Vegetarians are defined as people who do not eat any meat, poultry or fish. They may be sub-classified as lacto-ovo-vegetarians who eat dairy products and/or eggs and vegans who do not eat any animal products.
The prevalence of vegetarianism (the practice of following a vegetarian diet) varies widely around the globe. India has the highest proportion of vegetarians of any country with about 30 % of the population following a vegetarian diet( Reference Agrawal, Millett and Dhillon 1 , Reference Shridhar, Dhillon and Bowen 2 ). Elsewhere, vegetarianism is considerably less common, with less than 10 % of the population following a vegetarian diet( 3 ). For example, it has been estimated that vegetarians and vegans represent 5 and 2 %, respectively, of the US population( Reference Le and Sabaté 4 ). These figures indicate that vegetarians represent a sizeable minority of the global population, and with calls for a worldwide reduction in consumption of animal products( Reference McMichael, Powles and Butler 5 ), their long-term health is a matter of considerable interest.
Many studies have assessed the nutritional adequacy of vegetarian diets. Overall, these have shown that a well-planned vegetarian or vegan diet can supply all the nutrients required for good health( Reference Craig and Mangels 6 ). However, some concern remains over the possibility of low intakes of some nutrients such as vitamin B12, vitamin D, calcium and n-3 fatty acids in poorly selected and/or unfortified vegetarian or vegan diets( Reference Pawlak, Lester and Babatunde 7 , Reference Tucker 8 ); in particular, vitamin B12 status has been widely observed to be relatively low in vegetarians and especially in vegans, and this is associated with relatively high plasma homocysteine( Reference Obersby, Chappell and Dunnett 9 ).
Many studies have assessed health-related factors such as BMI, plasma cholesterol concentrations and blood pressure in vegetarians, but relatively few studies have been of sufficient magnitude and duration to examine the long-term health of vegetarians and vegans. In this overview, we concentrate our attention on the findings of prospective cohort studies with a high proportion of vegetarian participants, extending and updating those described in a previous review by the authors( Reference Key, Appleby and Rosell 10 ). The present paper is based on the material presented at a conference and is not a full systematic review of the topic. A further caveat is that, because vegetarian diets are defined by the foods that they exclude, the foods included in vegetarian diets can vary substantially and therefore the associations observed may differ between studies; in particular, all the prospective studies we discuss were conducted in western countries, therefore the conclusions in this review may not apply to vegetarians in non-western countries.
Prospective studies of vegetarians
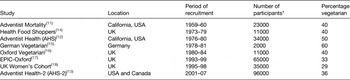
Table 1 summarises eight prospective studies with a high percentage of vegetarian participants (at least 29 % each), the results from which will form the basis of this review. The studies include a total of nearly 280 000 participants, including over 100 000 vegetarians (although there is slight overlap between some of the studies conducted within the same country). Most of the studies were designed with the aim of recruiting a high proportion of vegetarian participants, along with non-vegetarians drawn from the same population. For example, the three North American studies are drawn from members of the Seventh-day Adventist Church, a Christian denomination with a high proportion of vegetarian adherents( Reference Snowdon 11 – Reference Butler, Fraser and Beeson 13 ). In contrast, the five European studies were all drawn from free-living populations, although recruitment was deliberately targeted at vegetarians and the health-conscious, with the assistance of vegetarian organisations and health-related publications and establishments( Reference Burr and Sweetnam 14 – Reference Cade, Burley and Greenwood 18 ). In all these studies the non-vegetarians were recruited with the aim of providing a reasonable comparison group, in that they were drawn from the same population and had a similar socio-economic status to that of the vegetarians, thus reducing the likelihood that any health differences observed would be due to non-dietary rather than dietary factors.
Table 1. Prospective studies with a high percentage of vegetarian participants
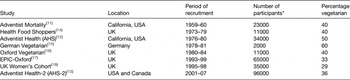
EPIC, European Prospective Investigation into Cancer and Nutrition.
* To nearest 1000.
Obesity and weight gain
More than one billion adults worldwide are overweight and at least 300 million of these are obese( Reference Smyth and Heron 19 ). Studies of western vegetarians have consistently shown that vegetarians have a lower BMI than otherwise comparable non-vegetarians, with differences typically in the region of 1–2 kg/m2 across all adult age groups, vegans generally having the lowest BMI( Reference Davey, Spencer and Appleby 17 , Reference Key, Fraser and Thorogood 20 , Reference Tonstad, Butler and Yan 21 ). These differences are reflected in a lower prevalence of obesity among western vegetarians( Reference Key and Davey 22 , Reference Newby, Tucker and Wolk 23 ), and lower weight gain in vegetarians and vegans during adulthood( Reference Rosell, Appleby and Spencer 24 , Reference Japas, Knutsen and Dehom 25 ). Obesity is a major cause of morbidity/mortality, so these findings might be expected to result in a reduced risk of obesity-related diseases and conditions in vegetarians. Some studies have also suggested a role for vegetarian and vegan diets in weight management( Reference Turner-McGrievy, Barnard and Scialli 26 – Reference Mishra, Xu and Agarwal 28 ). The consistent findings of low BMI in western vegetarians may not apply in non-western populations; for example there was no difference in mean BMI between vegetarians and non-vegetarians in the Indian Migration Study of 7000 participants, 33 % of whom were vegetarians( Reference Agrawal, Millett and Dhillon 1 ).
Diabetes
The risk of type 2 diabetes is very strongly linked to obesity. Diabetes rates have now reached epidemic proportions according to the WHO, mirroring the rapid rise in the prevalence of obesity worldwide( Reference Smyth and Heron 19 ). It would be expected that, due to their relatively low BMI, western vegetarians would have a lower risk of diabetes than comparable non-vegetarians. Using data from the Adventist Health Study-2 (AHS-2) cohort, Tonstad and colleagues showed a lower risk of self-reported diabetes in semi-vegetarians, lacto-ovo-vegetarians and vegans compared with non-vegetarians, risks in the vegetarian groups being approximately half those of the non-vegetarians overall, after adjusting for BMI( Reference Tonstad, Stewart and Oda 29 ). These findings have led some authors to propose a role for vegetarian and vegan diets in the management of type 2 diabetes( Reference Barnard, Katcher and Jenkins 30 ), but more research is needed, ideally with diabetes cases identified through medical records, and further examination of whether the possible lower risk of diabetes in vegetarians is entirely due to their lower BMI. More data are also needed from non-western populations: in a cross-sectional study of Taiwanese Buddhists, Chiu and colleagues found the prevalence of diabetes in vegetarians to be lower than those of non-vegetarians( Reference Chiu, Huang and Chiu 31 ), whereas in the Indian Migration Study there was no difference in the prevalence of diabetes between vegetarians and non-vegetarians( Reference Shridhar, Dhillon and Bowen 32 ).
Cardiovascular disease
Risk factors: plasma cholesterol, hypertension and blood pressure
Plasma total cholesterol is lower in vegetarians than in non-vegetarians, primarily due to a reduction in LDL cholesterol, with little difference in HDL cholesterol( Reference Thorogood, Carter and Benfield 33 , Reference Bradbury, Crowe and Appleby 34 ). This difference in plasma cholesterol is likely to be large due to differences in fat intake, since meat is a rich source of SFA whereas some plant foods such as vegetable oils, nuts and seeds are rich sources of PUFA. In 1987, Thorogood et al. concluded that the differences in cholesterol concentration suggested that the incidence of CHD may be 24 % lower in lifelong British vegetarians and 57 % lower in lifelong vegans than in meat eaters( Reference Thorogood, Carter and Benfield 33 ).
The main diet-related determinants of hypertension are high salt intake, obesity and excess alcohol consumption( 35 ). Western vegetarians have a lower average BMI than non-vegetarians, but do not necessarily have low intakes of salt and alcohol. Data from the European Prospective Investigation into Cancer and Nutrition-Oxford (EPIC-Oxford) study showed significant differences in age-adjusted prevalence of self-reported hypertension across four diet groups (meat eaters, fish eaters, vegetarians and vegans) with the lowest prevalence in the vegans and the highest prevalence in the meat eaters, although these differences were attenuated by further adjustment for BMI; differences in measured systolic blood pressure between the diet groups were moderate and were non-significant after adjustment for BMI( Reference Appleby, Davey and Key 36 ). In AHS-2, an analysis of data from 500 white members of the cohort found lower mean systolic and diastolic blood pressure in lacto-ovo-vegetarians and vegans compared with omnivores, these differences translating into significantly lower risks for hypertension, effects that were only partly explained by differences in BMI between the diet groups( Reference Pettersen, Anousheh and Fan 37 ). Vegetarians in the Indian Migration Study also had lower systolic and diastolic blood pressure than non-vegetarians, but the differences were very small (<1 mm Hg) and only statistically significant for diastolic blood pressure( Reference Shridhar, Dhillon and Bowen 32 ). Overall the data show small differences in blood pressure and the prevalence of hypertension between vegetarians and non-vegetarians, but are inconclusive as to whether these small differences are partly or wholly attributable to differences in BMI.
Ischaemic heart disease
IHD is the most common cause of death globally, being responsible for more than 8 million deaths worldwide in 2013( 38 ). Risks for both fatal and non-fatal IHD appear to be lower in vegetarians compared with non-vegetarians. A collaborative re-analysis in 1999 of data from five prospective studies (the first five studies listed in Table 1) showed that IHD mortality was 24 % lower (95 % CI 6, 38) in vegetarians than in non-vegetarians( Reference Key, Fraser and Thorogood 20 ).
More recently, analyses in EPIC-Oxford included non-fatal as well as fatal end points and the risk of hospitalization or death from IHD was 32 % (95 % CI 19, 42) lower in vegetarians compared with non-vegetarians( Reference Crowe, Appleby and Travis 39 ). Thus there is strong evidence that the risk of IHD is lower in vegetarians than in comparable non-vegetarians, and the data suggest that much of this difference may be due to the lower LDL cholesterol of vegetarians, together with their lower BMI and slightly lower systolic blood pressure.
Stroke
Stroke (cerebrovascular disease) is the second most common cause of death globally, being responsible for more than 6 million deaths worldwide in 2013( 38 ). A collaborative re-analysis in 1999 of data from five prospective studies (the first five studies listed in Table 1) showed that stroke mortality did not differ significantly between vegetarians and non-vegetarians (the death rate ratio in vegetarians v. non-vegetarians was 0·93; 95 % CI 0·74, 1·17)( Reference Key, Fraser and Thorogood 20 ). In a subsequent analysis of data from the EPIC-Oxford study, cerebrovascular disease mortality also did not differ significantly between dietary groups (relative risk in vegetarians compared with meat eaters 1·11; 95 % CI 0·76, 1·62)( Reference Key, Appleby and Spencer 40 ). More research is needed, in particular to examine risks of sub-types of stroke and to determine whether dietary factors such as a low intake of vitamin B12 in vegetarians might have an adverse impact on risk of stroke.
Cancer
A collaborative analysis of data from the first five studies listed in Table 1, published in 1999, found no significant difference in death rates between vegetarians and non-vegetarians for cancers of the stomach, colorectum, lung, breast or prostate( Reference Key, Fraser and Thorogood 20 ). This analysis did not examine overall cancer mortality, but a subsequent analysis of mortality in AHS-2 found no significant difference in overall cancer mortality between vegetarians and non-vegetarians( Reference Orlich, Singh and Sabaté 41 ).
For cancer incidence, information on site-specific cancer incidence comes from a pooled analysis of nearly 5000 incidence cancers using data from the EPIC-Oxford and Oxford Vegetarian studies( Reference Key, Appleby and Crowe 42 ). In this analysis, the non-vegetarians were subdivided into meat eaters and fish eaters (who ate fish but not meat) and incidence rates compared across the three diet groups. Significant heterogeneity of risk between the diet groups were found for the following cancers: stomach cancer, with lower risk in vegetarians (relative risk and 95 % CI compared with meat eaters 0·37, 0·19, 0·69); colorectal cancer, with lower risk in fish eaters (0·66, 0·48, 0·92) but not in vegetarians; cancers of the lymphatic and hematopoietic tissues, with lower risk in vegetarians (0·64, 0·49, 0·84), largely due to a significantly lower risk of multiple myeloma in vegetarians (0·23, 0·09, 0·59). There were no significant differences in incidence rates for other common cancers sites including the breast and prostate. Overall cancer incidence rates were significantly lower in both fish eaters (relative risk and 95 % CI compared with meat eaters 0·88, 0·80, 0·97) and in vegetarians (0·88, 0·82, 0·95). When the vegetarians were subdivided into lacto-ovo-vegetarians and vegans, risks for all cancers combined relative to meat eaters were statistically significant (0·89, 0·83, 0·96 for lacto-ovo-vegetarians and 0·81, 0·66, 0·98 for vegans). Further adjustment for BMI made little difference to the relative risks, and the associations remained statistically significant.
Analyses of the incidence of cancer in relation to diet group have also been reported for AHS-2( Reference Tantamango-Bartley, Jaceldo-Siegl and Fan 43 , Reference Orlich, Singh and Sabaté 44 ). Colorectal cancer incidence was compared across five diet groups; the lowest risk was found among fish eaters (described as pesco-vegetarians in the study), with an adjusted relative risk for all colorectal cancers of 0·57 (95 % CI 0·40, 0·82) compared with non-vegetarians( Reference Orlich, Singh and Sabaté 44 ). Risks were non-significantly lower than in non-vegetarians for semi-vegetarians (who ate meat at least once per month but not more than once per week), lacto-ovo-vegetarians and vegans (relative risks and 95 % CI 0·92, 0·62, 1·37; 0·82, 0·65, 1·02; and 0·84, 0·59, 1·19, respectively). When the vegetarian groups, including the fish eaters, were combined, the relative risk compared with the non-vegetarians was 0·78 (95 % CI 0·64, 0·95)( Reference Orlich, Singh and Sabaté 44 ). For all cancers combined, the incidence in comparison with non-vegetarians was 0·98 (95 % CI 0·82, 1·17) for semi-vegetarians, 0·88 (95 % CI 0·77, 1·01) for fish eaters, 0·93 (95 % CI 0·85, 1·02) for lacto-vegetarians and 0·84 (95 % CI 0·72, 0·99) for vegans, with a significantly lower risk for all vegetarian groups combined (relative risk and 95 % CI 0·92, 0·85, 0·99)( Reference Tantamango-Bartley, Jaceldo-Siegl and Fan 43 ).
Breast cancer incidence was also compared across four diet groups in the UK Women's Cohort study: red meat eaters, poultry eaters (who did not eat red meat), fish eaters (who did not eat meat) and vegetarians( Reference Cade, Taylor and Burley 45 ). In pre-menopausal women there were no differences in risk between the diet groups. In postmenopausal women fish eaters but not vegetarians had lower risks compared with meat eaters (relative risks and 95 % CI 0·60, 0·38, 0·96; and 0·85, 0·58, 1·25, respectively).
In summary, there is some evidence that the risk for cancer at all sites combined is slightly lower in vegetarians than in non-vegetarians, and that people who eat fish but not meat may have a lower risk of colorectal cancer, but the findings for other individual cancer sites are inconclusive.
Fracture risk and bone health
The role of diet in bone health is complex. It has been suggested that vegetarians, and especially vegans, may be at greater risk of low bone mineral density and fracture than non-vegetarians( Reference Tucker 8 ). Data from the EPIC-Oxford study showed no differences in self-reported incident fractures between meat eaters, fish eaters and lacto-ovo-vegetarians, but vegans had a 30 % (95 % CI 2, 66) higher risk of fracture compared with meat eaters( Reference Appleby, Roddam and Allen 46 ). Among subjects consuming at least 525 mg/d calcium (an amount equal to the UK estimated average requirement) there was no difference in fracture risk between the diet groups, suggesting that the low calcium intakes of many vegans (below the estimated average requirement in almost half of the vegans, compared with less than 6 % below the estimated average requirement in each of the other diet groups) was responsible for the raised risk. In the Adventist studies, risks of self-reported wrist fractures in older women (AHS)( Reference Thorpe, Knutsen and Beeson 47 ) and hip fractures in men and women (AHS-2)( Reference Lousuebsakul-Matthews, Thorpe and Knutsen 48 ) were both higher in those who never ate meat than in those who ate meat frequently; there was also evidence suggesting a protective effect of protein, whether of plant or animal origin( Reference Thorpe, Knutsen and Beeson 47 ).
A meta-analysis of nine studies found that bone mineral density was 4 % (95 % CI 2, 7) lower in vegetarians than in omnivores at both the femoral neck and the lumbar spine, with a greater difference at the lumbar spine in vegans (6 % lower bone mineral density than omnivores) than in lacto-ovo-vegetarians (2 % lower than omnivores)( Reference Ho-Pham, Nguyen and Nguyen 49 ); a subsequent study of 210 postmenopausal women in Vietnam found no difference in femoral bone mineral density between vegans and omnivores( Reference Ho-Pham, Vu and Lai 50 ). More research is needed on bone mineral density in vegetarians, in particular to provide better understanding of the relative importance of dietary factors and body composition.
Other diseases and conditions
Analyses of the risks for several other diseases and conditions have been reported from EPIC-Oxford. The risk of diverticular disease of the colon was 31 % (95 % CI 14, 45) lower in vegetarians compared with meat eaters( Reference Crowe, Appleby and Allen 51 ); when the vegetarians were subdivided into lacto-ovo-vegetarians and vegans the latter group had a 72 % (95 % CI 26, 90) lower risk of diverticular disease compared with meat eaters. This study also found a strong inverse association between dietary fibre intake and diverticular disease risk, but both associations remained statistically significant after mutual adjustment. Other analyses in EPIC-Oxford showed that vegetarians (including vegans) were at lower risk of eye cataract compared with meat eaters (relative risk 0·74, 95 % CI 0·63, 0·86), with a progressive reduction in risk from high (at least 100 g/d) to low (<50 g/d) intake meat eaters, fish eaters, lacto-ovo-vegetarians and vegans( Reference Appleby, Allen and Key 52 ). Vegetarians in the EPIC-Oxford study also had a 31 % (95 % CI 2, 52) lower risk of kidney stones compared with participants consuming a high meat diet( Reference Turney, Appleby and Reynard 53 ).
Analyses from AHS showed that high meat consumption was associated with a higher prevalence of degenerative arthritis and soft tissue disorders( Reference Hailu, Knutsen and Fraser 54 ); compared with non-meat eaters, multivariate OR for the condition in occasional (<1 x/week) and regular (≥1 x/week) meat eaters were 1·31 (95 % CI 1·21, 1·43) and 1·49 (1·31, 1·70) in women, and 1·19 (1·05, 1·34) and 1·43 (1·20, 1·70) in men. A cross-sectional analysis of 773 participants in AHS-2 found that vegetarians had a significantly lower risk of having metabolic syndrome compared with non-vegetarians (OR 0·44, 95 % CI 0·30, 0·64)( Reference Rizzo, Sabaté and Jaceldo-Siegl 55 ). In the same study, prevalence of self-reported hyperthyroidism was significantly lower in each of fish eaters, lacto-ovo-vegetarians and vegans compared with omnivores (OR and 95 % CI 0·74, 0·56, 1·00; 0·65, 0·53, 0·81; and 0·49, 0·33, 0·72, respectively)( Reference Tonstad, Nathan and Oda 56 ).
All-cause mortality and life expectancy
In the pooled analysis of mortality in five prospective studies in 1999, the death rate ratio in vegetarians compared with non-vegetarians, based on a total of 8330 deaths, was 0·95 (95 % CI 0·82, 1·11)( Reference Key, Fraser and Thorogood 20 ). However, the death rate ratios for vegetarians compared with non-vegetarians varied between studies from 0·80 to 1·17, and the test for heterogeneity between studies was highly significant (P < 0·0001). When the diet groups were subdivided, all-cause mortality was significantly lower in occasional meat eaters (death rate ratio and 95 % CI 0·84, 0·77, 0·90), fish eaters (0·82, 0·77, 0·96), and lacto-ovo-vegetarians (0·84, 0·74, 0·96), but not in vegans (1·00, 0·70, 1·44) compared with regular meat eaters (defined as those eating meat at least once per week)( Reference Key, Fraser and Thorogood 20 ). Subsequent analyses of mortality data from the EPIC-Oxford and AHS-2 studies, based on 1513 and 2570 deaths, respectively, produced contrasting results. In EPIC-Oxford, there was no significant difference in all-cause mortality between vegetarians and non-vegetarians (death rate ratio and 95 % CI 1·05, 0·93, 1·19)( Reference Key, Appleby and Spencer 40 ). When the non-vegetarians in this study were subdivided as meat eaters and fish eaters (who ate fish but not meat) the death rate ratios compared with meat eaters were 0·89 (95 % CI 0·75, 1·05) in fish eaters and 1·03 (95 % CI 0·90, 1·16) in vegetarians. Analyses in both AHS and AHS-2 have shown lower mortality in vegetarians and semi-vegetarians combined than in non-vegetarians( Reference Fraser and Shavlik 57 , Reference Orlich, Singh and Sabaté 41 ); in AHS-2, death rate ratios in semi-vegetarians, fish eaters, lacto-ovo-vegetarians and vegans compared with non-vegetarians were 0·92 (95 % CI 0·75, 1·13), 0·81 (0·69, 0·94), 0·91 (0·82, 1·00), and 0·85 (0·73, 1·01), respectively( Reference Orlich, Singh and Sabaté 41 ).
In the analysis of mortality data from the EPIC-Oxford study, standardised mortality ratios relative to the UK population for all causes of death were 52 % for both vegetarians and non-vegetarians( Reference Key, Appleby and Spencer 40 ). Low mortality relative to the general population is a common finding in prospective cohort studies owing to the ‘healthy volunteer effect’, partly as a consequence of healthy lifestyle choices such as the avoidance of tobacco( Reference Davey, Spencer and Appleby 17 , Reference Butler, Fraser and Beeson 13 ), but the strikingly low mortality of both vegetarians and non-vegetarians in EPIC-Oxford does suggest that the general health of both groups is good.
Conclusions
The amount of data available is not large, but the results so far suggest that the long-term health of vegetarians is good, and may be better than that of comparable non-vegetarians for some conditions and diseases such as obesity and IHD. Stroke mortality has not been shown to differ between vegetarians and non-vegetarians. Overall cancer rates may be slightly lower in vegetarians, but the data are inconclusive for most common individual cancers. Bone fracture rates in lacto-ovo-vegetarians may be similar to those in non-vegetarians, but more data on this are needed; fracture rates are higher in vegans if they have inadequate intakes of calcium. Vegetarians have also been found to have lower risks for diabetes, diverticular disease, eye cataract, degenerative arthritis, hyperthyroidism and the metabolic syndrome, but these findings need to be further investigated in other studies. Overall mortality is similar for vegetarians and comparable non-vegetarians, but vegetarian groups compare favourably with the general population.
More data are needed, for example on stroke and sub-types of stroke, bone health and diseases and conditions not yet studied, as well as for vegetarians and others with a low intake of animal products in non-western populations. For vegans, the current data are insufficient to draw any strong conclusions and much more research is required.
Acknowledgements
We thank our colleagues, past and present, at the Cancer Epidemiology Unit, the many researchers who have studied the health of vegetarians and vegans, and participants in these studies, irrespective of their dietary preferences.
Financial Support
Medical Research Council MR/M012190/1.
Conflicts of Interest
T. J. K. is a member of the Vegetarian Society and the Vegan Society.
Authorship
P. N. A. and T. J. K. wrote the paper.