Hyperactivity is the most common neuropsychiatric disorder of childhood, with prevalence rates for the broader syndrome - attention-deficit hyperactivity disorder (ADHD) - of between 2 and 18% (Reference Rowland, Lesesne and AbramowitzRowland et al, 2002) and around 1% for the narrower syndrome of hyperkinesis (Reference Meltzer, Gatward and GoodmanMeltzer et al, 2003). Effective treatments are available, but routine community treatment of the disorder is less effective than similar treatments delivered in research protocols (MTA Cooperative Group, 1999). Although there could be several reasons for this, one possibility that has not received attention is that community services might struggle to detect persistent hyperactivity symptoms. It is known that hyperactivity symptoms may be underestimated without the use of screening questionnaires at initial assessment (Reference Foreman, Foreman and PrendergastForeman et al, 2001), judgements of symptom severity may not relate to diagnostic criteria (Reference Evink, Crouse and ElliottEvink et al, 2000) and prescription of stimulants may be better predicted by oppositional/defiant behaviour than hyperactivity itself (Reference Angold, Erkanli and EggerAngold et al, 2000). Current guidelines recommend using multiple informants and standardised measures for diagnosis (National Institute for Clinical Excellence, 2000) but there are no recommendations for follow-up assessments, which typically involve a single clinician interviewing the parent and assessing the child in clinic. We therefore compared clinical judgements of continuing hyperactivity with a standardised parental questionnaire on a sample of hyperkinetic children attending a routine community stimulant follow-up clinic. We wished to see whether the clinical use of a standardised measure would be a helpful addition to the routine assessments clinicians already made in follow-up clinics.
Method
Design, service and sample
The study was designed to audit follow-up assessments of children with a diagnosis of hyperactivity attending a secondary care child and adolescent mental health service (CAMHS), serving a population of approximately 90 000, who were prescribed methylphenidate in either conventional or slow-release forms. Questionnaire and routine clinic assessment of continuing hyperactivity were compared. The service diagnosed ICD–10 hyperkinesis (World Health Organization, 1992), rather than ADHD (Reference Taylor, Sergeant and DoepfnerTaylor et al, 1998) and was provided by two psychiatrists (D.M.F. and R.K.). The audit standards set were that no child reviewed should have significant hyperactivity on either clinic report or the Strengths and Difficulties Questionnaire (SDQ; Reference GoodmanGoodman, 1999), and there should be no difference between patients of the two psychiatrists. Follow-up assessment was based largely on interview and examination of the parents and child at clinic attendance, with the parents being treated as the main informants about all unobserved aspects of the child’s life. School and other reports or questionnaires were sought only if the clinic assessment or parental accounts were unclear. Figure 1 summarises the exclusion criteria and study attrition.
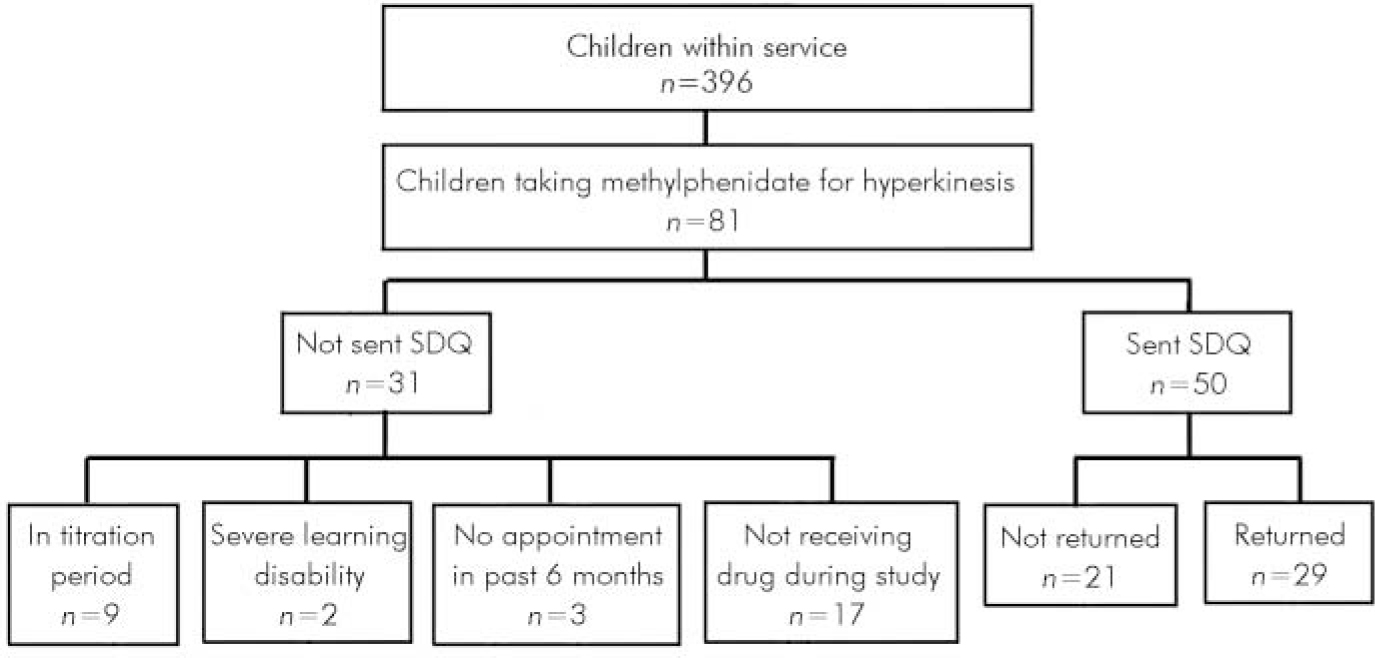
Fig. 1. Selection criteria and attrition path. Questionnaires were sent by post with one follow-up telephone call. SDQ, Strengths and Difficulties Questionnaire.
Measures
Parents were sent the extended version of the parental SDQ (Reference GoodmanGoodman, 1999), which is now freely available in several languages (http:/www.sdqinfo.com). We used the UK version for 4- to 16-year-olds, which covered the clinic’s typical age-range. This is a brief screening questionnaire of 25 symptom and 8 impact questions with check-box responses, which provides scale measures for general caseness (total difficulty score), prosocial behaviour, peer relationships, hyperactivity, conduct and emotional problems. Diagnostic algorithms combine symptom and impact scores to provide population-based cut-offs for predictions of three broad diagnostic categories: conduct–oppositional disorder; anxiety–depressive disorder; and hyperactivity–inattention disorder (Reference Goodman, Renfrew and MullickGoodman et al, 2000). These predictions are rated as ‘unlikely’, ‘possible’ (the top 10-20% of the population) or ‘probable’ (the top 10% of the population) for each diagnosis (Reference GoodmanGoodman, 2001).
The routine clinical assessment was always summarised in a letter to the referrer that included physical status (weight, height and body mass index), psychiatric symptoms, recommended medication dosage or changes, and change in any psychosocial treatment offered. The letters closest in time prior to (and thus independent of) the SDQ were coded by D.F., who was unaware of the SDQ scores, into hyperactive symptoms being ‘unlikely’, ‘ possible’ or ‘probable’, thus generating an ordered category set equivalent to that of the SDQ but reflecting clinical opinion. Mention of overactivity, impulsivity and inattention in the letter was coded as ‘probable’; at least one of these symptoms as ‘ possible’; and no mention of any hyperactive symptom was coded as ‘ unlikely’. Other information abstracted from the case records is shown in Table 1.
Table 1. Sample characteristics
| Mean (s.d.) | n (%) | |
|---|---|---|
| Age, years | 11 (2.5) | |
| Gender | ||
| Male | 27 (93.1) | |
| Female | 2 (6.9) | |
| Adversity indicators | ||
| Statement of special | 9 (31) | |
| educational needs | ||
| Social services involvement | 6 (20.1) | |
| History of parental | 20 (69) | |
| mental health issues | ||
| Non-nuclear family | 9 (31) | |
| Number of adversity indicators | ||
| 0 | 6 (20.7) | |
| 1 | 10 (34.5) | |
| 2 | 6 (20.7) | |
| 3 | 6 (20.7) | |
| 4 | 1 (3.4) | |
| Jarman Underprivileged | -0.24 (6.38) | |
| Area Score | ||
| Time since stimulant | 38.7 (21.6) | |
| began, months | ||
| Standardised stimulant | 0.67 (0.35) | |
| dose, mg/kg | ||
| Non-drug treatments | ||
| Clinic | ||
| Family therapy | 8 (27.6) | |
| Behaviour modification | 8 (27.6) | |
| Self-instructional training | 2 (6.9) | |
| Educational or other | ||
| Educational psychology | 2 (6.9) | |
| School behaviour support | 5 (17.2) | |
| team | ||
| Youth offences team | 2 (6.9) | |
| Number of non-drug treatments | ||
| 0 | 9 (31) | |
| 1 | 13 (44.8) | |
| 2 | 7 (24.1) | |
| Comorbidity (from case notes) | ||
| Conduct/oppositional defiant | 14 (48.3) | |
| Tourette syndrome | 1 (3.4) | |
| Asperger syndrome | 5 (17.2) | |
| Anxiety disorder | 1 (3.4) | |
| Specific learning difficulties | 7 (24.1) | |
| Number of psychiatric diagnoses | ||
| 1 | 7 (24.1) | |
| 2 | 17 (58.6) | |
| 3 | 4 (13.8) | |
| 4 | 1 (3.4) |
Analysis
Owing to the small size of the data-set, tabulation and visual displays were used to display important relationships, with non-parametric tests for hypothesis testing.
Results
The questionnaire was sent to 50 families but returned by only 29 (58%); the response probably reflects data collection having to be undertaken during the school summer holidays, which also prevented the concurrent use of the teachers’ version of the SDQ. No difference was found between returners and non-returners on clinic estimate of hyperactivity (Jonckheere–Terpstra test 172, P=0.23).
The sample characteristics are summarised in Table 1; 15 of the children (52%) were seen by D.F., 14 (48%) by R.K. There was no difference between the children for either the clinical (Mann–Whitney U=79, P=0.27) or the SDQ (Mann–Whitney U=86.5, P=0.43) estimates of the probability of the children still being significantly hyperactive. So, this audit standard was met.
The audit standard that no child should have significant continuing hyperactivity was not met using either criterion, and the overall agreement between them, although significant, was poor (Table 2): 25 (86%) children were symptomatic by the SDQ, 13 (45%) by clinical opinion. No other variable predicted the clinicians’ estimate of symptoms. No child had their medication or psychosocial treatment changed at the clinic appointment referred to in the letter.
Table 2. Association between questionnaire and clinic assessments of continuing hyperactivity1

| Clinical assessment of likelihood of continuing hyperactivity, n (%) | |||
|---|---|---|---|
| Unlikely | Possible | Probable | |
| Questionnaire assessment of likelihood of continuing hyperactivity, n | |||
| Unlikely | 3 (10.3) | 1 (3.4) | 0 (0) |
| Possible | 12 (41.4) | 7 (24.1) | 1 (3.4) |
| Probable | 1 (3.4) | 2 (6.9) | 2 (6.9) |
Fifteen children (52%) had a maximum score on the SDQ hyperactivity sub-scale. Although numerical analysis suggested an overall association between the SDQ measure of impairment–impact and this sub-scale (Spearman’s rho=0.436, P=0.009), Fig. 2 shows that this relationship broke down at higher hyperactivity sub-scale scores, as did the relationship between the hyperactivity sub-scale, the SDQ total difficulty score and clinical opinion.
Discussion
A substantial proportion of young people attending an ordinary hyperactivity medication follow-up clinic have continuing problems with hyperactivity, despite having been in treatment for, on average, more than 3 years. The SDQ detected more hyperactive symptoms than the clinic letters indicated. However, high SDQ scores for hyperactive symptoms had little association with SDQ estimates of total difficulty or impairment. So, although parental SDQ can demonstrate imperfections in the detection of hyperactive symptoms in ordinary clinic assessment, its routine adjunctive use could further confuse, rather than improve, assessment at follow-up, as the differing scores do not afford a simple interpretation. Although a range of physical and psychological treatments are used (Table 1) no child’s treatment was changed, despite continuing hyperactive symptoms being identified clinically in nearly half. Clinicians may be considering the risk of side-effects, or they may be benchmarking current symptoms and impairment against greater past difficulty, neither of which this study measured.
The chief limitations of the study are the small sample size, the risk of selection bias, and the children being from a single, secondary care psychiatric clinic. Despite all this, including the inevitable confounding of general with local characteristics of staff and patients, the sample characteristics, symptoms and treatment profiles are typical of hyperactive children seen and treated in secondary care (Reference Coffey, Kernberg and BemporadCoffey, 1997; Reference Swanson, Kraemer and HinshawSwanson et al, 2001). The study did not include children with non-hyperkinetic ADHD or children managed in primary care alone. It is likely that hyperactivity will be harder to detect in the broader syndrome of ADHD, and that more general services will have less skill and experience than dedicated secondary care provision, so the difficulties identified here may be more apparent in settings using the broader diagnosis and fewer specialist staff. The study did not separately consider other factors affecting treatment decisions, such as perceived risks of side-effects, parental preferences over drug dosage or current availability of psychological treatments, so it cannot be inferred that the clinicians’ decisions not to modify treatment in the presence of hyperactive symptoms are irrational.
As was suspected, even alert clinicians do struggle to detect continuing hyperactivity in follow-up clinics. The SDQ results suggest that simply adding a questionnaire to be completed by parents at follow-up will identify more symptoms, but its clinical significance will be uncertain. Given the small sample size and the single centre of the present study, larger confirmatory studies in multiple centres are needed. It seems unlikely that another questionnaire would have produced different results: most questionnaires seem similar in their abilities to detect hyperactivity (Reference Collett, Ohan and MyersCollett et al, 2003), and there seems little to choose between more general and more specific questionnaires (Reference Foreman, Foreman and PrendergastForeman et al 2001). It might seem prudent to ensure that follow-up assessment includes additional data to those provided by the parents and clinic observation (e.g. first-hand reports or observations from the school). However, following such recommendations would require limiting follow-up clinics to the school terms, and making prior arrangements to obtain school-based reports or questionnaires. Both these changes would present considerable logistical problems and might not change clinicians’ behaviour, as even the clinical identification of continuing hyperactive symptoms does not necessarily lead to a change in treatment. Further research is needed to clarify the factors influencing clinicians’ treatment decisions: for example, clinical detection of side-effects and impairment was not assessed in this study. Structured treatment protocols that limit clinical judgement, as used in research trials, might produce better outcomes. This goes beyond current clinical guidelines (American Academy of Pediatrics, 2001; National Institute for Clinical Excellence, 2000) but is consistent with research. However, it would need testing by appropriate studies.
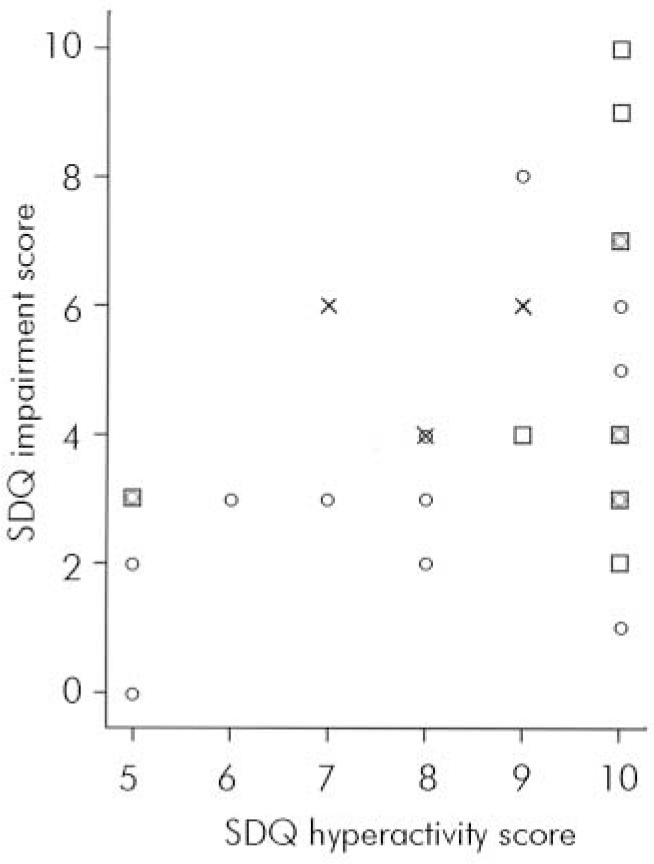
Fig. 2. Hyperactivity v. impairment scores on the Strengths and Difficulties Questionnaire (SDQ). Clinical opinion of presence of continuing hyperactivity: ○, unlikely; □, possible; X, probable.







eLetters
No eLetters have been published for this article.