Introduction
Epilepsy is the commonest of neurological disorders. A primary care trust (PCT) of 100 000 patients is likely to contain 400–800 patients with active epilepsy (Hauser and Kurland, Reference Hauser and Kurland1975). Although the overall prognosis is good, 25% of patients have a refractory condition (Annegers et al., Reference Annegers, Hauser and Elveback1979) that adversely affects their quality of life (Jacoby et al., Reference Jacoby, Baker, Steen, Potts and Chadwick1996) and life expectancy (Lahtoo et al., Reference Lahtoo, Johnson, Goodridge, MacDonald, Sander and Shorvon2001).
Previous research and audit have established that (a) the process of care of people with epilepsy has been poor (Clinical Standards Advisory Group (CSAG), 2000); (b) there may be a link between the delivery of care and adverse outcomes including sudden unexpected death in epilepsy patients (Nashef and Brown, Reference Nashef and Brown1997); and (c) there are clear advantages of specialist review. Two studies, using different methods, have demonstrated that a proportion of patients with apparent refractory epilepsy, can, if properly diagnosed and classified, achieve remission when treated appropriately (Smith et al., Reference Smith, Dafala and Chadwick1999; Leach et al., Reference Leach, Lauder, Nicolson and Smith2005).
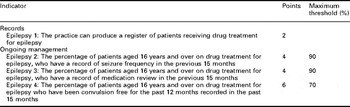
Improvements in the process of care of patients with epilepsy are recommended in government-sponsored reports (CSAG, 2000) and national guidelines (Scottish Intercollegiate Guidelines Network (SIGN), 2003; National Institute of Clinical Excellence (NICE), 2004). The New General Medical Services Contract (2003) included epilepsy as a core quality indicator (Table 1) and the NICE guidelines state that ‘if seizures are not controlled and/or there is diagnostic uncertainty or treatment failure, individuals should be referred to tertiary services for further assessment’ (NICE, 2004:2).
Table 1 The quality indicators for the New GP Contract
In the Chester City audit, we reported that educational intervention can improve review rates and documented remission rates, but we also pointed out that a significant proportion of patients (45%) with poor seizure control were still not receiving shared care (Minshall and Smith, Reference Minshall and Smith2008).
In the rural practices outside Chester, the timing of the introduction of the New Contract had a confounding effect upon the potential impact of our educational intervention. Therefore, for those practices, we have focussed upon the outcomes of subsequent very high review rates with particular reference to patients with drug-resistant epilepsy.
Methods
First audit
Between September 2003 and January 2004, the records of 388 patients, of all ages, with a diagnosis of epilepsy, who were receiving repeat prescriptions for anti-epileptic drugs, were reviewed.
Interventions
The results were summarised in a letter sent to the senior partner of each practice. This included demographics, review patterns, documented remission at that time, and diagnosis. The information was also summarised on a computer template for each patient. The latter concluded with a specific recommendation: (a) patient needs general practitioner's (GP) review or (b) consider specialist referral, subdivided into patients in prolonged remission – consider drug withdrawal, diagnostic doubt, and poor seizure control.
This was supplemented by a half-day educational session in March 2004, including an overview of the diagnosis and management of epilepsy, and direct feedback on the audit findings for the 13 practices involved.
The New GP Contract came into force in April 2004.
Re-audit
Each practice was revisited four years after the initial audit. If a referral, or intervention, was made in the first consultation for epilepsy, which related to an issue highlighted by the audit, it was assumed to be due to the audit and recorded accordingly.
Statistics were analysed using Graphpad computer software, using χ2, proportional χ2, and Wilcoxon matched-pairs signed-ranks test.
Results
Re-audit
A total of 121 patients who did not complete the audit cycle were excluded. There had been 40 deaths, with one attributable to epilepsy. Fifty-nine patients had left their practice. Eight patients had treatment stopped under hospital supervision, all had at least six months follow-up and none had relapsed. Fourteen had stopped treatment without medical supervision. Twelve of these patients had definite epilepsy, one patient, who had never had a seizure, had been receiving prophylactic medication after a head injury, and one patient had their diagnosis changed to migraine. All had stopped treatment at least six months before the end of the audit, and none had a documented relapse.
Table 2 displays a significant improvement in annual review rates, and Table 3 reveals that this change occurred in the year immediately after both the educational intervention and the introduction of the New Contract and has been sustained over the period of the audit.
Table 2 Summary of findings from the first audit and re-audit
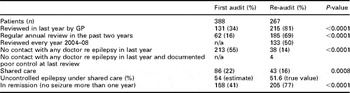
GP = general practitioner; n/a = not applicable.
Table 3 Number of patients reviewed and corresponding statistical difference year on year
ns = not significant.
Shared care and refractory epilepsy
In all, 43 of the 267 (16%) patients were received shared care compared with 86 of 388 (22%) before April 2004 (P = 0.0008). Of the 86 patients under shared care, 39 were under the age of 20 years and received paediatric specialist care, leaving 47 adult patients under shared care. If we assume that 25% of patients have intractable epilepsy, (Annegers et al., Reference Annegers, Hauser and Elveback1979) then 87 patients of the remaining 349 over 20 years of age should be under shared care. Therefore, only 54% (47 of 87) of the adult patients likely to have refractory epilepsy were receiving shared care. In the re-audit, there were actually 62 of 267 (23%) patients with uncontrolled epilepsy, of whom 32 of 62 (51.6%) patients were received shared care.
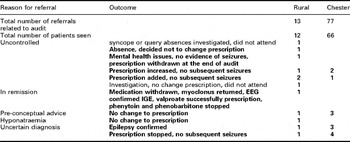
Referrals
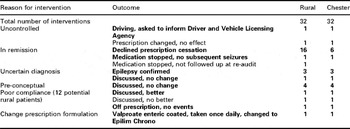
In all, 13 of 302 (4%) patients were referred because of issues highlighted in the first audit. Eight of 40 (20%) adults with refractory epilepsy, who were not already receiving secondary care, were referred. The outcomes of all referrals (10 positive in bold) are described in Table 4 with comparisons to the Chester audit. Three patients entered remission after treatment change, one relapsed after drug withdrawal but re-entered remission on simpler regime, and two patients, previously misdiagnosed, had medication stopped.
Table 4 Referrals related to audit and outcomes
Practice interventions
Thirty-two patients had interventions in practice related to the audit (Table 5), and there were 29 positive outcomes in bold.
Table 5 Interventions in practice related to the audit
Deaths
An 86-year-old lady was found dead in her bathroom with head and eye injury, attributed to epilepsy as a possible cause on death certificate. She had documented poor control, had been admitted in 2005 and 2006 with seizures, and was not under shared care. She had been reviewed for her epilepsy by a GP in 2005, was not seen in 2006, saw a district nurse in 2007, and a health-care assistant in 2008.
Discussion
Government-sponsored reports (CSAG, 2000) have emphasised the need for improvements in the process of care of patients with epilepsy. Published guidelines (SIGN, 2003; NICE, 2004) include explicit standards of care for the diagnosis, management, and follow-up of patients with epilepsy. The role of the GP is described as ‘pivotal’, with audit being an essential tool in the care of patients with epilepsy (CSAG: 35).
The Chester City and Cheshire West epilepsy audit is a long-term project that has previously reported improvements in annual review rates and documented remission rates (Minshall and Smith, Reference Minshall and Smith2008) and a reduction in the inappropriate use of therapeutic drug monitoring (Minshall et al., Reference Minshall, Berry and Smith2011). We believe that these changes were at least partly attributable to the educational intervention inherent in the audit process.
The Chester practice audit, however, found that 45% patients with refractory epilepsy were not being referred for specialist review. In the rural practice, audit GPs received their educational session, and individualised patient feedback, only one month before the New Contract commenced. NICE guidelines were published six months later. Therefore, these practices were in a position to optimise the care of their patients.
There was a dramatic increase in the proportion of patients reviewed and in the documentation of remission. These changes occurred immediately after the New Contract and have been sustained. The first audit estimated that 47 of 87 (54%) patients with refractory epilepsy were receiving shared care. After the intervention, only 8 of 40 (20%) patients were referred for specialist opinion, and the re-audit indicates that only 32 of 62 (52%) patients recorded as having active epilepsy are receiving specialist advice.
Guidelines clearly suggest patients who have uncontrolled epilepsy should be under shared care (NICE, 2004). GPs are reviewing these patients now, so why are they not being referred?
Some patients will choose not to be referred because they have had poor experiences with hospital care, or have previously been told that nothing further can be done and assume that this situation has not changed. In fact, many patients have never seen a specialist and the advice previously received is likely to be inaccurate (Leach et al., Reference Leach, Lauder, Nicolson and Smith2005). Inevitably there are some patients with whom all reasonable therapeutic options have been tried.
Another possibility is the quality of communication between patients and their GP. In all, 50% of patients with epilepsy have anxieties about their condition, which they do not discuss with their GP (Cooper and Huitson, Reference Cooper and Huitson1986); 40% do not find their GP easy to talk to about their epilepsy (Jacoby et al., Reference Jacoby, Baker, Chadwick and Johnson1993).
The barrier may be the GP, who is unaware of the different options now available therapeutically or surgically. Many GPs perceive epilepsy to be a condition with complex management and that they lack sufficient knowledge of the condition (Brown et al., Reference Brown, Betts, Chadwick and Hall1993). Two-thirds of GPs acknowledged difficulties in diagnosis, counselling, and the prescribing of drugs (Taylor, Reference Taylor1987). Many GPs consider their knowledge of epilepsy to be inadequate (Thapar et al., Reference Thapar, Stott, Richens and Kerr1998). The patient may have their epilepsy wrongly classified and hence be on inappropriate medication (Marson et al., Reference Marson, Al-Kharusi, Alwaidh, Appleton, Baker, Chadwick, Cramp, Cockerill, Cooper, Doughty, Eaton, Gamble, Goulding, Howell, Hughes, Jackson, Jacoby, Kellett, Lawson, Leach, Nicolaides, Roberts, Shackley, Shen, Smith, Smith, Smith, Vanoli and Williamson2007a; Reference Marson, Al-Kharusi, Alwaidh, Appleton, Baker, Chadwick, Cramp, Cockerill, Cooper, Doughty, Eaton, Gamble, Goulding, Howell, Hughes, Jackson, Jacoby, Kellett, Lawson, Leach, Nicolaides, Roberts, Shackley, Shen, Smith, Smith, Smith, Vanoli and Williamson2007b); are GPs aware of these important studies?
PCTs have been pursuing a policy to encourage discharge and hence avoid unnecessary follow-up and the cost that incurs. Although this is perfectly reasonable for patients with epilepsy in remission, it should not be applied to those with drug-resistant epilepsies.
The benefit of specialist review has been well established. Smith et al. (Reference Smith, Dafala and Chadwick1999) reported that 16 of 80 (20%) patients, referred with refractory epilepsy, were rendered seizure free after specialist assessment. Whereas four had surgery, and another four were treated with new drugs, eight of these patients achieved remission because of manipulation of conventional treatment. Seven of these had unrecognised idiopathic generalised epilepsy and had never received valproate. Nearly a decade later, Leach et al. (Reference Leach, Lauder, Nicolson and Smith2005) assessed 275 patients who were not going to be referred. In all, 17 of 55 (31%) patients with an active epilepsy (10 partial, seven generalised) achieved at least a one-year remission, and for 15 this was a first ever remission. None of these patients had surgery. Whereas nine benefitted from the addition of new drugs, the other eight were reclassified and treated with conventional drugs. In the rural practices 3 of 7 (43%) patients and in Chester 3 of 36 (8%) patients with uncontrolled epilepsy achieved remission after specialist review; of these six patients, none had surgery, and one was rendered seizure free after reclassification (Table 6).
Table 6 Summary of the three studies reviewing patients with refractory epilepsy
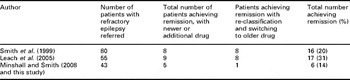
Therefore, although it is true that patients with truly drug-resistant epilepsy rarely achieve remission, there are other patients with the label of refractory epilepsy who simply need proper classification and appropriate treatment. In a PCT of 100 000 patients with an average population of 600 patients with epilepsy; we calculate 150 (25%) will have resistant epilepsy, of which 72 (48%) will not be under specialist care. Sixteen from this group (22% average of the three studies above) will have the potential to be rendered seizure free. With the UK population equating to approximately 61 million, then 9760 patients might become seizure free with appropriate review.
A national sentinel audit of 812 epilepsy-related deaths suggests that there are shortcomings in the care of people with epilepsy in the United Kingdom (Hanna et al., Reference Hanna, Black and Sander2002). Forty-two per centage of deaths were thought to be potentially preventable. It is therefore disappointing to find a death attributable to epilepsy within this cohort – a patient with clearly uncontrolled epilepsy, not under specialist care and not having been reviewed by her GP for three years with regard to her condition before her death.
In this study, the overall level of shared care dropped significantly. One might speculate that neurologists were reviewing some patients annually but not altering treatment, for those whom they knew were not having primary care reviews. With the introduction of the New Contract, these patients were discharged to their GP.
Since the introduction of the New Contract, a higher proportion of patients with epilepsy are reviewed and the recording of remission is rewarded. However, neither refractory epilepsy nor lack of specialist input is currently highlighted. Patients in these categories should be prioritised for referral and, perhaps, reward should be related to objective patient benefit.
We recommend that new satisfaction surveys should be performed to determine whether the care of patients with epilepsy has improved since the New Contract was introduced. GPs too should be consulted about whether they feel better equipped to care for their patients with epilepsy or whether their knowledge is just as ‘inadequate’ as it was over ten years ago.
Acknowledgements
Approval for the study was obtained from the South Cheshire Local Research Ethics Committees Audit no. 49. The authors have no conflict of interest to declare. The authors thank Dr Richard White, Consultant Neurologist, Walton Centre for Neurology, and Dr Jim Finnerty, Consultant Physician, Countess of Chester Hospital, for statistical support.








