Iodine deficiency in pregnant women can lead to an inadequate supply of thyroid hormones to the fetus resulting in impaired fetal brain development, reduced intelligence scores and impaired motor skills in the offspring of deficient women(Reference Haddow, Palomaki and Allan1). The importance of adequate iodine intake in pregnancy is such that WHO recommendations of 150 μg/d for non-pregnant adults are increased to 250 μg/d in pregnancy(2). Although the UK is normally considered to be iodine sufficient(Reference Lee, Lewis, Buss, Holcombe and Lawrance3), concern has been expressed recently about the iodine status of UK women(Reference Kibirige, Hutchison, Owen and Delves4).
A cross-sectional pilot study was therefore undertaken in thirty-one women of child-bearing age (median age 23 years) to investigate the iodine status of Surrey women. Urine collections (24 h) were obtained and their total volume measured. Iodide concentration was measured using inductively-coupled plasma MS. Total 24 h iodide excretion was calculated and used to assess the individual risk of deficiency. Daily iodine intake was calculated assuming that the 24 h urinary iodide excretion represents 92% of daily iodine intake(5).
The Figure shows the 24 h iodide excretion for each subject and the categorisation of iodine status according to Thomson et al.(Reference Thomson, Colls, Conaglen, Macormack, Stiles and Mann6) and Als et al.(Reference Als, Minder, Willems, Van Thi, Gerber and Bourdoux7). One subject (3.2%) was classified as moderately deficient, eight (25.8%) had mild deficiency, ten (32.3%) had marginal iodine status and the remaining twelve subjects (38.7%) had adequate iodine status. The median total 24 h iodide excretion was 140.5 μg, categorising the group as a whole as having marginal iodine status. Calculation of iodine intake (extrapolated from urinary iodide excretion) indicated that 48% did not meet the WHO adult requirement of 150 μg/d, 42% had an intake below the UK reference nutrient intake and 87% would not meet the 250 μg/d WHO intake requirement for pregnancy(2).
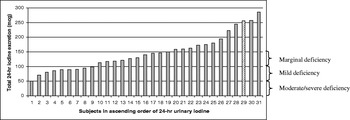
Figure. The 24 h urinary iodide excretion for Surrey women of child-bearing age and iodine deficiency classification(Reference Thomson, Colls, Conaglen, Macormack, Stiles and Mann6, Reference Als, Minder, Willems, Van Thi, Gerber and Bourdoux7). (![]() ), Subject took iodine-containing supplement.
), Subject took iodine-containing supplement.
The findings of the present small study give cause for concern as approximately 30% of individuals were classified as mildly to moderately iodine deficient. This finding could have serious consequences if these women were to become pregnant. Various limitations of the study (selection of subjects and season) suggest that this outcome is likely to be a best-case scenario. It may be prudent to advise all pregnant women to increase their intake of iodine-rich foods during pregnancy or to include an iodine supplement in order to minimise potentially adverse effects on the fetus.



