The lifetime prevalence of bipolar affective disorder is approximately 1% in both men and women (Reference Reiger, Boyd and BurkeReiger et al, 1998). In women the illness is most prevalent in the child-bearing years (Reference Robins, Helzer and WeissmanRobins et al, 1984). While lithium for the treatment of bipolar disorder is a cornerstone of modern psychopharmacology (Reference Llewellyn, Stowe and StraderLlewellyn et al, 1998), there are inherent problems in treating this sizeable subgroup of patients, as lithium presents small, but significant, risks to a potential foetus. It is also becoming increasingly obvious that serious mental illness poses a risk to the unborn child. This paper reviews those risks, presents a protocol in algorithmic form for dealing with the prescription of lithium in pregnancy and discusses practical issues pertaining to dosage and lithium monitoring.
Risks of lithium to the foetus
Historically, lithium has been associated with a high incidence of a rare congenital heart defect; Epstein's anomaly, a prolapse of the tricuspid valve into the right ventricle. Original papers put the risk as high as 400 times that expected in the general population (Reference Nora, Nora and ToewsNora et al, 1974). However, more contemporary epidemiological studies indicate that the teratogenic risk of first-trimester lithium exposure is lower than previously suggested (Reference Cohen, Friedman and JeffersonCohen et al, 1994). The UK National Teratology Information Service have concluded that lithium increases the risk of all types of malformation of approximately three-fold and with a weighting towards cardiac malformations of around eight-fold (McElhatton, personal communication, 1997). Considered against a background incidence of spontaneous malformations of 2-3% of live births, this probably means that there is a one in 10 chance of some form of congenital problem from a woman taking lithium during pregnancy.
There are potential dangers towards the end of the third trimester. These appear to be related to lithotoxicity in the foetus, with case reports of cardiac arrhythmias (Reference Stevens, Burman and MidwinterStevens et al, 1974), cyanosis and hypertonicity (Reference WoodyWoody, 1971). Some studies have also described congenital goitre and neonatal hypothyroidism.
Both risks of teratogenicity and lithotoxicity can be minimised by close and careful monitoring of lithium treatment.
To treat or not to treat?
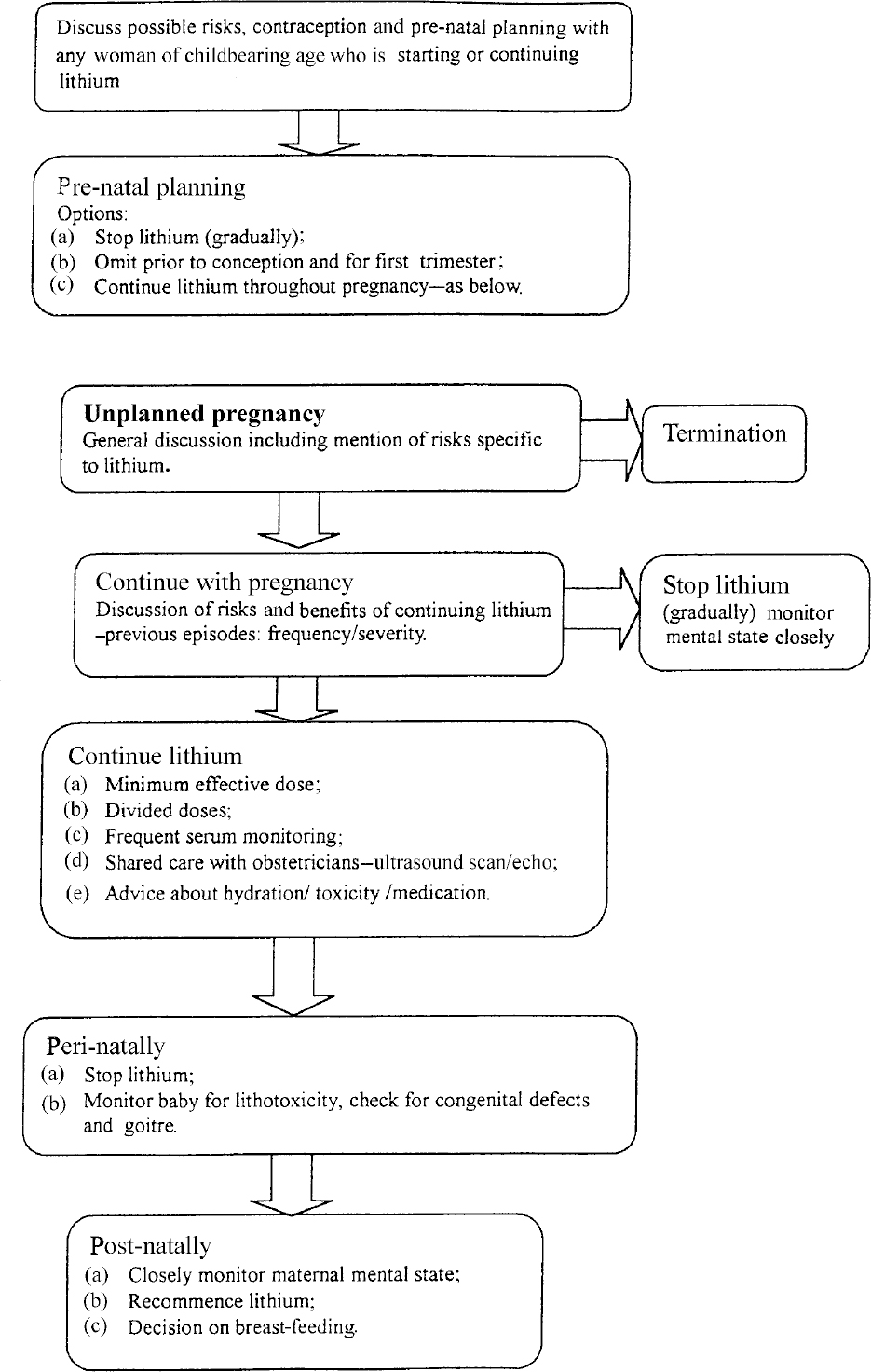
When consideration is given to prescribing lithium to any women of child-bearing age, appropriate counselling regarding possible risks in pregnancy should form part of the more general discussion of therapy (see Fig. 1).
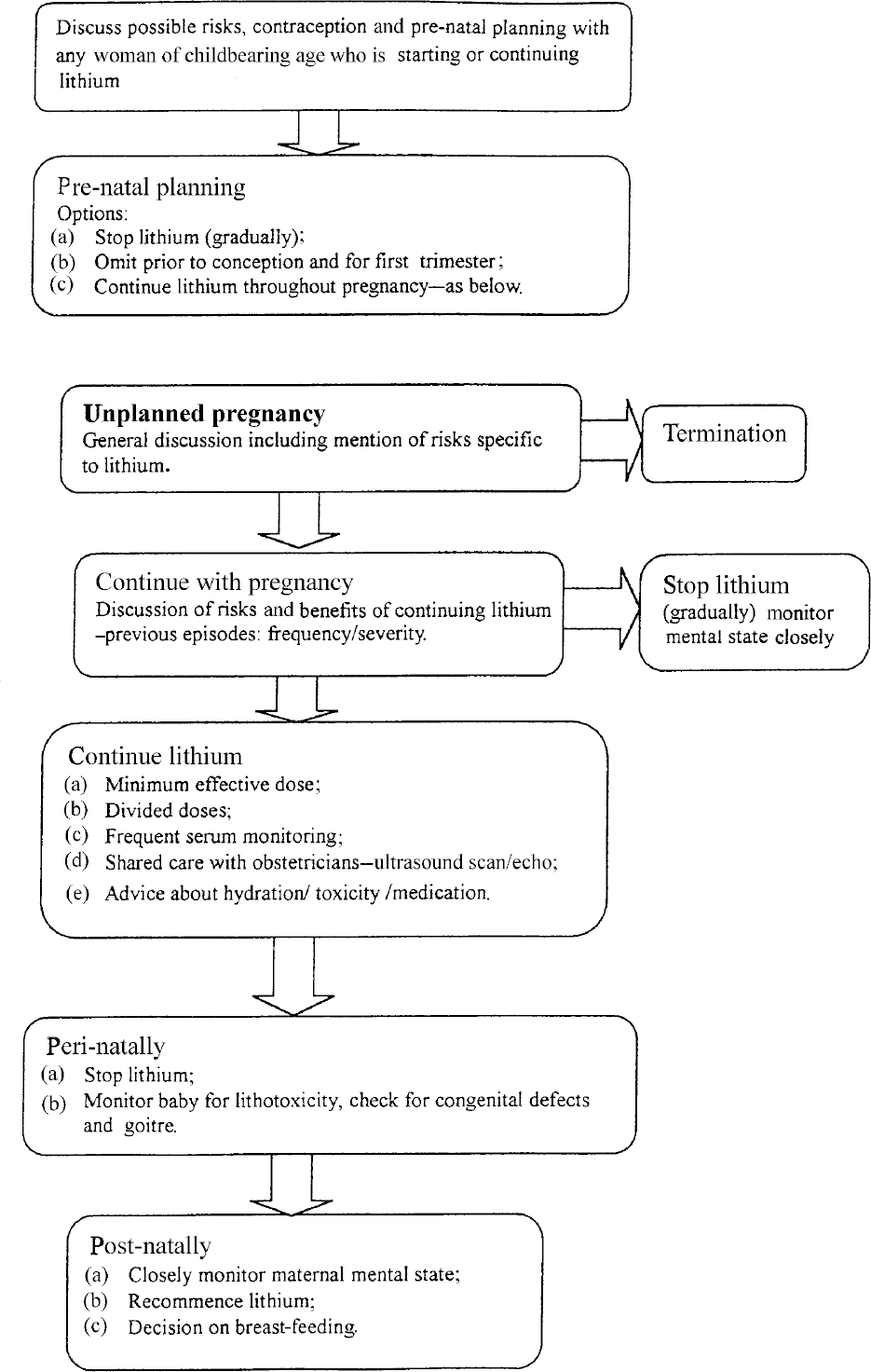
Fig. 1 Algorithm: managing lithium in pregnancy
If pregnancy is planned, ideally lithium should be avoided throughout the period including the time of conception. If lithium is to be discontinued in this context, it is advisable to taper it off slowly over the course of at least two weeks as the likelihood of relapse is far greater when withdrawal is abrupt (Reference Suppes, Baldessarini and FaeddaSuppes et al, 1991). One option in a planned pregnancy is to omit lithium during the period of conception and embryogenesis, then recommence it in the second trimester.
It may, therefore, be appropriate to continue therapy for all of the pregnancy. However, the patient can only make such a decision after a full discussion of possible risks to the foetus from lithium, balanced against the dangers of a relapse of affective illness should the medication be discontinued. This risk takes the form of disturbed behaviour and physical harm to the unborn child, poor antenatal care, increased risk-taking behaviour, drug and alcohol misuse, deliberate self-harm and suicide and disturbed behaviour during labour and delivery. As well as this there are the potential hazards to the foetus of exposure to drugs and to electroconvulsive therapy used in the treatment of an acute relapse. Teixeira et al (Reference Reiger, Boyd and Burke1998) described the possible physiological effects of anxiety on the foetus. It is possible to conjecture a similar physiological disturbance secondary to disturbed mental state in an acute relapse. Clear documentation of the discussion of these risks with the patient and her family is crucial. In some situations a second opinion may be useful.
A common management dilemma is in the presentation of a patient towards the end of the first trimester who has conceived unknowingly while on lithium. The decisions facing the patient are two-fold. First, whether to continue with the pregnancy or opt for termination. Discussion here involves consideration of broader issues, but must include mention of possible risks to the foetus. An ultrasound scan and foetal echo cardiography can be helpful at 18-20 weeks. The results of this can advise whether a late termination of pregnancy should be considered. Advice from the paediatrician is essential at this point. Preparatory counselling is obviously essential before such an investigation is undertaken. Second, if the pregnancy is to continue, the next decision is whether to stop or continue lithium therapy.
Continuing lithium in pregnancy
In continuing lithium during pregnancy, the rationale is to maintain a stable mental state on the minimum dose of lithium possible.
Physiological changes during pregnancy mean that body fluid space for the distribution of lithium increases, tending to dilute plasma concentrations. The increase in glomerular filtration rate can increase renal clearance of lithium; paradoxically the tendency to sodium depletion and selective resorption of lithium at the proximal tubule can increase lithium levels. Hyperemesis, fever, reduced fluid intake or dietary restriction of salts can all raise lithium levels. Various drugs including thiazide diuretics and non-steroidal anti-inflammatory drugs have similar effect. Given this, more frequent monitoring of lithium levels is appropriate, and we would recommend monthly checks of lithium, urea, electrolytes and creatinine with at least one check of thyroid function in mid- to late pregnancy.
During delivery renal clearance of lithium falls dramatically and may lead to toxicity in both mother and newborn. It is, therefore, recommended that lithium dose should be decreased or discontinued 7-10 days before delivery (Reference Goldberg and NissimGoldberg & Nissim, 1994).
Care needs to be shared with a consultant obstetrician. High-resolution ultrasound examination and foetal echocardiography at 16-18 weeks is recommended.
Lithium perinatally
Lithium should be omitted once labour has begun to minimise foetal levels at birth. The paediatric team should be aware of impending delivery and may wish to attend. A period of observation of the neonate may be appropriate.
Lithium postnatally
Lithium should be restarted a few days after delivery with an appropriately reduced dose. The mother's mental state should be monitored closely in the puerperal period because of increased risk of relapse. Physiological adjustments after birth means that a close check needs to be made on serum lithium levels and the patient advised to maintain adequate levels of hydration. We would recommend that in normal circumstances, levels be checked towards the end of the first week then re-checked after a month. A repeat thyroid function test in the puerperium is also advisable.
The issue of breast-feeding while on lithium is controversial. Lithium readily passes into breast milk with subsequent exposure of the nursing infant. Reliable longterm data of infants exposed to lithium in breast milk is not available. Despite the benefits of breast-feeding extreme caution should be exercised in considering it as an option.
Monitoring lithium levels
Lithium readily crosses the placenta and foetal serum concentration is similar to that of the mother (Reference Llewellyn, Stowe and StraderLlewellyn et al, 1998). Therefore, dividing the daily dose of lithium reduces peak levels of lithium and the potential for adverse effects on the foetus.
Following a single dose of lithium, plasma levels peak at 2-4 hours before falling to half of the peak level after about six hours (Reference Aronson, Hardman and ReynoldsAronson et al, 1993). There is little difference between plasma levels after 12 and 24 hours (> <0.1). It is convention to assay levels at 12 hours. If twice-daily dosage is being used, 12-hour serum levels are checked before the second dose is taken. For appropriate therapeutic ranges reference should be made to the product manufacturer.
Original literature recommended that individual doses should not exceed 300 mg (Reference Goldfield and WeinsteinGoldfield & Weinstein, 1973). However, it is our view that the size of the dose is irrelevant, providing that serum monitoring reflects an appropriate therapeutic level. There is probably little to be gained from using a regime of more than twice daily dosing, because of adherence problems and difficulties interpreting serum monitoring.
Acknowledgement
The National Teratology Information Service at the NHS Northern and Yorkshire collates a wealth of information on drugs in pregnancy and has been of invaluable help in preparing this paper. We would like to thank Professor Channi Kumar for his advice and support.



eLetters
No eLetters have been published for this article.