Every day, around 4000 elderly psychiatric patients (National Audit Office, 2003) are stuck unnecessarily in hospitals across England. These patients are referred to as ‘delayed discharges’ – or more commonly ‘bed blockers’ – because they occupy beds when they no longer need the care provided in a hospital setting.
The Community Care Act 2003 (Department of Health, 2003), which received Royal Assent on 8 April 2003, was introduced to produce a real and sustained reduction in delayed transfers of care from hospital. Specific government funding (the Delayed Discharge Grant) of £300 million over 3 years was made available to support the development of services to deal with this. However, the Act concerned only patients in ‘acute care’ and decreed that ‘there will be further discussion in Parliament before mental health patients are brought into the scope of the Act’ (Department of Health, 2003). Thus, elderly psychiatric patients continue to remain as the subgroup of patients most exposed to delays in hospital discharge. A study conducted in 2000 (Angunawela et al) examined the impact of the Community Care Act 1990. It was found that there had been delays in the care management process by social services in discharges for people with dementia requiring residential or nursing home placements.
The present study was carried out at Leigh Infirmary (Wrightington, Wigan and Leigh National Health Service (NHS) Trust), a district general hospital in Lancashire, in the old age psychiatry unit. There are two 25-bed in-patient wards there: one for functional patients and one for patients with dementia. The department is led by three consultants and their respective teams who are responsible for the mental health needs of around 48 000 residents aged 65 years and over in the catchment area.
Patients who are admitted to the wards undergo assessment by the medical and nursing teams, an occupational therapist and a social worker, together deciding on the level of care required by the patient. These recommendations are then put to the family who, with the help of the social worker, choose an appropriate package of care for their relative.
Method
We considered all elderly psychiatric in-patients discharged from Leigh Infirmary in the period between 1 October and 31 December 2005. Our initial source of information about patient admissions, discharges and transfers was the daily ward listing kept by each ward.
Once a patient was listed as ‘discharged’ on the daily ward listing, their file was retrieved and information classified according to the pro forma template. The template contained essential demographic data plus the following:
-
1. Date for the patient fit for discharge, as entered in the notes by the medical team.
-
2. Total length of in-patient stay (the number of days from date of admission to date of discharge, excluding time spent on medical wards (other than psychiatry wards) or in accident and emergency if the patient's physical health declined).
-
3. Delay incurred (the number of days elapsed from ‘patient fit for discharge’ to ‘date of discharge’).
-
4. Patient destination, namely home, Elderly Mentally Infirm (EMI) unit, nursing home, residential home or sheltered accommodation.
-
5. Cause of delay, for example carer decision resulting in delay, non-availability of residential or nursing home, patient going out of area, medical/nursing/physiotherapy/occupational therapy delay.
Results
A total of 50 patients were discharged during the study period (five became physically unwell during their stay, whereupon they were transferred to accident and emergency and passed away; they were not included in the study). There were 32 women and 18 men in this group, aged 61–97 (mean 76.3) years old.
In terms of the conditions the patients were diagnosed with, 24 (48%) had a primary diagnosis of dementia, 15 (30%) depression, 3 (6%) bipolar illness, 3 (6%) psychosis, 2 (4%) had organic problems and 5 (10%) had ‘other’ problems (persistent delusional disorder, alcohol dependence and no formal diagnosis).
The discharge destination was as follows: 24 patients were discharged to their homes, 9 went to an EMI unit (5 to nursing and 4 to residential homes), 7 into sheltered accommodation, 6 into a residential home and 4 into a nursing home.
In-patient stay and delay
The total length of in-patient stay for all patients (excluding time spent on other medical or surgical wards) varied between 4 and 326 days (mean stay was 60 days). The total length of delay varied between no delay up to 201-day delay (mean delay was 14 days; Fig. 1).
There were a number of causes for the delay in discharge: an unavailable destination placement caused a total of 229 days’ delay (affecting 12 patients); a 201-day delay happened because of patient ‘out-of-area’ (only one case); carer delay accounted for 117 days (12 patients); funding issues were the reason behind 84 days of delay (4 patients); nursing and residential home assessment and feedback resulted in 59 days’ delay (5 patients); delays in patient transfer to destination cost 9 days’ delay (2 patients); and setup of homecare cost 7 days (3 patients).
Consequences of delay
These include ‘bed-blocking’, of particular relevance in mental healthcare units as patients who are in crisis in the community may not be able to access hospital care; increased carer stress; risk of nosocomial infections (Reference Lim, Doshi and CastasusLim et al, 2006) and financial costs to the NHS.
Cost of delay
The 50 patients in the study spent a total of 2997 days on the two hospital wards being observed; the total number of delayed days arising from their stay was 706; this figure represents 23.5% of the total number of in-patient days.
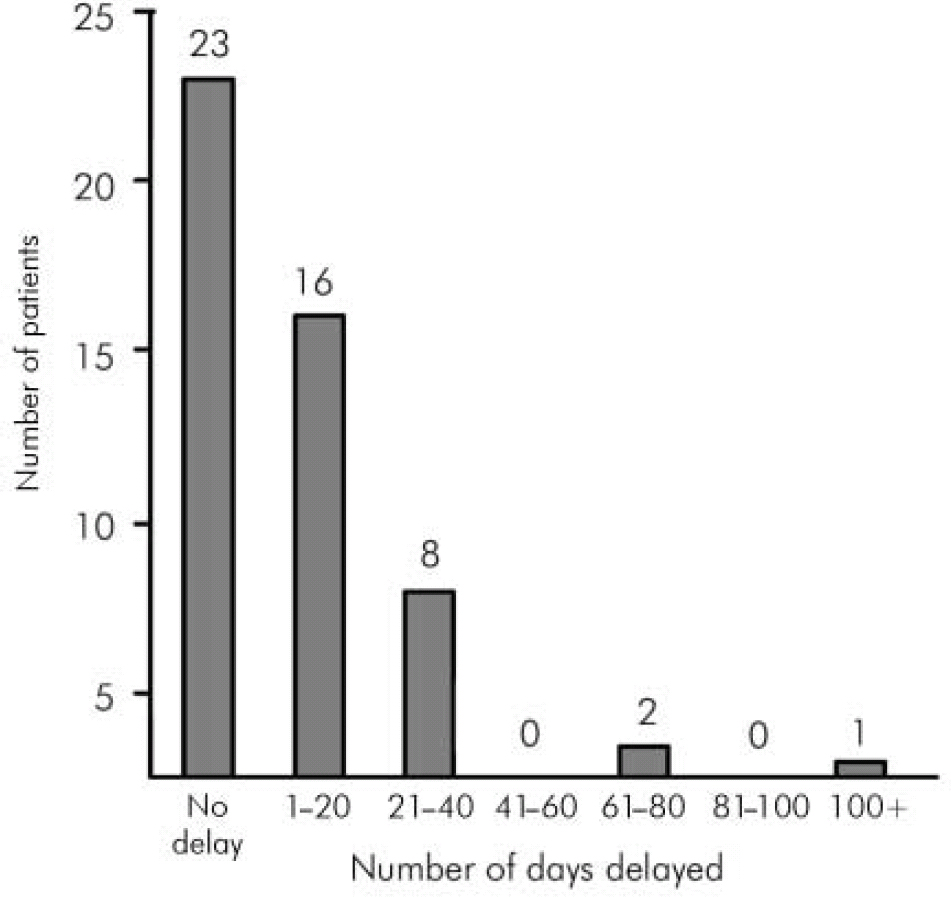
Fig. 1. Delay between ‘patient fit for discharge’ and actual discharge.
The average cost of a hospital bed in the Trust was put at £250 per day, and so for 706 delayed days this equates to a cost of delay of £176 500 for the 3-month period we collected data for. If extrapolated for 12 months, over £700 000 would be spent on unnecessarily keeping patients in hospital.
For the 50 patients, the delay cost £3530 per person over 3 months; since there were 27 patients delayed 1 day or more, this brings a cost of £6540 per delayed patient over 3 months. Of the patients experiencing delay, 19 were diagnosed with dementia, 6 with depression, 1 with bipolar affective disorder and 1 with an organic illness. If we consider how the destination of the patient affects the delay, it is clear that those awaiting EMI placements are affected most, followed by those awaiting a nursing home place (Table 1).
Table 1. Destination of patients after discharge, delay incurred and its cost
| Destination | Patients (n) | Total number of days delayed (for n patients) | Average delay per patient (days) | Cost of delay per patient (£)1 |
|---|---|---|---|---|
| EMI unit | 9 | 446 | 50 | 12 390 |
| Nursing home | 4 | 96 | 24 | 6000 |
| Sheltered accommodation | 2 | 33 | 17 | 4125 |
| Residential home | 5 | 74 | 15 | 3700 |
| Home | 7 | 57 | 8 | 2035 |
Discussion
We found that there exists a significant delay in discharging elderly psychiatric patients. In our study, 23.5% of total in-patient stay was attributed to delay; most delay was due to non-availability of placement (especially EMI and nursing homes) and carer delay. A study looking at the delays in discharging psychiatric in-patients with learning disabilities (Reference Watts, Richold and BerneyWatts et al, 2000) found that those who remained in hospital longer were the least able and most challenging – the equivalent in patients with dementia would be those awaiting EMI placements, as they often have the highest level of care needs. It must be emphasised that timely and not early discharge should be the goal as the latter may result in the elderly patient being discharged to an inappropriate placement, potentially leading to hospital readmission.
The financial cost of delay to Leigh Infirmary over 12 months was estimated at £706 000, for elderly psychiatric in-patients only.
The demand for hospital beds is immense and one measure of the efficiency of a hospital is its throughput; therefore, when a blockage occurs in the system, it has a knock-on effect at other levels of care. Delayed discharge not only exposes the patient to health risks such as infection, social isolation, increased dependency and loss of skills (Reference Lambourne, Ashaye and LambourneLambourne et al, 2005) but also affects the health and well-being of those awaiting hospital admission and their carers.
Limitations
This study was conducted at a district general hospital and as such it may not be relevant to elderly psychiatric patients in other locations. Other considerations were the relatively small number of patients (n=50) and a short time frame of the study (3 months). We assumed the entries in the daily ward listing for the date a patient was medically fit for discharge had been accurate – prior to commencement of the study, an information sheet was distributed to the teams asking to pay particular attention to accuracy. Confounding factors identified in previous studies in this area which may also delay discharge such as age, severity of illness, complex comorbid physical health problems, poor mobility and informal status (Reference Watts, Richold and BerneyWatts et al, 2000) were not taken into account in this study. It may be expected that the rate of staff turnover in social services and changes in care coordinators could have an effect on the length of in-patient stay and this would be a useful consideration for a future study.
Recommendations
Proactive discharge planning with emphasis on carer involvement should be encouraged together with the appointment of an elderly discharge coordinator to facilitate and monitor discharge.
Ways of improving inter-disciplinary communication between health and social services should be examined – our observations highlighted the importance of social worker attendance at the weekly multidisciplinary team ward reviews (the fact that social workers were based in the hospital greatly helped here); when social workers are based externally, regular updated reports from the ward (and vice versa) should be agreed upon. Assertive outreach services have been established nationwide for certain groups of adult mental healthcare users and extension to older-age clients should also be investigated. At Leigh Infirmary, a document detailing results of medical tests and investigations was completed for each patient to expedite provision of the medical report and early completion of a Part I discharge summary was widely encouraged among medical staff.
Increased care home provision is paramount if the problems of delayed discharge are to be adequately addressed (Reference Epstein, Kaplan and LaviEpstein et al, 2001); another factor for consideration here would be ‘step-down’ facilities to act as a buffer between ward and eventual placement to reduce unnecessary in-patient stay.
Bed-blocking is a result of finite resources being used inappropriately. To quote Dr Andrew Murrison, MP for Westbury, ‘It costs £1630 to have someone in hospital for a week and £319 for a week in a care home. Where is the sense in that?’ (Parliament Publications, 2002).
Declaration of interest
None.





eLetters
No eLetters have been published for this article.