A significant link between vitamin D and CVD risk has been suggested, with strong associations being found between poor vitamin D status and CVD risk factors such as dyslipidaemia and hypertension. The aim of this subsidiary study was to further investigate the association between summer vitamin D status (25 hydroxyvitamin D 25OHD) and CVD risk factors, as defined by serum lipid profiles and insulin levels with specific 25OHD cut-off values(Reference Hakim1).
The D-FINES study (Vitamin D, Food Intake, Nutrition and Exposure to Sunlight in Southern England) was a longitudinal study that investigated the interaction between diet and sunlight exposure on 25OHD status. A total of 279 Caucasian (C) and 94 Asian (A) women aged 19–70 years living in Southern England participated in the study, providing fasted blood samples for the assessment of 25OHD) and lipid profile. The Table below compares lipid levels between vitamin D status groups, defined according to differing levels of 25OHD cut-offs.
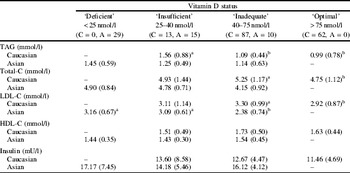
Cells within a row with different superscript letters are significantly different. ANOVA, P<0.05. Mean (sd) given.
Differences in plasma lipids between vitamin D sub-groups were more pronounced in ‘C’ than ‘A’ women. ‘C’ women with optimal vitamin D status had lower TAG, total and LDL cholesterol than groups of insufficient or inadequate status. In ‘A’ women, only LDL cholesterol was significantly negatively associated with vitamin D level. All results remained significant after adjusted for BMI, except for TAG among ‘C’ women. The lack of an association between 25 OHD status and CVD markers in Asian women may be reflective of the almost complete 25 OHD ‘deficiency’ in this entire group. These data provide new evidence for significant associations between poor 25 OHD status and markers of CVD risk, especially in Caucasian women.
The D-FINES Study was funded by the Food Standards Agency (Project No. NO5064). O. A. Hakim is grateful to the Royal Embassy of Saudi Arabia for PhD funding.


