort in participating in the study. We also acknowledge the contributions of the EU-AIMS Consortium: Jumana Ahmad, Sara Ambrosino, Bonnie Auyeung, Tobias Banaschewski, Simon Baron-Cohen, Sarah Baumeister, Christian Beckmann, Sven Bölte, Thomas Bourgeron, Carsten Bours, Michael Brammer, Daniel Brandeis, Claudia Brogna, Yvette de Bruijn, Bhismadev Chakrabarti, Ineke Cornelissen, Flavio Dell’ Acqua, Guillaume Dumas, Christine Ecker, Claire Ellis, Jessica Faulkner, Vincent Frouin, Pilar Garcés, David Goyard, Hannah Hayward, Joerg Hipp, Rosemary Holt, Mark H. Johnson, Prantik Kundu, Meng-Chuan Lai, Xavier Liogier D'ardhuy, Michael Lombardo, David J. Lythgoe, René Mandl, Luke Mason, Andreas Meyer-Lindenberg, Carolin Moessnang, Nico Mueller, Laurence O'Dwyer, Marianne Oldehinkel, Bob Oranje, Gahan Pandina, Antonio M. Persico, Barbara Ruggeri, Amber Ruigrok, Jessica Sabet, Roberto Sacco, Antonia San José Cáceres, Emily Simonoff, Roberto Toro, Heike Tost, Jack Waldman, Steve C.R. Williams, Caroline Wooldridge and Marcel P. Zwiers.
Financial support
This study received support from two EU IMI initiatives (EU AIMS and AIMS-2-TRIALS). EU-AIMS receives support from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement no. 115300, resources of which are composed of financial contribution from the European Union's Seventh Framework Programme (FP7/2007–2013), from the European Federation of Pharmaceutical Industries and Associations (EFPIA) companies' in-kind contribution, and from Autism Speaks. This project has also received funding from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No. 777394 for the project AIMS-2-TRIALS. This Joint Undertaking receives support from the European Union's Horizon 2020 research and innovation programme and EFPIA and AUTISM SPEAKS, Autistica, SFARI.
Conflict of interest
Prof. Charman reports grants from Innovative Medicines Initiative, during the conduct of the study; grants from Medical Research Council, the National Institute of Health Research, MQ, Autistica, Charles Hawkins Fund, The Waterloo Foundation, H2020 (EU); personal fees from Guilford, Sage, F. Hoffmann-La Roche, outside the submitted work. Prof. Buitelaar has been in the past 3 years a consultant to/member of advisory board of/and/or speaker for Janssen Cilag BV, Eli Lilly, Lundbeck, Shire, Roche, Novartis, Medice and Servier. He is not an employee of any of these companies, and not a stock shareholder of any of these companies. He has no other financial or material support, including expert testimony, patents and royalties. Prof. Murphy receives consultancy fees from F. Hoffmann-La Roche and is also supported by the NIHR Biomedical Research Center. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. There are no other declarations.
Ethical standards
All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and the Helsinki Declaration of 1975, as revised in 2008. Full ethical approval was obtained at each study site and participants (and parents, where applicable) provided full informed consent/assent.