Introduction
The NHS is actively encouraging people to undertake more self-care in relation to their own health and has issued a series of policy documents on this subject (see, for example, Department of Health, 2005a; 2006a). While the introduction of such policies is a relatively recent occurrence, self-care is not a new phenomenon. The Joining Up Self-Care (JUSC) project aimed to implement and evaluate the first Primary Care Trust (PCT)-wide integrated programme of supported self-care. The intention was not to invent something new but rather to build on existing initiatives and to develop a shared understanding of self-care,Footnote 1 building on a visual representation of the scope of self-care (Figure 1).

Figure 1 The self-care continuum
The interventions were three service modules delivered by the PCT relating to disease prevention (community-based coronary heart disease (CHD) prevention aimed at people aged over 30 years), care of people with long-term conditions (a disease-specific self-care skills training course for asthma) and the management of minor ailments aimed at mothers of children aged three months to 12 years.
The detailed content of each module is reported elsewhere (Working in Partnership Programme, 2006). Briefly, the CHD module involved promotion through community pharmacies and local employers with participants receiving an information pack on lifestyle changes to achieve risk reduction. The disease-specific asthma course comprised the generic Expert Patient Programme (EPP) with an additional session on asthma developed by EPP and Asthma UK, plus separate half-day ‘taster’ sessions. The minor ailments module comprised seasonal information campaigns, expansion of the ‘Pharmacy First’Footnote 2 service, and ‘Self-Care Aware’ training for health professionals. Each of the three modules aimed to provide information to support problem-solving and decision-making and to increase self-efficacy. Information materials were distributed through community-based locations including schools, local employers and pharmacies and the modules were promoted through media including newspapers and radio.
Community-based health promotion has been the subject of many previous studies, some of which have addressed prevention of heart disease (see, for example, Lindholm et al., Reference Lindholm, Rosén, Weinehall and Asplund1996; Tudor-Smith et al., Reference Tudor-Smith, Nutbeam, Moore and Catford1998). The findings have been mixed and, it could be argued, positive effects have been at best moderate (Merzel and D’Afflitti, Reference Merzel and D’Afflitti2003). The JUSC CHD module aimed to explore the effect of linked individual self-assessment of risk and user-friendly practical written information on risk reduction.
Self-care skills training for members of the public has gradually become accepted as a valuable tool in the management of long-term conditions. In the UK the EPP has been the subject of both an internal monitoring process and a randomized controlled trial. Positive effects on self-efficacy have been shown (Department of Health, 2005b). At the time of the JUSC study there were no previous published UK evaluations of disease-specific, as opposed to generic, EPP courses. The JUSC evaluation aimed to address this gap.
Many PCTs have introduced community pharmacy-based schemes to support the transfer of minor ailments management away from general practitioner (GP) consultations so that doctors can spend more time dealing with more serious conditions. A review of previous schemes found them to be acceptable to, and well used by, the public (Blenkinsopp and Noyce, 2002). However, only one scheme had previously measured the impact on GP consultations for minor ailments (Hassell et al., 2001) and none had investigated the effect on people’s self-confidence in dealing with minor ailments or intended future use of health services for this purpose. The JUSC evaluation included these aspects.
The overall aims of the evaluation were to measure the effects of an integrated programme of supported self-care on three stakeholder groups: members of the public, health professionals and the PCT. For members of the public the outcomes measured were awareness, behaviour and attitudes towards self-care, and for health professionals, attitudes and practice in relation to self-care. For the PCT we wanted to evaluate any changes in strategic and operational approaches to supporting self-care.
Methods
Study design
The study design is summarized in Figure 2. A multi-stakeholder Steering Group oversaw the evaluation design and its subsequent implementation. Data on patient/public and health professional attitudes and behaviours were collected, comparing baseline measures during the period February–December 2005 with follow-up 5–12 months later (February–May 2006). Specific research methods included postal survey questionnaires (for the three intervention modules), a GP record audit (for the minor ailments module) and qualitative techniques including focus groups and (for health professionals) individual interviews. Control groups were recruited at baseline for the Asthma and Minor Ailments modules, and at follow-up (using a community-wide survey) for the CHD module.

Figure 2 Study design
Outcome measures
Key outcomes relating to members of the public were uptake of self-care support measures, self-reported lifestyle changes, consultations with health professionals and stated intentions for future behaviour. For CHD prevention these were changes in diet, exercise, smoking cessation and alcohol consumption and consultation rates with health professionals regarding heart health; for asthma management, participation levels in the ‘Staying Well with Asthma’ programme, participants’ attitudes towards taking care of their asthma and that of any other family members, medicines usage and GP consultation rates for asthma; and for minor ailments, participation levels in ‘Pharmacy First’, use of pharmacies and NHS Direct for advice, rates of GP consultations for children’s minor ailments, awareness levels of self-care options and likely future actions by mothers.
Key outcomes relating to health care professionals and PCT staff were as follows: for health care professionals, attitudes towards self-care in illness prevention, minor illness management and long-term conditions management, knowledge of and referral to local self-care resources; for PCT staff, operational implications of establishing and sustaining the JUSC programme; for the general population, awareness of the self-care programme and use of sources of healthcare advice.
Data collection
Baseline postal questionnaires were sent to participants in the CHD, minor ailments and asthma modules and to controls for the latter two modules. All were piloted with the PCT’s ‘Reader Panel’ and members of the public to ensure that they were understandable and feasible. Follow-up questionnaires were sent to all intervention and control respondents at the end of the study.
For the CHD module comparisons were made with responses in a general population survey at the end of the study so there were no control data at baseline. The general population survey involved in-home interviews with respondents in a sample of 540 households (including a ‘booster’ sample of 40 mothers aged 20–29 years to obtain further feedback on the minor ailments module). The interviews were conducted by a market research agency.
For asthma respondents the postal survey questionnaire included the Mini Asthma Quality of Life Questionnaire (MiniAQLQ) (Juniper et al., Reference Juniper, Guyatt, Willan and Griffith1994; Reference Juniper, O’Byrne, Guyatt, Ferrie and King1999). Those who participated in the EPP were also asked to complete a pre-course questionnaire at the start of the final (seventh) session and a post-course questionnaire at the end of the final session, developed in conjunction with Asthma UK.
In the minor ailments module, a GP record audit was undertaken for 83 intervention participants and matched controls in the Minor Ailments module, to obtain numbers of consultations for the ailments included in the Pharmacy First scheme prior to and after registration with the service. Four focus groups were held with mothers in the target group for the Pharmacy First service (three with service users and one with non-users).
Telephone interviews using a pre-piloted structured interview schedule were conducted with 64 health care professionals at baseline, and with 51 at follow-up (GPs, pharmacists, health visitors and district/practice/school nurses) and an additional four practice managers. The self-care team within the PCT included the Chief Executive, Director for Primary Care, Head of the Prescribing Team, Patient and Public Involvement Manager, Associate Director of Health Improvements and Communications Officer and the Self-Care Programme Manager. Structured telephone interviews were conducted with nine PCT directors and managers at follow-up.
Study participants
For the intervention groups, patients were recruited for the prevention of CHD module using an invitation contained in a CHD information pack distributed by community pharmacies, the PCT and local employers.
Community-based promotion and GP invitation (nine practices) to adults diagnosed with ‘active’ asthma, i.e. who had recognized Read codes for asthma on their medical records and had received asthma medication within the last 12 months, were used for the ‘Staying Well with Asthma’ EPP-based programme. Respondents were allocated to the intervention or control group depending on whether they were willing to attend the asthma-specific EPP course. Respondents were also recruited via community-based promotion of two half-day asthma self-care sessions held in September and November 2005.
For the minor ailments module a GP invitation was sent to a sample of mothers whose children were registered for the ‘Pharmacy First’ scheme.
For the CHD prevention control group, a general population sample was used, excluding people who had participated in the intervention. Controls for the asthma module were those who responded to the GP invitation letter and did not want to participate in an asthma course. For the minor ailments module controls were sampled from mothers who had not yet had access to the Pharmacy First service but responded to an invitation to participate in the evaluation.
Health professionals
Three half-day educational events, targeted at general practices and called ‘A Partnership of Experts – Breaking the cycle of Dependency’, were provided. Practice visits and meetings were organized for general practices and community pharmacies. The PCT developed a Local Enhanced Service (LES) under the new GMS contract to establish systematic approaches within general practices for support of self-care. The specification followed the Quality and Outcomes Framework points system for payment, with points being allocated for a series of indicators.
Study PCT
The PCT has two main areas of population, with a total population of approximately 75 000. In 2004, 18% of the PCT’s population were aged 14 years or under, and 16% were aged 65 years or over, with a low black and minority ethnic population. There are 14 GP practices. At the start of JUSC there were 18 community pharmacies, and this increased to 20 as a result of changes in the control of entry regulations.
Ethical approval for the evaluation was received from South Derbyshire Research Ethics Committee. An application was also made to, and granted by, the local NHS Research and Development organization.
Data analysis
For the Minor Ailments and Asthma modules, once follow-up responses had been received, the control sample was matched to the intervention sample in each module on a number of key socio-demographic variables. Analysis then focused on change between baseline and follow-up in the intervention group compared to change in the control group using a paired t-test. This was seen as the most important comparison for the overall evaluation of JUSC and was applied to most of the data where means could be calculated.
Cross-sectional comparisons between the intervention and control groups were undertaken (at baseline and follow-up separately) using a χ 2-test. A χ 2-test was also used for data reporting frequencies or proportions. Statistical significance was taken as the 5% level (P-values < 0.05 represent significant differences between the intervention and control groups or between baseline and follow-up for an individual group).
Health professional attitudes, PCT management attitudes and focus group data on the Minor Ailments module were analysed qualitatively. The focus group data were coded from audiotapes using Atlas software. PMSI Healthcare undertook all data analysis, with advice from relevant members of the steering group. Qualitative data analysis was conducted using framework analysis (Ritchie and Spencer, Reference Ritchie and Spencer1993).
Results
The numbers of questionnaire respondents for each of the three JUSC modules are shown in Table 1. Response rates at follow-up ranged from 71% to 92%.
Table 1 Numbers of questionnaires issued and returned, by the Joining Up Self-Care (JUSC) module

CHD = coronary heart disease.
aFollow-up questionnaires were only issued to baseline respondents who provided address details.
bRespondents who attended an intervention session (a larger number returned the questionnaire but for logistical reasons not all were able to attend a course).
cAsthma intervention and control groups were not pre-selected.
dRespondent mothers, excluding duplicate responses for multiple children.
Coronary heart disease
The demographic profiles of respondents in the CHD intervention and control groups are shown in Table 2.
Table 2 Coronary heart disease – follow-up sample profile
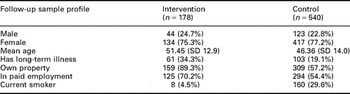
There were some differences between the two groups. The percentage of people with a long-term illness was almost twice as high in the intervention group (34% versus 19%). Respondents in the intervention group were more likely to own their own property and more likely to be in paid employment. The percentage of smokers in the general population survey was almost 30% compared with 4% in the intervention group at follow-up.
Lifestyle change in the intervention group was significantly higher than in the control group across four key risk factors – reduction of saturated fat in the diet, increased physical exercise, reduction of alcohol intake and smoking cessation (Table 3).
Table 3 Self-reported lifestyle change in intervention and control groups at follow-up

At follow-up, there was significantly more awareness of the JUSC programme in the intervention group compared to the general population. This was the case across both genders and all age groups. Over half the intervention group were aware of local self-care programmes, and 40% were aware of ‘something to do with heart disease’ compared to 1% of the general population. Less than 2% of either the intervention or the control group had sought advice from a pharmacist or called NHS Direct about their heart health, or bought a heart medicine (such as a statin) without prescription, at baseline or follow-up.
Asthma
The demographic profiles of respondents in the asthma intervention and matched control groups are shown in Table 4.
Table 4 Asthma – follow-up sample profile
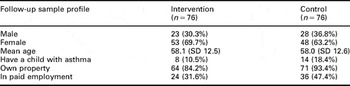
Participants in the intervention group were less likely to be in paid employment and less likely to own their own property compared with controls. In total 83 people participated in the intervention, 30 of whom attended a seven-week asthma-specific EPP course and 53 attended a half-day taster session on asthma. Participants’ mean age was 58 years, with matched controls. In the intervention group, participants’ asthma was slightly less well controlled at baseline than that of control group respondents. The most common reason reported by intervention respondents for seeing a health or social care professional at baseline was a chest infection. At follow-up, there was no significant difference between groups in numbers of GP consultations.
At follow-up there were significant increases in intervention respondents’ confidence in asking the GP questions about their asthma, and in discussing asthma openly with the GP compared with controls. There were also significant changes in attitudes towards asthma medication among intervention group participants compared with controls (Table 5).
Table 5 Confidence and attitudes towards asthma management at baseline and follow-up (1 = never, 6 = all the time; I = Intervention, C = Control)

Participants in the intervention group reported an increased appreciation of other things they could do (as well as using medication) to take care of their asthma and had become less worried about the side-effects of their medicines.
Participants’ responses to the experience of the asthma-specific EPP course (21 of whom responded) are shown in Figure 3.

Figure 3 Participants’ response to the asthma-specific Expert Patient Programme course (n = 21)
Course participants were positive about the benefits they felt they had obtained. They felt more knowledgeable about the treatments they used for their asthma, more confident that they would be able to discuss the ‘Stepwise’ programme for asthma with their doctor and more knowledgeable about what they could do to reduce their asthma symptoms. Spontaneous written comments indicated that, for some participants, the course appeared to have positive effects:
I learnt new things such as breathing exercises which I found did improve my symptoms.
We have learnt different things from each other.
I’ve learned more in the past few weeks than I have in the last fifteen years.
All 72 respondents to the questionnaire at asthma taster sessions rated the session as ‘good’ or ‘excellent’ and 40 (56%) said they would now be likely to attend an EPP course. When the asthma taster sessions were initially promoted, applicants were asked whether they had signed up for an EPP course, and if not why not. Of the 103 respondents, 51% said they felt they could take care of their asthma well and would not benefit from an EPP course, 29% said the day or time of the course was not suitable (often because they could not get time off work) and 23% said they would not have been able to attend all the sessions.
Minor ailments
Approximately one in five eligible families registered with the Pharmacy First service and over the period April 2005–March 2006, there were 1384 pharmacy consultations. Most (63%) were for children aged under 16 years, the most common condition being head lice. Most service users reported a positive experience and said they would continue to use the scheme.
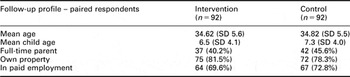
Key demographic characteristics were similar for intervention and controls (Table 6). We compared the responses and consulting behaviours of mothers with children who had used the ‘Pharmacy First’ service against controls who had not. The GP record audit data showed no significant difference between the intervention and control groups in numbers of GP consultations between baseline (the point at which intervention participants registered with Pharmacy First) and follow-up. There was a small increase in practice nurse consultations in the intervention group. Awareness of local efforts to promote self-care was higher amongst mothers aged 20–29 years (4%) than amongst the general population in the PCT. Amongst those who recalled any self-care support programme, ‘something to do with children’s minor ailments’ was cited by 38% of mothers.
Table 6 Minor ailments survey – follow-up sample profile
The focus group data indicated that many mothers were concerned not to ‘waste’ a GP’s time and sometimes needed support to decide whether a GP appointment was necessary:
I don’t like to think of the doctors being overstretched if it’s something I can deal with myself.
I’ve found myself apologising and saying ‘it’s been a couple of days now so I thought I ought to come.’
There are things you just don’t need to see the doctor for but you would like to speak to someone for a bit of professional advice.
They saw the pharmacist as a midway point between seeing a GP and treating a child themselves, and a source of decision support:
This (Pharmacy First) is like a little bit of a step in between.
I’d feel more confident going to the doctor and saying “the pharmacist suggested I came” .
The pharmacy was seen as a place where advice and treatment could be sourced more quickly and conveniently:
He is more accessible.
You don’t have to make an appointment – you can go at your convenience.
Mothers in the intervention group felt that the pharmacy service had developed a sense of how to use a pharmacist’s skills. There was some evidence that the pharmacy service had changed behaviour in becoming the first port of call:
If you’ve had that advice once you feel a bit more confident. You know which way to go, well I’ll go back to the pharmacist and I’ll know that if they can’t help me I’ll ring the doctor and know that I’m not wasting anyone’s time.
I always go to the pharmacy first…I’ll just explain and they’ll put me through to the doctor if they can’t help me.
However, participants felt first-time mothers would still be more likely to go to their GP and there was some dissatisfaction and misunderstanding in relation to the limited list of free medications that pharmacists could provide under the Pharmacy First scheme.
Healthcare professionals
At baseline many healthcare professionals believed that their consultations already included self-care advice:
I always did something like it but without the title.
I’ve always done something along those lines.
It tends to be what we do anyway.
It’s a slight change but basically what I was doing already.
Participants’ comments and the ensuing discussion at the JUSC ‘Self-care aware’ training sessions showed that there was neither a consistent approach within practices nor a coherent policy in practices for supporting self-care among all partners and staff in the practice around specific conditions.
Most healthcare professionals said they were comfortable about informing patients of their self-care options in CHD prevention, and care of asthma and children’s minor ailments. Existing self-care support was thought to be most effective in relation to care of minor ailments (Figure 4).

Figure 4 Healthcare professionals’ attitudes to self-care support at follow-up
There was high awareness of the Pharmacy First minor ailments scheme across all professional groups at baseline, and this increased at follow-up. There was also high awareness of the EPP amongst GPs, although at follow-up over three quarters of those who were aware of it only considered it ‘rarely’ for people with long-term conditions.
Respondents cited perceived barriers within the health service locally to further development of self-care support:
The whole game plan [in self-care] is lacking.
So many initiatives being thrown at GPs it’s hard to engage them.
Delivery methods to get information to patients need to be looked at.
Organizational development
The respondents agreed that support for self-care is a legitimate activity for the organization. Involvement in the JUSC programme was said to have raised the profile of self-care within the PCT, leading to work being undertaken on a strategy for future support for self-care. Respondents said, however, that effective cross-directorate working on self-care had not been achieved. This was partly attributed to the ongoing merger of the PCT and also to a perceived lack of Director-level involvement in leading integration of self-care work within the organization.
Respondents thought that the JUSC programme would have a lasting effect on the PCT, although there was a concern that organizational memory would be diminished by the changes resulting from NHS reorganization. When asked what other PCTs might do strategically to support self-care, respondents suggested that self-care needs to be established within PCTs as strategically important with a clear management framework including identification of appropriate skills and accountabilities. Reflecting on JUSC, respondents identified several principles for the future: agreeing to a ‘vision’ for where self-care support is going within the PCT and then specifying priority areas, including some ‘early wins’; establishing a task group within the PCT, including Director-level support as well as senior operational managers, to implement a self-care support programme; getting all stakeholders signed up at the start (including the Strategic Health Authority, PCT Director of Public Health, Local Representative Committees, Professional Executive Committee, Practice-based Commissioning leads, GPs and community and voluntary groups) in order to promote shared ownership of the programme; find, develop and work with lay and professional champions; and use contractual and other levers to incentivise care professionals.
Discussion
While several existing Department of Health, NHS and community-based initiatives involve and relate to supporting self-care, at the time of the JUSC programme research had shown that these are not ‘joined-up’ in a whole systems approach at the local level (Blenkinsopp and Dost, Reference Blenkinsopp and Dost2005; Reference Blenkinsopp and Dost2006). JUSC attempted to demonstrate how a PCT, working with local clinicians and community stakeholders, could provide support for self-care. The evaluation used a pragmatic case-control type design to investigate the impact of three self-care intervention modules organized by the PCT.
Participant response rates at follow-up were excellent, providing data from more than 70% of participants in each module. The evaluation found changes associated with each of the three JUSC modules. In CHD prevention, participants reported making significantly more lifestyle changes to reduce their risk of CHD. People who participated in the asthma self-care skills training were more confident in asking questions and discussing their asthma with the GP. They also knew more about things other than medication that they could do to control their asthma, and were less concerned about possible side effects from asthma medicines. The asthma programme did not change overall attitudes towards coping with, or wanting to take control of, asthma. Parents who used the Pharmacy First service were mostly positive about their experience and were more likely to state an intention to consult a pharmacist about minor ailments before seeking a GP consultation. They also reported feeling more confident about self-care for certain minor ailments without input from a health professional. There was some evidence from the general population survey of awareness of some of the JUSC modules but we did not ask respondents whether they identified these as being parts of a wider programme.
In the use of health services, participants in the CHD module were more likely to have seen a GP about heart health during the JUSC programme. There was a small but significant increase in numbers of GP consultations in the asthma intervention group; this may be associated with the poorer levels of asthma control seen at baseline compared with the controls, and also the higher level of change in their condition (at follow-up) as perceived by the intervention participants. The short follow-up period meant it was not possible to determine whether this increase was transient or sustained. There were no significant differences in the numbers of GP consultations for minor ailments between the intervention and control groups.
The JUSC programme was therefore associated with greater change in attitudes than in behaviours. The challenges inherent in attempting to change behaviour are well known, and changes in attitudes are an important prerequisite to changes in behaviour. The limitations of the evaluation include the shortness of the timeframe, during which it might be optimistic to expect to witness significant changes in levels or patterns of demand for particular services. However, the effects of interventions also decline over time without reinforcement and so sustained inputs would be important for longer-term evaluations. It is also likely that there was preferential participation by those motivated to change, also a finding from previous research on participation in self-management programmes (Bury et al., Reference Bury, Newbould and Taylor2005). It proved difficult to achieve wide community involvement in CHD risk reduction. A self-selected group took up the JUSC interventions, and those who did so were more affluent than those who did not. During the course of JUSC the PCT undertook an active programme of establishing links to local employers, who showed considerable interest and subsequently were active distributors of information about the CHD module in the workplace. Nevertheless, the findings indicate at least some of the issues and opportunities to be tackled by PCTs in developing self-care.
Recruiting participants to the asthma EPP courses proved particularly challenging. This in part reflected the logistical difficulties in organizing the courses at times convenient to patients, and the time commitment required from participants. These problems were not unique to JUSC and a national study conducted at the time found that only a quarter of PCTs had ‘good’ rates of recruitment (Kennedy et al., Reference Kennedy, Rogers and Gately2005). In the national study problems with recruitment were associated with a reliance on a paper-based strategy and poorly developed links to the broader community and health professionals. To our knowledge the JUSC programme was the first to use direct mailing (a letter of invitation from the GP was used) as a local recruitment strategy for EPP but this was not sufficiently effective in recruiting patients to justify the level of resource required. Recruiting to an EPP in a PCT, which does not yet have well-established community contacts and networks, required significant input from the PCT in terms of both organization and explanation. There were 30 participants for the EPP course, compared with the target of 100, and the time gap between baseline and follow-up was much shorter than originally planned. It is therefore not possible to draw definitive conclusions about the effectiveness of the course. The qualitative data however strongly suggest that the EPP course had a positive impact on participants. The asthma ‘taster’ sessions were found useful in their own right by participants besides being effective in recruiting people to the EPP course. However, the level of understanding and engagement of health professionals with EPP has been questioned (see, for example, Blakeman et al., Reference Blakeman, Macdonald, Bower, Gately and Chew-Graham2006).
The Pharmacy First service achieved registration levels of around one in five families, compared with a similar Scottish service, where a steady state of registrations appeared to have been reached after two years with 26.5% of people registered in one area and 5.6% in another (Sheehy and Jones, Reference Sheehy and Jones2003). Local practices’ commitment to promoting the service was thought by the Scottish researchers to be the reason for differential enrolment in the two areas. The Pharmacy First service in JUSC was well accepted as a way of accessing primary care. With the exception of younger mothers, respondents in both intervention and control groups said they were more likely to consult a pharmacist in the future. Trends towards use of self-care for several childhood minor ailments were slightly greater in the Pharmacy First group. Unfortunately it was not possible to directly link GP and Pharmacy First consultations for the episodes of illness. This and the fact that steady state had not yet been reached and registrations were still increasing indicate that it was not possible to draw conclusions about the effect on GP workload. The information booklets on minor ailments were widely distributed but the evaluation was not able to determine how they were used. Overall the minor ailments module in JUSC showed the potential for changing the perceived roles of health professionals. It did not, however, provide evidence of any increase in participants’ self-efficacy in minor ailments management.
Health care professionals perceived opportunities for self-care to be further encouraged and supported. Many thought they were already practicing support for self-care but at the same time many also said it was a role they could not take on due to other workload pressures. Local self-care support services were well known at the end of the study but health professionals rarely reported referring patients to them. These findings indicate a gap between professionals’ self-perception and their actual practice.
There is some evidence that GPs perceive a conflict between encouraging more self-care and fulfilling their own professional obligations, which may at least partly explain our findings (Blakeman et al., Reference Blakeman, Macdonald, Bower, Gately and Chew-Graham2006). Research has also shown that different health professional groups appear to have a relatively greater or lesser level of comfort in encouraging self-care. In one study, nurses were the least likely to be supportive, with GPs and physiotherapists relatively more positive (Wilson et al., Reference Wilson, Kendall and Brooks2006). In a study of patient engagement with their health care in six countries patients reported lower levels of support for self-care from health professionals in the UK than in almost all of the other five countries (Coulter, Reference Coulter2006). Many of the participants in an EPP programme reported ‘doctors devaluing through negation or sidelining the new expertise of the patient’ (Wilson et al., Reference Wilson, Kendall and Brooks2007). Given that health professionals’ endorsement is a key influence for many patients, further work is needed to explore the underlying attitudes and concerns of health professionals and work towards finding ways to address them.
Contractual levers such as LESs in general practice and pharmacy could be instrumental in changing these attitudes, as demonstrated by the 100% uptake of the self-care LES by general practices. The Essential Services component of the pharmacy contract already includes support for self-care in relation to public health, long-term conditions and minor ailments. PCTs could build on this by using mechanisms such as a cross-team primary care LES for self-care involving both pharmacists and GPs. Incentives for support of self-care could be further strengthened with a nationally directed Enhanced Service framework for GPs and pharmacists through their contracts. Ways of influencing contracts for midwives, district nurses and health visitors need to be similarly explored.
Embedding self-care support into existing organizational structures presented challenges for the PCT. Securing maximum effectiveness from a strategy to support self-care depends on adding up existing resources, mechanisms and programmes. Our findings show that an effective self-care support programme requires champions at all levels within the organization and that a cultural shift is likely to be needed if self-care is to become an integral part of PCT policy and translated into coordinated action on the ground. The JUSC evaluation suggests that other mechanisms, in addition to the involvement of health professionals, have to be utilized in order to generate attitudinal change at the community level. PCTs need to view self-care support as requiring community-wide engagement, developing and sustaining relationships with other actors, including local employers, schools, social services, the voluntary sector, the media and ‘civil society’Footnote 3 rather than health service initiatives alone. There also needs to be a much greater recognition of the need for cross-agency working to target communities as a whole, beyond their interactions with the NHS. As health and social care commissioning come together, there is also potential for the development of joint strategies.
To our knowledge, the JUSC programme is the first in which a PCT has provided self-care support for the public across a spectrum of self-care areas with associated training for primary care teams. A limitation of the study was that although information about the three individual JUSC modules was promoted to the public, there was not a public information campaign to explain how they were connected or to explain the underlying thinking. Although the ‘Self-Care Aware’ sessions for primary care teams provided a forum for discussion and questioning beyond professionals’ beliefs that they were already ‘doing’ self-care, clearly more was needed. More recent work by the Working in Partnership Programme has built on JUSC by testing the effects of a training course on self-care for members of the public and of practice-led training for health professionals in self-care support (Leeds Metropolitan University, 2008). These studies have the potential to shed further light on the complex areas of public and professional understanding and activity in relation to self-care.
Conclusion
The evaluation demonstrated the potential for coordinated self-care support and promotion at the PCT level, and also the challenges of doing this widely and effectively. In primary prevention of CHD, significant behavioural change aimed at risk reduction was reported by more affluent patients, many of whom were already interacting with the health service. In the care of people with asthma and children’s minor ailments, patients’ and mothers’ confidence improved significantly. The JUSC programme showed that an NHS focus, even where some parts of the programme were delivered in community settings, inevitably has limitations in reaching people if they are not ready to think about their health or are not already interacting with the health service. Integration of self-care across different directorates in the PCT was not achieved. Key principles for PCTs to include in self-care strategies in the future were identified.
Acknowledgements
The evaluation was funded by the Working in Partnership Programme of the Department of Health. We would like to thank the staff of Erewash PCT for their contribution and commitment to JUSC during a time of rapid change within the NHS. Our steering group provided advice and guidance throughout the programme and we are grateful for their input.












