Introduction
Osteoporosis is a chronic and progressive disease leading to gradual deterioration of skeletal tissue, which predisposes the sufferer to an increased risk of fracture, deformity, disability and even premature death. The growth of this ‘silent epidemic’ is projected to escalate worldwide with the changing demographics of an ageing population (Khaw, Reference Khaw1999).
Recent studies have shown that 80%–90% of fractures in post-menopausal women are associated with osteoporosis, and in these individuals there is a 20-fold increase in risk of sustaining a further fracture in the future (Andrade et al., Reference Andrade, Majumdar, Chan, Buist, Go, Goodman, Smith, Platt and Gurwitz2003). The high morbidity and mortality rates following an osteoporotic fracture are particularly distressing given that since the early 1990s, several effective pharmacological therapies have been proven to reduce fracture risk by 40%–60% within the first year (Epstein and Goodman, Reference Epstein and Goodman1999). There is a general worldwide consensus that osteoporosis should be actively sought in patients over 50 presenting with a fragility fracture, and it is widely recognised that great benefit can be gained from timely initiation of effective treatment (National Osteoporosis Foundation, 1999).
Two detailed reviews were conducted on this topic in (Elliot-Gibson et al., Reference Elliot-Gibson, Bogoch, Jamal and Beaton2004 and Giangregorio et al., Reference Giangregorio, Papaioannou, Cranney, Zytarukm and Adachim2006) and both highlighted the frequency of missed opportunities for secondary prevention following a fracture (Figure 1). It is important to note, however, that these reviews included many studies reporting on practice in the mid-1990s when pharmacologic approaches to fracture reduction were in transition, and did not focus specifically on older patients in whom osteoporosis is most prevalent.
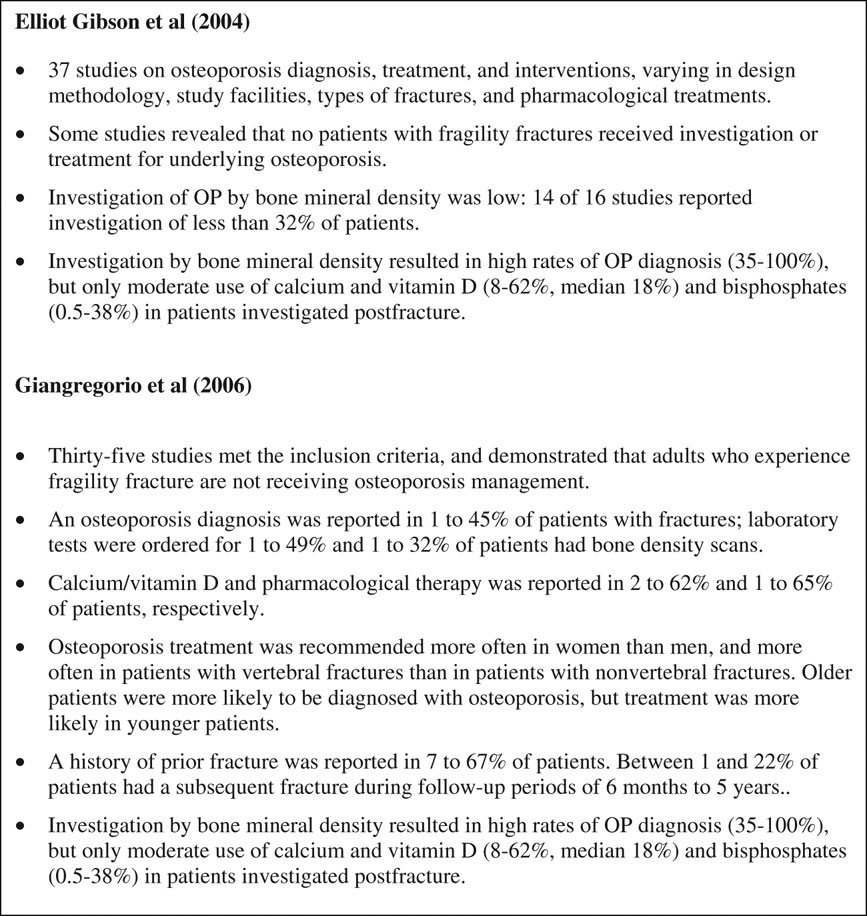
Figure 1 Summary of the results of the literature reviews of 2004 and 2006
In the US, 2002–2011 has been named the National Bone and Joint Decade (Bush, Reference Bush2002), which was implemented to increase awareness of osteoporosis amongst patients and physicians. Thus, there is now a need to discover if there has been an improvement in osteoporosis care since these earlier reviews, particularly in light of recent management guidance and education aimed at healthcare practitioners (National Osteoporosis Foundation, 1999; NICE, 2003; NICE, 2008).
The specific question to be addressed is: is there a lack of investigation to detect osteoporosis and prescribing of secondary bone prevention medication to older patients following fragility fractures?
The terms in bold warrant further clarification:
• ‘Investigation’: the use of bone mineral density (BMD) scans or ‘dual energy X-ray absorptiometry’ (DEXA) scans to confirm osteoporosis.
• ‘Secondary bone prevention’: the use of medication to reduce the risk of further osteoporosis-related fractures, including bisphosphonates, raloxifene, teriparatide, hormone replacement therapy, calcium and vitamin D supplements.
• ‘Older’: patients aged over 50.
• ‘Fragility fracture’: fracture resulting from a fall from standing height or less, suggesting for skeleton weakness.
Method
Search strategy
The databases, electronic journals and search engines used were:
• PubMed
• MEDLINE
• EMBASE
• HMIC
• BMJ
• Cochrane Library
• Google Scholar
All searches were restricted from 1995–2008, as this was deemed appropriate to yield the most relevant span of literature, and only English language studies were located.
The standard Boolean search framework was used to find all pertinent studies on the literature review question. A further set of results was obtained using a ‘snowballing’ technique by perusing the reference lists of the initial studies and reviews found.
Table 1 demonstrates the key search terms and selected synonyms employed during the search.
Table 1 Search terms used
The four key search terms were determined using the original research question. These were then exploded using the MeSH tool in the PubMed database to obtain the relevant synonyms. For example, when the term ‘osteoporosis’ was exploded, the entry term ‘post traumatic osteoporosis’ was obtained which was not considered relevant as the research question was only concerned with the age-related osteoporosis, and thus was excluded. The specific anatomical fragility fracture terms used were selected, as these are the most common osteoporotic fracture sites.
As the primary aim for the review was to establish the rates of secondary bone prevention prescribing, it was not necessary to include ‘investigation’ or ‘diagnosis’ as a search term as this was not a pre-requisite for inclusion – if this had been used, studies that only focused on medication rates would not have been located.
The search terms were combined systematically, by using one synonym from each column every time and until all possible combinations were exhausted. In practice, it was not necessary to use every combination each time, as data saturation occurred before the list was completed in each individual database or search engine. The algorithm was continued until no additional new studies were obtained.
The search strategy yielded 803 abstracts from the databases, once duplications were deleted.
Study selection criteria
Studies were selected for review if they met the following inclusion criteria:
a) The subjects included patients with a fragility fracture.
b) The subjects were all over the age of 50.
c) The results reported the number of patients who had been treated for osteoporosis following the fracture treatment outcomes included the initiation of calcium, Vitamin D, multivitamins, hormone replacement therapy, bisphosphonates, calcitonin and any other anti-resorptive therapies.
Articles were excluded if:
a) They were not reported in the English language.
b) They were evaluating an intervention to improve treatment practice.
c) They focused on concomitant diseases such as corticosteroid-induced osteoporosis.
d) They had been previously included in the prior reviews of 2004 and 2006.
e) They were an opinion article or a letter to the editor.
Following application of these inclusion and exclusion criteria, only nine studies remained. Of these, only seven were formally appraised for the review since, on closer evaluation, two were not directly relevant to the research question (Table 2).
Table 2 Justifications for the rejection and inclusion of studies appraised
Results
Critical appraisal of the evidence
Examination of the nine studies obtained revealed several consistent themes. All of the studies assessed the treatment outcomes in patients following a fragility fracture, but six of the nine studies further reported the rates of investigation in the affected patients, and several additionally commented on the influence of age and gender on prescribing patterns (Table 3).
Table 3 Summary of the studies used
DEXA = dual energy X-ray absorptiometry; M = male; F = female.
Treatment rate
All of the studies concluded that there continues to be a lack of active therapeutic intervention for osteoporosis in elderly people.
For example, the two lowest rates of treatment intervention reported were 9.5% and 15.4% by Papaioannou et al. (Reference Papaioannou, Kennedy, Ioannidis, Gao, Sawka, Goltzman, Tenenhouse, Pickard, Olszynski, Davison, Kaiser, Josse, Kreiger, Hanley, Prior, Brown, Anastassiades and Adachi2008) and Bessette et al. (Reference Bessette, Ste-Marie, Jean, Davison, Beaulieu, Baranci, Bessant and Brown2008), respectively. These studies adopted prospective cohort designs through the use of patient surveys as their primary research method. Both involved substantial sample numbers focusing on a particular gender (2187 men and 903 women, respectively).
Papaioannou et al. (Reference Papaioannou, Kennedy, Ioannidis, Gao, Sawka, Goltzman, Tenenhouse, Pickard, Olszynski, Davison, Kaiser, Josse, Kreiger, Hanley, Prior, Brown, Anastassiades and Adachi2008) found that after five years, 90% of community dwelling Canadian men aged 50 or over with a clinical fragility fracture remained untreated. Participation was entirely voluntary in this study, however, and thus subject to non-response bias. For example, those on treatment may have been more or less willing to participate due to personal views about the medication they had been prescribed. Furthermore, though the number of men lost to follow up was small (2.4%), a greater proportion of these were older. As the study concluded that older men are more likely to have fractures and to be treated, this may have led to an underestimation of the true treatment rate.
The validity of the method used is also questionable since the detailed interviewer led questionnaire resulted in fractures being self-reported and the medication rates were based on the instruction to participants to ‘bring all of the contents of their medicine cabinets’. Clearly medications that were not adhered to are unlikely to have been included, regardless of prescription. Nevertheless, the sample size was and this is the first population based, cohort study to examine this topic in men.
The second lowest prescribing rate of 15.4% reported by Bessette et al. (Reference Bessette, Ste-Marie, Jean, Davison, Beaulieu, Baranci, Bessant and Brown2008), also in Canada, was determined through a series of telephone interviews over a six to eight month period following the initial fracture. Once again, whilst a clear strength of the study is its large sample size, this is undermined by the fact that participation was significantly lower amongst women over 70. Since osteoporosis prevalence increases with age one might expect a correlation between the rate of secondary bone prevention prescribing and the age of the patient. Consequently the selection bias caused by the over representation of younger women in the sample may have overestimated the true medical care gap the study claims to identify.
In addition, the internal validity of the results is questionable due to the effects of recall bias from relying on patients’ accounts to determine prescribing rates. The validity may also have been influenced through the use of telephone interviews, since the extent of a patients’ osteoporosis, and thus potential degree of immobility, may affect their likelihood of answering a telephone survey. The acknowledgement of funding provided by pharmaceutical companies such as Procter and Gamble also raises concerns, as this could have incentivised the researchers to report low prescribing rates to encourage increased usage of anti-resorptive drugs.
This is also true of Gehlbach et al. (Reference Gehlbach, Avrunin, Puleo and Spaeth2007), though the credibility of their finding of only a 32% treatment rate in American females over 65 with a prior fracture is strengthened by the use of 9700 females – the largest sample size of all the studies included. However, similar to Papaioannou et al. (Reference Papaioannou, Kennedy, Ioannidis, Gao, Sawka, Goltzman, Tenenhouse, Pickard, Olszynski, Davison, Kaiser, Josse, Kreiger, Hanley, Prior, Brown, Anastassiades and Adachi2008), the validity of their method is in part undermined by confirming reporting of prescription rates by subjects with ‘interviewer inspection of containers’ only, as opposed to direct examination of their medical records.
Whilst all the aforementioned studies were conducted in America, in the UK the publication of osteoporosis guidelines by the British Orthopaedic Association (BOA) and most recently the National Institute of Clinical Excellence (NICE) hoped to address ways that the care of fragility fracture patients could be improved (Figure 2). To assess the effect of publication of the BOA guidelines in 2003, Nixon et al. (Reference Nixon, Ibrahim, Johari, Eltayef, Hariharan and Taylor2007) reviewed the case notes of 602 fracture patients from 2003 to 2005. They found that the proportion of patients discharged on osteoporosis medication remained below 25% every year, with no significant improvements between the years. The authors assert that this demonstrates that the BOA guidelines have had no impact, but this conclusion is weakened by the limited generalisability of their results, based only on proximal femoral fractures admitted to two Leicester hospitals in only January and February each year.
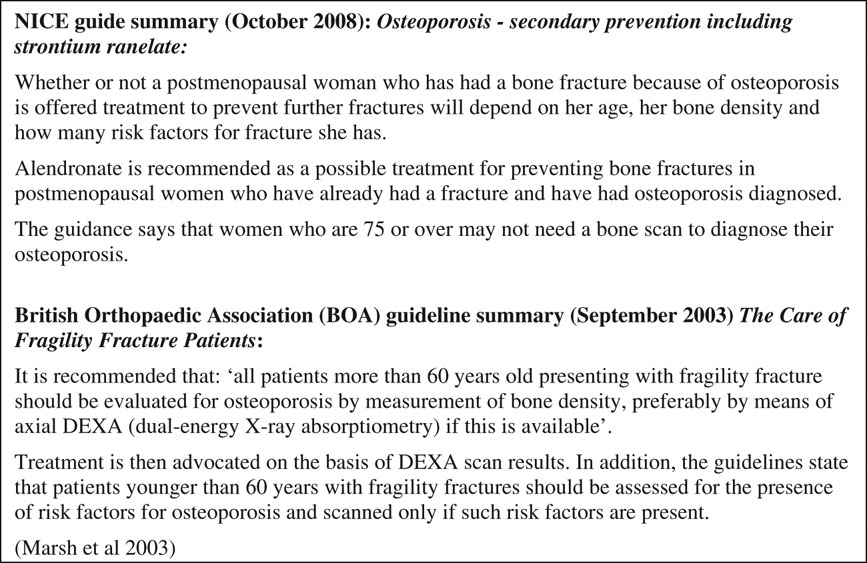
Figure 2 Summary of National Institute of Clinical Excellence and British Orthopaedics Association Guidelines for Osteoporosis Management
Investigation rate
Prescriptions are not the only indicator of a healthcare practitioner’s recognition of osteoporosis in patients with recently diagnosed fragility fractures. Diagnostic modalities are known to be relatively accurate, inexpensive, non invasive and readily available for these patients (Brown and Bradio, Reference Brown and Bradio2000). Nevertheless, this review found consistently low rates of investigation of osteoporosis with possible fragility fracture.
Prasad et al. (Reference Prasad, Sunderamoorthy, Martin and Murray2006) found that, on conducting a retrospective audit of patient records for those admitted to a Scottish hospital over a two-month period, just one of the 27 patients eligible were referred for a DEXA scan. These findings, alarming though they may appear, must be viewed with discretion due to the small sample size and focus on one type of fracture in one hospital and over a short period of time. An additional limitation of the retrospective method employed is that it is impossible to determine whether the lack of prescribing was influenced by drug tolerability, other co-morbidities, or individual patient choice.
Further studies reported similarly low investigation rates. Most recently in October 2008 Suhm et al. found that DEXA scans were used in just 31.4% of the 3667 patients recruited across eight Swiss medical centres. A limitation of this study is that although a dedicated nurse was responsible for data collection at each site, the variation between sites in the time they could allocate to the project sometimes led to incomplete data collection.
These limitations should be viewed in context with several strengths, such as the large sample and the increased validity of using patient records to obtain the relevant information, in comparison to the approach adopted in some of the studies mentioned previously of asking the patients directly.
The low rates of diagnostic workup were confirmed by Perreault et al. (Reference Perreault, Dragomir, Desgagné, Blais, Rossignol, Blouin, Moride, Ste-Marie and Fernandès2005) who focused solely on Canadian female patients over 70, by randomly selecting 40% of women listed in a health database from 1995 to 2001. Crude rates of BMD testing improved from 20.4% in 1995 to 41.1% in 2000, though remaining unsatisfactory overall. Though a large sample was used over the five years (ranging from 1370 to 1883 patients), the validity may be reduced by the possibility of differential and non-differential information bias from determining anti-resorptive therapy usage using a computer-based administrative database, as acknowledged by the authors.
Influence of age and gender on prescribing patterns
The following analysis of the studies commenting on the influence of age and gender on prescribing patterns is not directly relevant to the main research question, but is nonetheless valuable in developing a more detailed picture of the influences on the current medical care gap in osteoporosis management.
It is widely recognised that the prevalence of osteoporosis increases with age, and the efficacy of anti-resorptive therapies has been most successfully demonstrated in the elderly population. Furthermore, the adverse impact of future fragility fractures on quality of life, morbidity and mortality is far more consequential in older patients. Combined with the expectation that the number of people over 60 years of age is expected to increase by 40% over the next 40 years, it is clear that there is a critical need for adequate detection and urgent treatment of osteoporosis in elderly fragility fracture patients.
Encouragingly, Hooven et al. (Reference Hooven, Gehlbach, Pekow, Bertone and Evan2005) and Bessette et al. (Reference Bessette, Ste-Marie, Jean, Davison, Beaulieu, Baranci, Bessant and Brown2008) reported an increase in the likelihood of treatment following a fracture with increasing age. Once again the use of a survey by Hooven et al. (Reference Hooven, Gehlbach, Pekow, Bertone and Evan2005) raises concerns over the representative nature of the sample due to the influence of non-response bias, and the impact on validity of recall bias. The internal validity is also affected because the critical question asked (Figure 3) could have been interpreted in varying ways by the patients. Often different medications are known by several generic brand names, and confusion may have arisen if patients had experienced fragility fractures before the fracture in question. The use of a postal as opposed to an interviewer led survey resulted in the authors not being able to clarify such inherent ambiguities, and there is no evidence of a pilot study having being used to pre-empt such difficulties.
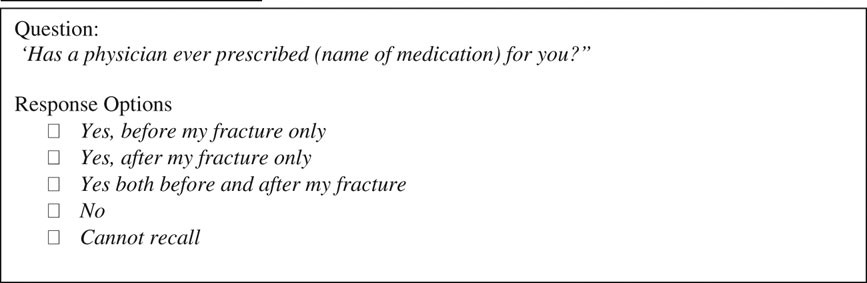
Figure 3 Critical question used in survey by Hooven et al. (Reference Hooven, Gehlbach, Pekow, Bertone and Evan2005)
Whilst the focus on a predominantly white female population from one medical centre reduces the generalisability of the authors’ findings that a sizeable intervention opportunity exists for patients with a fracture history, the study has merits in its sample size of 311 patients and the inclusion of patients over an extended time period of two years.
Despite the fact that postmenopausal females are often regarded as the population subset most at risk of osteoporosis, it is increasingly being recognised as an important cause of morbidity and mortality on older men. Given that the long term risk of subsequent fracture and diagnostic and therapeutic recommendation are the same in both genders, it is important to note that Freedman et al. (Reference Freedman, Potter, Nesti, Giuliani, Chadwick and Kuklo2008), for example, concluded that there is a significant deficiency in care in males in particular. Though their use of only 156 predominantly male participants from a military retiree population in a single US healthcare system limits the generalisability of this conclusion, their findings were confirmed by Suhm et al. (Reference Suhm, Lamy and Lippuner2008) who included over 3000 patients across eight healthcare centres in Switzerland.
Discussion
The findings of this review are in accordance with the previous reviews of 2004 and 2006, but differ in that the focus was exclusively on individuals over 50 years of age. Furthermore, all of the studies included were conducted since 2006, when pharmacologic approaches to fracture reduction are no longer regarded as in transition, but have been reinforced through published guidance.
Several factors may contribute to missed opportunities in osteoporosis management for patients presenting with fragility fractures. As Ferrari (Reference Ferrari2008) suggests, the fragmented delivery of care – where the role of the orthopaedic surgeon is to ‘fix’ the fracture, the geriatricians’ to manage any potential systemic complications, and the primary care physicians’ to rehabilitate the patient and facilitate their return to a normal degree of function – may result in blurred lines of responsibility for the initiation of osteoporosis treatment.
A perception that orthopaedic surgeons were not well attuned to osteoporosis care led the Bone and Joint Decade and the International Osteoporosis Foundation to survey 3422 orthopaedic surgeons in France, Germany, Italy, Spain, the UK and New Zealand in 2004. The authors concluded that the orthopaedic surgeon, as often the only physician seen by the fracture patient, has a unique opportunity to assess the risk of future fractures and initiate treatment if required and thus they must be provided with more educational opportunities regarding appropriate care (Dreinhöfer et al., Reference Dreinhöfer, Féron, Herrera, Hube, Johnell, Lidgren, Miles, Panarella, Simpson and Wallace2004). However in a UK survey of 230 surgeons and general practitioners by Chami et al. (Reference Chami, Jeys, Freudmann, Connor and Siddiqi2006), only 17% of orthopaedic surgeons said they would initiate treatment or refer a 55-year old women with a low-trauma wrist fracture to the appropriate service. A similar survey at the Mayo Clinic found orthopaedic surgeons favoured addressing osteoporosis with patients if necessary, but advocated the use of a nurse practitioner so that the onus would not rest solely with them (Simonelli et al., Reference Simonelli, Killeen, Mehle and Swanson2002).
Harrington et al. (Reference Harrington, Barash, Day and Lease2005) argue that weaker interventions that simply overlay traditional care, such as the education of busy physicians, have failed in many healthcare systems. Therefore they implemented a four-year clinical improvement project in a US health system using evidence-based guidelines and rapid cycle process improvement methods (plan-do-study-act cycles). Their adoption of a multi-faceted approach, incorporating a nurse centred management program, direct referral from orthopaedics to an osteoporosis care service, clinical process management software, telephone monitoring, and algorithms to define care and provider roles, was found to be highly effective in addressing the care gap of osteoporotic patients, and may have applicability to the UK.
Rather than passing responsibility between the orthopaedic surgeon and primary care physician, consistent and continuous collaboration between healthcare professionals is more likely to be effective in promoting appropriate osteoporosis care. In 2003, an Ontario initiative known as the ‘Fracture? Think Osteoporosis’ Program, aimed to reduce the rate of future fractures in patients presenting with fragility fractures by improving osteoporosis recognition and treatment. It involved education of the geriatric and rehabilitation teams, including one-on-one and group-based sessions, and since its launch the initiation of secondary anti-resorptive therapy has substantially improved. Again, the approach may have utility in the UK.
Beyond the lack of sufficient education amongst physicians as a root cause of the deficiency in care, Simonelli et al. (Reference Simonelli, Killeen, Mehle and Swanson2002) found that the most frequently indicated factors limiting the treatment of presumed osteoporosis in post-fracture patients were concerns about medication adverse effect and cost. Yet a cost effectiveness analysis by Borgström et al. (Reference Borgström, Ström, Coelho, Johansson, Oden, McCloskey and Kanis2009), assuming a willingness to pay for a quality-adjusted life years of £30 000, concluded that a prior fragility fracture was a sufficiently strong risk factor to indicate that treatment was cost-effective from the age of 65 years – even in women in whom BMD was not known. Such issues require to be addressed by appropriately tailored education to health professionals.
However, whilst many prospective clinical trials have demonstrated the efficacy and cost effectiveness of bisphosphonates, an increasing number of studies have concluded that compliance with this treatment in normal practice might differ from that in the trials (Andrade et al., Reference Andrade, Walker, Gottlieb, Hollenberg, Testa, Saperia and Platt1995; McClung, Reference McClung and McClung2001). Only approximately 1% of bisphosphonates are absorbed during oral ingestion, and due to their action as chelators for mineral ions, they easily form complexes with mineral ions in the diet. Therefore there are many restrictions for the ingestion of these drugs – such as being taken on an empty stomach, without milk, and with the patient advised to remain in an upright position for 30 to 60 min after consumption. As Kamatari et al. (Reference Kamatari, Koto, Ozawa, Urao, Suzuki, Akasaka, Yanagimoto and Sakota2007) found, it was these restrictions that resulted in the poor compliance rates for the majority of patients. Furthermore, three types of adverse effects are associated with some or all bisphosphonates: renal toxicity, acute-phase reactions and gastrointestinal disorders. More recently, osteonecrosis of the jaw has also emerged as a growing issue (Diel et al., Reference Diel, Bergner and Grötz2007). In light of these adverse effects, it is important to remember the demographics of the patient population under discussion – in whom polypharmacy is an increasing concern and multiple comorbidities are likely to be present. The impact of such factors, which would have remained hidden, in many of the studies included here, need to be fully investigated.
Nonetheless, the National Osteoporosis Foundation guidelines explicitly indicate that all postmenopausal women who experience a low-impact fracture deserve attention to osteoporosis, and therapy may be offered without BMD testing if necessary. With the availability, accuracy and relative inexpensive nature of diagnostic modalities and the high efficacy of antiosteoporotic drugs, there is a clear need to recognise the possible presence of osteoporosis underlying fragility fractures. Subsequent initiation of the necessary treatment has the potential to dramatically reduce the detrimental impact of osteoporosis on the morbidity and mortality of our elderly population. The advent of more recent therapies, such as the fully human monoclonal antibody Denosumab, which is currently being studied, may offer further effective treatment avenues for postmenopausal osteoporosis (McClung et al., Reference McClung, Lewiecki and Cohen2006). The potential economic impact must also be considered – in the UK more than £1.7 billion a year is spent on social and acute care for treating the current level of osteoporotic fractures, and this is expected to increase to £2.1 billion by 2010 with an ageing population (Nice Guidelines, 2003).
Of particular relevance to UK primary care, the National Orthopaedic Society has campaigned since 2005 against the omission of osteoporosis from quality and outcomes framework (QOF) guidelines. In the latest QOF review, an independent expert panel considered the evidence and agreed that including some osteoporosis indicators in the QOF was necessary on both clinical and cost effectiveness grounds. However, in the face of a lack evidence from the UK the reviewers eventually concluded that future research was required to more clearly delineate the true extent any deficiencies of osteoporosis care in this country. Such research must include a detailed exploration the barriers to adhering to current guidelines, and a search for the precise reasons for any treatment gap identified. Only then can guidelines be improved and treatment delivery optimised.
In conclusion, the changing demographics of our population and increasing workload and financial pressures on the National Health Service, means it would be perilous to ignore the growing tide of the ‘silent epidemic’ of osteoporosis. The consistently low-intervention rates reported in all of the seven studies appraised to provide evidence that elderly individuals in the US and Switzerland who experience fragility fractures are still not receiving adequate investigation or treatment for osteoporosis. Further research is needed as a matter of priority to describe the situation in the UK.








