There is an abundance of scientific literature that links healthy diets to physical and mental health. Yet inequalities have endured and continue to widen. It is increasingly recognised that wide-scale adoption of healthy behaviour requires a shift in thinking from individuals to populations and from proximal determinants to the ‘causes of the causes’. The social ecological model(Reference Bronfenbrenner1) provides a broad perspective integrating multiple levels of influence (e.g. families, neighbourhoods and communities, policies) that impact on health behaviour and ultimately health outcomes. Health promotion programmes that focus only on behavioural change or downstream impacts through educational activities or other strategies to change behaviours at the within-person level, often neglect the social and environmental contexts in which adverse behaviours occur and are reinforced(Reference Al-Khudairy, Loveman and Colquitt2). Improving the health of vulnerable populations necessitates interventions that target multiple levels of influence, in multiple settings and use multiple intervention strategies. Interventions that engage with this complexity are challenging to design, implement and evaluate, but likely to leverage substantive sustainable impacts. This has been a central consideration of our Kings and Communities for Youth Health research programme which is exploring how best to promote healthy nutrition among adolescents living in urban environments and at high risk of nutrition-related diseases.
London's global context: an asset and a risk
London is a global city characterised by a multiplicity of ethnicities, languages, cultures, food choices and religious beliefs. Data from the 2011 Census showed London to have above national average proportions for most minority ethnic groups including African (7 %), Indian (6·6 %) and Caribbean (4·2 %), with the proportion of non-UK born residents increasing >10 % between 2001 and 2011. Over 250 languages are spoken in London, with almost a quarter (22 %) of the population reporting a language other than English as their main language and with 4·1 % of the population unable to speak English(3).
The perceived threat of diversity has received much media emphasis recently, fuelled by political events including Brexit and anti-immigration rhetoric, increased social inequalities and terrorism events. Several studies propose, however, that diversity is linked to London's social capital and economic growth(Reference Fukuyama4, Reference Putnam5). Social capital, i.e. access to social networks and resources, has been theorised to operate through ‘bonding capital’ within groups or ‘bridging capital’ across groups(Reference Waterston, Alperstein and Stewart Brown6). Diversity has been shown to improve perceptions of and relations between ethnic groups with ‘bridging ties’ in diverse social settings resulting in greater social cohesion and positive social interactions(Reference Laurence7, Reference Stolle, Soroka and Johnston8). Cultural diversity and its associated social capital, the synergistic interplay of community assets (e.g. trust, cooperation, shared values, social networks), also contribute to London's diet and nutrition-related behaviour diversity(Reference Rawlins, Baker and Maynard9). London's reputation as one of the world's culinary capitals, for example, is based on the variety of ethnic food options. Local high streets reflect ethnic enclaves, forming geographical and cultural niches with a plethora of food-related businesses and services adapted to the needs of different ethnic groups.
London's social and ethnic inequalities are, however, deep and enduring: 22·5 % of London falls within the most deprived 20 % of England, while the boroughs of Tower Hamlets, Haringey, Hackney, Lambeth, Lewisham, Barking and Dagenham are among the top 1 % of lower super output areas for deprivation in England(Reference Leeser10). The rate of early deaths from preventable causes is twice as high in Tower Hamlets as it is in the nearby City of London(11). Ethnic differences in deprivation are stark, with Pakistanis, Bangladeshis and Black ethnic origin people more likely to live in the most deprived areas(12). Pakistani households are more likely to be overcrowded compared with White British(12). The social and economic aspects of deprivation (i.e. poverty, social exclusion) present major challenges for public health initiatives aimed at tackling obesity in urban areas.
People of South Asian or Black African descent have respectively 4- and 3- fold elevated risks of diabetes compared with White Europeans. Risks of hypertension and stroke are also greater in these groups, but while South Asians also experience higher rates of coronary disease, people of Black African origin are protected(Reference Riste, Khan and Cruickshank13, Reference Tillin, Hughes and Mayet14). There is increasing evidence that ethnic differences in risk factors, such as blood pressure, emerge in childhood with greater metabolic sensitivity to adiposity than in White ethnic groups(Reference Whincup, Nightingale and Owen15, Reference Harding, Whitrow and Lenguerrand16). Our work focuses on adolescence, a key stage of the life course characterised by a complex development period during which physical, psychological, social and emotional capabilities are consolidated and underpin future health, social and economic trajectories. On a global scale, the benefits of investment in adolescent health are increasingly recognised and failure to address health inequalities at this stage can set young people on a path to lifelong socio-economic and health adversity(Reference Sheehan, Sweeny and Rasmussen17).
More than two million children and young people live in London, about a quarter of the London population, with an 11 % rise expected by 2020(18). London has a high rate of child obesity compared with other global cities. Young people face the challenge of negotiating obesogenic environments(Reference Lake and Townshend19): their physical activity shaped by the built environment, their diets by food systems that bombard them with energy-dense foods often cheaper than healthier alternatives and their well-being compromised by precarious employment and high costs of housing. Our research engages with this complexity of context faced by adolescents, to address inequalities in health and obesity. We first discuss key findings from the Determinants of young Adult Social well-being and Health (DASH), our longitudinal study of adolescents living in London, before reporting on early findings from a programme of feasibility studies in London, the Caribbean and Saudi Arabia.
Socio-cultural influences on London's adolescent health
The DASH study is the largest longitudinal study of ethnically diverse young people in the UK designed to examine ethnic inequalities in health. Details of DASH are described elsewhere(Reference Harding, Whitrow and Maynard20). Underpinned by the life course model(Reference Kuh and Shlomo21), the study centres on adolescence, a critical stage for establishing lasting health trajectories, both mental and physical, and consolidation of lifestyle behaviours. The sample was recruited between 2002 and 2003 from fifty-one schools in ten London boroughs. A total of 6643 pupils, aged 11–13 years, took part in the baseline survey and about 80 % took part in a follow-up survey at 14–16 years. A pilot follow-up was conducted with 10 % of the sample at 21–23 years, including qualitative interviews with forty-two participants from diverse ethnic backgrounds. About 80 % of the cohort are from ethnic minorities and speak more than forty languages. Two-thirds of these were UK born, with about a hundred countries of birth reported among those born abroad. We take the position that ethnic identity is dynamic and multidimensional, reflecting historic social and cultural traditions and current context(Reference Bradby22). Ethnicity in DASH was measured by self-report utilising over twenty-five ethnic categories derived from the British Census, including options for ‘mixed’ and ‘other’. Separate questions were asked about country of birth of self, parents and grandparents. Self-ascribed ethnicity was compared with these responses to check for inconsistencies. The sample is well characterised in relation to diversity, psychosocial and biological measures.
Despite the recent polarised debate observed in the mid-Brexit climate, findings from DASH support a view of diversity as a public health asset which can be protective against adverse health outcomes. As reported in the qualitative interviews, growing up in contexts of cultural diversity and religious values was perceived to have positive benefits (Table 1). Ethnic minority adolescents in the DASH cohort exposed to London's multi-lingual/religion environments exhibited strong psychological resilience and sense of pride from cultural straddling, despite more material disadvantage and experience of racism throughout adolescence compared with their White peers (Fig. 1).
Table 1. In their own words: The Determinants of Adults Social well-being and Health (DASH)
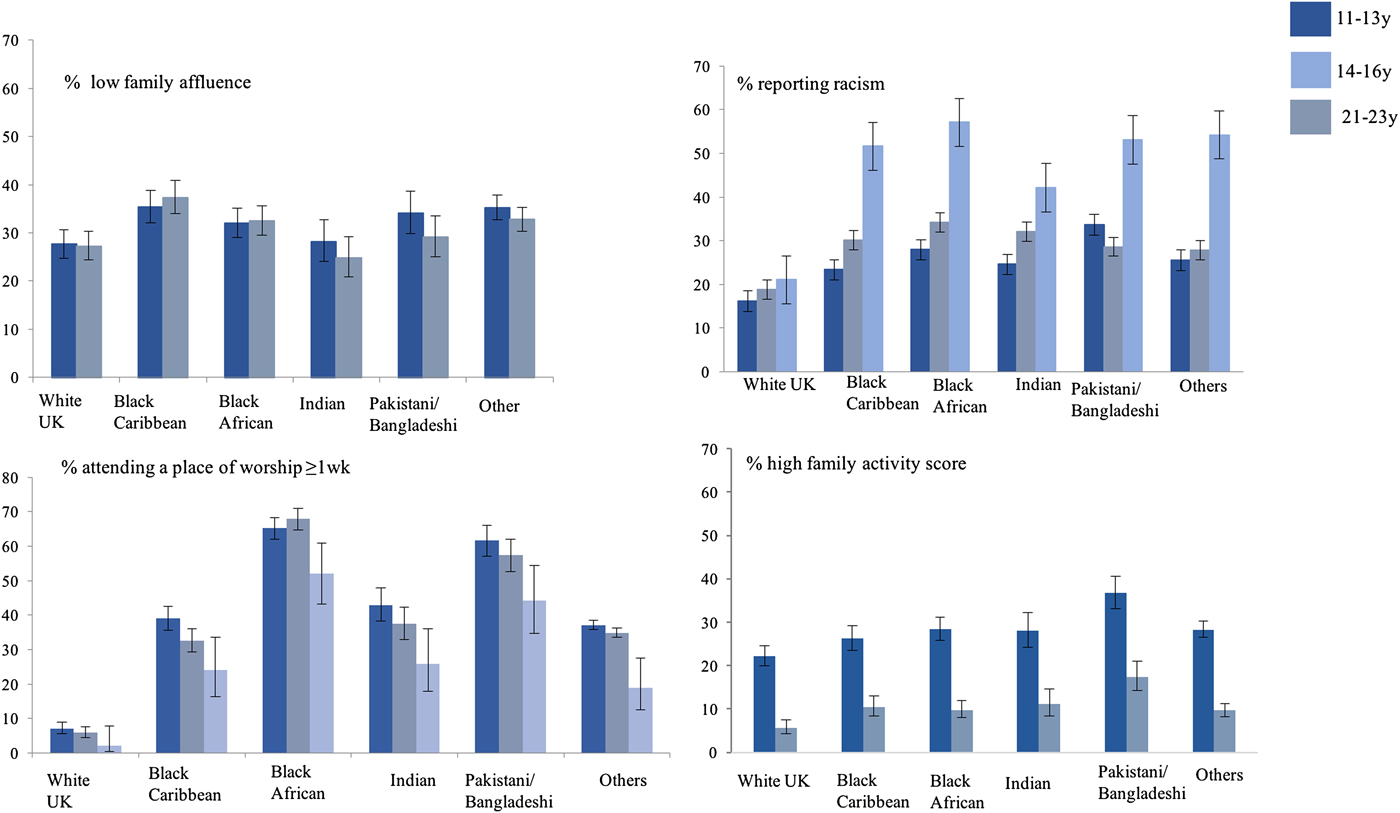
Fig. 1. (Colour online) Cumulative exposure to disadvantage, family activities, racism, religious engagement and family engagement activities at 11–13 years, 14–16 years (y) and 21–23 years, by ethnicity: percentage and 95 % CI. The Determinants of young Adult Social well-being and Health (DASH) study(Reference Harding, Read and Molaodi28). Family activities(Reference Sweeting and West26) included watching television or videos, playing indoor games, eating a meal, going for a walk or playing sports, visiting friends or relatives and going other places; a score was derived based on frequencies of all six activities, with a higher score indicating better family connectedness. The score was recoded into tertiles (based on thresholds for tertiles at 11–13 years). Only the high score tertile is shown. Family Affluence Scale(Reference O'Donnell, Harding and O'Keeffe76) was derived from number of cars, computers, holidays and own bedroom, coded high (≥3), medium (1–2) and low (0); high affluence only shown. Experiences of discrimination(Reference Elia, Karamanos and Joao Silva78) scale which includes questions on ‘unfair treatment’ on the grounds of race, skin colour place of birth and religion in various locations e.g. school, work, on the street. Sample sizes 11–16 years/21–23 years: White British 867/107; Black Caribbean 695/102; Black African 818/132; Indian 397/98; Pakistani Bangladeshi 451/111; Others 1459/115.
Although the frequency of attendance to a place of worship declined in their early twenties, compared with White participants, more ethnic minority participants continued to attend a place of worship into young adulthood, as well as reporting regular engagement with family activities, issues which we will return to in relation to their health benefits. In adolescence, better mental health was observed among ethnic minority youths, particularly Nigerian/Ghanaian males, compared with their White British peers(Reference Maynard, Harding and Minnis23, Reference Bhui, Silva and Harding24). Measures of linguistic diversity, attendance at a place of worship, parenting styles(Reference Klimidis, Minas and Ata25), family centredness(Reference Sweeting and West26) and cultural integration(Reference Bhui, Stansfeld and Head27), were independently associated with improved adolescent mental health, after adjustment for social adversity(Reference Harding, Read and Molaodi28). A London-based study further documented this psychological resilience (better mental health problems despite the greatest socioeconomic disadvantage) among Bangladeshi adolescents compared with their White peers(Reference Bhui, Silva and Harding24, Reference Stansfeld, Haines and Head29). The impact of place of worship attendance, independent of religious affiliation, suggest that health benefits may be mediated through social support, cultural identity and resilience to adversity, particularly racism(Reference Assari30). Regular attendance to a place of worship may promote ‘ethnic socialisation’, which may have benefits for mental health, adaptation and health behaviours(Reference Berry, Phinney and Sam31, Reference Schwartz, Unger and Zamboanga32).
Ethnicity and dietary habits
We focus here on two key dietary habits measured in adolescence: fruit and vegetable intake and breakfast consumption. An extensive literature base has demonstrated that reduced intake of fruit and vegetables is associated with an increased risk of CVD and cancer(Reference Lim, Vos and Flaxman33, Reference Lock, Pomerleau and Causer34). Breakfast skipping is associated with adolescent obesity and less favourable metabolic profiles(Reference Aune, Giovannucci and Boffetta35–Reference Rampersaud, Pereira and Girard40), increased risk-taking behaviours (tobacco, alcohol abuse, increased snacking and sedentary lifestyles)(Reference Keski-Rahkonen, Kaprio and Rissanen41) and poorer academic performance(Reference Rampersaud, Pereira and Girard40). In a systematic review, Pearson and colleagues reported that family correlates of fruit and vegetable consumption included parental intake and modelling, family rules and parental encouragement(Reference Pearson, Biddle and Gorely42). As with fruit and vegetable intake, the family environment has a key influence on breakfast consumption and parental breakfast consumption, two-parent family units being positively associated, whereas socioeconomic disadvantage is inversely associated(Reference Pearson, Biddle and Gorely43, Reference O'Dea and Caputi44).
DASH has shown that throughout adolescence, ethnicity, parental care(Reference Parker, Tupling and Brown45) and family activities were independently associated with fruit and vegetable consumption of <5 portions daily among both men and women, after adjusting for main confounders (Table 2). Black Caribbeans, Black Africans and Pakistanis/Bangladeshis were more likely to consume <5 portions of fruit and vegetables daily than their White British peers. Decreasing parental care and family activities were associated with a greater likelihood of lower than 5 portions daily. Among females, increasing age was associated with a lower likelihood of consuming <5 portions daily. There were some ethnic-specific effects for females as tested by interaction terms ethnicity × parental care and ethnicity × family activities. In particular, Black Africans who reported low parental care and Black Caribbeans and Black Africans who reported low family activities score significantly more likely to have <5 portions daily. We did not find an association between socioeconomic circumstances with fruit and vegetable intake, adding to the inconsistencies reported in the literature(Reference Pearson, Biddle and Gorely42, Reference Neumark-Sztainer, Story and French46, Reference Giskes, Turrell and Patterson47). Another important feature of the findings in Table 2 is that lower frequency of physical activity was associated with <5 portions of fruit and vegetable consumption, reflecting a clustering of unhealthy behaviours.
Table 2. Correlates of <5 portions of fruit and vegetables daily from 11–13 years(Reference Huang, O'Keeffe and Harding74) to 14–16 years(Reference Currie, Elton and Todd75)
The Determinants of young Adult Social well-being and Health (DASH) study.
OR were estimated by multilevel mixed-effects logistic regression, adjusted for ethnicity, age, generational status, physical activity, smoking, drinking alcohol, vegetarian, religious prohibition of food, slimming diet, worry about weight gain, unhappy if overeating, paternal smoking, maternal smoking, paternal overweight, maternal overweight, parental care, parental control, family activities score, family affluence and family structure. Parental care and control were measured using the Parental Bonding Instrument(Reference Klimidis, Minas and Ata25), with scores recoded into tertiles (based on thresholds for tertiles at 11–13 years); Family activities(Reference Sweeting and West26) included watching television or videos, playing indoor games, eating a meal, going for a walk or playing sports, visiting friends or relatives, and going other places; a score was derived based on frequencies of all six activities, with a higher score indicating better family connectedness; the score was recoded into tertiles (based on thresholds for tertiles at 11–13 years). Physical activity measured frequency of nineteen or more activities over last 7 days. Family Affluence Scale(Reference O'Donnell, Harding and O'Keeffe76) was derived from number of cars, computers, holidays and own bedroom, coded high (≥3), medium (1–2) and low (0). Significant level for values in Table is P < 0·05.
Risk-taking behaviour peaks in adolescents so that clustering of risky dietary behaviour is not surprising(Reference Leech, McNaughton and Timperio48, Reference Hardy, Grunseit and Khambalia49). DASH shows some evidence for clustering adverse dietary behaviours. Fig. 2 shows that in early adolescence (11–13 years) fruit and vegetable consumption of <5 portions daily was associated with skipping breakfast, among both genders, in White British and Other Ethnicity groups, and among Black Caribbean males, Black African males and Indian girls, after adjusting for confounders.
Fig. 2. Breakfast skipping among 11–13-year-old adolescents with fruit and vegetable consumption <5 portions/d v. ≥5 portions/d by sex and ethnicity, plotted on a log scale. The Determinants of young Adult Social well-being and Health (DASH) study(Reference Currie, Elton and Todd75). White British males: n 595; White British females: n 555; Black Caribbean males: n 413; Black Caribbean females: n 410; Black African males: n 427; Black African females: n 510; Indian males: n 255; Indian females: n 210; Pakistani/Bangladeshi males: n 373; Pakistani/Bangladeshi females: n 205; Other males: n 1030; Other females: n 869. p/d = portions daily. Models adjusted for fruit and vegetable consumption, age, parental care, parental control, family activities and family affluence. Skipping breakfast was defined as not eating breakfast every day. Parental care and control were measured using the Parental Bonding Instrument(Reference Klimidis, Minas and Ata25); Family Affluence Scale(Reference O'Donnell, Harding and O'Keeffe76) was derived from the number of cars, computers and holidays and own bedroom. Family activities included watching television or videos, playing indoor games, eating a meal, going for a walk or playing sports, visiting friends or relatives, and going other places(Reference Sweeting and West26).
Table 3 shows that fruit and vegetable consumption was a longitudinal correlate of skipping breakfast from early adolescence to early adulthood (21–23 years). Even with a smaller sample, a higher likelihood of skipping breakfast was still observed among Black Caribbeans (OR 1·98, 95 % CI 1·10, 3·58, P = 0·024) and Black Africans (OR 2·62, 1·45, 4·73, P = 0·001). Here we also see that a longitudinal measure of unemployment (parental at 11–13 years and own at 21–23 years) was associated with skipping breakfast, indicating the importance of persistent economic disadvantage on skipping breakfast. Understanding the drivers of multiple dietary risk factors warrants further investigation particularly given the obesogenic urban environments in which young people live(Reference Bagwell50, Reference Townshend and Lake51).
Table 3. Association between fruit and vegetable consumption and breakfast skipping from early adolescence (11–13 years) to early 20s
Determinants of young Adult Social well-being and Health (DASH) study.(Reference Harding, Silva and Molaodi53)
Based on 10 % pilot sample (n 558). OR were estimated by multilevel mixed-effects logistic regression, adjusted for fruit and vegetable consumption, age, sex, ethnicity, parental care, parental control, and parental/own employment. Interaction term ‘ethnicity × fruit and vegetable intake’ was not significant. Skipping breakfast was defined as not eating breakfast every day. Parental care and control were measured using the Parental Bonding Instrument(Reference Klimidis, Minas and Ata25), with scores recoded into tertiles (based on thresholds for tertiles at 11–13 years). Parental employment was used as the measurement of employment at 11–13 years, while own employment was used at 21–23 years. Significant level for values in Table is P < 0·05.
Ethnicity and overweight
We recently reported on the ethnic patterning of growth from early adolescence and a prospective association between adiposity measures and CVD risk from early adolescence to early adulthood(Reference Cruickshank, Silva and Molaodi52, Reference Harding, Silva and Molaodi53). The greater cardiovascular risks observed in some ethnic minority groups in childhood signals a continuation of the biological legacy of earlier generations. Black Caribbeans and Black African girls in DASH continued to present higher rates of unhealthy BMI compared with their White peers from early adolescence to early adulthood (Fig. 3). About one-third of the sample was overweight or obese at both ages. Overweight, which was related to poor nutritional habits (cited earlier) in early adolescence, was associated with early markers of CVD risk in adulthood, including an increase in blood pressure, arterial stiffness and glycosylated Hb(Reference Cruickshank, Silva and Molaodi52, Reference Harding, Silva and Molaodi53). A key driver of these patterns are the neighbourhoods that ethnic minority adolescents live in. They tend to be clustered in poorer areas, with fewer opportunities for physical activity and increased access to fast-food outlets(Reference Molaodi, Leyland and Ellaway54).
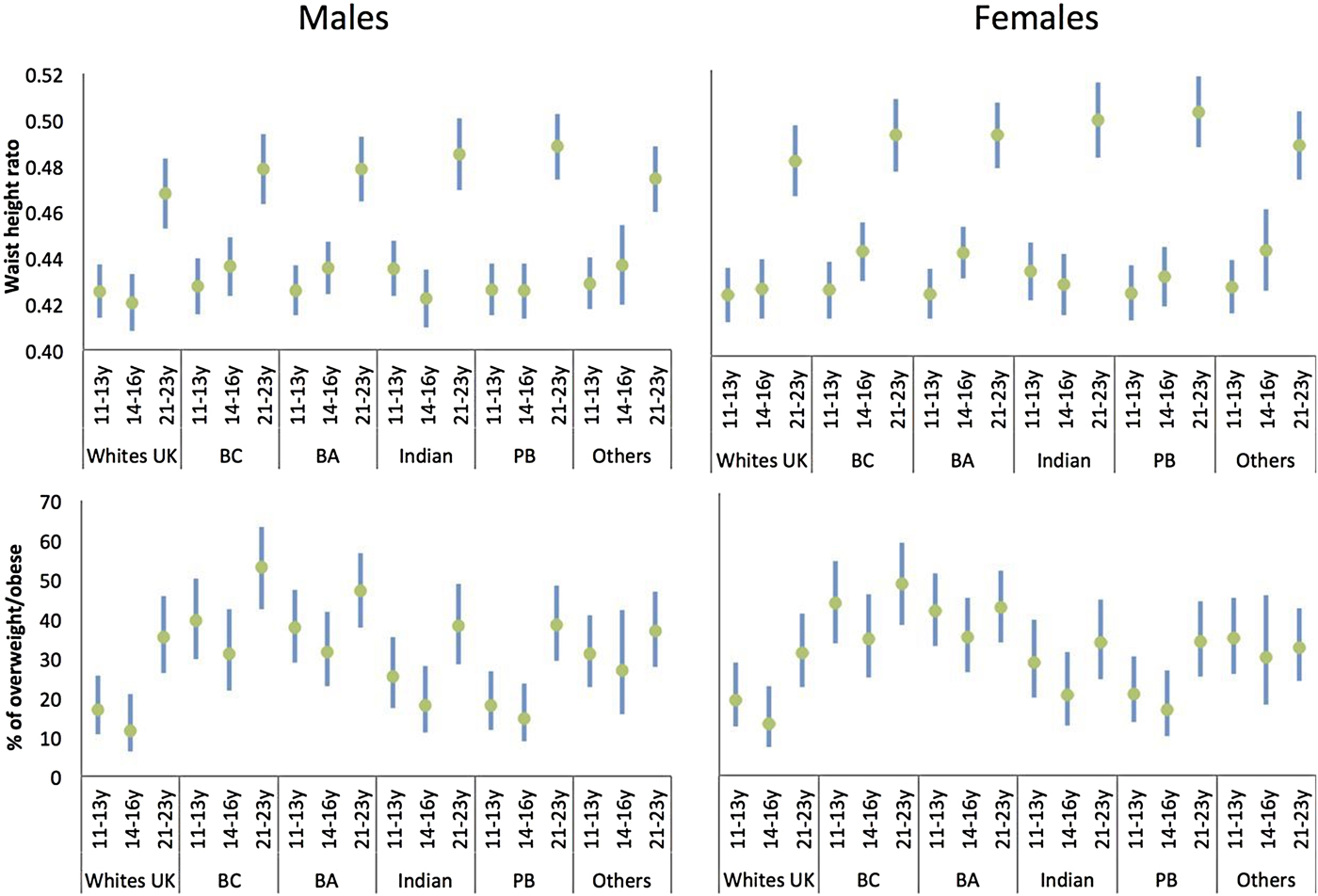
Fig. 3. (Colour online) Waist to height ratio and per cent of overweight/obese, by age and ethnicity for males and females: means/percentage and 95 % CI, adjusted for sex and ethnicity(Reference Cruickshank, Silva and Molaodi52). BA, Black African; BC, Black Caribbean; PB, Pakistani/Bangladeshi. Adapted from ‘Longitudinal study of cardiometabolic risk from early adolescence to early adulthood in an ethnically diverse cohort’.
Nutrition is important for the physical and mental health of young people. In high-income countries, 75 % of adult mental health issues have an onset before age 18 years(Reference Gore, Bloem and Patton55, Reference Patton, Coffey and Romaniuk56). We have been exploring the influence of discordance between the perception of weight and objective measures on the mental health of young people in the DASH population(Reference Elia, Karamanos and João Silva57). This literature is dominated by US research. For example, Duong and Roberts found that 22 % of female adolescents of a healthy weight were less satisfied with their weight, compared with 15 % of males and that the trend persisted over time. African American adolescents tend to underestimate their weight status(Reference Duong and Roberts58). Adolescents’ social network, parental overweight and overweight peers contribute to weight discordance, particularly underestimation(Reference Duong and Roberts58–Reference McCabe, Mavoa and Ricciardelli60). In the DASH cohort, about 40 % of adolescents perceived their weight status to be different to their objectively measured weight status. Perceived weight status was assessed using the following question ‘given your height and weight would you say you are…’ and responses included (1) about right (2) too heavy (3) too light or (4) not sure. Sex differences in discordance were observed only at the baseline where girls (46 %) were more likely to be discordant than boys (38 %, P < 0·05; unpublished results). Compared with their White peers, Pakistani/Bangladeshi girls were more likely to have a discordant weight perception throughout adolescence, Conversely, Black African, Indian and Pakistani/Bangladeshi boys were more likely to be discordant at 14–16 years (Fig. 4). Among those discordant, 9 % at age 11–13 years and 6 % at age 14–16 years perceived themselves to be normal weight but measured overweight; the corresponding figures for perceiving themselves to be underweight but measured normal were 8 % and 10 %. At both ages, 22 % were unsure of their weight but measured overweight or normal weight. Regardless of ethnicity, age and sex were longitudinal correlates of weight misperception throughout adolescence. Alcohol consumption and reported experiences of racism at 11–13 years and religious prohibition of food at 14–16 years (particularly among Muslims) were age-specific independent correlates of weight misperception. Given the impact on mental health and its common occurrence across all ethnic groups, these findings underscore the importance for addressing the influences that trigger discordant weight perceptions among different ethnic groups and genders.
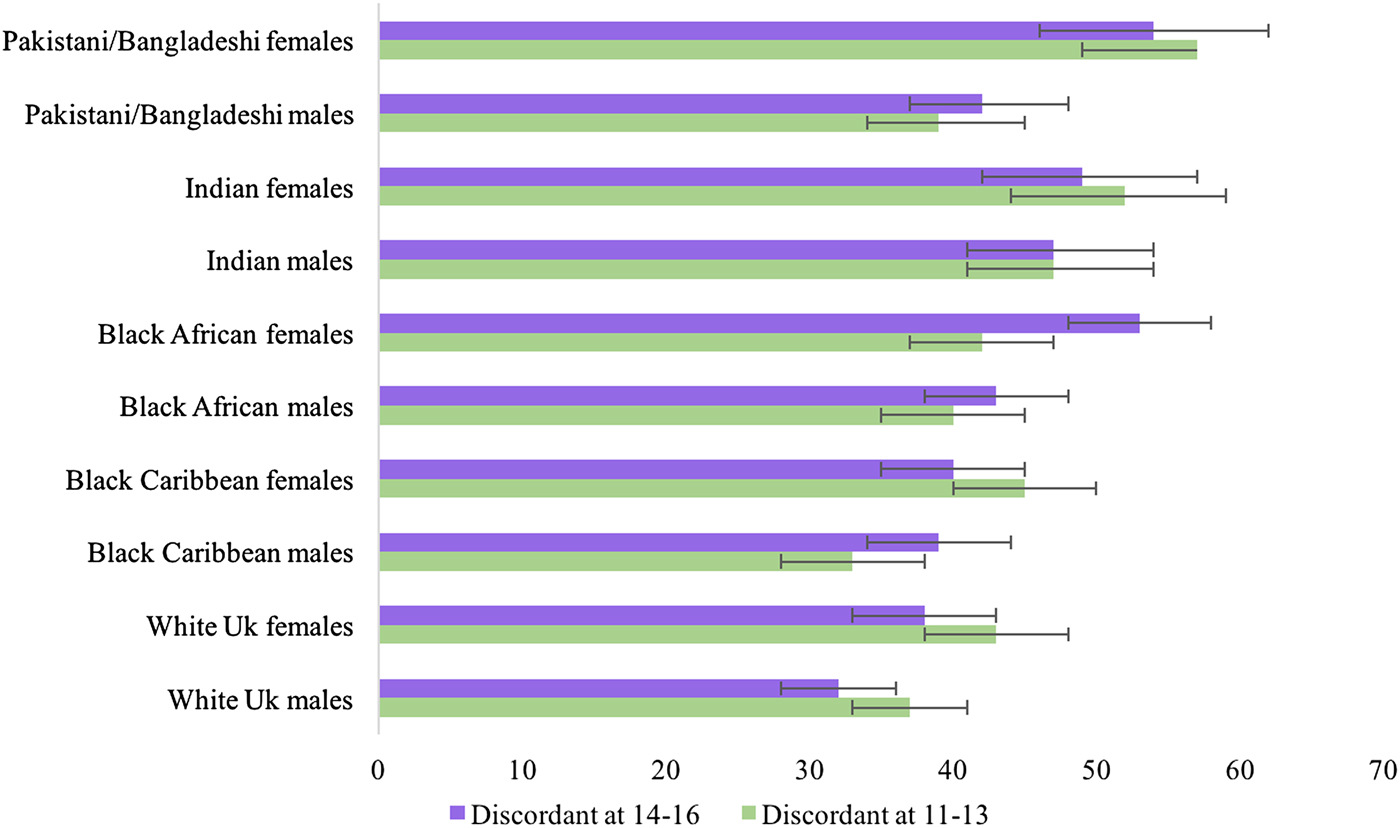
Fig. 4. (Colour online) Percentage with the perception of weight status discordant to measured weight by age and ethnicity: percentage and 95 % CI, the Determinants of young Adult Social well-being and Health (DASH) study(Reference Cole, Bellizzi and Flegal79). (n 3228). Perception of body size was assessed using the question ‘Given your height and weight would you say you are…’ and four response categories were used: (1) about right (2) too heavy (3) too light and (4) not Sure. Based on their BMI, participants were classified as underweight, normal weight, overweight or obese based on the 1990 British age and sex specific growth reference curves(Reference Cole, Bellizzi and Flegal79). Participants were classified into eight categories which are combined here as concordant or discordant weight status perception relative to measured weight status.
The next section illustrates how these findings have informed our translational studies. The sustainability of public health interventions has become increasingly important for researchers, evaluators, community partners and funders(Reference Schell, Luke and Schooley61). Our collaborations extend beyond individuals and classrooms to bridge schools, communities and service providers, and focus on prevention as a priority, with the hope that this approach will enhance sustainable capacity to support healthy nutrition.
Promoting healthy nutrition among London's adolescents
The high attendance of ethnic minority children to places of worship in London and its protective role for risk behaviours and mental health prompted us to explore places of worship as community settings for culturally tailored obesity prevention. Places of worship have long been involved in advocacy for social change including inequalities and because of their broad public reach and focus on both spiritual and physical needs have successfully delivered health programmes targeting a wide range of health outcomes(Reference Maynard, Baker and Harding62). The DASH-DiEt and Active Living study was our first exploration, small-scale but detailed, of the challenges and opportunities of engaging with the complexity of schools and places of worship (e.g. mosques, temples and churches) in London to maximise the programme impact(Reference Maynard, Baker and Harding62, Reference Maynard63). While schools provide a better infrastructure to deliver interventions, places of worship provide access to parents and other family members and potentially wider community support and reach among hard to reach ethnic minority populations. Engaging both types of setting, working in close partnership with primary and community healthcare, could provide a comprehensive approach towards reaching universal coverage for health promotion interventions. A key outcome of the DASH-DiEt and Active Living study was that the complexity of the different religious settings necessitated specific strategies. In the next section, we discuss some key findings from our current developmental studies with Black Majority Churches (BMC) and secondary schools in deprived neighbourhoods in South London with a high density of Black Caribbeans and Black Africans. BMC are defined as Black-led churches with a high density (approximately 90 %) of Black African and/ Black Caribbean congregational members. Working with community partners is an iterative organic process and there are challenges in balancing scientific rigour with the needs, interests and values of partners. Our flexible mixed-method approach, including photovoice, ethnography, focus groups and concept mapping workshops, walk along and telephone interviews, enriched our understanding of feasible solutions and optimised engagement from those who would have been difficult to reach using conventional approaches.
Community partnerships with Black Majority Churches in London for nutrition interventions
A number of factors may be related to the capacity to initiate and sustain community partnerships with BMC to implement prevention programmes. We scoped the distribution of BMC with the help of key Black Church leaders to ensure adequate representation of Black Caribbean and Black African churches. Most BMC are Pentecostal, with the highest concentration in Southwark, estimated to be >240 churches. With the help of senior Black pastors, responsible for clusters of BMC, we chose two clusters with six BMC to learn about their social programmes, including youth clubs, Sunday-schools and community clubs, all of which could provide intervention focal points for young people. We summarise some key barriers and facilitators that emerged from thematic analysis of the qualitative data from seventeen semi-structured interviews with representatives from BMC (including from youth clubs, leadership, administration and congregation), local primary care and public health, care commissioners, National Health Service England and the voluntary sector.
Challenges to collaboration
The meshing of views across practitioners, commissioners and national bodies indicated strong support for engaging with faith groups for prevention, but there appeared to be a distinct lack of shared understanding with faith groups. Reluctance to engage with faith groups attributed to perceived conflicts in attitudes, knowledge and values were acknowledged as potential barriers to partnership building:
‘I think there is an anxiety sometimes …about working with faith groups… I think it's about values… there's a reluctance sometimes to embrace those kinds of groups with open arms.’ Participant 8, face-to-face interview, commissioner, male.
‘… NHS mentality of, you know, the clinicians are the only people whose voices matter. So there's kind of attitude issues.’ Participant 11, telephone interview, national body, female.
Engagement was linked to trust and membership of communities, ‘understanding where everybody is coming from, the ‘need to build bridges for the right reasons’, and the recognition of complexity and inequality:
‘We've got such inequality…makes it a challenge because there aren't answers, you haven't got easy answers… that's a bit of a challenge.’ Participant 7, face-to-face interview, commissioner, male.
Organisational cultures were often cited as a barrier to developing partnerships and aligning agendas, with ‘silo working’, ‘competing priorities’ and challenges in finding the ‘right people that have the levers to change’:
‘… [we] need to understand the agendas of different silos because each one is trying to exist and maintain its existence… if you don't understand what's driving that…, then you're never going to be able to get that work between the silos.’ (Participant 9, face-to-face interview, practitioner, male).
Other potential challenges cited included no ‘one size fits all’, with the additional dimension of planning for ‘transient populations’ and the risk of ‘unrealistic timescales’ for building partnerships, the need for ‘stable funding streams’ rather than ‘infighting for limited funds’ and political contexts linked to ‘ever-changing directions’ of policies and cuts to local public health budgets.
Factors supporting partnerships
Having a clear vision, mission and shared interests are regarded as the key to successful partnerships(Reference Andrews and Entwistle64). Aspects such as trust, goal alignment and positive working relationships between like-minded sectors have been found to be more important determinants of cross-sectoral working (including public–private partnerships) than practical resources(Reference Merzel and D'Afflitti65).
Incentives, such as opportunities for training or work experience, were considered by congregants to be crucial for the initial involvement of communities, given the time commitment required. These were linked to capacity development and in particular to ownership of interventions and sustainability:
‘Especially when you're doing 16 plus [high school examinations], people will be looking for jobs and things like that… if you highlight what they're going to take away from this, if it's skills or if it's something for their CV that's through their involvement.’ Participant 2, focus group, congregant, female.
‘You have to train people…from this community… So they'll be shadowing you from infancy, watching it mature, understanding how it works. Then you want to kind of transfer your skills…’ Participant 1, focus group, congregant, female.
Maintaining a sense of informality, consistency and visibility were of paramount importance to congregants and generally recognised by practitioners and commissioners as facilitators for collaborative partnerships. Congregants felt it was important for there to be a humorous and light-hearted approach. Communication via online forums, social media and websites were positively reviewed by all participants. This has implications for coordination and governance arrangements, including in the healthcare sector, the extent to which partnerships are voluntary or formal and how evaluation should be conducted.
A key lesson for us has been the time and patience it takes to forge trusting relationships particularly as lack of trust is the most widely cited challenge for community-based research(Reference Israel, Schulz and Parker66). The results presented here provide some essential domains for a conceptual framework for partnership sustainability with BMC and have informed our readiness assessment for implementation.
Challenges and priorities for healthy nutrition identified by adolescents
We used concept-mapping, focus groups and researcher observations over 2 weeks to develop our understanding of what adolescents felt were important issues to address in relation to their food choices. Concept mapping is steeped in participatory approaches and is gaining recognition in public health as a tool for improving the reliability of findings via cross-sectoral cooperation from the outset(Reference Burke, O'Campo and Peak67). It entails a mixed methods approach that combines qualitative group processes (e.g. brainstorming, categorising ideas) with descriptive statistical analyses to facilitate a group description of ideas and represent them graphically. Through this process, a visual representation of the factors that are felt to be important and modifiable are created.
The findings are based on perspectives of 11–13-year-olds (sixty-nine pupils) in two secondary schools, one in a very deprived neighbourhood but both with ethnically diverse pupil populations. Thirty-seven pupils took part in four focus groups, and thirty-two pupils took part in two sets of four concept mapping workshops. Photovoice(Reference Wang and Burris68) was used whereby pupils created a picture narrative of the things that influenced their diets which was then used to brainstorm ideas about influences on healthy eating. Pupils then categorised and rated their ideas for importance and modifiability for a positive change. Results of our concept mapping analysis identified five clusters of influences: home life; school context; strong beliefs/opinions; food literacy; neighbourhood food outlets.
The position of the clusters relative to each other indicates the conceptual similarities between the different domains; those shown closer together are more similar than those that are farther apart. The size of each block denotes the perceived cohesiveness of the cluster. The statements within smaller, tighter groupings (e.g. home life) were more conceptually cohesive than the statements within more diffuse clusters (e.g. beliefs/opinions). Table 4 shows the number of items within clusters and average ratings of the clusters for importance and modifiability. We drew from the focus groups and researcher observations to help us identify the items in the clusters and highlight some salient points.
Table 4. Concept Mapping results for the domains of influence on dietary behaviours(Reference Krieger and Sidney77)

*Score out of 5.
Home life and neighbourhood environments
The ready availability of unhealthy foods at home and in neighbourhoods appeared to frustrate adolescent motivation to manage their dietary habits to their benefit. These issues appeared to be common regardless of socio-economic context, although differences appear in relation to what was available in cupboards and fridges at home:
‘I wake up with the mindset that I'm going to be extremely healthy, but as I open the fridge and I see the Gatorade or the Snickers, and I have to!’ Participant 1·02, male, 13years.
‘You're at home and you're like, ‘Mum, I really want to eat healthy’ and she's like, ‘Okay, well we're having macaroni and cheese for dinner’.’ Participant 3·04, female, 12years.
School and home neighbourhoods, and the journey from school to home derailed good intentions, as pupils passed many fast-food outlets and shops and were tempted in:
‘In primary school, you just go straight home, but now every day you walk past the shops. Like, oh, I didn't want to go to the shops, but now that they're there, I do.’ Participant 2·04, female, 13years.
This was confirmed by observations of pupils in the morning before school hours shopping in grocery outlets near to their schools.
Other participants described the ready availability of cheap unhealthy foods which could be ordered easily online and delivered to home:
‘Like a click of a button and you already have unhealthy foods, but just the thought of eating healthy seems a lot harder because they make it seem like it isn't easy to get healthy foods.’ Participant 4·01, male, 11years.
Some pupils showed awareness of how food producers targeted teenagers through marketing:
‘… they [food companies] know what they're doing. They target people our age and know how to draw us in.’ Participant 2·03, female, 13years.
School environments
School environments received less emphasis in pupils’ responses, but researcher observations illustrated the challenges in implementing healthy food policies for inner city schools in deprived areas. For example, despite policies that disallow sugar-sweetened drinks and unhealthy snacks, pupils were observed to be hiding sweets, crisps and large bottles of sugary drinks in their school bags. Although schools conduct random searches of pupils’ bags upon entering school grounds, pupils appear to know how to avoid being checked. One pupil even reported how other pupils sold prohibited fizzy drinks on the school premises:
‘It's the school's fault. People can't bring fizzy drinks or juice to school, but they [pupils] sell it here’ Participant 1·02, male, 13y.
Skipping lunch at school was common, labelled by pupils as ‘not important’ and often substituted with snacks. Pupils were observed to be rushing in and out of the canteen so as to maximise their break time in the playground. Pupils also mentioned avoiding long lunch lines and choosing fast-food establishments or microwaveable foods instead of school meals or packed lunches. This ambivalence towards regular mealtimes is a challenge for intervention and could set up lifelong patterns of unhealthy nutritional behaviour. Meal skipping and as noted earlier, breakfast skipping, in particular, is related to cardio-metabolic health and childhood obesity.
Food literacy. Food literacy levels varied. Among some adolescents the connection between body physiology and food choices was often misguided, for example, one participant stated ‘…[you] need sugar in your belly for energy…healthy food has less sugar, it makes you weaker’ (participant 3·02, female, 12 years). Others acknowledged that fruits have ‘healthy sugars’ and make for a good dessert substitute. Some spoke about replacing white rice with brown rice, but the most common reasoning behind this argument was that brown rice ‘has other things in it’. Another notable feature of pupils’ responses was a lack of awareness of wider issues such as how food choices are influenced by wider environmental or societal contexts. These findings strongly support a multi-level multi-component intervention approach that straddles family, schools and communities to promote nutritional self-regulation among adolescents.
Urban living and adolescent nutrition in globalised cities
Improvements in national incomes and life expectancies globally have been accompanied by striking increases in social disparities, urbanisation and globalisation of risky exposures for global transitions in nutrition(Reference Popkin69). Young people are experiencing dramatic changes in opportunities and constraints in low- and middle-income countries. Our global health projects span countries of widely divergent cultural, socio-economic and political contexts including Guyana and Saudi Arabia. Guyana, for example, is the third poorest country in the Western hemisphere, with 55 % of its population living below the poverty line. Non-communicable diseases are a significant public health problem in the country and in the Caribbean region. Overweight and obesity (19 %) and underweight (8 %) contribute to the burden of childhood malnutrition(70). The Kingdom of Saudi Arabia, conversely, is a high-income Islamic country in the Gulf that has experienced alarming rises in childhood/adolescent obesity in the 2000s, such that about one-third of children/adolescents are overweight/obese by adolescence(Reference Almughamisi, George and Harding71). Our feasibility studies focus on exploring how to strengthen families, schools and communities, and on working with policymakers and practitioners to acquire, interpret and eventually use the research evidence for the physical and mental well-being of young people.
Despite different socio-political contexts, our mixed methods of developmental studies reveal notable commonalities across London, UK, Georgetown, Guyana and Jeddah, Saudi Arabia. As in some parts of London, markets in Guyana are a focal point for weekly shopping. The pictures illustrate the abundance of fruit and vegetables but affordability and availability have reduced over the years(Reference Miller, Yusuf and Chow72), with urbanisation in Guyana significantly affecting local supplies. Despite the contextual differences, the results of our concept mapping workshops with secondary school children in all three countries highlighted some generic issues across the different settings for nutrition interventions. There has been a shift in diets with increases in eating away from home, access to fast foods, low fruit and vegetable intake, and lack of physical activity opportunities in school curricula. Reports of consumption of fast foods resonated with those we heard from London's adolescents, for example in Jeddah adolescents reported that ‘fast food is tasty, easy to obtain’ and ‘healthy food is limited in the mall’, and in Guyana ‘too much unhealthy snacks’ and ‘not having enough vegetables’. Issues around breakfast skipping were also correspondent with reports of ‘limited time to have breakfast’ (Jeddah), ‘not having a hot cup of tea every morning because of trying to make it to school on time in traffic’ (Guyana). The use of mobile technology was prevalent across all of these settings, and mobile applications and social media were cited as important potential modes of delivery for nutrition interventions. The level of health-promoting activities in schools varied with the fewest activities in Jeddah, despite being the most affluent. Unlike London and Georgetown, mosques were not considered appropriate for the delivery of nutrition interventions as usage is for religious activities. Partnership working differed with strongest central government involvement, i.e. the Ministry of Education, in Guyana, although this is the most economically unstable country of the three. A sustainable school-based programme seemed most feasible, however, in Jeddah where the prevention agendas of all partners appeared to coalesce.
Conclusions
In summary, our studies informed our understanding of the contextual drivers for changes in dietary habits among young people living in London in families, schools, neighbourhoods, and faith-based organisations. Our developmental studies also gave detailed insights of the challenges and opportunities for partnerships with places of worship and other sectors for prevention and the need for advanced methodologies in this area.
We are applying the learning from our ongoing studies which use mixed methods and pragmatic as well as realist evaluation, to develop the design of follow-on studies, with programme adaptability being a key consideration to suit different socio-cultural contexts. For example, the Health Eating and Active Lifestyles for Diabetes study uses extensive community engagement with African and Caribbean type 2 diabetes patients in London to continually adapt its design and theory of change to optimise reach. The Congregations Taking Action against non-communicable diseases study in South America and the Caribbean is a system intervention that is exploring how best to integrate places of worship into the primary health care system to benefit those most at risk. Diverse challenges and opportunities for feasibility and sustainability are being mapped and tested as the intervention is implemented. The Children and Young People's Health Partnership intervention study in South London aims to shift healthcare towards community settings and bring prevention and health promotion, including nutrition, into responsive healthcare in all settings.
There are significant health gains for both physical and mental health to be had from addressing intersections of inequalities (e.g. deprivation, racism, food dense neighbourhoods). Our findings signal opportunities for cross-sectoral engagement which could lever benefits across several outcomes, including healthy nutrition, with an emphasis on the translation of proven strategies to reach young people from vulnerable communities.
Acknowledgements
For the DASH study, we acknowledge the invaluable support of participants and their parents, the Participant Advisory Group, schools, civic leaders, local GP surgeries and community pharmacies, the Clinical Research Centre at Queen Mary University of London, the Clinical Research Facility at University College Hospital, the survey assistants and nurses involved in data collection, the Primary Care Research Network, and Professors Sanders and JKC at the Diabetes and Nutritional Sciences Division at King's College London for hosting the feasibility study. We also thank those who contributed to our King's and Communities for Youth Health Research programme including members of the Black Majority Churches, local stakeholders, representatives from local Public Health Authorities and, importantly, school and adolescents from diverse communities in London, Saudi Arabia and Guyana.
Financial Support
The DASH study was funded by the Medical Research Council (10·13039/N4 501100000265, MC_U130015185/MC_UU_12017/1/ MC_UU_12017/13) North Central London Consortium and the Primary Care Research Network. The King's and Communities for Youth Health developmental studies were supported by the King's Together Multi & Interdisciplinary Research Scheme.
Conflicts of Interest
None.
Authorship
S. H. is the Principal Investigator of DASH, led on the analysis and drafted the first version of the manuscript. M. M. and L. G. oversaw the collection of the dietary data on DASH. U. R. designs and conducts the qualitative data collection and analysis for DASH and the CONTACT study and assisted in the analysis and write up of all qualitative data. M. O. K., S. H., C. E. oversaw the conduct of the London and Guyana developmental studies, recruitment of schools, collection and analysis of data. The Kings and Communities for Youth Health study was designed by S. H., M. O. K., A. D., T. G., I. W. and K. C. Some of this formed MSc and MPH dissertations for P. H., C. A., K. C., G. O. D., E. C. The study in Jeddah is part of the doctoral studies of M. A. All authors contributed to redrafting and critical review of the manuscript.










