Background
Norway has 4.6 million inhabitants, 55 public hospitals, 41 052 nursing home beds and 1796 beds in old people's homes, 96.8% of nursing home beds are in single rooms and 43.3% of all deaths (total 41 342) are in nursing institutions (Statistics Norway, 2010). The health care system is split in first- and second-line services. The second line contains the 55 hospitals and specialist services (included private specialists). Second line is administered and financed directly from the state. First-line services are administered and financed by the municipalities (n = 431). First line covers general practice services, mother and child care, home care and nursing homes (n = 900).
The high consumption of psychopharmaceuticals in nursing homes has been emphasized in a number of studies and the prevalence of psychoactive drugs has been well documented earlier, but some years ago (Ruths et al., Reference Ruths, Straand and Nygaard2001; Ranhoff and Brors, Reference Ranhoff and Brors2005; Selbaek et al., Reference Selbaek, Kirkevold and Engedal2008). Few authors have placed the emphasis on treatment differences between nursing homes and the general differences in medication of patients suffering dementia as opposed to non-demented nursing home patients (Nygaard et al., Reference Nygaard, Naik, Ruths and Straand2003).
The high drug consumption among elderly people over 65 is problematic. On average, the elderly nursing home residents in Bergen had five drugs each some years ago (Nygaard et al., Reference Nygaard, Naik, Ruths and Straand2003). In a study of drug consumption at five smallish nursing homes in Norway, drug consumption was found to be greatest within drugs for ‘digestive organs and metabolism’, ‘blood and blood-forming organs’, ‘heart and circulation’, ‘urogenital system and sex hormones’ and ‘nervous system’ (Nygaard, Reference Nygaard2001).
Polypharmacy has usually been defined as the use of five or more drugs (Hunskår, Reference Hunskår2003). Polypharmacy is the most important risk factor for drug side effects and increases the risk of drug interactions (Fastbom, Reference Fastbom2001; Johnell and Klarin, Reference Johnell and Klarin2007).
The elderly are particularly vulnerable to the side effects of psychopharmaceuticals, and anticholinergic burden involves a risk of delirium (Turnheim, Reference Turnheim2000). Use of long-acting benzodiazepines can be one of the causes of falls in patients over 65 years of age (Blain et al., Reference Blain, Blain, Trechot and Jeandel2000). Concurrent use of three or more psychopharmaceuticals has been found to be associated with the risk of falling (Gales and Menard, Reference Gales and Menard1995).
In the BEDNURS (The Bergen district nursing home) study, 23% of the patients suffering from dementia, nursing home population in Bergen, Norway, were found to be on antipsychotics (Ruths et al., Reference Ruths, Straand and Nygaard2001). Double-blind studies have shown little symptom reduction connected with the use of antipsychotics as compared with placebo (Druckenbrod et al., Reference Druckenbrod, Rosen and Cluxton1993; Jeste et al., Reference Jeste, Blazer, Casey, Meeks, Salzman, Schneider, Tariot and Yaffe2008). Of 27 patients, 23 fare well or better without antipsychotics (Ruths et al., Reference Ruths, Straand and Nygaard2001). In particular, conventional antipsychotics are associated with extra pyramidal side effects, like drug-induced Parkinsonism (Tison et al., Reference Tison, Lecaroz, Letenneur and Dartigues1999; Saltz et al., Reference Saltz, Woerner, Robinson and Kane2000). Both atypical and conventional antipsychotics are associated with a significantly greater mortality risk than placebo. The greatest increase in mortality occurred among people taking higher (above median) doses of conventional antipsychotic medications (Wang et al., Reference Wang, Schneeweiss, Avorn, Fischer, Mogun, Solomon and Brookhart2005).
We wanted to pinpoint any differences in treatment between participating nursing homes, investigate which drugs are currently prescribed most frequently for long-term patients in nursing homes, estimate prevalence of administration for the following drug groups: neuroleptics, antidepressants, antidementia agents, opioids and the neuroleptics/anti-Parkinson's drug combination, and study comorbidity correlations. We also wanted to study differences in the administration of medication for patients with reduced cognitive functions in relation to patients with normal cognition.
The study was approved by the Regional Ethics Committee of Western Norway.
Methods
Bergen has ∼250 000 inhabitants and 37 nursing homes (2300 beds). Bed numbers range from 20 to 189. Seven nursing homes participated in this study. Participating nursing homes were selected on the basis of a relative similarity of functions, county ownership (no private institutions) and physician staffing. Nursing home characteristics are presented in Table 1. Only long-term patients (n = 513) were included. Sufficient information was available for all patients and they were all included in the analyses.
Table 1 Nursing home characteristics: characteristics of the seven nursing homes with long-term patients participating in the city of Bergen, Norway, in 2008 (n = 513 long-term patients)
SD = standard deviation; SEM = standard error mean.
1Kruskal–Wallis test.
2Pearson χ 2 test.
3–4Wilcoxon test.
5–6Pearson χ 2 test.
Information about the patients was gathered during the period between March and April 2008. Twenty-four medical students conducted the data collection, which consisted of copying medication cards (information about drug names, if regular or as-needed, prescription and dosage), weighing, details of any stroke suffered and degree of cognitive impairment. Electrocardiography was conducted to diagnose atrial fibrillation and a standardized set of blood samples was analyzed.
In order to group the material into patients with/without cognitive impairment, we used the Berger scale (Berger, Reference Berger1980) and recorded patient information. A caregiver who knew the patient decided between six ‘level descriptions’ of cognitive impairment, thus rating the degree of severity as a score from 0 to 6. The method was validated by comparing the extent to which drugs for dementia were given to patients scoring above 0, giving a 95% overlap.
The recorded data were keyed into Excel and the drugs were coded according to the Anatomical Therapeutic Chemical (ATC) Drug Register (Skrbo et al., Reference Skrbo, Begovic and Skrbo2004). For each drug, the students punched in the full ATC code, dosage, number of times per day given, total daily dosage and whether regular/as-needed. For the psychoactive drugs, which are part of the comparison between institutions, Defined Daily Dosages (DDDs) were registered (except for opioids being part of codine–paracetamol combination drugs). To compare the total use of psychoactive drugs (hypnotics, anxiolytics, antidementia drugs, neuroleptics and opioids) between institutions, we used the calculated parameter: [(Drug DDD) × (% of patients in institution on drugs of drug-class)]. Straight counts were performed in Excel, but for statistical analyses JMP 8 was generally used. Means and standard deviations (SD) are reported. To analyze differences in the average between multiple groups for continuous data, the Tukey–Kramer (Honestly Significant Difference) multiple comparison procedure was used as a parametric method and the Kruskal–Wallis analysis of variance (ANOVA) as a non-parametric method. For analyzing ordinal and nominal data, the Pearson χ 2 test was used and the results are reported as odds ratios (OR) with 95% confidence intervals (CIs). All tests were done at significance level 0.05. To search for factors with potential impact on prescription rates, we conducted a multinomial logistic regression analysis, and to adjust for differences in patient and nursing home characteristics we performed a two-way ANOVA.
Results
The nursing homes were comparable in terms of nursing staff (county standard), financing (public, not private) and residents’ gender distribution (Pearson χ 2 test), Table 1. Two institutions had a significantly lower mean age (Tukey–Kramer) than the others, nursing homes F and G. Median age was between 82.7 and 87.3 years for all institutions.
Medications in general
The total number of prescriptions recorded was 3468. The average number of regular drugs was 6.1 per patient (n = 513, SD = 3.3, range: 0–20). Classified according to principal ATC groups (Skrbo et al., Reference Skrbo, Begovic and Skrbo2004), the three most frequent were drugs for the ‘nervous system’, ‘digestive organs and metabolism’ and ‘heart and circulation’ (Table 2). Paracetamol was the most frequently prescribed drug (regular and as-needed) with 5.7% (n = 197) of the total number of prescriptions (n = 3 468), administered to 38.4% of the patients.
Table 2 Prescriptions per ATC main groups: ranking of the number of prescriptions according to the classification of the ATC Drug Register among long-term patients at seven nursing homes in Bergen, Norway (n = 513)
ATC = anatomical therapeutic chemical.
The average number of as-needed drugs per patient was 3.8 (n = 513, SD = 2.2, range: 0–14).
Prescriptions of psychoactive drugs by way of regular or as-needed prescriptions are shown in Table 3. Of 513 patients, 24.4% (125) were regularly given one or several neuroleptics, 9.7% (50) of the patients (n = 513) had neuroleptics by way of an as-needed prescription and 6.4% (8) of the patients on regular neuroleptics (n = 125) were using two different ones regularly. Risperidone was the most frequent antipsychotic drug, and haloperidol was the most frequent as-needed neuroleptic.
Table 3 Psychoactive drugs: ranking of the most prescribed drugs affecting the central nervous system among 513 long-term patients at seven nursing homes in Bergen, Norway
ATC = anatomical therapeutic chemical.
Of all, 14.6% (75) of the patients (n = 513) were on opioids (N02A) by way of regular medication and 28.7% (147) by way of an as-needed drug, and 41.5% (215) of the patients received antidepressants as regular medication.
On the basis of our figures, prevalences of long-term patients in nursing homes being prescribed psychoactive medication were as follows: neuroleptics regular 244/1000 and as-needed 98/1000; antidepressants regular 419/1000; anxiolytics regular 220/1000 and as-needed 415/1000; and opioids regular 146/1000 and as-needed 287/1000.
Differences among the nursing homes
We discovered some significant correlations in the total material that could bias the differences between nursing homes. Morphine is given less in the nursing home where the physician was a specialist (Pearson, P = 0.0097) as were neuroleptics (Pearson, P = 0.0139). Neuroleptics were given more to patients suffering from dementia (P = 0.0259); fewer benzodiazepines were given with increasing age (P = 0.0066); the longer the stay, the fewer the antidementics that were given (P = 0.0001); and patients on antidepressants had a lower age (P = 0.0002). However, analyzing differences among institutions, correcting for these factors and for age and sex, impacted only slightly on some P-values, although not on the total picture.
We discovered significant differences between nursing homes as a percentage of patients on drugs within the actual ATC main group. Differences were highly significant statistically for morphine (Pearson χ 2 test, P = 0.0117), neuroleptics (P = 0.0026) and antidepressants (P = 0.0010), Table 4. Comparison of drug use among the patients with reduced cognitive functions by institution is demonstrated in Figure 1. Differences between institutions were significant for neuroleptics (Pearson χ 2 test, P = 0.0016) and antidepressants (P = 0.0010) but not for antidementics (P = 0.566).
Table 4 Institution differences, psychoactive drugs: proportions of long-term patients on one or more regular and as-needed psychoactive drugs prescribed in seven (A, B…) nursing homes in Bergen, Norway, 2008
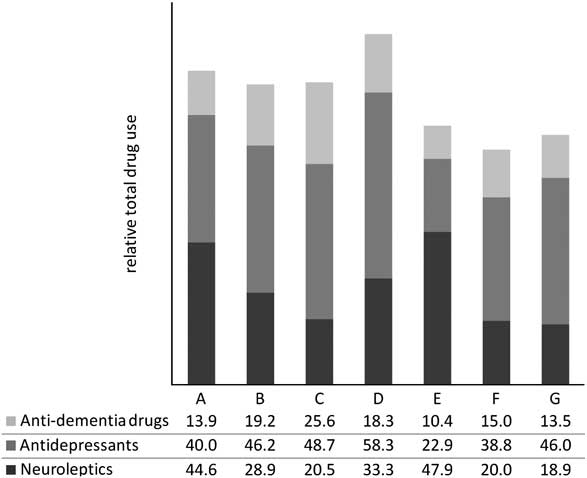
Figure 1 Use of three different psychoactive drugs among long-term demented patients at seven nursing homes (A, B…) in Bergen, Norway. Differences between institutions are significant for neuroleptics (Pearson χ 2 test, P = 0.0016) and antidepressants (P = 0.566). Differences are not impacted by corrections for age and sex.
The addition of DDDs and calculating total drug use per institution even increased the differences, and the differences were highly significant for all drug classes, Table 5 and Figure 2.
Table 5 Total psychoactive amount (DDD): differences of regularly prescribed psychoactive drugs in seven nursing homes in Bergen, 2008, expressed by the parameter (total DDD per drug class prescribed) × (per institution percentage of patients on drugs of actual class)
DDD = Defined Daily Dosages.
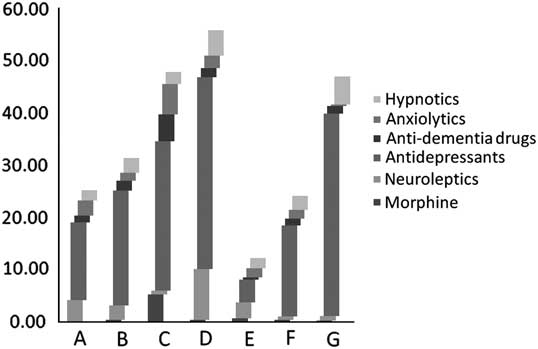
Figure 2 Total use (percentages × Defined Daily Dosage – DDD) for long-term patients on regularly prescribed psychoactive drugs in seven (A, B…) nursing homes in Bergen, Norway, 2008. Also see Table 5.
Neuroleptics – Parkinsonism
Five out of 18 patients being given drugs for Parkinsonism were also on neuroleptics. One of the patients was a psychiatric patient on biperiden. One was being given quetiapine, which is an atypical neuroleptic not contraindicated in the case of Parkinsonism. Three could be characterized as possibly harmful medications. On the basis of our material, the prevalence of current medication was 2/1000 among all long-term nursing home patients.
Medication for patients with impaired cognition
Patients with impaired cognitive function were prescribed significantly fewer regular drugs than patients without impairment. The average for patients without impairment was 7.1 drugs (n = 130) and for the patients with impaired cognitive functions 5.7 drugs (n = 381, Wilcoxon test, P < 0.0001). There was no difference in the number of as-needed drugs for the two patient groups. Among patients with impaired cognitive functions, 21.0% had suffered stroke, and among patients without impairment 32.0% (OR: 1.76, 95% CI: 1.13–2.75). In general, there was a tendency to lower the prescription rate of all cardiovascular drugs for the patients with reduced cognitive functions, significantly for angiotensin converting enzyme inhibitor or angiotensin II receptor blocker – ACEI/A2B (OR: 1.78, 95% CI: 1.07–2.94) and diuretics (OR: 1.77, 95% CI: 1.18–2.66). Neuroleptics were more frequently prescribed to patients with reduced cognitive functions (31%/21%, OR: 0.58, 95% CI: 0.36–0.94). ProBNP (brain natriuretic peptide) was significantly higher in the patient group without cognitive impairment (Wilcoxon, P = 0.0011). No such differences existed for atrial fibrillation (Pearson χ 2 test, P = 0.137) or renal function (Estimated Glomerular Filtration Rate, Wilcoxon, P = 0.1918). Significant negative correlation was found between age and weight (Pearson χ 2 test, P < 0.0001), and the average age among patients with reduced cognitive functions was lower than the rest of the population (Wilcoxon, P = 0.0407). Average patient weight was 62 kg, half of all patients (n = 513) having weight loss last 30 days.
Associations
With regard to comorbidity, we did not find any associations with the use of neuroleptics and stroke suffered, or associations between neuroleptics and patient weight or weight loss/30 days. Use of antidepressants was positively associated with patient weight (Wilcoxon test, P = 0.0037). No associations for benzodiazepines or hypnotics were found with stroke, weight or weight loss.
Discussion
The number of drugs given to nursing home patients in Bergen is higher than the number given 10 years ago. Considerable treatment rate differences existed between institutions. Patients with cognitive problems were prescribed fewer drugs in general but more neuroleptics. Except for significantly higher weight in patients on antidepressants, none of the other clinical factors tested for associations with psychoactive drugs was significant.
Limitations of the study
The role of nursing homes in the delivery of social and health care services differs between, as well as within, countries. Nursing homes in many countries are managed as part of social care. In Norway, nursing homes are regulated as a health care service. These differences may influence the health issue landscape and composition of staff. Thus, comparisons and generalizations based on our findings should be done with care.
For most planned purposes, we consider our material valid and robust with regard to both sample size and tested parameters. However, the size of the material may be too small to calculate the prevalence of rarer diagnoses/drugs. A weakness of our study is that comparisons between diagnosis and drug treatment cannot be performed.
The simple test we used to decide whether or not patients had reduced cognitive functions can be questioned (Berger, Reference Berger1980). Using Minimal Mental Score was beyond project resources. Our method was to a certain degree validated, however, by comparing the extent to which dementia drugs were given to patients scoring above 0 (reduced cognitive functions), giving a 95% overlap, and to a certain degree by medical record data. We thus found our method sufficient for the purposes of the study.
Earlier research
We found good concordance with results from previous studies in terms of the drug groups most frequently prescribed (N, A, C, B, R; Nygaard, Reference Nygaard2001). In our material, ATC group G (urogenital system and sex hormones) was used less than previously demonstrated. References to the use of these drugs are some years old, and drugs and diagnostics have evolved, which is probably the reason for this.
The proportion of patients taking neuroleptics was slightly higher than previously demonstrated in Bergen nursing homes (23%, 2001). The decreasing use of neuroleptics in nursing homes discussed by other authors has not been verified (Ruths et al., Reference Ruths, Straand and Nygaard2001). This is surprising, given research showing the lack of effect of neuroleptics among patients suffering dementia. Neuroleptics are needed in nursing homes, but for limited periods and for individual patients, and more often than is currently the case. Patients often end up with a regular prescription without any evaluation of the need to pause treatment and take stock after a period of time (Selbaek et al., Reference Selbaek, Kirkevold and Engedal2008).
The use of neuroleptics for patients with Parkinson's is low because of the low prevalence of Parkinson's (5.5%); however, the number of these patients with a drug combination that includes neuroleptics that are contraindicated is probably not negligible.
In our study, the prescription of antidepressants was similar to a comparable study in Bergen in 2001 (Ruths et al., Reference Ruths, Straand and Nygaard2001). An increase was expected. The selective serotonin reuptake inhibitor drugs (SSRIs) are important drugs for the elderly. Even in our study, we found a positive association between SSRI use and patient weight. However, interactions with certain drugs (antiepileptics, neuroleptics, cimetidine and codeine) do exist and they increase the risk of bleeding for patients on warfarin without impacting the International Normalized Ratio. Non-steroidal Anti-inflammatory Drugs together with SSRIs increase the risk of gastrointestinal bleeding (Van Der Steen et al., Reference Van Der Steen, Meuleman-Peperkamp and Ribbe2009).
Weight gain during antidepressant treatment can be either a sign of improvement in patients who have weight loss as a symptom of depression or a drug side effect. However, significant weight gain during the acute phase of treatment or weight gain that continues despite achieving full remission of depressive symptoms is likely to be a side effect of antidepressant treatment. Weight gain is a relatively common problem during both acute and long-term treatment with antidepressants (Fava, Reference Fava2000). In our material, the average patient weight was 62 kg, half of the patients suffering weight loss. The unwanted side effect by antidepressants in a common population may be an advantage among nursing home patients. More research is needed to shed more light on this issue. However, in our study, the lower age among patients with reduced cognitive functions may to a certain degree explain the higher weight in this group, as weight decreased by age, significantly.
The hazard from falls and fractures when on psychoactive drugs is well known (Gales and Menard, Reference Gales and Menard1995; Kiel et al., Reference Kiel, Magaziner, Zimmerman, Ball, Barton, Brown, Stone, Dewkett and Birge2007). In Norway, ∼9000 hip fractures (50% among persons > 85) are treated in hospitals, giving a yearly age-independent incidence of 2/1000 and for the population > 85 ∼9/1000 (Van Der Steen et al., Reference Van Der Steen, Meuleman-Peperkamp and Ribbe2009). In Bergen, yearly 90 hip fractures among 2300 nursing home beds were registered over 12 months, 2006−2007, giving an incidence of 39/1000 (Krüger et al., Reference Krüger, Jansen, Grimsmo, Eide and Geitung2011). The prevalence of hip fractures has also been estimated by other authors (Dobnig et al., Reference Dobnig, Piswanger-Solkner, Roth, Obermayer-Pietsch, Tiran, Strele, Maier, Maritschnegg, Sieberer and Fahrleitner-Pammer2006; Kiel et al., Reference Kiel, Magaziner, Zimmerman, Ball, Barton, Brown, Stone, Dewkett and Birge2007). More differentiation in the use of psychoactive drugs for patients at risk of falling could prove valuable, like patients with/without the ability to walk unaided.
A lower cardiovascular drug consumption by nursing home patients suffering reduced cognitive functions has been reported by others (Nygaard et al., Reference Nygaard, Naik, Ruths and Straand2003). This may reflect a selection effect as the majority of nursing home patients are admitted because of dementia (75–80%), and the others due to somatic illnesses, for example, cardiovascular diseases. However, general cardiovascular risk factors are also risk factors for developing Alzheimer's disease and the combination of cerebrovascular and degenerative causes make up a large proportion of all dementias. That ProBNP was significantly higher among patients without cognitive impairment indicates that morbidity differences may exist between the two groups, in nursing homes, with regard to cardiovascular disease. In contrast, no such differences existed for atrial fibrillation or renal function. The reasons for lower treatment rate among patients in nursing homes with impaired cognitive functions still remain unclear.
Differences between nursing homes
In our study, we have tried to evaluate the present status and have demonstrated sizable differences between the nursing homes when it comes to the use of medications, which cannot be explained by different prevalences alone. This was evidenced by our own research on the association between atrial fibrillation and stroke and warfarin, and it is logical to assume that it obtains for psychoactive drugs as well (same material, different publication). Drug differences and physician staffing have been indicated (Kersten et al., Reference Kersten, Ruths and Wyller2009), but the reasons for such differences are probably multifactorial, as is quality in general. Both employee skills and attitudes probably play a role, as do management, routines, tracking systems and a collaborative work climate. We did not see any bias because of sex, age and staffing differences between nursing homes or when blocking other potentially biasing factors discovered by multiple regression analysis. Calculating the total use of drugs within each drug class using DDDs, increased the differences between institutions, Table 5 and Figure 1. This probably shows that institutions with a high percentage use are also using higher dosages.
Documenting quality status and improving quality in nursing homes is a challenge. Internationally, several quality improvement studies have been undertaken: Nursing homes with a smaller number of beds, operating for profit and having a high level of nursing staff may improve quality (Wan et al., Reference Wan, Zhang and Unruh2006). It has been claimed that marginalization of physicians in the nursing home threatens the overall care of increasingly frail nursing home residents who have medically complex illnesses (Katz et al., Reference Katz, Karuza, Intrator and Mor2009). Medication quality improvement efforts in nursing homes should probably focus on the medications commonly implicated in errors and should continue to discourage or closely monitor the use of medications considered potentially inappropriate in the elderly (Hansen et al., Reference Hansen, Greene, Williams, Blalock, Crook, Akers and Carey2006). A menu-driven incident-reporting system has the potential to enhance quality improvement efforts in nursing homes (Wagner et al., Reference Wagner, Capezuti, Taylor, Sattin and Ouslander2005). In pain management, a multifaceted collaborative intervention proved valuable, involving audit and feedback on pain management, education, training, coaching using rapid-cycle quality improvement techniques and inter-nursing home collaboration (Baier et al., Reference Baier, Gifford, Patry, Banks, Rochon, Desilva and Teno2004). It has been shown that there exists a relationship between ambitious targets and nursing home quality (Baier et al., Reference Baier, Butterfield, Patry, Harris and Gravenstein2009). Implementing small, focused and inexpensive interventions, like monitoring BP controls, can improve quality (Choma et al., Reference Choma, Huang, Dittus, Burnham and Roumie2009).
Simply providing comparative performance feedback may not be enough to improve resident outcomes (Rantz et al., Reference Rantz, Popejoy, Petroski, Madsen, Mehr, Zwygart-Stauffacher, Hicks, Grando, Wipke-Tevis, Bostick, Porter, Conn and Maas2001). Targeting specific drugs in the surveyor's interpretative guidelines as a method of reducing potentially inappropriate medication use does not produce the desired gains in terms of improving the quality of medication use either (Lapane et al., Reference Lapane, Hughes and Quilliam2007).
It is difficult to envisage adequate quality control without the use of modern technology like medical record systems with alarms, statistics and decision-making support in addition to already proven tools for improving the quality of drug use. The effectiveness of decision support tools has been shown in several studies and should be tested in nursing homes (Ornstein et al., Reference Ornstein, Jenkins, Nietert, Feifer, Roylance, Nemeth, Corley, Dickerson, Bradford and Litvin2004; Kawamoto et al., Reference Kawamoto, Houlihan, Balas and Lobach2005).
Conclusions
There are differences in treatment with psychoactive drugs between nursing homes. Treatment differences also exist between patients with/without cognitive impairment but reasons remain unclear. Improvement strategies and more research are needed. The proportion of patients per institution on selected drugs can serve as a feedback parameter in quality systems, but adding DDDs increases differences.
Acknowledgments
We acknowledge all 24 medical students from the Faculty of Medicine and Dentistry at the University of Bergen, personnel at the seven participating nursing homes in Bergen and Dr Bahareh Jouleh. The study was funded by a grant from the Norwegian Research Council.









