The Department of Health publication Building a Safer NHS for Patients sets out the Government’s plans for promoting patient safety (Department of Health, 2001). This follows growing international recognition that health services around the world have underestimated the scale of unintended harm or injury experienced by patients as a result of medical error and adverse events occurring in health care settings. These plans include a commitment to replace the procedures set out in the Department of Health circular HSG(94)27. This guidance details the methods for investigating every homicide (and some suicides) by patients in current or recent contact with specialist mental health services. Part of the process to modernise HSG(94)27 includes a plan to build expertise within the National Health Service (NHS) in the technique of root cause analysis. This investigative process was developed in industry to identify causal or systems factors in serious adverse events.
What is root cause analysis?
Root cause analysis (RCA) is a component of the broader field of total quality management, which has arisen from the world of business management. Many of the ‘toolbox’ problem-solving techniques of total quality management are overarching concepts with the ultimate aim of continuous improvement in quality (Reference Gitlow, Oppenheim and OppenheimGitlow et al, 1995), and RCA is an integral part of this process. It has been defined as a structured investigation that aims to identify the true cause of a problem and the actions necessary to eliminate it. It incorporates a wide range of approaches, tools and techniques for uncovering such causes.
The causes of untoward events in large organisations often have complex interrelationships. These can be grouped into ‘first-level causes’ (causes that directly lead to a problem), ‘higher-level causes’ (which do not directly cause the problem, but provide links in the chain that ultimately leads to the problem) and ‘root causes’ - the ‘ evil at the bottom’ that sets in motion the cause and effect chain (Reference Andersen and FagerhaugAndersen & Fagerhaug, 2000). The application of RCA requires familiarity with the variety of problem-solving techniques available in order to be able to select the best one for the problem at hand. There is no prescribed RCA method for investigations in mental health services.
Application to mental health services
Rose (Reference Rose2000) has described in detail a method of conducting internal investigations in mental health services and the RCA process should aim to build on these experiences. A suggested process for investigating a serious incident is shown in the Appendix.
The team ‘brainstorming’ process (see Appendix) in an RCA is structured in various ways according to the problem under consideration (Reference Andersen and FagerhaugAndersen & Fagerhaug, 2000). A number of techniques have been identified as particularly suitable for RCA of a mental health service incident. The relations diagram (Fig. 1) is a tool used to identify logical relationships between different ideas or issues in a complex or confusing situation. The strength of the relations diagram lies in the way it enables investigators to visualise these relationships, understand how different aspects of the problem are connected, and detect links between the problem and its possible causes that can be further analysed. One method of determining an unexpected cause is to identify ‘drivers’ (more outputs than inputs) and ‘indicators’ (more inputs than outputs) in the relations diagram. Once the web of interrelationships has been established from the diagram, the ‘five whys’ technique can be used to delve more deeply into the higher levels of the causes. For each possible cause, the RCA team ask why that event occurred until all possible higher-level causes have been identified (Fig. 2). The technique is so called because asking the question five times, for each first-level cause, should be sufficient to determine all the contributory causes.
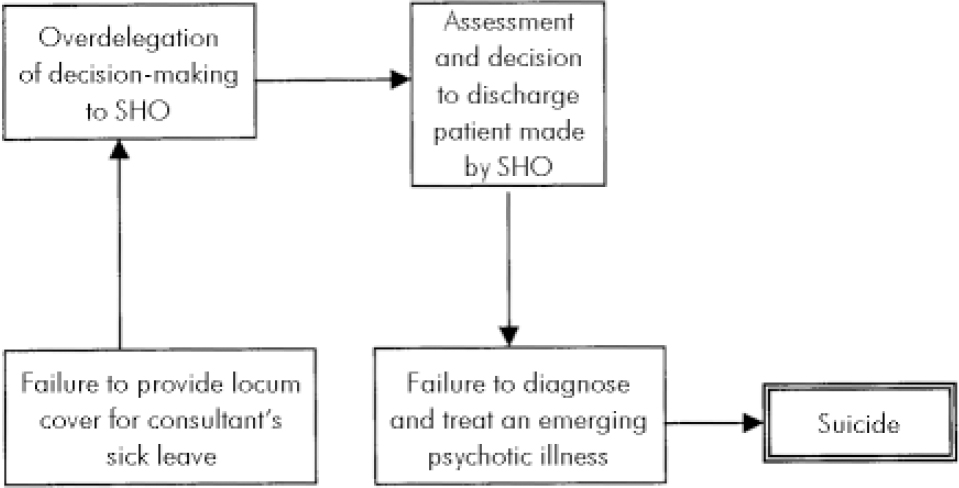
Fig. 1. Simplified relations diagram in a fictitious suicide. SHO, senior house officer.

Fig. 2. Charting the ‘five whys’ in the fictitious suicide.
A proposed classification system for factors contributing to serious incidents in mental health services is shown in Table 1. This can be applied to the fictitious suicide under consideration in the form of an ‘affinity chart’ (Table 2). This allows exploration of relationships among different causes (often at different levels in the cause hierarchy) and groups related causes into classes that can then be treated collectively. A series of recommendations for Trust policies and procedures are then generated. The final step in the RCA is for the organisation to use the findings to review its systems and introduce changes at the operational or managerial level where appropriate. An audit process should be developed to oversee the timely review and implementation of such changes.
Table 1. Draft classification system for factors contributing to serious untoward incidents in mental health services

| Factor type | Influencing and contributory factors |
|---|---|
| Institutional | Legislative, regulatory and economic context |
| Organisational and managerial | Resource management; aims and priorities; organisational structure, policy standards and development, interagency links; communication |
| Environmental | Real estate; equipment, support services and human resources |
| Team | Structure; aims; communication; leadership; management; supervision; monitoring; morale |
| Individual | Training; knowledge; skills, competence; health |
| Task and process | Delegation; communication; understanding; availability and utility of policies and procedures |
| Patient | Condition (physical, psychological and social); forensic history; culture; language and communication |
Table 2. Factor classification system applied to fictitious suicide

| Factor type | Influencing and contributory factors |
|---|---|
| Institutional | Recruitment and retention problems in psychiatry |
| Organisational | No policy for inability to provide consultant cover |
| Task or process | Manager’s decision to allow SHO to run the ward without supervision |
| Team | Unexpected temporary loss of consultant psychiatrist |
| Individual | Failure by SHO to diagnose and treat psychosis |
| Equipment and resources | No locum consultant psychiatrist available |
| Patient | Psychotic disorder with command hallucinations |
Limitations
Although RCA is a structured approach to investigation, using tried and tested principles from industry, it is unlikely to be a panacea for all of the problems linked with serious incident inquiries, which have been described as a ‘highly irrational quasi-legal form of local audit’ (Reference SalterSalter, 2003). It is therefore important not to allow the RCA to become a reinvented form of tribunal dressed up as a pseudoscientific process. There are three distinct areas where limitations should be recognised. First, the term ‘root cause analysis’ when used in this context is probably something of a misnomer. The process is unlikely to uncover some hitherto unknown fundamental (root) cause, but rather draw attention to areas of interrelated clinical and managerial processes that might be improved. The expectation of finding a ‘ cause’ is misleading. Inferring causation from a single case study requires a degree of confidence over and above determining an association, which is problematic in the scientific analysis of human behaviour. Determining that a specific activity or omission in the administration of mental health care (a harmful intervention) was actually the cause of a single homicide or suicide is almost impossible given the level of scientific evidence required (Reference Sackett, Haynes and GuyattSackett et al, 1991). Furthermore, biases have been identified, based on errors in human cognitive processing, associated with inferring causation retrospectively in inquiries. These include selectively focusing on data consistent with the previously revealed outcome ‘hindsight bias’ (Reference Hawkins and HastieHawkins & Hastie, 1990) and speculating on what might have happened if a different course of action had been taken. Conclusions from the latter may carry a pleasing ring of truth, but may be meaningless. This effect has been termed ‘ counterfactual bias’ (Reference ReissReiss, 2001).
The value and the ethics of risk assessment and management in reducing suicides and homicides is a topic of contemporary debate (Reference KennedyKennedy, 2001; Szmukler, 2001, Reference Szmukler2003; Reference MadenMaden, 2003). Methods of risk reduction such as the care programme approach and clinic risk assessment/management do not yet have good quality evidence derived from randomised controlled trials to establish their effectiveness in preventing suicides or homicides, despite their introduction as official health policy (Reference Marshall, Gray and LockwoodMarshall et al, 1997; Reference Macpherson, Cornelius and KilpatrickMacpherson et al, 2002). Therefore, categorical statements that failure to implement these processes correctly led to a particular serious incident are debatable, and RCA will not provide the answers to this issue.
Benefits
The original Department of Health procedures required all homicides and some suicides to be investigated by lawyers in a legalistic process, which seemed designed to find a culprit rather than a cause. This process was loathed by mental health staff who saw it as pointless and punitive (Reference SzmuklerSzmukler, 2000). In contrast, RCA is a systematic process of data collection and analysis, which should be consistent between investigations, does not require lawyers and need not be threatening or intrusive. If it is applied with respect to the limitations described above, it could be of value to the health care system while avoiding the need to apportion blame. The focus on systems, processes and mutual learning, rather than on personal failings, should make it more acceptable to individuals unfortunate enough to be caught under the microscope.
The application of RCA by an independent team from outside the NHS Trust in which the incident occurred might have additional benefits. The rarity of serious events means that an independent investigating team operating regionally or nationally would quickly gain experience that would only be acquired over many years by internal investigations in any individual Trust (Reference RoseRose, 2000).
Conclusions
The benefits of RCA as a means of reducing the incidence of serious untoward events in the mental health service are yet to be tested, but this process does promise to be more efficient and consistent, and less threatening and demoralising to clinical staff.
Appendix
The root cause analysis team
The root cause analysis (RCA) team comprises three or four experienced mental health workers (encompassing the professions of psychiatry, nursing and social work). The team leader is trained in RCA techniques and is also a mental health worker.
Process
-
1. Define the terms of the investigation.
-
2. Define the boundaries of the investigation in terms of the time frame (the critical event period).
-
3. Obtain all available documents relating to the critical event period.
-
4. Collect and tabulate data in the form of a chronology of events (event-specific, person-specific or both).
-
5. Develop a preliminary chronology from the available documents.
-
6. Use the preliminary chronology to inform whether more documents, individual interviews (including relatives of the dead person) or a site visit are required.
-
7. Interviews and site visit by two team members.
-
8. Refine the chronology with information from the additional sources.
-
9. Team meeting to‘brainstorm’ the analysis, facilitated by the RCA-trained team leaders, using relations diagram, the ‘five whys’ technique and an affinity diagram.
-
10. Formulate the findings in terms of listed suggestions for review and change.







eLetters
No eLetters have been published for this article.