Most people with mental health problems want to work, and employment is extremely important in maintaining and enhancing the health and social functioning of people with serious mental health problems and promoting their social inclusion (Royal College of Psychiatrists, 2002; Social Exclusion Unit, 2004). There is increasing research evidence which demonstrates that the ‘individual placement and support’ (IPS) approach, also known as evidence-based supported employment, is effective in enabling a substantial proportion of people with serious mental health problems to gain and sustain open employment (Reference Bond, Becker and DrakeBond et al, 2001; Reference Crowther, Marshall and BondCrowther et al, 2001; Reference BondBond, 2004).
Individual placement and support involves integrating employment specialists into community clinical teams and ensuring vocational issues are a core component of the care planning process. The approach requires that there is a primary focus on helping people to gain jobs in open employment, in line with their preferences, as quickly as possible, without protracted pre-vocational training. Support is provided to anyone who wishes to work, without any selection based on their ‘employability’ or ‘ work readiness’; advice on welfare benefits is provided and time-unlimited ongoing support enables people to maintain employment and develop their careers. Within some services, supported education is delivered concurrently to enable people with severe mental health problems to access, participate and succeed in postsecondary education (Reference Mowbray, Megivern and CollinsMowbray et al, 2003).
Much of the evidence for the effectiveness of IPS comes from the USA (Reference BondBond, 2004). There is little evidence of the impact of such approaches in routine clinical settings in the UK. Studies of supported employment focus on enabling people to gain jobs once they have lost them; however, it is equally important to prevent people from losing their jobs in the first place (see Royal College of Psychiatrists, 2002; Reference Rinaldi, Mcneil and FirnRinaldi et al, 2004).
This paper reports an evaluation of the impact of introducing IPS in community mental health teams (CMHTs) in two London boroughs. The naturalistic aspect of the design is strengthened by the fortuitive differential introduction of IPS across these two boroughs and the absence of its introduction in CMHTs in a neighbouring borough. A comparison of the number of people supported to work or study in mainstream settings offered the opportunity to observe the impact of the introduction of IPS within these CMHTs.
Method
Data
The CMHTs involved in this study were all within South West London and St George's Mental Health Trust; there were four from Kingston and four from Merton where IPS had been introduced and four from Sutton where there was no IPS in place. Demographic and clinical data were collected on all clients who received a vocational intervention between January 2002 and June 2005 across the 12 CMHTs. These included age, gender, ethnicity, diagnosis, care programme approach level, duration of contact with the team and professional providing vocational support. Information on vocational status was collected on first contact with each client and thereafter on a monthly basis.
Intervention
The initial vocational model adopted by the trust did not involve fully implemented IPS. Occupational therapists were designated as clinical vocational leads in the CMHTs. Care coordinators were expected to provide vocational support to clients on their case-load supported by the occupational therapists and a single employment specialist working across the four CMHTs in each borough. All three London boroughs involved started with this ‘ occupational therapist supported by a shared employment specialist’ model in 2002 (Reference Davis and RinaldiDavis & Rinaldi, 2004).

Fig. 1. Number supported in open employment, mainstream education and/or training and mainstream work experience and/or voluntary work across the four community mental health teams in Kingston.
As resources became available, the number of employment specialists increased to the point where there was a full-time specialist in each of the four Kingston CMHTs in September 2003, thus enabling the provision of IPS achieving high model fidelity (Reference Bond, Becker and DrakeBond et al, 1997). The resources to provide an employment specialist in the four Merton CMHTs were obtained a year later, with IPS implementation in January 2005. Fully implemented IPS was not introduced in the four CMHTs in Sutton: the ‘occupational therapist supported by a shared employment specialist’ model continued, with access to a sheltered workshop run by the voluntary sector with a supported employment service attached to it.
Employment specialist role
The employment specialist role within the team was threefold:
-
• They worked directly with clients in a case management approach: engaging them, assessing their vocational needs, proactively helping them to gain and retain work/educational courses, provided welfare benefits advice (in relation to work/education), and ensured that support needs were met, including any adjustments necessary to enable clients to retain work/education. They did not have a care coordination role, but only held vocational responsibilities and were fully integrated as an equal member of the CMHT.
-
• They worked indirectly, providing information, advice, guidance and support to care coordinators to help them support their clients in work/education and ensure that vocational needs were addressed. A key role for the employment specialist was to coordinate vocational plans with the relevant CMHT staff and to ensure clients' vocational goals were given a high priority in the care planning process. Much of the ongoing support to retain employment/education was provided by care coordinators, with both direct and indirect assistance from the employment specialist.
-
• They also developed a good knowledge of local labour markets and employment opportunities and worked directly with, and provided support for, employers, Jobcentre Plus, employment agencies, Connexions, colleges, other mainstream training providers, and specialist employment/training services for people with mental health problems run by other agencies. This sort of liaison and support increased the capacity of these organisations to accommodate people with mental health problems.
Results
The number of people supported in open employment, mainstream education and mainstream work experience/voluntary work in the CMHTs in each of the three boroughs is shown in Figs 1, 2 and 3. Although the design used does not allow confident statements about causality, a comparison of the outcomes does suggest that the introduction of IPS had a marked positive impact on the number of people supported in open employment.
The initial ‘occupational therapist supported by a shared employment specialist’ model had a limited effect in all boroughs. With the introduction of a half-time employment specialist into the Kingston CMHTs in October 2002, the number of people supported in work/education rose (Fig.1) but did not increase in Merton (Fig. 2) or Sutton (Fig. 3). When full, high-fidelity IPS was implemented in Kingston, the most striking impact was on the number supported in open employment, which rose from 36 in September 2003 to 128 in June 2005. Over the same period, the number supported in main-stream education/training more than doubled from 26 to 69, and the number supported in mainstream voluntary work/work experience rose from 16 to 23.
After an initial limited increase with the introduction of the ‘ occupational therapist supported by a shared employment specialist’ approach in Merton, vocational outcomes plateaued until February 2004 when an employment specialist was introduced into three of the four CMHTs. However, the major increase in the number supported in open employment, education and work experience/voluntary work, which was observed in Kingston, was not observed in Merton until full, high-fidelity IPS was introduced in January 2005. The number of people supported in open employment almost doubled from 45 to 89 in the 6 months between December 2004 and June 2005 (Fig. 2). There was also just under a 50% increase in the number supported in mainstream education/training (from 14 to 24) and mainstream work experience/voluntary work (from 18 to 27).
In Sutton, where full IPS was not introduced, the increases in number of people supported in open employment, mainstream education and mainstream work experience/voluntary work which were associated with the introduction of full IPS were not observed (Fig. 3).
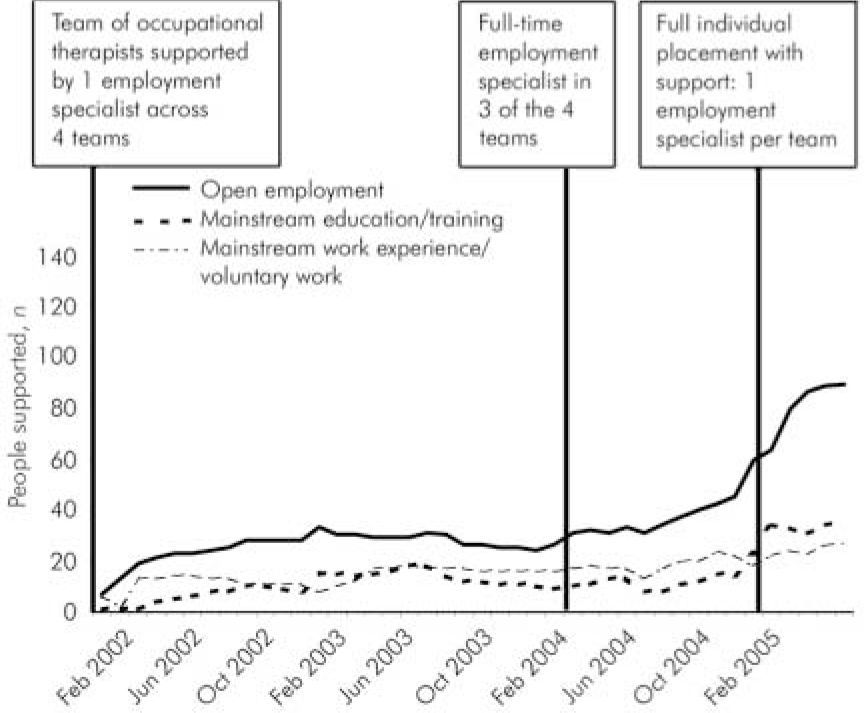
Fig. 2. Number supported in open employment, mainstream education and/or training and mainstream work experience and/or voluntary work across the four community mental health teams in Merton.
Data for 6-month follow-up were available for 451 clients who received a vocational intervention either directly from the employment specialist or from other care coordinators within the CMHTs supported by the specialist. Data for 12-month follow-up were available for 210 clients. The remaining 241 clients had either not received a vocational intervention for 12 months or had left the service between 6 and 12 months.
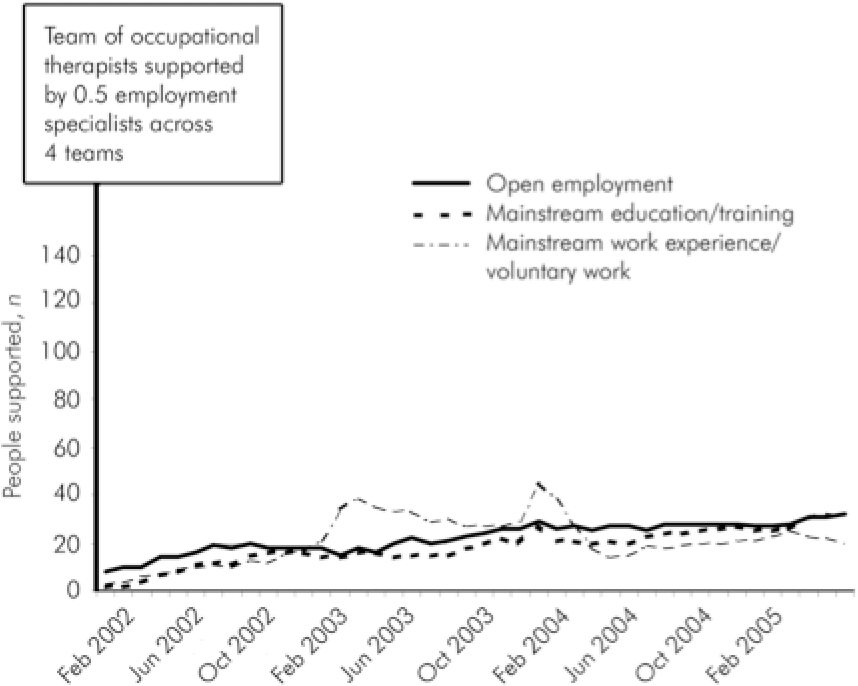
Fig. 3. Number supported in open employment, mainstream education and/or training and mainstream work experience and/or voluntary work across the four community mental health teams in Sutton.
Table 1 shows the demographic and clinical data for the 451 clients. Mean age was 39 years (s.d.=11.2, range 18-68 years). The majority of clients had more serious mental health problems: 57% had some form of psychotic diagnosis, 86% were on the enhanced level of care planning and 67% had been in contact with the CMHT for a year or more.
Table 1. Demographic and clinical characteristics of the 451 clients who received a vocational intervention between January 2002 and June 2005
| Clients n (%) | |
|---|---|
| Gender | |
| Male | 231 (51) |
| Female | 220 (49) |
| Ethnicity | |
| White | 329 (76) |
| Mixed | 21 (5) |
| Asian or Asian British | 36 (8) |
| Black or Black British | 41 (9) |
| Other ethnic group | 9 (2) |
| Diagnosis | |
| Schizophrenia | 145 (33) |
| Bipolar disorder | 68 (16) |
| Other psychosis | 33 (8) |
| Depression | 137 (31) |
| Anxiety-based problems | 14 (3) |
| Other | 40 (9) |
| Contact with community mental health | 300 (67) |
| teams >1 year at baseline | |
| Enhanced care programme approach | 378 (86) |
Table 2 shows the vocational status of those people for whom 6-month outcome data were available. These results suggest that the combined efforts of the employment specialist and care coordinators had a significant impact on vocational status. At the start of the intervention, 30% were working/studying in a mainstream setting, but by 6 months this had risen to 56%. The proportion in open employment rose from 18 to 30% whereas the proportion who were unemployed and had no structured day time activity fell from 48 to 21% (χ2=385.1, d.f.=16, P<0.001).
Table 2. Vocational status of clients at 6 months (n=451)
| Vocational status | Clients at start n (%) | Clients at 6 months1 n (%) |
|---|---|---|
| Open employment | 83 (18) | 136 (30) |
| Mainstream education/training | 28 (6) | 66 (15) |
| Mainstream voluntary work/work | 25 (6) | 48 (11) |
| experience | ||
| Other structured activity (sheltered work, day service, etc.) | 97 (22) | 104 (23) |
| Unemployed and/or unoccupied | 218 (48) | 97 (21) |
Table 3 shows the vocational outcomes for the 210 people for whom 12-month follow-up data were available. A smaller proportion of this group (24%) were working or studying in a mainstream setting at the start of the intervention, and a larger proportion were unemployed and without any structured day time activity (58%). However, by 12 months their vocational status had improved significantly: 63% were working/studying in mainstream settings and 16% were unemployed and without any structured day time activity (χ2=89.5, d.f.=16, P<0.001).
Table 3. Vocational status of clients at 12 months (n=210)
| Vocational status | Vocational status at start n (%) | Vocational status achieved in first 12 months1 n (%) |
|---|---|---|
| Open employment | 24 (11) | 68 (32) |
| Mainstream education/training | 12 (6) | 34 (16) |
| Mainstream voluntary work/work | 14 (7) | 31 (15) |
| experience | ||
| Other structured activity (sheltered work, day service etc.) | 39 (19) | 44 (21) |
| Unemployed/unoccupied | 121 (58) | 33 (16) |
Table 4 shows the difference between outcomes for the clients who received a vocational intervention directly from the CMHT employment specialist and those who received it from care coordinators supported by the employment specialist as necessary. Employment specialists appear to have been significantly more successful in enabling people to obtain and/or keep open employment than were other care coordinators. At 6 months, 38% of people receiving a vocational intervention from an employment specialist were being supported in open employment compared with 12% supported by other care coordinators (χ2=34.9, d.f.=4, P<0.001). At 12 months, 39% of people receiving a vocational intervention from an employment specialist were being supported in open employment compared with 10% of those supported by a care coordinator (χ2=19.2, d.f.=4, P<0.001).
Table 4. Vocational outcomes for clients of employment specialists and other care coordinators at 6 and 12 months
| With employment specialist | With other team member | |
|---|---|---|
| Open employment, n (%) | ||
| 6 months | 118 (38) | 18 (12) |
| 12 months | 63 (39) | 5 (10) |
| Mainstream education/training, n (%) | ||
| 6 months | 36 (12) | 30 (21) |
| 12 months | 23 (14) | 11 (22) |
| Mainstream work experience/voluntary work, n (%) | ||
| 6 months | 34 (11) | 14 (10) |
| 12 months | 25 (16) | 6 (12) |
| Working/studying in mainstream integrated settings, n (%) | ||
| 6 months | 188 (61) | 62 (43) |
| 12 months | 111 (69) | 22 (44) |
In order to explore the extent to which clients' vocational status had improved at 6 and 12 months, the vocational categories used were ranked. As open employment was the primary focus of IPS, this was ranked ‘1’; mainstream education was ranked ‘2’ and mainstream work experience/voluntary work was ranked ‘3’; structured occupation in segregated, specialist mental health settings was ranked ‘4’ and inactivity was ranked ‘5’. A person was considered to have improved if they moved from a lower to a higher ranked vocational category. Results showed that the proportion of people whose vocational status improved was greater for those supported by an employment specialist. Six months after the start of the intervention the vocational status of 46% of those supported by an employment specialist had improved compared with 30% of those supported by a care coordinator (Fisher's exact test P=0.001). Twelve months after the start of intervention this gap had widened: the vocational status of 62% of those supported by an employment specialist had improved compared with 37% of those supported by a care coordinator (Fisher's exact test P=0.002).
At the start of the intervention a higher proportion of women compared with men were in open employment (24 and 13% respectively; χ2=9.7, d.f.=4, P<0.05). This difference was maintained after 6 months: 37% of women and 24% of men were in open employment (χ2=19.5, d.f.=4, P<0.001). However, it was no longer evident at 12 months (χ2=5.3, d.f.=4, P=0.259). There was also a difference between the proportion of people from different ethnic groups who were in open employment. A higher proportion of Asian/Asian British clients were in open employment (31%) compared with White (17%) or Black/Black British clients (12%) (χ2=32.5, d.f.=16, P<0.01). However, after 6 months there was no longer a significant difference between ethnic groups (χ2=14.2, d.f.=16, P=0.582) or at 12 months (χ2=22.4, d.f.=16, P=0.131).
In relation to clinical variables, there was no difference between the proportion of people with psychotic and non-psychotic diagnoses who were in open employment either at the start (χ2=2.7, d.f.=4, P=0.613) or at 6 (χ2=2.8, d.f.=4, P=593) or 12 months (χ2=3.7, d.f.=4, P=0.450). However, although there was no difference in the employment rates for people on enhanced and standard care programme approach (χ2=2.3, d.f.=4, P=0.674) or for people who had been in contact with the CMHT for longer periods (χ2=6.3, d.f.=8, P=0.614), there was a difference at 6-month follow-up. Those on standard care were significantly more likely than those on enhanced care to be in open employment at 6 months (44 and 28% respectively, χ2=9.7, d.f.=4, P<0.05). However, this difference had disappeared at 12-month follow-up (χ2=6.5, d.f.=4, P=0.162). Similarly, at 6-month follow-up those who had been in contact with the CMHT for more than 1 year were less likely to be in employment than those who had been in contact for 6-12 months, or less than 6 months (41, 32 and 27% respectively, χ 2=15.0, d.f.=8, P<0.05). However, again, this difference had disappeared at 12-month follow-up (χ2=8.2, d.f.=8, P=0.412). This suggests that people with more complex needs and those who have been in contact with services for longer periods might require a longer period of support if they are to secure open employment.
Discussion
The results reported in this naturalistic study support the use of IPS in clinical practice in CMHTs. During the period from January 2002 to June 2005, the number of people supported to obtain and/or keep open employment, mainstream education and voluntary work/work experience rose substantially after the introduction of IPS in Kingston and Merton. The naturalistic aspect of the design is strengthened by the fact that IPS was introduced at different times in these two London boroughs and was not introduced at all in the neighbouring borough of Sutton.
Modifying the role of occupational therapists to enable them to dedicate designated time to vocational issues, and providing limited support from an employment specialist outside the CMHT, did increase the numbers of people supported in work and education. However, by introducing a full-time employment specialist into the CMHT and fully implementing IPS, the increases were far more striking, especially in relation to open employment. The former approach enabled 14 people in Kingston, 23 in Merton and 16 in Sutton to be supported in open employment. However, the introduction of IPS caused these figures to rise dramatically. In February 2004, 6 months after the full implementation of IPS across the Kingston CMHTs, 60 people were being supported in open employment but only 26 in Merton. However, in June 2005, 6 months after the introduction of IPS in Merton, 89 people were being supported in open employment. Eighteen months after the full implementation, 128 people were being supported in open employment in Kingston. The positive impact of IPS is further reinforced by the absence of such increases in Sutton where IPS was not implemented and the number supported in open employment plateaued at between 25 and 30.
Six-month follow-up data showed a significant increase in the proportion who were working or studying in mainstream settings (from 30 to 56%) and from those supported in open employment (from 18 to 30%). The 12-month follow-up data showed in this cohort a smaller proportion were working or studying in mainstream settings at the start of the intervention, but after 12 months this figure had increased to 63%.
The results obtained here indicate the importance of specialist employment expertise. O'Brien et al (Reference O'Brien, Price and Burns2003) failed to demonstrate any significant impact on employment of providing training for existing clinical staff in vocational issues. It is noteworthy that the present results show that outcomes for those people who were directly supported by an employment specialist were significantly superior to those supported by their care coordinator, even though these care coordinators had access to the advice and support of the employment specialist. Of those people for whom 6-month follow-up data were available, 38% of those receiving an intervention from the employment specialist were in open employment compared with 12% of those supported by their care coordinator. Of those for whom 12-month follow-up data were available, the comparable figures stood at 39 and 10% respectively.
These outcomes are in line with those achieved in randomised controlled trials of IPS in the USA (Reference Drake, Mchugo and BeckerDrake et al, 1996; Reference Lehman, Goldberg and DixonLehman et al, 2002; Meuser et al, 2004). They suggest that IPS can also be effective in the UK and in routine clinical practice as well as research trials. These results also replicate previous research findings that there is no relationship between diagnosis and the outcomes of supported employment. However, they do suggest that, although there is no relationship between complexity or duration of problems and outcomes at 12 months, those who are on the enhanced care programme approach and those who have been in contact with services for a longer period might require slightly longer periods of support if they are to be successful in gaining open employment.
Research data from the USA consider only those people who were assisted to gain employment. Those with more serious mental health problems are even more likely to become unemployed (Reference Perkins and RinaldiPerkins & Rinaldi, 2002). The current results suggest that IPS might be equally effective in enabling those who were already in employment to retain this employment where it was jeopardised by the person's mental health difficulties. In those CMHTs where IPS was fully implemented, 88% of those who were employed at the start of their intervention remained in employment in June 2005.
In conclusion, this naturalistic study supports the use of IPS in clinical practice in UK CMHTs, as recommended in the Department of Health commissioning guidance (Department of Health, 2006).
Declaration of interest
None.










eLetters
No eLetters have been published for this article.