The reported prevalence of psychiatric illnesses among adults with learning disabilities varies widely between 10 and 39% (Reference Deb, Thomas and BrightDeb et al, 2001). Estimated prevalence rates for specific conditions are: schizophrenia 3%, bipolar disorder 1.5%, depression 4%, obsessive–compulsive disorder 2.5%, dementia 20%, and autism 7% (Reference Cooper and BaileyCooper & Bailey, 2001). The prevalence of epilepsy in learning disability is said to be 20–30%. Challenging behaviour has a prevalence of 10–15% and is more common in men than in women. It reaches a peak by 15–34 years of age and increases in severity relative to the level of learning disability. Problem behaviour tends to be long-lasting and more than one type of behaviour is usually found (Reference SmileySmiley, 2005).
A study by Turkistani (Reference Turkistani2004) looked at the prevalence of epilepsy in learning disabilities and its association with mental illness and behavioural problems. The study found no significant association between epilepsy and behavioural disturbances or mental illness and concluded that epilepsy does not necessarily increase the incidence of mental illness and/or behavioural disturbance. Furthermore, Chung & Cassidy (Reference Chung and Cassidy2001) concluded in their study that there was no significant difference in the degree of learning disabilities between epileptic and non-epileptic groups. In a cross-sectional analysis, Tyrer et al (Reference Tyrer, McGrother and Thorp2006) found no relationship between aggression and the presence of epilepsy or autism. Similarly, Kerr (Reference Kerr2002) concluded that behavioural disturbance is independent of epilepsy or its management. On the other hand, Espie et al (Reference Espie, Watkins and Curtice2003) found that a third of people with epilepsy and intellectual disability met the criteria for possible psychiatric disorder, particularly affective/neurotic disorder; twice the comparison rates for intellectual disability alone.
The Community Learning Disabilities Team in Waltham Forest caters to a total population of about 218 000. The region has a multi-ethnic population with Afro-Caribbean groups forming at least 14%, and Asian groups forming 12.5% of the overall population (Office for National Statistics, 2003; London Borough of Waltham Forest, 2007). The main aim of the study was to ascertain the prevalence of epilepsy and the difference in morbidities between epileptic and non-epileptic individuals in contact with the learning disability service. We also postulated that there is no association between epilepsy and high prevalence of psychiatric morbidities and/or challenging behaviour in our learning disability population.
Method
At the time of the study there were 353 individuals with learning disabilities in contact with the service. A total of 177 case notes belonging to active clinical cases were included in the study. Information gathered from the case notes was collected in a pre-formatted data collection sheet, where it was placed in the following categories: gender, date of birth, ethnicity, residential status and diagnosis (including epilepsy, psychiatric diagnosis and challenging behaviour). These data were tabulated to ascertain the differences in the above parameters between epileptic and non-epileptic service users.
Results
Demographic details
The prevalence of epilepsy in the study group was 30% (Table 1). There were more men (n=95) than women (n=82) in the study; there were also more men than women in the epileptic group (30 v. 23). The 10-year age distribution across the two groups was almost equal in all age ranges, except in the 35–44 years old, and above 65 years old range. In the former, more users were non-epileptic while in the latter more were epileptic. Ethnically, White British service users were more likely to be epileptic, whereas this was not observed in the Afro-Caribbean group. In the Asian group, Pakistani service users were over-represented in both groups (67% of all Asian users in non-epileptic and 75% in epileptic group). Others included diverse groups such as mixed Italian and Spanish, Turkish, Cypriot, Portuguese, etc. There was almost no difference in the residential status of the users from the two groups.
Table 1. Demographic details (total case notes n= 177)
| Non-epileptic n (%) | Epileptic n (%) | |
|---|---|---|
| Gender | ||
| Male | 65 (52) | 30 (57) |
| Female | 59 (48) | 23 (43) |
| Age, years | ||
| 17-24 | 24 (19) | 9 (17) |
| 25-34 | 18 (14) | 8 (15) |
| 35-44 | 28 (23) | 9 (17) |
| 45-54 | 27 (22) | 10 (19) |
| 55-64 | 17 (14) | 9 (17) |
| > 65 | 10 (8) | 8 (15) |
| Ethnicity | ||
| White British | 71 (57) | 33 (63) |
| Afro-Caribbean | 20 (16) | 6 (11) |
| Asian | 12 (10) | 8 (15) |
| Other | 11 (9) | 6 (11) |
| Unspecified | 10 (8) | 0 |
| Residential status | ||
| Residential home | 56 (45) | 25 (47) |
| Supported living | 19 (15) | 7 (13) |
| Private home | 47 (38) | 20 (38) |
| Unspecified | 2 (2) | 1 (2) |
| Total | 124 (70) | 53 (30) |
Details of diagnoses
Figure 1 shows the distribution pattern of the level of learning disability between the two groups. There were more non-epileptic service users with mild learning disability (58% non-epileptic v. 40% epileptic) and almost equal number with moderate learning disability (31% and 26%) in the two groups. Users with epilepsy were nearly three times more likely to have severe learning disability than those without epilepsy (respectively 11% and 30%).
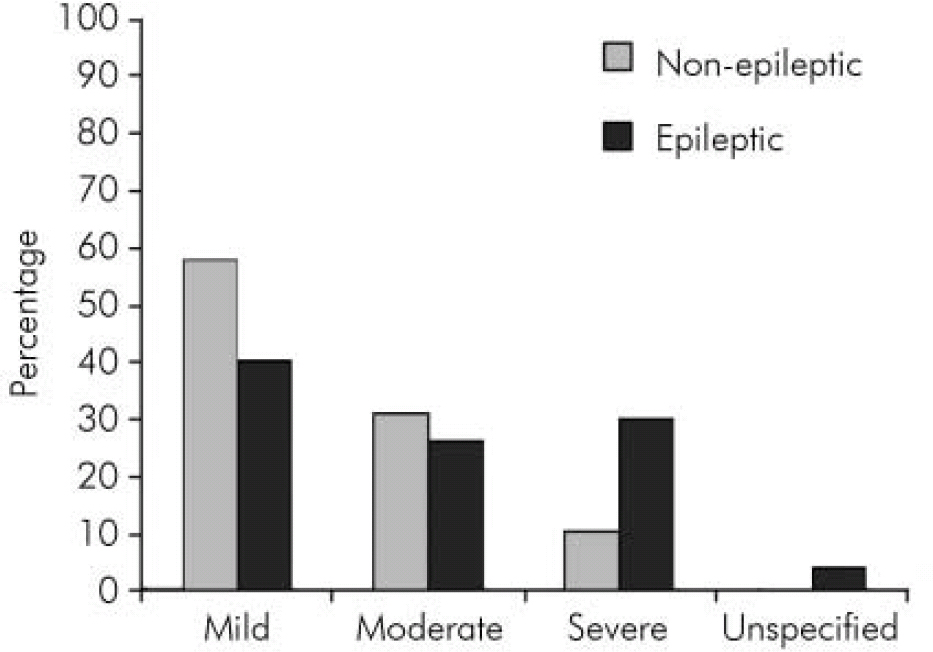
Fig. 1. Level of learning disabilities.
Figure 2 depicts the distribution of challenging behaviour between the two groups: 70% of users with any type of challenging behaviour were in the non-epileptic group, as opposed to 59% in the epileptic group. Verbal challenging behaviour, which included shouting and swearing, was more common among those without epilepsy (35%) than those with epilepsy (11%). Physical challenging behaviour, for example physical assaults, damage to property, etc., was almost equally prevalent in the two groups (35% and 34%). Sexualised behaviour, in the form of indecent exposure, unconcealed masturbation, inappropriate touching, etc., was again more common in the non-epileptic group (6% and 2%). Physical challenging behaviour was the more common type among those with epilepsy. Other types of challenging behaviour, which included self-injurious behaviour, absconding, difficulty in engaging, deliberate falls, deliberate incontinence, rituals and hoarding food, among others, were more common among users with epilepsy (17% and 30%).
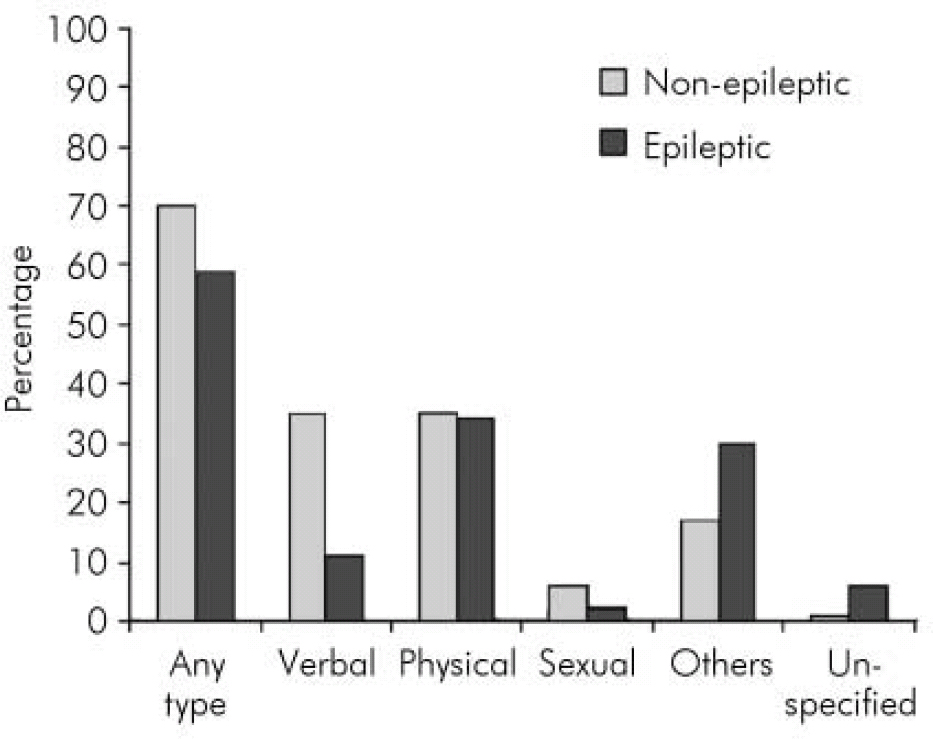
Fig. 2. Comorbid challenging behaviour.
As regards psychiatric conditions, depression was by far the most common diagnosis in both groups (Table 2), being slightly more common among people without epilepsy. Other conditions such as anxiety disorders, psychoses, schizophrenia and autistic-spectrum disorders were also prevalent among this group. There was no significant difference between the prevalence of conditions with an organic element such as dementia and Down syndrome between the two groups.
Table 2. Psychiatric comorbidity
| Common disorders | Non-epileptic group, n (%) | Epileptic group, n (%) |
|---|---|---|
| Depression | 32 (26) | 10 (19) |
| Bipolar affective disorder | 8 (6) | 0 |
| Anxiety disorders | 23 (19) | 4 (8) |
| Psychoses | 23 (19) | 1 (2) |
| Schizophrenia | 12 (10) | 2 (4) |
| Personality disorders | 6 (5) | 1 (2) |
| Autistic spectrum disorders | 13 (11) | 5 (9) |
| Dementia | 10 (8) | 4 (8) |
| Down syndrome | 8 (6) | 3 (6) |
Discussion
Even though the total number of users included in the study (n=177) was less than the actual number of service users on the practice database, we believe that all people requiring regular review of mental state and management have been included in the study. This is reflected by the high prevalence of challenging behaviour and psychiatric illnesses in both groups.
Our findings suggest that there is no increase in challenging behaviour in people with learning disability and epilepsy. This is especially true for the more ‘conventional’ types of behaviour such as verbal, physical and sexual challenging behaviours. The findings also suggest that having epilepsy does not increase the chance of developing psychiatric illnesses in people with learning disability. This is in keeping with the findings from other studies described in the published literature. This also confirms our postulation that there is no association between a high prevalence of mental and behavioural disorders with epilepsy in people with learning disability.
Declaration of interest
None.







eLetters
No eLetters have been published for this article.