Introduction Background
The traditional features of primary care (PC) are: longitudinal comprehensive care for the individuals, mobilizing sources of community support, advocacy both for and against governance as the personal and particular circumstances require (Meads, Reference Meads2006; Hummers-Pradier et al., Reference Hummers-Pradier, Beyer, Chevallier, Eilat-Tsanani, Lionis, Peremans, Petek, Rurik, Soler, Stoffers, Topsever, Ungan and van Royen2009). Several previous studies have shown that in countries where the PC system is stronger, the healthcare system performs better (Starfield, Reference Starfield1994; De Maeseneer et al., Reference De Maeseneer, De Prins and Gosset2003; Macinko, Starfield & Shi, Reference Macinko, Starfield and Shi2003; Schellevis et al., Reference Schellevis, Westert and De Bakker2005; Schäfer et al., Reference Schäfer, Boerma, van den Berg, De Maeseneer, De Rosis, Detollenaere, Greß, Heinemann, van Loenen, Murante, Pavlič, Seghieri, Vainieri, Willems and Groenewegen2019). Health services research often focuses to describe what kind of structures of primary health care systems are associated with better health outcomes, in terms of quality, equity, and costs. Appropriate data collection is needed on the essential features of the structure and delivery of PC services in many countries (Kringos et al., Reference Kringos, Boerma and Bourgueil2010; Kringos, Reference Kringos2012; Schäfer et al., Reference Schäfer, Boerma, Kringos, De Ryck, Heinemann, Greß, Murante, Rotar-Pavliⓒ, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013). There are different types of organizations in PC systems in Europe, therefore analyses of the relationship between delivery of PC service and health outcomes are very important (Delnoij et al., Reference Delnoij, Van Merode and Paulus2000; Schellevis et al., Reference Schellevis, Westert and De Bakker2005; Ashworth & Armstrong, Reference Ashworth and Armstrong2006; Zebiene et al., Reference Zebiene, Švab and Sapoka2008; Kringos et al., Reference Kringos, Boerma and Bourgueil2010; Schäfer et al., Reference Schäfer, Groenewegen, Hansen and Black2011; Reference Schäfer, Boerma, Kringos, De Ryck, Heinemann, Greß, Murante, Rotar-Pavliⓒ, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013; World Health Orgaisation (WHO), 2016).
To analyze these relations the Quality and Costs of Primary Care in Europe (QUALICOPC) study was designed to describe and to compare how the primary health care systems of 35 countries perform in terms of quality, costs, and equity. The findings and results of the study are expected to give evidence on the benefits of strong primary health care and on the performance of health care systems in general (Schäfer et al., Reference Schäfer, Boerma, Kringos, De Ryck, Heinemann, Greß, Murante, Rotar-Pavliⓒ, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013). While family physicians/general practitioners (GPs) are the main providers of primary health care, they were involved in the study as survey subjects. The expectations and experiences of patients were also surveyed in other questionnaires, which were not included in our recent study (Kringos, Reference Kringos2012; Schäfer et al., Reference Schäfer, Boerma, Kringos, De Ryck, Heinemann, Greß, Murante, Rotar-Pavliⓒ, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013).
Ten dimensions were chosen as indicators to measure primary health care: governance and economic conditions of the PC system, PC workforce development (structure); access to PC services, continuity, coordination, and comprehensiveness of PC services (process); quality, efficiency of PC, and equity in health (outcome indicators).
The researchers of the QUALICOPC Consortium have developed four questionnaires; a questionnaire for GPs, another to describe the infrastructure and technical provision of services (Practice questionnaire), filled in by fieldworkers and two questionnaires for PC patients: Patients values, and Patients’ experiences (Schäfer et al., Reference Schäfer, Boerma, Kringos, De Ryck, Heinemann, Greß, Murante, Rotar-Pavliⓒ, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013). All these questionnaires were previously tested and validated (Kringos, Reference Kringos2012; Schäfer et al., Reference Schäfer, Boerma, Kringos, De Ryck, Heinemann, Greß, Murante, Rotar-Pavliⓒ, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013).
In each country, the response target was 220 GPs and 2200 patients. The questionnaires were translated into national languages via an official forward- and back-translation procedure. The study was completed in 32 European and three overseas countries (Australia, Canada, and New Zealand) (Kringos, Reference Kringos2012).
While a similar wide-range evaluation has never been performed earlier in Hungary, the study offered an excellent option for data collection and investigation within the national PC settings.
Aims
This paper targets to provide selected data of the Hungarian-arm of the QUALICOPC study and provide an overview about the recent Hungarian PC system.
Methods
Two questionnaires were distributed, from a total of the four developed for the study.
1. Practice questionnaire
A practice questionnaire, with 12 questions was developed to measure the practice-related indicators, to describe the impressions of patients or visitors on infrastructure, their comfort level in the waiting area, the communication of opening hours, and the equity of access (eg, for handicapped persons). These were filled by the fieldworkers.
2. GP questionnaire
It contained 60 questions (pre-structured multiple choice answers and options of numerical answers), on the background and characteristics of the practice, additional professional activities and time allocation of the GP, job satisfaction, workforce development, efficiency, economic conditions, continuity and accessibility of care, coordination and cooperation, referral, medical record keeping, quality and comprehensiveness of services, equity in accesses, available equipment, task profiles, use of guidelines, and feedback received from colleagues or the authorities.
The study center of the Hungarian arm of the QUALICOPC project was established at the University of Debrecen, with close collaboration with the other three departments, based on the other Hungarian Medical Faculties (Budapest, Pécs, Szeged). Advertisements were published to recruit participating GPs in the whole country. GPs who wanted to contribute were selected randomly from 310 applicants, but the requisite geographic representativeness was also considered.
All of the questionnaires were transported to the practices by fieldworkers, most of whom were medical students. The patients involved were contacted directly and consecutively in the waiting area by the fieldworkers. They had three tasks: (1) Recruiting patients to fill in the patients’ questionnaires; (2) To check and evaluate the infrastructure of PC facilities filling in the Practice questionnaire; and (3) Distribution of the GPs questionnaires to the family physicians who posted them back to the study center after completing.
Presentation of data, statistics
Although the original order of questions in the QUALICOPC study was usually followed, few sub-chapters were formed to summarize the answers thematically. Mainly distributions are presented. Some columns, where similar answer options were given, were merged, which is always indicated in the text. Descriptive analysis was performed the data using STATA software.
Results
Practice questionnaire
Recruitment of patients in the waiting room was successful, only 25% refusal was recorded. Opening hours were clearly indicated in 91% of the doctors’ offices while out-of-hours care was advertised in 88%. Eighty-eight percent of practices were located on the ground floor, 54% in multilevel buildings, having inbuilt elevators. Half of them offered free parking facilities for handicapped visitors and toilets accessible by wheelchair.
The cleanliness of facilities was evaluated as very clean (45%) and rather clean (54%).
Intimacy was appropriately provided. Doors were usually closed in the waiting room, 80% of visitors did not hear what is being said at the reception desk and 94% could not hear or see what was happening in the doctor’s office.
GP questionnaire
Altogether 222 questionnaires were completed, by 118 (53%) male and by 104 (47%) female family physicians/GPs. Answers are presented mainly according to the order of questionnaire.
The mean of their age was 53.4 (SD ± 10.9) years. Ninety two percent of them were born in Hungary, others come mainly from the neighboring countries, where high density of Hungarian population is living (ie, Ukraine, Romania).
Location and composition of practices
Most of the practices (31%) were in big (inner) cities, 8.6% in suburbs, 20.3% in (small) towns, 28.4%. in rural and 11.3% in mixed urban–rural locations. The mean of the practice population (number of enrolled patients) were 1857(± 912) persons. Comparing to the national distribution, they rated the ratio of elderly people (over 70 years) in the practice as average (46.9%), above (39.2%) or 9% below average. Ratio of socially disadvantaged people was estimated as average (38%), above averages (42%), and below average (18.5%). A quarter of family physician estimated that ratio of ethnic minority patients are closely to their national representatives, while 52% expected higher, 20% believed lower figures.
Most of the doctors considered the turnover of the patients enrolled in the practice, as average (57%) and 37% below average.
Workload
The means of weekly working hours were 37.7(± 8.6), GPs spent 31.5(± 8.7) hours with direct consultations, home visits, and telephone consultations. Doctors above 55 years worked longer 39.1(± 7.5) hours/week, while younger (below 55 years) spent 36.1(± 9.5) hours only (P = 0.059). There were no differences between genders. The reported means of face-to-face consultations were 50.4(± 16.1) patients per working days. Besides these, 11.7(± 7.9) patients needed telephone consultations, while 0.9(± 0.6) persons were contacted by e-mails. Average patient consultations lasted 8.2(± 5.4) minutes. Participating family physicians done 14.5(± 13.1) home visits per week, 5.7(± 4.5) for elderly patients and 1.9(± 1.3) institutionalized patients were visited in other settings.
In the past three working months, they reported 4.8(± 3.9) night and 1.5(± 1.2) weekend day shifts.
The highest part of GPs (86.5%) was working alone, or in shared accommodation with other GPs (11.3%) or medical specialists (4.1%).
GPs were rarely away from their practices. Their vacation lasted 2.6(± 1.4) weeks, attended conference or educational activities in 1.2(± 1.1) weeks, yearly.
Sick leave lasted for 0.45(± 0.2) weeks a year; even less participation on scientific events were reported 0.4(± 0.4) weeks.
Financing
Beside their daily work in the family practice, 33% of GPs had no other remunerated activities, while 7% worked as company doctor (occupational health), 41% of them performed teaching activities, mainly medical education. Almost all the practicing GPs (93%) were working as a self-employed, contracted with the National Health Insurance Fund and local municipalities, 2% were self-employed without contract and 3.2% was a salaried employee.
The financing of GPs from the National Health Insurance Fund is based mainly on capitation, representing 52.9(± 32.7)% as mean of estimated income. Fee for service activities represented 9.6(± 8.3)%, performance payment 5.0(± 4.8)%, while out of pocket payments 4.7(± 3.6)%. Other financial resources were mentioned in 11.8(± 11.4)%.
There are additional elements (quality indicators), represented in the financing. For the proper diabetes care 19.4% of GPs get a financial bonus, 37.8% for reaching the targeted screening activities, 21.6% for the proper referral rate and 5.9% for working in remote areas.
Professional competences
Applied clinical guidelines are widely known and used by GPs (chronic heart failure in 70%, asthma in 65%, diabetes in 79%, and COPD (Chronic Obstructive Pulmonary Disease) in 64%), although there are no specific PC-oriented guidelines available. Feedback regarding prescriptions is usually provided by the insurer (73%), less by health authority.
In case of referrals, the preference of patients is mainly considered (in 60%), while 35% of GPs prefer own decision, not shared with the patients.
The available devices and equipment’s in the questioned practices are listed in Table 1.
Table 1. Available devices and equipment’s in practices
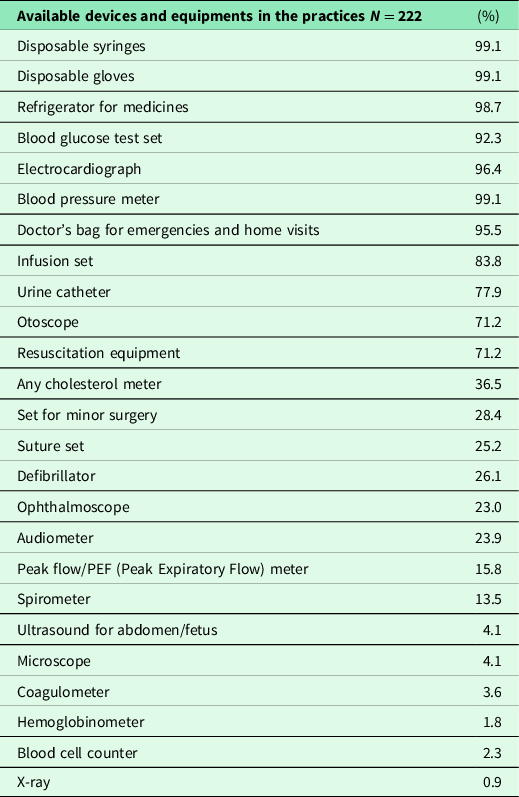
Regarding location of X-ray facility, it can be reached in the same building (4%) where the practice is located, 89% are accessible easily, only 7% are too far. The nearest GP practice was in the same building (39%), within a distance of 10 km (55%). The nearest outpatient’s clinic was in the same building (10%), or less than 10 km (57%). Half of the nearest hospitals were also within this range.
The questioned practices offered 6.7(± 3.5) opening hours on weekdays. Consultations in the evening, access to the practices after opening hours was quite different, although 32% were still open after 18 h (6 pm). On a rota basis, availability was reported by between 11% and 18% of them, while 14% of GPs were always available for their patients, even at weekends. Most of the hospital-based emergency and center-based non-emergency services are run by other physicians.
Recently, 23(± 23)% of GPs provide consultations by appointment and 59(± 39)% offer a walk-in hour.
Almost all of the GPs prescribe cheaper equivalent drugs (generics) and 87(± 11)% provide free samples of medication, if available. Doctors estimated that 13% of patients are frequently and 61% of them are occasionally delaying their visits for financial reasons.
Enrolment into the practice
Almost half (48%) of the new patients, entering the practices provided their medical records or these documentations were sent by the previous GP, while 41% of them enrolled without handling previous files. Thirty four percent refuse patients from other geographical area, 43% never use any restriction, 5% consider the past medical history of patients and 12% of GPs respect the number of their enrolled patients to avoid financial restrictions.
Forty one percent of family physicians always accept non-insured patients, but 24% of them only in case of emergency.
Cooperation with other specialists, referrals
The previous experience of GPs is the determining factor in case of referrals (by 58%), other points of view which are always considered: travel distance for the patients (42%), patient’s own preference (37%), expected waiting time (39%), comparative information on the specialist getting from other patients (22%), and cost for the patients (46%).
Practice nurse is employed by 95% of GPs, other health care professionals in a much less extent: receptionist (28%), midwife (0.5%), and laboratory assistant (2.2%). In the same centers where the questioned GPs worked, other professionals were also available: home care nurse (7.7%), psychiatric nurse (1.8%), dentist (4.5%), pharmacists (2%), social workers (4.1%), and practice manager (1%).
Practice nurses independently give immunization/vaccination (in 70% of practices), provide advice regarding health promotion, lifestyle, smoking cessation (in 83%), check routinely chronically ill patients (80%), and perform minor procedures (ear syringing, wound treatment) (in 83%).
Referral letters (including findings, provisional diagnosis, and test results) are written by 48% of GPs for all, by 41% for most, and by 10% for the minority of the patient. After consultation with specialist, treatment or diagnosis of the patients is told always (40%), usually (25%), seldom, or never (25%).
After a patient has been discharged from the hospital, 81% of doctors receive summary/discharge report within 1–4 days and 5% of them within 5–4 days. The remaining 13% complained that it never or only rarely arrives.
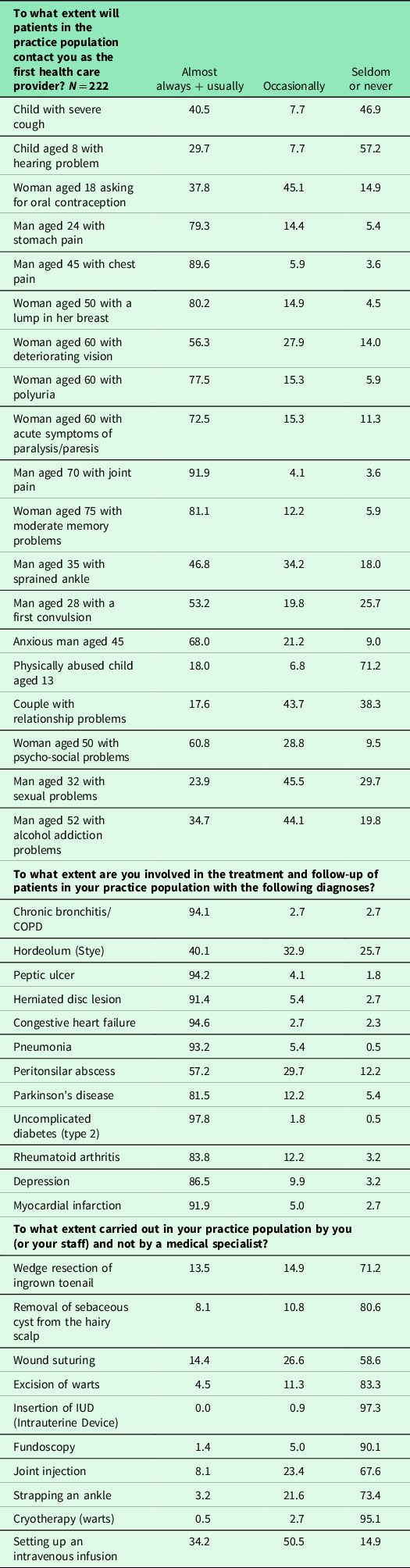
Hungarian GPs are involved in the management of almost every chronic disease (diabetes, hypertension, cardiovascular, musculoskeletal, mental disorders) and even palliative care. When procedures or interventions are required, these are usually provided by surgical specialists (urologist, ENT, etc.). Some examples were offered in the questionnaire, and doctors were asked how frequently they are involved in these or similar cases. Ratios are presented in Table 2.
Table 2. Professional competences of GPs
All Hungarian PC practices are using computers, with specific software for GPs. The functions and recorded data are presented in Table 3.
Table 3. Recorded data in the electronic medical system
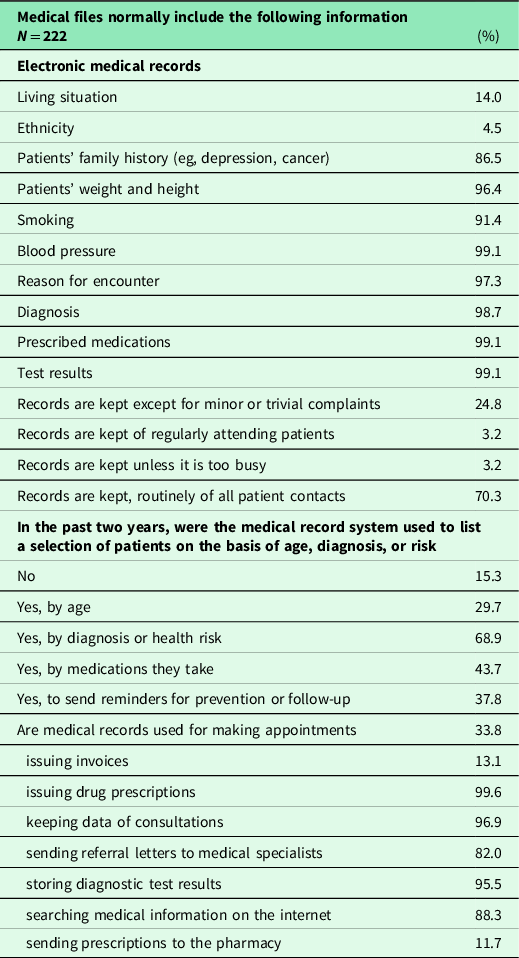
Blood pressure is usually measured by the staff, regardless of the reason for visit (79.3%). Advices regarding the cessation of smoking, diet, physical activity, and misuse of alcohol are the most frequent topics of life-style consultations, discussed with the patients in about 90%. Family physicians are routinely involved in antenatal care (51%), in immunizations (29%), and paediatric surveillance of children, influenza vaccination (96%), and palliative care (87%).
Occupational health problems are rarely discussed with family physicians including accidents at the workplace. If doctors diagnose frequent respiratory problems, repeated cases of food poisoning among people living in a certain district, they usually report them to the relevant authority.
Burn out
Job related stress was mentioned by 27(± 24.3)% of the responding GPs, overloading with unnecessary administrative tasks by 48.2(± 36.6)%. Half (54%) of them estimate their job as still interesting, while only 13% believe that GPs have well-respected jobs and even less (2.2%) found a good balance between effort and reward. There were no significant differences between genders or the length of time in practice.
Discussion
Main findings
The Hungarian family physicians have wide-ranging professional competences, but not appropriately regulated. The ‘gate-keeping’ is symbolic. The requisite infrastructure, devices, and equipment are generally available. Single-handed practices are predominant. The capitation-based financing is insufficient; therefore, additional income is often needed.
Study limitations and strengths
In the original questionnaires, more answer options were offered, but we had to merge those where only a few answers were received, to make the presentations easier (Schäfer et al., Reference Schäfer, Boerma, Kringos, De Ryck, Heinemann, Greß, Murante, Rotar-Pavliⓒ, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013).
Questions used in the study-questionnaires could have different meaning for GPs working in different national systems, especially regarding the respective structures of practice, ethnic minorities, insurance system, and remuneration.
Whether a GP was a salaried employee or self-employed private practitioner was not differentiated by the questionnaire. This may be relevant with respect to the assessment of personal income.
After development of the questionnaires, there were no options to modify them according to national characteristics or to add national-specific questions. Some of the missed topics are explained later.
The presentations of data within other respective national publications of the QUALICOPC study were very different and most of them had narrower focus, only limited comparison could be made in this paper.
There are strengths of this study as well. Due to the validated method and uniform questionnaires, we are able to present the actual state of the Hungarian PC system, including changes made after the study finished. Combined with other data and information published, it provides a comprehensive updated description, suitable for international comparison.
Nationally and geographically representative data were collected provided from 3.4% of all (6.400) GPs. Their mean of age was two years lower than the national average.
Description of the recent Hungarian system, some information about its history and actual trends were also discussed here, together with the findings of the QUALICOPC survey.
All the Hungarian GPs are overburdened by the volume of administrative tasks, although the majority of them still like and enjoy their profession. They are usually working longer hours than their Dutch colleagues and almost the same as providers in the UK (Kringos et al., Reference Kringos, Boerma and Bourgueil2010). There were no visible differences between the levels of urbanization and number of working hours such as in Austria, in the neighborhood and in most of the participating countries where GPs working in rural areas have significantly higher workloads and provide more medical procedures to their patients (Hoffmann et al., Reference Hoffmann, Wojczewski, George, Schäfer and Maier2015; Groenewegen et al., Reference Groenewegen, Bosmans, Boerma and Spreeuwenberg2020).
The funding by the National Health Insurance Fund is based mainly on capitation, with additional elements and minor quality incentives introduced a few years ago. Payment in Hungary is far from the ‘West European’ remuneration. While it was increased in the past few years, its value is only about 30%–40% of the income of GPs in the Netherlands and the UK (Kringos, Reference Kringos2012). Financial incentives to improve the quality of service provision represent only about 5% of remuneration, with low effectiveness (Rurik, Reference Rurik2009; Balogh, Reference Balogh2019). The whole PC provision is covered by the National Health Insurance Fund, but there are limited numbers of services that the patients had to pay for (ie, issuing driver’s permit, some type of certifications). Overall, the personal income from the governmental financing is considered insufficient, thus many GPs are involved in alternative activities to generate extra revenue. Occupational medicine is one of the favourite part time jobs for GPs.
After the democratic changes in Hungary (1990), the politico-economic system and the legal circumstances have changed significantly. There were initiatives for privatization also in the health care system. Family physicians were the first who got a right to establish their own enterprises based on two contracts, one with the National Health Insurance Fund for financing and the other with the local municipalities for provision of PC within a geographically defined area. Since 1992, patients can choose a GP out with their catchment area. GPs are obliged to enrol all inhabitants living there, and are entitled to accept others from outside (Kolozsvári & Rurik, Reference Kolozsvári and Rurik2016).
Almost all of the Hungarian practices are single handed. Its ratio is above 50% in Austria, the Czech Republic, Germany, Greece, Slovakia, while less than 25% in Portugal, Spain, Turkey, in the Scandinavian countries, and in the UK (Schäfer et al., Reference Schäfer, Boerma, van den Berg, De Maeseneer, De Rosis, Detollenaere, Greß, Heinemann, van Loenen, Murante, Pavlič, Seghieri, Vainieri, Willems and Groenewegen2019).
For patients, enrolment into a practice is an easy procedure; they have a right to change doctors, without explanation and any legal or financial consequences.
The available instrumentation, devices, and professional competences of Hungarian PC providers are similar to those of the majority of GPs in EU member states, who are well equipped and can provide a wide range of medical services, with a substantial variation between countries (Eide et al., Reference Eide, Straand, Björkelund, Kosunen, Thorgeirsson, Vedsted and Rosvold2017). There were no specific questions about the routine usage of these instruments. In most of the ‘QUALICOPC countries’, rural practices are offering a broader range of services, such as medical procedures (Groenewegen et al., Reference Groenewegen, Bosmans, Boerma and Spreeuwenberg2020).
The ‘gate-keeping’ is light, without appropriate financial interest. Gate keeping of rural doctors does not differ significantly from urban based practices. Using referral letters by GP to specialist for all of the patients (44%) was higher than in Italy or Germany (about 10%), but lower than in the UK (95%). Feedback come from the specialist almost always (38%) was higher than in Austria, Greece, Germany (below 10%), but much lower than in Norway or the UK (about 75%) (Scaioli et al., Reference Scaioli, Schäfer, Boerma, Spreeuwenberg, Schellevis and Groenewegen2020).
Shared decision-making (SDM) is ideally a treatment decision making process. GPs in gatekeeper systems frequently consider patient interests, while in non-gate keeping countries GPs prefer more often own experience with specialists as benchmarking information (Rotar et al., Reference Rotar, Van Den Berg, Schäfer, Kringos and Klazinga2018). Hungarian GPs are better inclined to SDM, using mostly their experiences on previous referrals. In European context, the patients questioned in the same study about the shared involvement of decision making reported lower improvement potential in Hungary, Germany, UK, and Turkey, while it was higher by patients in Portugal, Italy, Poland, and Greece (Schäfer et al., Reference Schäfer, Boerma, van den Berg, De Maeseneer, De Rosis, Detollenaere, Greß, Heinemann, van Loenen, Murante, Pavlič, Seghieri, Vainieri, Willems and Groenewegen2019).
Price of the prescriptions became an issue for Hungarian patients only in the last decades, and GPs are aware it. There are many drugs, mainly innovative and expensive medications, when reimbursements are different. Prescribed by specialists, patients should pay less (Jermendy et al., Reference Jermendy, Kiss, Rokszin, Abonyi-Tóth, Wittmann and Kempler2017). This regulation does not help the competences of GPs.
Earlier, appointment-systems at GPs were not routinely implemented in Hungary, by now it has become more popular, mainly among better-educated and urban patients. Scheduled consultations are offered by Hungarian GPs as well, but to a lesser extent than in the Finish arm of the study, where it is almost universal (Tolvanen et al., Reference Tolvanen, Koskela, Mattila and Kosunen2018).
According to the legislations, GPs have to provide at least four hours for personal consultation with patients, every workday. When the offices of GPs are closed, out of hours services are available for the inhabitants, but the type and involvement of GPs is different. The organization of emergency services is not uniform; it is dependent on the contracts between the service providers and the local municipalities. In the other participating countries, patient’s reported visits at emergency department varied between 18% and 43%, while these figures were 33% in Hungary (Schäfer et al., Reference Schäfer, Boerma, van den Berg, De Maeseneer, De Rosis, Detollenaere, Greß, Heinemann, van Loenen, Murante, Pavlič, Seghieri, Vainieri, Willems and Groenewegen2019).
All Hungarian GP practices have been computerized since 1997, wide variety of data are recorded and reported to the National Health Insurance Fund. It does not provide universal (free) software, this has to be procured buy from profit-oriented IT companies. A ‘cloud based’ internet connection was established in 2017, in order to serve and connect the whole national health care system, but data upload and accesses are yet insufficient. Based on the findings of the QUALICOPC study, more effort is needed in Southern and Central-Eastern Europe, to decrease gaps in the adoption of IT services and to facilitate the interconnection of the health care systems (De Rosis & Seghieri, Reference De Rosis and Seghieri2015).
Community orientation was found more frequently within countries having a list system, among self-employed GPs, those using medical records to make overviews, and is more active in prevention and multidisciplinary cooperation. Rural GPs and areas with more people from ethnic minorities are more community oriented (Vermeulen et al., Reference Vermeulen, Schäfer, Pavlic and Groenewegen2018). In the other participating countries, community orientation was rated as low in Hungary, in Portugal, in Germany, and in Ireland while it was higher in Italy, in Spain, in Turkey, and in the UK (Schäfer et al., Reference Schäfer, Boerma, van den Berg, De Maeseneer, De Rosis, Detollenaere, Greß, Heinemann, van Loenen, Murante, Pavlič, Seghieri, Vainieri, Willems and Groenewegen2019).
Ethnic minorities are represented in Hungary by the Roma population only, although it is forbidden by legislations to register ethnicity in medical files. They have more morbidities and visible lower life expectancies (Sándor et al., Reference Sándor, Pálinkás, Vincze, Sipos, Kovács, Jenei, Falusi, Pál, Kőrösi, Papp and Ádány2018).
Based on the variation between the 35 participating countries and their GPs, the importance of multidisciplinary cooperation should be emphasized (Vermeulen et al., Reference Vermeulen, Schäfer, Pavlic and Groenewegen2018). This cooperation facilitated a broader variety of technical procedures, wider coordination with secondary care, and increased collaboration among different providers (Bonciani et al., Reference Bonciani, Schäfer, Barsanti, Heinemann and Groenewegen2018). Unfortunately, the screening opportunities (secondary prevention) of occupational providers are not utilized; practically, there is no professional communication and data exchange between family and occupational physicians.
The treatment and management of chronic diseases is the ‘challenge of the century’. Closer location of providers can improve access to services and to devices that aid chronic disease management (Rumball-Smith et al., Reference Rumball-Smith, Wodchis, Koné, Kenealy, Barnsley and Ashton2014). There are similar initiatives in Hungary as well (Sándor et al., 2018). Continuity and comprehensiveness of care are closely linked to national healthcare expenditures; however, coordination of care is not (Pavlič et al., Reference Pavlič, Sever, Klemenc-Ketiš, Švab, Vainieri, Seghieri and Maksuti2018). Coordination between different levels of healthcare provision is a problematic issue in Hungary. As found also in the Polish-arm of the study, accessibility of care was considered as the best dimension (Krztoń-Królewiecka et al., Reference Krztoń-Królewiecka, Oleszczyk, Schäfer, Boerma and Windak2016).
In the European countries, in the past decades the involvement of GPs in the care of diseases increased, while their preventive activities decreased (Sándor et al., Reference Sándor, Nagy, Jenei, Földvári, Szabó, Csenteri, Vincze, Sipos, Kovács, Pálinkás, Papp, Fürjes and Ádány2018). Service profiles of GPs have expanded more in the past decades in those countries, where higher growth of health care expenditures was reported (Schäfer et al., Reference Schäfer, Boerma, Spreeuwenberg, Schellevis and Groenewegen2016; Semánová et al., Reference Semánová, Rurik, Dózsa, Jancsó, Kolozsvári, Nánási, Pfeiferová and Rurik2019). This is the case in Hungary as well, however, without an increase in health care expenditure.
In the past two decades, there was a tangible improvement of the standards of service, as well as the financial circumstances of the Hungarian PC. However, it remains far below the ‘Western European’ standards (Rurik, Reference Rurik2009; Kolozsvári & Rurik, Reference Kolozsvári and Rurik2016; Schäfer et al., Reference Schäfer, Boerma, Spreeuwenberg, Schellevis and Groenewegen2016; Rurik, Reference Rurik2019). Currently, the Hungarian health care system faces two major challenges, inadequate financial resources and a shortage of manpower, mainly in PC (Sándor et al., Reference Sándor, Pálinkás, Vincze, Sipos, Kovács, Jenei, Falusi, Pál, Kőrösi, Papp and Ádány2018; Rurik, Reference Rurik2019). The overall ageing of the GP population is evident in Hungary, as described in other participating countries (Groenewegen et al., Reference Groenewegen, Bosmans, Boerma and Spreeuwenberg2020). The Hungarian population is as yet broadly satisfied with the PC system, although performances of other health care levels (mainly hospitals) are rated negatively. Among the evaluated process indicators, access, continuity, comprehensiveness, and coordination were rated as satisfactory, together with equity among health outcome indicators. In contrast, quality and efficiency have deteriorated in the previous years, influenced mainly by other levels of provision (secondary care, hospitals). In the upcoming years, hopefully more governmental initiatives will be made to improve the level of the Hungarian PC to approach the expected international requirements (Expert Panel on Effective Ways of Investing in Health (EXPH), 2014; WHO, 2008; 2016).
Conclusion
Cooperation and communication between different levels of health care provision is often insufficient. Without specific PC-oriented guidelines, the expected service profile of GPs is not clearly determined. There is, yet a lot of room for improvement among the structure indicators, the financial conditions, and workforce development. Preventive services should be appropriately implemented in PC, beside the improvement in community orientation.
Acknowledgements
The authors are very grateful to the participating GPs that they contributed and gave information about their working condition. Thanks to the fieldworkers (mainly students of the University of Debrecen) who distributed the questionnaires. Thanks to the former staff members of the Departments of Family Medicine: Dr Mária Végh (Pécs), Dr Lajos Mester (Szeged), and Dr Judit Szidor (Debrecen). Thanks to Prof Ferenc Antoni (University of Edinburgh) for corrections in English.
Author contributions
Author contribution in the frame of a national network: IR – study coordination, paper design, literature search, text writing, and final editing; AN – data analysis and text writing; ZJ – literature search, text writing, editing; TU – data processing and analysis; LIL – organization of field-work; CM – editing tables, managing questionnaires and was involved in regional network organization as well; CS – data analysis, literature search; PS, PT, LRK – advisory board members, literature search; LRK – study coordination, literature search, and text writing.
Financial support
The QUALICOP project was funded by the European Commission, under the Seventh Framework Programmes-Health, Project ID242141. Analysis and interpretation of data, writing of the manuscript did not get any financial support.
Conflict of interests
None.
Ethical standards
The Hungarian Medical Research Council (TUKEB) approved the Hungarian arm of the study assigning the number: 20024/2011-EKU (643/PI/11.). Informed written consent was included in the questionnaire, and refusal of participation was also offered as an option.
All authors have read and approved the manuscript and consent to publish.
Hungarian data and materials are available at the University of Debrecen (Hungary) and in the NIVEL (Netherlands Institute for Health Services Research), together with the data of other participating countries.






