Obsessive-compulsive disorder (OCD) and body dysmorphic disorder run a chronic course and have similar features. The former is characterised by intrusive, anxiety-provoking thoughts, images or impulses which are relieved temporarily by performing an anxiety-relieving compulsion (World Health Organization, 1992; American Psychiatric Association, 1994). In the latter there are also anxiety-provoking intrusive thoughts but these tend to concern an aspect of the person's appearance and lead to compulsions like checking appearance or in many cases even repeatedly seeking surgical solutions (World Health Organization, 1992; American Psychiatric Association, 1994). The National Institute for Health and Clinical Excellence (NICE) draft guidelines on the treatment of OCD (National Institute for Health and Clinical Excellence, 2006) propose a 6-stage model of stepped care, with the most severe and resistant individuals being treated using in-patient psychological and drug treatment or other intensive treatment programmes. Treatment-resistant OCD is associated with high levels of dependency on mental health services and high levels of comorbidity, with suicide reported in up to 15% of cases (Reference Angst, Gamma and EndrassAngst et al, 2005).
The behavioural cognitive psychotherapy unit in South West London and St George's Mental Health National Health Service (NHS) Trust was commissioned by the local five boroughs to provide a comprehensive service for obsessive-compulsive and body dysmorphic disorders based on the NICE guidelines. This service was to concentrate on individuals requiring highly specialised treatment, particularly those described in the NICE guidelines as level 5 severity. Those with less severe conditions would also be helped by the unit working jointly with other healthcare teams. Individuals with the most severe illness (level 6 severity) are treated under the provisions made by the Department of Health's National Commissioning Group (www.ncg.nhs.uk). Treatment is provided by a network of services and free of cost to individual commissioners in Scotland and England (in Wales and Northern Ireland it is via a named patient service agreement). The unit continues to provide in-patient (Reference Drummond, Pillay and KolbDrummond et al, 2007), community and out-patient treatment for these individuals. Although some of our staff work across both services, they operate as independent services with different funding streams and working arrangements.
The five boroughs covered by the community treatment for obsessive-compulsive and body dysmorphic disorders and severe neurotic conditions have a combined population of approximately 1 million adults. They comprise Kingston, Merton, Richmond, Sutton and Wandsworth. The Trust has several hospitals and numerous community bases throughout the boroughs. Demographically, the population and area served varies from deprived inner city areas to affluent suburbs in the commuter belt. Similarly the population varies from a very high mix of Black and minority ethnic population in areas such as Tooting in Wandsworth and a more predominantly White population in areas such as Hampton Wick in Richmond. It has been estimated that in general approximately 1-2% of the population have clinically relevant obsessive-compulsive/body dysmorphic disorders (Reference Karno, Golding and SorensonKarno et al, 1988), which would potentially mean between 10 000 and 20 000 adults in our area.
The healthcare commissioners envisaged a service based in the community. To this end we devised a ‘hub and spoke’ model and would provide one whole time equivalent (WTE) therapist per borough, 0.2 WTE consultant psychiatrist and 0.5 administrator. Clearly a small service such as the behavioural cognitive psychotherapy unit cannot treat all adults with obsessive-compulsive/body dysmorphic disorders in all the five boroughs. Therefore the service would concentrate on individuals with the most severe illness, also providing input in terms of raising public awareness and education, and working with colleagues in primary care and the community mental health services to deliver evidence-based best practice treatment. This model has been described on the NICE shared learning website (www.nice.org.uk/page.aspx?o=391017).
Method
Setting up the service
Staff were recruited from 1 April 2006 but not all were in post until 17 January 2007. Some staff were already working in other areas of the behavioural cognitive psychotherapy unit and just needed their working hours rebranded, but there were some considerable problems in recruiting therapists with the necessary qualifications and experience. Also, the provision of appropriate interviewing rooms for therapy sessions in the community was sometimes problematic.
Medical and administrative staff were in post on 1 April 2006. Overall, over the year this equates to 3.6 WTE in post (including medical staff). We assumed that as staff work a 37.5-h week and a 42-week year (allowing for annual, sick and study leave), a total of 5670 working hours were worked April 2006 to April 2007 in the unit.
Operationalisation of the NICE guidelines
NICE guidelines discuss obsessive-compulsive and body dysmorphic disorders at 6 levels of intervention and treatment. It is implied, but not defined, that these stages correlate to severity as well as chronicity of condition and resistance to treatment. We have operationalised the guidelines for the purposes of reporting on activity, using the Yale-Brown Obsessive Compulsive Scale (YBOCS; Reference Goodman, Price and RasmussenGoodman et al, 1989), an internationally recognised scale for measuring the severity of obsessive-compulsive and body dysmorphic disorders (maximum score 40, 0-8 mild handicap due to obsessive-compulsive/body dysmorphic disorders, 8-16 moderate, 16-24 considerable, 24-32 severe and 32-40 profound handicap). We used the operationalised definitions as follows (please note that these are a rough guide only and some individuals may require more intensive treatment owing to comorbidity):
Level 1
-
• Individual recognising that he/she has a problem and starting to seek help.
-
• YBOCS score normally less than 16.
-
• Life only minimally impaired, person likely to still be working.
Level 2
-
• Probably still in work, YBOCS approximately 16.
-
• Suitable for self-help, cognitive-behavioural therapy (CBT) with or without treatment with selective serotonin reuptake inhibitors (SSRIs).
Level 3
-
• May still be able to work, but is having problematic symptoms, YBOCS 16-24.
-
• Suitable for self-help, CBT with or without SSRIs.
-
• Referral to psychotherapy in primary care team if necessary.
Level 4
-
• Considerable symptoms, YBOCS 16-24, less likely to be working.
-
• Referred to community mental health team.
-
• Trial of alternative SSRI with or without augmentation with other agent.
-
• Trial of CBT by member of the community mental health team.
Level 5
-
• YBOCS approximately 24-32, unlikely to be working due to disability.
-
• Has already unsuccessfully received CBT from community mental health and/or psychotherapy in primary care teams.
-
• Needs either clinic-based CBT or more likely intensive home-based treatment from a unit specialising in obsessive-compulsive/body dysmorphic disorders.
-
• Has received/is receiving SSRI and augmentation with either dopamine blocker or supranormal SSRI dosage etc. as described by Pallanti et al (Reference Pallanti, Hollander and Bienstock2002).
Level 6
(This is the level at which a person enters the national network of services funded by the National Commissioning Group of the Department of Health.)
-
• YBOCS score more than 30, unlikely to be working because of disability.
-
• Two previous trials of two different SSRIs at British National Formulary recommended dosages for a minimum of 3 months.
-
• Trial of psychopharmacological augmentation of SSRI with either dopamine blocker or supranormal SSRI dosage, etc.
-
• Two previous trials of CBT (including exposure and response prevention) with at least one being carried out in the environment where the symptoms are maximal, for example intensive community and home-based treatment. The latter would normally be expected to be carried out by an individual/service specialising in CBT for obsessive-compulsive/body dysmorphic disorders.
The behavioural cognitive psychotherapy unit community service was devised particularly to have an input at level 5 of the NICE guidelines and also offer help and advice in levels 1-4. Individuals with the most severe illness are referred to the national services for obsessive-compulsive/body dysmorphic disorders (Reference Drummond, Pillay and KolbDrummond et al, 2007).
Results
Activity levels are given in Table 1.
Table 1. Activity levels
| NICE level | Examples of activity (number of hours) | Approximate number of hours dedicated to this activity in 2006/2007 | Percentage of total available hours |
|---|---|---|---|
| Level 1. Public awareness | Production and administration of talk for schoolchildren about obsessive–compulsive/body dysmorphic disorders (10) | 48 | 0.8% |
| Production of leaflet about the disorders (30) | |||
| Production of information packs for Black and minority ethnic groups (8) | |||
| Level 2. Awareness in general practice | Production of information packs for general practitioners (20) | 40 | 0.7% |
| Level 3. Treatment in general practice | Liaison with psychotherapy in primary care team if necessary (71) | 71 | 1.2% |
| Level 4. Treatment in specialist community mental health teams | Provision of certificate in cognitive-based therapy to community mental health team members (32) | 471 | 8.3% |
| Clinical supervision with members of community mental health team (279) | |||
| Joint working with community mental health team (40) | |||
| Peer supervision and paperwork for this (120) | |||
| Level 5. Treatment in specialist teams with expertise in obsessive–compulsive/body dysmorphic disorders | Direct clinical care (2123) | 3185 | 56.1% |
| Paperwork, supervision and telephone calls (1061) | |||
| Level 6. Intensive programmes and in-patient services – provided nationally | One individual has been admitted onto national service during April 2006–April 2007 and two were referred and awaiting admission. This required 10 h of liaison and report preparation in total | 10 | 0.2% |
| Assessments | Referral meetings (147) | 492 | 8.7% |
| This is for all individuals both accepted and rejected with levels 1–6 coming through community service and those with other resistant severe neurotic disorders | Assessment (141) | ||
| Peer discussion and supervision re-assessments (110) | |||
| Paperwork and liaison re-assessments (94) | |||
| Treatment of individuals with severe neurotic disorders (other than obsessive–compulsive/body dysmorphic disorders) | 50 | 0.9% | |
| Mandatory training courses, continued professional development and individual supervision of therapists | 534 | 9.4% | |
| Travel to patients, between sites, etc. | 734 | 12.9% | |
| TOTAL | 5635 | 98.5% |
Clinical outcome for level 5 individuals treated by the enhanced community service
There were 108 individuals referred over the first year. Many were issued advice or offered joint working and supervision of other healthcare professionals, and 68 have been referred and found suitable for treatment by specialist staff over the past year. These low figures reflect time spent in setting up the team, recruitment and informing potential referrers of the new resource.
Of these 68 individuals, 57 had OCD, 5 body dysmorphic disorder, 3 post-traumatic stress disorder and 3 other refractory anxiety disorders. Because there was a relatively low number of individuals with body dysmorphic disorder referred that year, the analyses were performed on those with OCD: 28 men and 29 women, average age 39 years old (s.d.=11, range 19-73). The mean duration of the clinical problem was 19 years (s.d.=12, range 2-50). The mean Beck Depression Inventory (BDI; Beck et al, 1978) score for all individuals was 25 at the start of treatment (s.d.=12, range 2-45) indicating moderate to severe depression. The average YBOCS score was 28 at the start of treatment (s.d.=6, range 13-40) indicating severe OCD (Reference Goodman, Price and RasmussenGoodman et al, 1989). Many individuals with OCD had comorbid diagnoses: 31 clinical depression, 29 other anxiety disorders, 6 drug or alcohol misuse, 2 secondary body dysmorphic disorder, 1 eating disorder and 1 post-traumatic stress disorder.
Individuals were offered a course of treatment comprising CBT with the emphasis on prolonged graded exposure in real life with self-imposed response prevention. Medication was also reviewed which resulted in one person receiving a new prescription for an SSRI and two receiving dopamine-blocking agents as augmentation for the ones they were already receiving. This low rate of change in prescribed medication reflects the working of the team where it is expected that individuals should normally have received a trial of appropriate drug treatment prior to referral.
All the individuals on an intention-to-treat paradigm showed a clinically and statistically significant reduction in OCD symptoms after 24 weeks of CBT comprising graded exposure and self-imposed response prevention. The mean YBOCS score dropped from 28 (severe disorder) to 19 (considerable disorder). Fifteen individuals (26%) dropped out within the first 12 weeks of therapy. The depression scores are also given on an intention-to-treat analysis but only 55 recorded an initial BDI score. Results are given in Table 2 and Figs 1 and 2. The improvement for each service user on the YBOCS score (and intention to treat) at 24 weeks is shown in Fig. 2.
Table 2. Patient severity scores before treatment and after 12 and 24 weeks of treatment
| Measures | Start of treatment mean (s.d., range) | After 12 weeks Mean (s.d., range) | After 24 weeks Mean (s.d., range) |
|---|---|---|---|
| YBOCS (n=57) | 28 (6, 13–40) | 21 (7, 4–35) | 19 (8, 2–35)* |
| BDI (n=55) | 25 (12, 0–45) | 20 (12, 0–48) | 19 (11, 0–48)* |
Discussion
With the current emphasis on local services, there is a tendency to assume that local generic community mental health services can provide optimal treatment for individuals with a variety of conditions and a range of severity. All the individuals presented in this study were severely disabled by their illness. They had received appropriate treatment in their local areas but had failed to improve significantly. However, they responded to treatment from a unit with special interest and expertise in OCD.
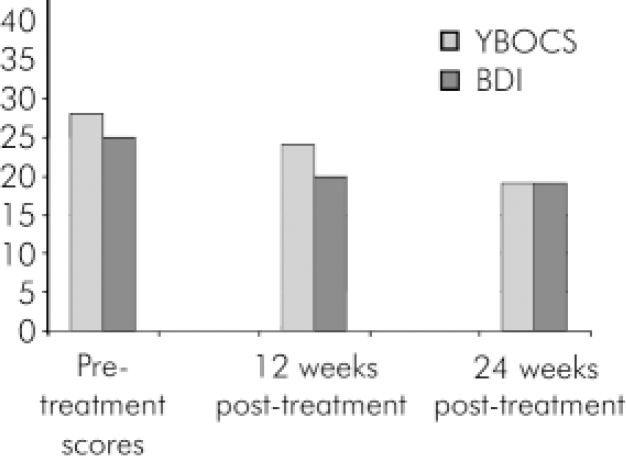
Fig. 1. Patient severity scores before treatment and after 12 and 24 weeks of treatment. YBOCS, Yale–Brown Obsessive Compulsive Score (maximum 40); BDI, Beck Depression Inventory (>20 is severe depression).
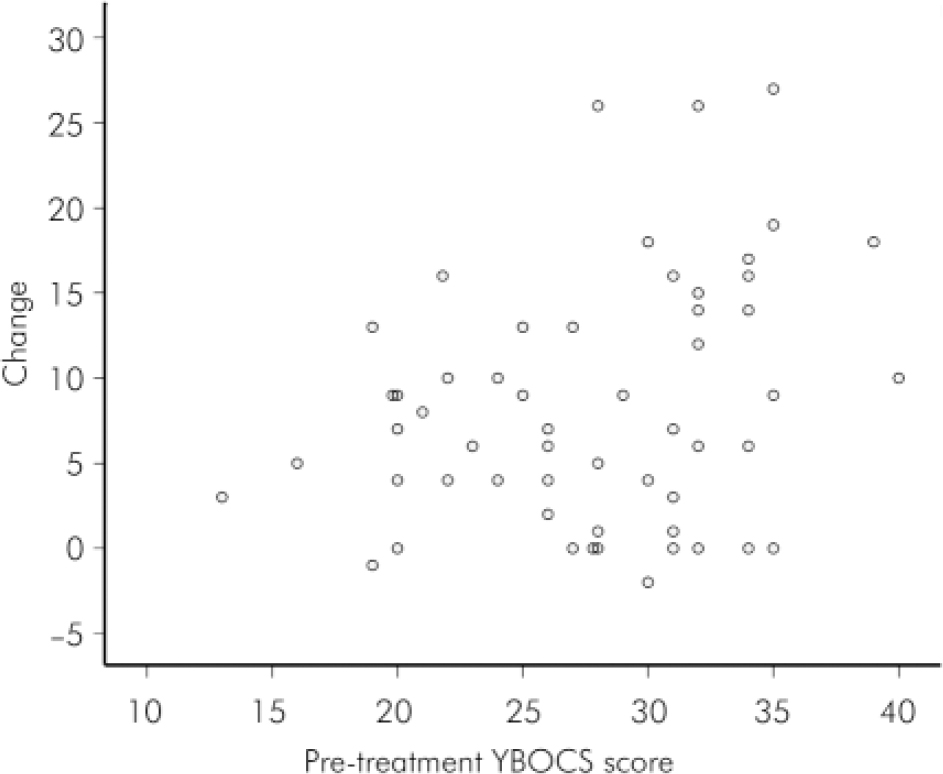
Fig. 2. Individual improvement against initial Yale–Brown Obsessive Compulsive Scale (YBOCS) score. Pre-treatment YBOCS minus YBOCS at 24 weeks; 0=no change or drop-out, negative score indicates worsening of symptoms. Two individuals each scored 28.0; 22.10 and 20.9 respectively and are not fully shown on the graph.
This model of delivery of care which is rooted in the stepped care model of the NICE guidelines may be applicable to other conditions such as eating or personality disorders. The specialist team directly treats individuals with the most severe illness but also has an input with those less ill via other healthcare workers.
One of the disadvantages of this model of delivery of care is that therapists have to ensure they do not directly take on all individuals with obsessive-compulsive/body dysmorphic disorders for treatment. In order to prevent this we have devised clear guidelines about who is directly treated by the team. This can lead to resentment from our colleagues in the community mental health teams or primary care who may feel we are being over-restrictive and not appreciating their workload and wish for us to treat all individuals with obsessive-compulsive/body dysmorphic disorders. If we were to do that, however, we would not only deskill our colleagues but also would soon be overwhelmed with clinical work.
By operationalising the NICE guidelines and offering support at various stages of treatment while concentrating on those with the most severe illness, we believe we are an extremely cost-efficient service. We suggest that each healthcare region could benefit from developing similar specialist community treatment centres for individuals with obsessive-compulsive/body dysmorphic disorders.
Declaration of interest
None. All authors work in the service described.







eLetters
No eLetters have been published for this article.