Introduction
Anorexia nervosa (AN) is a severe mental disorder that has significant consequences for affected people (Schlegl et al., Reference Schlegl, Quadflieg, Löwe, Cuntz and Voderholzer2014), their relatives (Coomber and King, Reference Coomber and King2013) and public health (Stuhldreher et al., Reference Stuhldreher, Wild, König, Konnopka, Zipfel and Herzog2014). In Europe, ~1–4% of women are affected by AN, with stable incidence rates over the past decade (Keski-Rahkonen and Mustelin, Reference Keski-Rahkonen and Mustelin2016). The physical health impairments associated with AN include cardiac arrhythmias, electrolyte imbalances, renal insufficiency, osteoporosis and severe infections (Agras, Reference Agras2001). Comorbid mental health disorders are frequent with anxiety, and affective disorders being the most common comorbidities (eg, Herpertz-Dahlmann et al., Reference Herpertz-Dahlmann, Müller, Herpertz, Heussen, Hebebrand and Remschmidt2001). The high mortality associated with AN might be attributable to the increased risk for suicide and reasons directly related to the symptoms of AN (Löwe et al., Reference Löwe, Zipfel, Buchholz, Dupont, Reas and Herzog2001; Smink et al., Reference Smink, van Hoeken and Hoek2012; Keski-Rahkonen and Mustelin, Reference Keski-Rahkonen and Mustelin2016).
A brief period of untreated AN and a body mass index (BMI) close to the normal range at treatment initiation are strong predictors of a successful treatment outcome and positive prognoses (Löwe et al., Reference Löwe, Zipfel, Buchholz, Dupont, Reas and Herzog2001; Sly and Bamford, Reference Sly and Bamford2011). Consequently, the German and British Guidelines for eating disorders (NICE, 2017; Herpertz et al., Reference Herpertz, Herpetz-Dahlmann, Fichter, Tuschen-Caffier and Zeeck2011) as well as the American Psychiatric Association (2006) stress the importance of early diagnosis and treatment commencement amongst patients with AN to prevent chronic disease.
The time between illness onset and the initiation of a recommended treatment is the ‘duration of untreated illness’. This period has been estimated as 1.78 years on average amongst people with AN (Schoemaker, Reference Schoemaker1997). Individual and systemic factors influence the duration of untreated AN. Only half of affected individuals report eating disorder symptoms to their general practitioners (Becker et al., Reference Becker, Thomas, Franko and Herzog2005). In turn, evidence shows that physicians rarely recognize (Linville et al., Reference Linville, Brown and O’Neil2012) or diagnose AN (Hudson et al., Reference Hudson, Cumby, Klaber, Nicholls, Winyard and Viner2013); furthermore, they lack sufficient knowledge about eating disorder treatment (Girz et al., Reference Girz, Robinson and Tessier2014). Even after receiving an eating disorder diagnosis, affected individuals tend to refuse to begin the recommended treatment because of ambivalent attitudes towards treatment and recovery (Leavey et al., Reference Leavey, Vallianatou, Johnson-Sabine, Rae and Gunputh2011), or a lack of knowledge of specialized treatment options (Weigel et al., Reference Weigel, Gumz, Uhlenbusch, Wegscheider, Romer and Löwe2015). Availability and the networking of different health care providers might be deficient (Waller et al., Reference Waller, Schmidt, Treasure, Murray, Aleyna, Emanuelli, Crockett and Yeomans2009). These limitations may negatively influence individual pathways through the health care system (House et al., Reference House, Schmidt, Craig, Landau, Simic, Nicholls, Hugo, Berelowitz and Eisler2012).
Public health interventions have been shown to prevent disorders and promote physical and mental health (Kahn et al., Reference Kahn, Ramsey, Brownson, Heath, Howze, Powell, Stone, Rajab and Corso2002; Brousseau et al., Reference Brousseau, Sauvageau, Ouakki, Audet, Kiely, Couture, Pare and Deceuninck2010; Mears et al., Reference Mears, Abubakar, Crisp, Maguire, Innes, Lilley, Lord, Cohen, Borgdorff, Vynnycky, McHugh and Sonnenberg2014). Successful public health interventions have been designed to reduce suicide rates amongst individuals suffering from depression (Mann et al., Reference Mann, Apter, Bertolote, Beautrais, Currier, Haas, Hegerl, Lonnqvist, Malone, Marusic, Mehlum, Patton, Phillips, Rutz, Rihmer, Schmidtke, Shaffer, Silverman, Takashi, Varnik, Wasserman, Yip and Hendin2005; Hübner-Liebermann et al., Reference Hübner-Liebermann, Neuner, Hegerl, Hajak and Spiessl2010). However, little research has been conducted with regard to the potential of public health interventions to increase health care use amongst people with eating disorders (Becker et al., Reference Becker, Plasencia, Kilpela, Briggs and Stewart2014).
The present study evaluated the effect of the ‘psychenet Healthcare Network Campaign’ on the duration between AN symptom onset and the initiation of contact with the health care system as well as the initiation of an evidence-based eating disorder treatment in a female patient population. We hypothesized that after the implementation of this systemic public health intervention, (a) patients would report a briefer duration of untreated AN compared with those whose first treatment occurred before the implementation, and (b) the time between symptom onset and the first contact with the health care system would decrease. In addition, we investigated the type of health care professionals who were patients’ first point of contact after the onset of AN symptoms.
Methods
Participants
This non-randomized pre–post-intervention study was conducted between 2011 and 2014 across the metropolitan area of Hamburg, Germany. The study compared the duration of untreated AN using two independent cross-sectional samples of female patients who were in treatment for the first time. The first patient sample (ie, the ‘pre-sample’; recruitment period, January 2012 to February 2013) was assessed before the implementation of the systemic public health intervention. The second sample (ie, the ‘post-sample’; recruitment period, November 2013 to May 2014) was assessed after the implementation of the ‘psychenet Healthcare Network Campaign’. The trial was registered with an online public registry (ISRCTN44979231; Principal Investigator: B.L.). Figure 1 displays an overview of the study course, elements of the systemic intervention and the study outcomes.
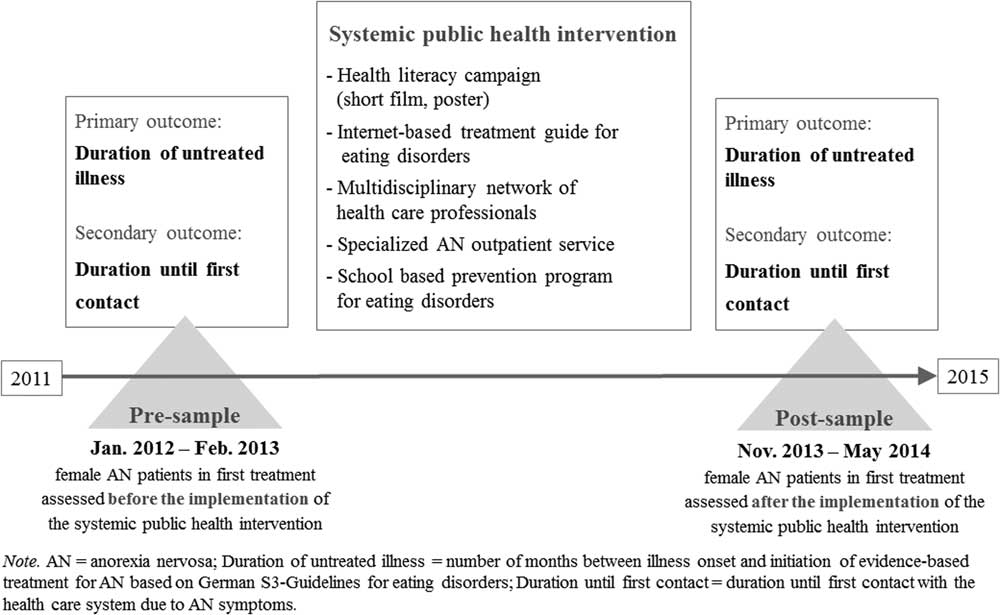
Figure 1 Study design of a community-level systemic public health intervention for patients with anorexia nervosa (AN). Duration of untreated illness = number of months between illness onset and initiation of evidence-based treatment for AN based on German S3-Guidelines for eating disorders; Duration until first contact = duration until first contact with the health care system for eating disorder symptoms.
Recruitment over the first three months in the pre-sample indicated that the initial recruitment goal of 100 patients in each sample was not feasible. Therefore, we extended the initial age range from between 12 and 39 years to between 10 and 60 years to sample individuals with (a) particularly early AN onset and (b) an average age of onset but a long duration of untreated AN. In addition, the recruitment period for the pre-sample was extended to 12 months. The project duration prevented an extension of the recruitment period for the post-sample. Additional inclusion criteria for both samples were as follows: female gender, current diagnosis of AN according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria (American Psychiatric Association, 2000), participation in a diagnostic telephone interview, currently undergoing their first eating disorder-specific treatment, and the provision of written informed consent. Eligible participants aged 10–15 years were required to provide written informed consent from their parent or legal guardian in addition to their own written informed consent. Participants between the ages of 16 and 18 years are legally able to provide written informed consent and were not required to provide additional consent from a parent or legal guardian. The exclusion criteria were as follows: insufficient German language skills or severe organic or psychological complaints preventing participation (based on the recruiting medical doctors’ or psychotherapists’ point of view). In addition, participants who did not live in Hamburg were excluded because they were regarded as unable to receive the systemic public health intervention.
Procedure
The procedure followed our published study protocol (Gumz et al., Reference Gumz, Uhlenbusch, Weigel, Wegscheider, Romer and Löwe2014). Participants were recruited from all available institutions in the Hamburg metropolitan area that offered evidence-based treatment for AN (Herpertz et al., Reference Herpertz, Herpetz-Dahlmann, Fichter, Tuschen-Caffier and Zeeck2011). In total, 11 inpatient wards, one day clinic, 19 outpatient departments and four eating disorder-specific counselling centres were contacted for recruitment. Each of these settings appointed a study therapist who was responsible for recruitment. Before recruitment, these study therapists received a preparatory training that included information regarding the overall study, procedure, eligibility criteria, materials and so on. During the recruitment period, the study therapists informed all eligible patients about the study’s purpose, obtained written informed consent and distributed the survey package. The survey package was composed of self-report measures assessing prior help-seeking behaviour, current eating disorder pathology, depression and anxiety symptom severity, and additional items regarding age, height, weight and educational level. If the patients met the inclusion criteria, then they were contacted via telephone to participate in a semi-structured diagnostic interview about AN. Participants were regarded as having dropped-out if they refused to participate in the telephone interview or if they could not be contacted after 10 attempts. Participants received a voucher for a free film of their choice at a local cinema in exchange for their participation, and the therapists were given a €7 online book voucher for each person they successfully referred to the study. The study and consent procedures were reviewed and approved by the ethics committee of the Psychotherapist Chamber of Hamburg.
Systemic public health intervention
The systemic public health intervention was designed to facilitate the early recognition of AN and diagnostic and treatment initiation for individuals suffering from AN by reaching affected individuals through their social environments and practitioners. The social environment was addressed with a health literacy campaign that consisted of a brief film presented at regional cinemas and a corresponding poster campaign in the Hamburg region (Figure 1). The film portrayed the personal experiences of a woman suffering from AN. The posters showed a portrait of the woman’s eyes, a quotation from the film and a note about the prevalence of AN. This film and the corresponding poster campaign sought to increase awareness of eating disorders and decrease the stigma of mental disorders and faciliate help-seeking.
An internet-based treatment guide for people with eating disorders was developed to reach affected individuals as well as their relatives, peers and health care professionals. The treatment guide provided information about AN, bulimia nervosa and binge eating disorder, treatment guidelines, and the contact information of local inpatient and outpatient institutions specialized in treating eating disorders. Information was adapted for each target group (patients, relatives and practitioners) and available in German, English and Turkish to address individuals with non-German backgrounds.
Practitioners were addressed through the establishment of a multidisciplinary health care network focussing on patients with eating disorders. The network met quarterly, and members of all recruitment centres as well as practitioners from other institutions with a focus on eating disorder participated. Each meeting was composed of a theoretical input from the study team (eg, current treatment guidelines, new therapeutic approaches for AN, medical management of AN), and a network member presented the casework.
Furthermore, a specialised AN outpatient service at the Department of Psychosomatic Medicine and Psychotherapy at the University Medical Centre Hamburg-Eppendorf was implemented. At this centre, affected individuals receive eating disorder diagnoses and treatment recommendations according to the current national guidelines (Herpertz et al., Reference Herpertz, Herpetz-Dahlmann, Fichter, Tuschen-Caffier and Zeeck2011) for eating disorders. Moreover, their primary care providers are provided with suggestions for the accompanying medical management. Lastly, a dissonance-based prevention programme for eating disorders was developed and evaluated within a large randomised controlled trial (for the study protocol, see Weigel et al., Reference Weigel, Gumz, Uhlenbusch, Wegscheider, Romer and Löwe2015). In this programme, all participating schoolchildren and their parents received a flyer including information about treatment options for adolescents suffering from eating disorders. All of the aforementioned elements of the systemic intervention were delivered between March 2013 and December 2014. The distribution of project flyers, talks at different public events, interviews in local newspapers and advertisements in journals for psychotherapists and medical practitioners were used as dissemination strategies. A more detailed description of the ‘psychenet Healthcare Network Campaign’ can be found elsewhere (Gumz et al., Reference Gumz, Uhlenbusch, Weigel, Wegscheider, Romer and Löwe2014).
Measures
The ‘duration of untreated illness’ was the primary study outcome and was operationalized as the number of months between AN symptom onset and the commencement of an evidence-based treatment, based on the German S3-Guidelines for eating disorders (Herpertz et al., Reference Herpertz, Herpetz-Dahlmann, Fichter, Tuschen-Caffier and Zeeck2011). During the telephone interview, AN was diagnosed using the eating disorder section of the Structured Clinical Interview for DSM-IV (Wittchen et al., Reference Wittchen, Zaudig and Fydrich1997). Therein, the onset of each diagnostic criterion for AN was specified. The date when all AN criteria were first met was operationalized as the illness onset. To quantify the individual duration of untreated AN in months, the date of the first eating disorder-specific treatment was recorded.
‘Duration until first contact with the healthcare system’ was the secondary study outcome and was assessed with a self-report measure that was part of the survey package. This variable was included to improve the understanding of the interval preceding the initiation of an evidence-based treatment for AN (House et al., Reference House, Schmidt, Craig, Landau, Simic, Nicholls, Hugo, Berelowitz and Eisler2012). It was operationalized as the number of months between illness onset and first contact with a health care professional for eating disorder-related symptoms. This variable might indicate patients’ help-seeking behaviours before beginning a specialized treatment. A questionnaire developed for the current study comprised different potential health care professionals that were contacted for eating disorder-related symptoms (eg, general practitioner, gynaecologist, dentist, psychotherapist and so on). In this questionnaire, participants indicated (a) whether they had contact with one or more of these health care practitioners, and (b) the year and month of the first contact with each health care professional.
To compare the current eating pathology of both samples, the German version of the Eating Disorder Examination-Questionnaire (EDE-Q; Hilbert et al., Reference Hilbert, Tuschen-Caffier, Karwautz, Niederhofer and Munsch2007) or its version for participants younger than 16 years of age (Ch-EDE-Q; Hilbert et al., Reference Hilbert, Hartmann and Czaja2008) was applied. Both self-report measures have satisfactory psychometric properties (Hilbert et al., Reference Hilbert, De Zwaan and Brähler2012). Current depression and anxiety symptom severity, the most common AN comorbidities, were collected to further characterise the study sample. These variables were assessed using the German versions of the nine-item depression module of the Patient Health Questionnaire (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe1999; Löwe et al., Reference Löwe, Gräfe, Zipfel, Witte, Lörch and Herzog2004a; Reference Löwe, Spitzer, Gräfe, Kroenke, Quenter, Zipfel, Buchholz, Witte and Herzog2004b) and the Generalized Anxiety Disorder Scale (Löwe et al., Reference Löwe, Decker, Müller, Brähler, Schellberg, Herzog and Herzberg2008; Kroenke et al., Reference Kroenke, Spitzer and Williams2010; Wild et al., Reference Wild, Eckl, Herzog, Niehoff, Lechner, Maatouk, Schellberg, Brenner, Müller and Löwe2014), respectively. Both instruments exhibited acceptable reliability and validity (Kroenke et al., Reference Kroenke, Spitzer, Williams and Löwe2001; Löwe et al., Reference Löwe, Spitzer, Gräfe, Kroenke, Quenter, Zipfel, Buchholz, Witte and Herzog2004b, Spitzer et al., Reference Spitzer, Kroenke and Williams2006; Löwe et al., Reference Löwe, Decker, Müller, Brähler, Schellberg, Herzog and Herzberg2008). Age, weight, height and educational level were also assessed as part of the questionnaire.
Statistical methods
Based on previous studies (Schoemaker, Reference Schoemaker1997) with an average duration of untreated AN of 19 months and an estimated effect size of Cohen’s d=0.4, we considered a decrease of untreated AN of 4.8 months or 25% as clinically relevant. Thus, when conducting linear mixed-model analyses, a two-tailed type-I error of 5%, and a power of 80%, two samples with 100 participants each were required.
The data were analysed using IBM SPSS Statistics for Windows, version 21 (IBM Corp., Armonk, NY, USA). We conducted two-tailed independent-samples t-tests and χ 2-tests for nominally scaled and non-parametric variables to compare both cross-sectional samples with regard to participant characteristics and levels of observed psychopathology. Frequencies are reported for answers to the variable ‘member of the health care system first contacted for eating disorder symptoms’.
Before conducting the linear mixed-model analyses, numerical data were inspected for normality using histograms. ‘Duration of untreated illness’ and ‘duration until first contact with the health care system’ were skewed and were consequently logarithmically transformed. The primary hypothesis (ie, whether differences exist between the pre- and post-intervention measures of the mean ‘duration of untreated illness’) was tested by applying a linear mixed-model analysis using maximum likelihood estimation. The period of assessment was specified as the independent variable, and the duration of untreated illness was the primary endpoint. Recruitment setting was included as a random control variable, and age was included as a fixed control variable.
As a secondary analysis, we calculated an analogous linear mixed-model with the mean ‘duration until first contact with the health care system’ as the dependent variable. In each case, 95% confidence intervals (CIs) were used to express the uncertainty in the data. As no variable showed missing values over 5%, the analyses were performed using complete cases and were not imputed. Two-tailed P-values <0.05 were considered as significant.
Results
Patient sample characteristics
The participation rates were 60.8% for the pre-intervention and 50.0% for the post-intervention groups. Figure 2 illustrates the flow of patients before and after the implementation of the systemic public health intervention.
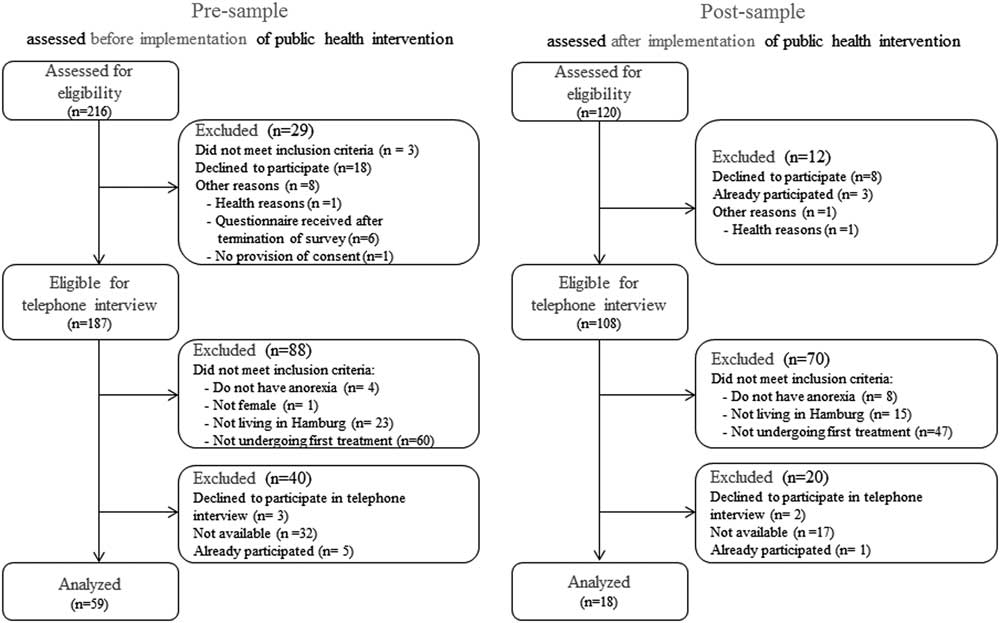
Figure 2 Flowchart of female anorexia patients in first treatment assessed before and after the implementation of a community-level systemic public health intervention. Participants who were not living in Hamburg were excluded because they were regarded as not having received the systemic public health intervention.
Both cross-sectional samples were well balanced with respect to participant characteristics and levels of observed psychopathology (Table 1). The majority of patients in both samples met the diagnostic criteria for the restrictive subtype of AN according to the DSM-IV. Based on the DSM-5 criteria for full threshold AN (American Psychiatric Association, 2013), 74.6% (n=44) of the patients in the pre-intervention group and 94.4% of the patients in the post-intervention group (n=17) would have received this diagnosis.
Table 1 Characteristics of female patients with anorexia nervosa (AN) undergoing their first specialized anorexia treatment pre- and post-implementation of a systemic public health intervention
Pre-sample=female AN patients in first treatment assessed before the implementation of the systemic public health intervention; Post-sample=female AN patients in first treatment assessed after the implementation of the systemic public health intervention; BMI=body mass index; EDE-Q=Eating Disorder Examination-Questionnaire; PHQ-9= depression module of the Patient Health Questionnaire; GAD-7=anxiety module of the Patient Health Questionnaire. Educational level=‘higher’ level of education – at least a general qualification to begin university.
Two-tailed t-tests for independent samples were used for metric variables as well as χ 2-tests for nominal scaled and non-parametric variables. Two-tailed P-values <0.05 were considered significant.
Evaluation of the systemic intervention
The mean duration of untreated AN was 36.5 months (SD=68.2, range 1–438 months) before the intervention and 40.1 months (SD=89.4, range 3–393 months) after the implementation of the systemic public health intervention. The mean duration until first contact with the health care system was 25.0 months (SD=53.0, range: −6 to 313 months) before the intervention and 32.8 months (SD=86.5, range 1–375 months) after intervention. Thus, neither the duration of untreated AN (adjusted mean difference =0.07 months, 95% CIs −0.18 to 0.32, P=0.58) nor the duration until first contact with a health care professional (adjusted mean difference =0.08 months, 95% CI −0.37 to 0.20, P=0.57) significantly decreased from pre- to post-assessment amongst women who received treatment for AN for the first time (Figure 3).
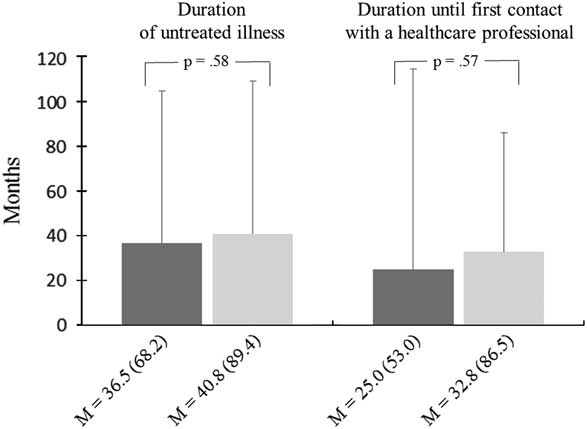
Figure 3 Duration of untreated illness and duration until first contact with a health care professional in female patients with anorexia nervosa before and after the implementation of a systemic public health intervention. Dark grey bars reflect the results of the pre-intervention group, and light grey bars reflect the results of the post-intervention group. Standard deviation in brackets. M=mean.
At the beginning of the individual treatment initiation process, participants in both samples most frequently consulted their general practitioner or paediatrician for their eating disorder-related symptoms (χ 2=4.86, df=2, P=0.71; Figure 4).
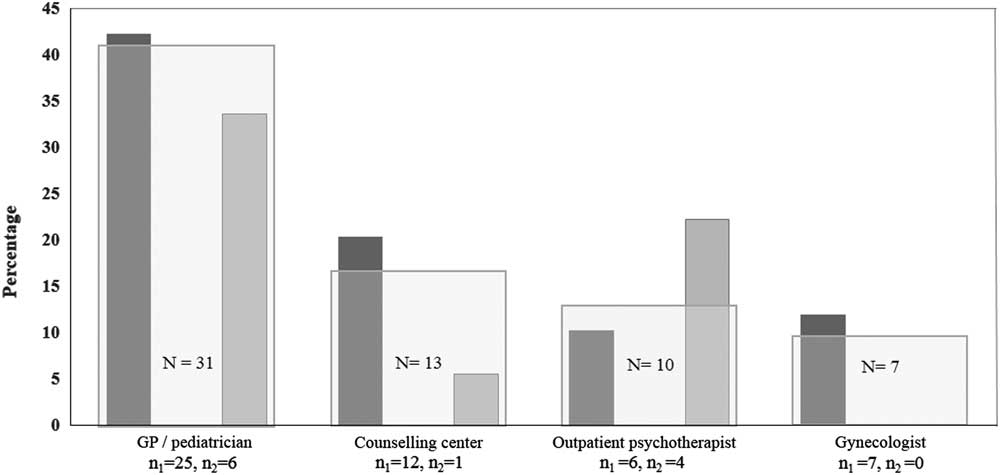
Figure 4 Health care professional first visited by female patients with anorexia nervosa because of eating disorder symptoms before treatment initiation. n 1=58 patients assessed before the implementation of a community-level systemic public health intervention; n 2=18 patients assessed after the implementation. Bar charts reflect the percentages of settings indicated n>5. Settings indicated <5 were not included (eg, neurologist, dermatologist, endocrinologist, dentist, non-medical practitioner and nutritionist). GP=general practitioner.
Within the post-intervention group (ie, participants assessed after the implementation of the systemic intervention), 16.7% (n=3) of the patients were aware of the brief film that had been shown in cinemas. Another 22.2% (n=4) had visited the main psychenet homepage and the internet-based treatment guide. Finally, 22.2% (n=4) had used the specialised AN outpatient clinic at the Department of Psychosomatic Medicine and Psychotherapy, University Medical Centre Hamburg-Eppendorf.
Discussion
The primary aim of the present study was to evaluate the effect of a systemic community-level public health intervention on the duration from AN onset to the initiation of contact with the health care system as well as the initiation of evidence-based eating disorder treatment in a sample of women with AN.
Before the implementation of the intervention, more than three years passed on average between the onset of AN and treatment initiation. Against our expectations, the time span remained statistically unchanged after the implementation of the systemic public health intervention. Likewise, the ‘psychenet Healthcare Network Campaign’ did not affect the time span between symptom onset and first contact with a health care professional.
The average duration of untreated AN observed in this study was considerably longer than the average duration of untreated AN according to a previous review (19 months; Schoemaker, Reference Schoemaker1997). The inclusion of adolescent and adults with AN in the present study and the consideration of both in- and outpatient sectors might explain these differences. From a clinician’s point of view, these results are alarming and underline the need to improve early diagnosis and treatment amongst patients with AN to prevent affected individuals from chronic disease and the severe complications of this disorder (Herzog et al., Reference Herzog, Deter, Fiehn and Petzold1997; Löwe et al., Reference Löwe, Zipfel, Buchholz, Dupont, Reas and Herzog2001).
The possible reasons for why the ‘psychenet Healthcare Network Campaign’ did not improve early treatment for AN include the following.
First, the sample size might have been too small to capture the effects. Second, it is possible that the intervention as a whole was ineffective. Third, the intervention might not have reached the relevant target groups. Fourth, the implementation period might have been too brief to allow for changes in the duration of untreated AN to become apparent. Finally, systemic community-level public health interventions in general might not be an appropriate tool to reach patients with AN during the early phase of their disorder.
We were unable to achieve our recruitment goal of 100 patients in each sample. This limitation is the greatest of our study because it decreases the interpretability of our results. In the pre-intervention group, we attempted to reach our recruitment goal by extending the age range and the recruitment period. As a consequence, it was necessary to compromise between a sufficiently long blanking period between the pre- and post-intervention groups in which the public health intervention was implemented and a sufficiently long recruitment period for the post-intervention group before the end of the study. This compromise resulted in different sample sizes of the two groups. The low prevalence of AN impedes the assessment of large samples in this population (Jacobi et al., Reference Jacobi, Hofler, Strehle, Mack, Geschler, Scholl, Busch, Maske, Hapke, Gaebel, Maier, Wagner, Zielasek and Wittchen2014). Nevertheless, we assessed the eligibility of 336 patients with AN over the course of the study. Of these patients, many were not experiencing their first treatment and therefore did not meet the inclusion criteria. If we had included patients with AN whose first treatment occurred in the past, then the sample size and associated statistical power would have been higher. However, such a change might have decreased the internal validity of our study because of a potential recall bias.
The second major drawback of the present study is that the exposure to the intervention could not be evaluated. This issue is common amongst public health interventions (Craig et al., Reference Craig, Dieppe, Macintyre, Michie, Nazareth and Petticrew2008). Therefore, we cannot determine whether the intervention was not effective because it did not diffuse sufficiently to reach all relevant community members or whether the intervention period was too brief to affect the relevant participants.
In addition, randomly assigning patients to different groups was not considered as feasible. As the intervention was conducted across the Hamburg metropolitan area, randomly allocating eligible participants to one group receiving the intervention and another group (ie, the control group) not receiving the intervention was not possible. However, we attempted to overcome this limitation by assessing one sample of patients before the implementation of the intervention and the other after implementation. Future studies evaluating the effect of public health interventions on early treatment among patients with AN should apply a randomized controlled design with a sufficiently large sample to increase internal validity (Becker et al., Reference Becker, Plasencia, Kilpela, Briggs and Stewart2014).
In addition, the variables of interest (eg, information about first treatment) were primarily assessed through retrospective self-reports and are vulnerable to inaccuracies. To counteract this possible recall bias, self-reported data were reviewed during the telephone interview. Importantly, a prospective assessment of these variables was not feasible given the low prevalence of AN. In addition, BMI was assessed through self-reports, which might have resulted in overestimation. However, the self-reported weight assessed during the telephone interview referred to the weekly mandatory weight measurements during the inpatient or outpatient treatments.
Patients with extremely low body weights were excluded from our sample when cognitive deficits prevented them from completing the self-report measures or from participating in the telephone interview. These patients might display a particularly long duration of untreated AN.
Finally, our sample only included women. We decided to focus on this gender to achieve homogeneity within the sample. However, conclusions drawn from our results are not transferable to men who suffer from AN.
Implications of research
Our study was the first to investigate the influence of a community-level systemic public health intervention on treatment initiation amongst people with AN. Given the high prognostic value of early treatment and the mean duration of untreated AN of more than three years, our results underline the need for an improved understanding of the process of treatment initiation amongst people with AN to develop effective interventions and prevent affected individuals from severe, chronic disease.
In line with prior evidence, our results emphasized that primary caregivers are an important interface on the path towards evidence-based AN treatment (Kessler, Reference Kessler2009). Future public health interventions to improve early diagnosis and treatment for people with AN might benefit from a collaboration with primary caregivers (Martin-Misener et al., Reference Martin-Misener, Valaitis, Wong, MacDonald, Meagher-Stewart, Kaczorowski, O-Mara, Savage and Austin2012). However, previous studies showed that primary caregivers might suffer from a lack of knowledge regarding the recognition, diagnosis and management of eating disorders (Linville et al., Reference Linville, Brown and O’Neil2012; Hudson et al., Reference Hudson, Cumby, Klaber, Nicholls, Winyard and Viner2013; Girz et al., Reference Girz, Robinson and Tessier2014). Shared care attempts based on a multiprofessional collaboration between primary care providers and mental health professionals might facilitate the recognition, diagnosis and management of AN in primary care. Although shared care models have revealed promising results in the areas of maternal mental health (Li et al., Reference Li, Bowen, Szafron, Moraros and Muhajarine2016) as well as depression and anxiety (Archer et al., Reference Archer, Bower, Gilbody, Lovell, Richards, Gask, Dickens and Coventry2012) evidence from the eating disorder field is still needed. A systemic qualitative review of enablers and the barriers to implementing collaborative care for patients with anxiety and depression (Overbeck et al., Reference Overbeck, Davidsen and Kousgaard2016) indicated that future shared care attempts for patients with AN should put particular emphases on (a) effective educational programs, (b) appropriate reimbursements for extra work related to primary care providers, (c) the establishment of effective systems to ensure communication and monitoring between stakeholders and (d) the promotion of regular face-to-face interactions between care managers and primary care providers.
Implications for practice
-
∙ The mean duration of untreated AN exceeds three years.
-
∙ Help-seeking in patients with AN most frequently begins with the general practitioner.
-
∙ Evidence-based treatment does not typically begin until one year after the initial help-seeking event.
Acknowledgement
The authors would like to thank Anne Daubmann for her comments on this manuscript.
Financial Support
The study was part of a health service research project (psychenet) that was funded by the German Federal Ministry of Education and Research (ISRCTN44979231; subproject Anorexia and Bulimia Nervosa; Principal Investigator: B.L.).
Conflicts of Interest
None.
Ethical Standards
The study protocol and consent procedure were reviewed and approved by the ethics committee of the Psychotherapist Chamber of Hamburg. The authors also assert that all procedures contributing to this work comply with the Helsinki Declaration of 1975 as revised in 2008.








