Introduction
A wildfire is an uncontrolled event occurring in an area of combustible vegetation, categorized dependent on the fuel consumed such as a forest or grass fire, collectively referred to as bushfires in some parts of the world. Such vegetation provides a carbon rich source of fuel, and when combined with seasonally dry conditions, can produce devastating results to local ecosystems and human habitation. Reference Flannigan, Amiro, Logan, Stocks and Wotton1 Wildfires are not a new occurrence and have many natural and anthropogenic causes including lightning strikes, volcanic activity, as well as arson, and as an unintended result of agricultural land clearance. Reference Bowman, Balch and Artaxo2 For example, it was estimated that the majority of the 2019-2020 summer fires that devastated the south-eastern parts of the mainland of Australia were caused by lightning. Reference Filkov, Ngo, Matthews, Telfer and Penman3 However, in that same period, other Australian fires which destroyed approximately 21,000 hectares of land were attributed to arson, Reference Richards and Brew4 believed in part to be due to seeded ideas from extensive media coverage of these events and perceived anonymity of the arsonists gained from other large fires burning in the surrounding areas. Reference Amos5
Climate variability, including heat waves, droughts, seasonal weather patterns, and periodic variation in winds and sea surface temperatures, known as El Niño in its warming phase, can all increase the likelihood of wildfire prevalence. In addition, the effects of climate change are predicted to lead to fire seasons starting earlier, finishing later, and inducing more extreme fire weather conditions. Reference Williams, Abatzoglou and Gershunov6 These predicted hot, dry, and windy situations, secondary to climate change, will likely lead to fast moving fires which are difficult to control and thus respond to, causing wide-spread fire effects and associated health impacts. Reference Ribeiro, Viegas and Almeida7 Smoke produced by wildfires typically contains a number of air pollutants, including carbon monoxide, nitrogen dioxide, ozone, particulate matter (PM), polycyclic aromatic hydrocarbons, and volatile organic compounds that can all impact public health. Reference Naeher, Brauer and Lipsett8 The primary health effects of air pollutants include respiratory and cardiovascular disorders, Reference Walter, Schneider-Futschik, Knibbs and Irving9 however ophthalmic and psychiatric problems can also result, as well as severe burns requiring treatment in special burn units, commonly resulting in multi-organ failure, a complication of complex trauma. Reference Finlay, Moffat, Gazzard, Baker and Murray10
The health effects and hospital admissions related to heat exposure have been well-documented, Reference Luther, Gardiner, Hansen and Caldicott11 though studies focusing on heat exposure presentations related to wildfires are less common. The literature, however, has outlined a number of common themes related to these events, including associations between atmospheric PM of less than 10 microns in diameter (PM10) and respiratory-related hospital admissions, Reference Chen, Verrall and Tong12,Reference Morgan, Sheppeard and Khalaj13 and between PM10 and asthma emergency department (ED) presentations. Reference Johnston, Kavanagh, Bowman and Scott14 Demographic data from Australia also indicate indigenous people experienced approximately three-fold higher associations between same-day estimated ambient PM10 and total respiratory admissions when compared to non-indigenous people following exposure to bushfire (wildfire) smoke. Reference Hanigan, Johnston and Morgan15 This study noted that these effects may also be linked to underlying health status, access to medical services, or other social/societal characteristics such as poorly managed symptoms or a reluctance to access health care facilities. Other factors such as population size, distance to a hospital or response time of emergency services, and the residents’ ability to be less reliant on primary health care providers to manage respiratory problems all appear to influence the number of presentations to a health care facility associated with wildfire smoke/atmospheric PM. Reference Davies, Konings and Lal16,Reference Liu, Wilson and Mickley17
Climate predictions indicate wildfires will likely increase in frequency and severity and it is therefore imperative that EDs are adequately prepared for, briefed, and resourced to facilitate rapid mobilization of intervention teams following a disaster to minimize potential associated morbidity and mortality. Reference Anderson18 This literature review will therefore examine these challenges, together with the strategies for planning that have been implemented to best manage their effects. Reference Salinger, Stigter and Das19 Without such knowledge, significant future adverse health effects associated with wildfires will likely continue and be exacerbated following the predicted trends in global climate change. Reference Westerling20 The aim of this literature review is to identify papers relating to wildfires and their impact on EDs. The objective is to analyze these identified papers for patient presentation characteristics, resource utilization, and patient outcomes to enhance the preparedness of EDs through an accessible format that clearly illustrates the strategies and procedures suggested.
Methods
Design
This integrative literature review was guided by the Preferred Reporting Items of Systematic Reviews and Meta-Analysis (PRISMA) guidelines for data collection, as promoted by the Enhancing the QUAlity and Transparency of Health Research (EQUATOR) network, Reference Liberati, Altman and Tetzlaff21 and Whittemore and Knafl’s framework for data analysis. Reference Whittemore and Knafl22
Data Collection
Literature was collated from various databases and search engines as artefacts of evidence to be included in this review. Databases and search engines that were included in this review include: OvidSP (Ovid Technologies; New York, New York USA); MEDLINE (US National Library of Medicine, National Institutes of Health; Bethesda, Maryland USA); DARE (Rutgers University Libraries; New Brunswick, New Jersey USA); CINAHL (EBSCO Information Services; Ipswich, Massachusetts USA); PubMed (National Center for Biotechnology Information; Bethesda, Maryland USA); and Scopus (Elsevier; Amsterdam, Netherlands).
The search strategy included different combinations of Medical Subject Headings (MeSH) terms and keywords that were identified as relevant to wildfires/bushfires and EDs. All proposed MeSH terms and keywords are outlined in Table 1. Terms and keywords in the columns were combined using the OR search strategy, while terms and keywords in the rows were combined using AND combinations. All original publications were included, however editorials, conference abstracts, and systematic reviews were omitted. Inclusion and exclusion criteria for this literature review are listed in Table 2.
Table 1. MeSH Terms and Keywords
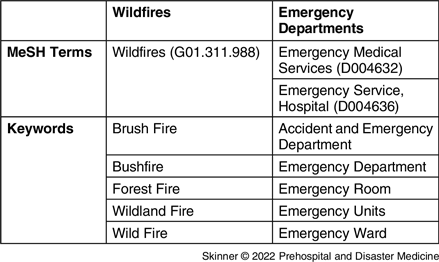
Abbreviation: MeSH, Medical Subject Headings.
Table 2. Inclusion and Exclusion Criteria

Abbreviation: ED, emergency department.
Data Analysis
An analysis of the resultant data was undertaken using the approach from Whittemore and Knafl’s framework. Reference Whittemore and Knafl22 Information extracted from each paper was entered into a Microsoft Word 2018 table (Microsoft Corporation; Redmond, Washington USA). Where available, this information/data included: publication characteristics (author(s), year); wildfire description (country and year of wildfire, location, duration, fire type, and smoke PM measurement); ED patient presentation characteristics (respiratory and cardiovascular presentations); patient outcomes (length-of-stay, discharge disposition); and key themes of findings.
Results
In total, 21 papers met the criteria for inclusion (Figure 1).

Figure 1. Modified PRISMA Flow Diagram. Reference Liberati, Altman and Tetzlaff21
Abbreviation: PRISMA, Preferred Reporting Items of Systematic Reviews and Meta-Analysis.
The impact of wildfires on EDs has primarily been documented in the literature from a relatively narrow number of geographical locations. These have included several southern and western states of America (n = 16; 76%) and the eastern states of Australia (n = 3; 14%). They principally included effects from wildfires, although some other international studies have used data obtained from peat fires (n = 2; 9%) and biomass burning (n = 2; 9%) in examining PM10 and PM2.5 concentrations. Data extracted to inform this literature review are displayed in Table 3. Reference Alman, Pfister and Hao23-Reference Wettstein, Hoshiko, Fahimi, Harrison, Cascio and Rappold43
Table 3. Wildfire Details

Abbreviations: NR, not reported; PM, particle matter.
A significant positive relationship existed between exposure to wildfire smoke, PM2.5, PM10, and an increase in the risk for ED presentation and subsequent hospital admission. This literature review identified small-scale localities were involved in the response to patient presentations, with approximately five to 15 EDs receiving patients. Reference Resnick, Woods, Krapfl and Toth38 There were a limited number of large-scale studies in America which included over 100 EDs in their review of patient presentations. Reference Delfino, Brummel and Wu25
Data extracted from the literature included information on the number of presentations, primary presenting complaint, and a description of ailments. A summary of changes in patient presentations is outlined in Table 4, indicating those presentation complaints that either increased or decreased during the observed fire periods. Further to the descriptions in Table 4, a lag time between PM10/2.5 increase and ED presentation of up to three days was observed in a number of studies Reference Viswanathan, Eria, Diunugala, Johnson and McClean42 and attributed to an increase in the cumulative worsening of fires, patients attempting to self-medicate to manage their own symptoms in the early stages of an event, and the logistics of getting to a relevant ED. The primary presentation complaint detailed in the literature reviewed was respiratory, including asthma and bronchitis, as well as fractures and burns. Several papers indicated that there was an approximate 10%-30% increase across all-cause respiratory presentations during a wildfire event, with a notable increase specifically for asthma of over 100% compared to pre-wildfire ED presentations. Other ailments such as corneal abrasions, burns, and chronic obstructive pulmonary disease/COPD were documented with a lower overall increase of between one percent and five percent. It was also noted that PM2.5 from wildfires displayed greater toxicity to the lungs when compared to equivalent concentrations of PM2.5 from common urban pollution sources, possibly due to its higher carbonaceous content and greater oxidative potential. Reference Aguilera, Corringham, Gershunov and Benmarhnia44 A greater prevalence of hospital admissions was observed in children and women in some studies. Reference Delfino, Brummel and Wu25
Table 4. Changes to Patient Characteristics and Outcomes in the ED during Wildfires

Note: ↑ = increase in presentations; ↓ = decrease in presentations.
Abbreviations: AMI, acute myocardial infarction; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; ED, emergency department; NR, not reported; LOS, length of stay; PVD, peripheral vascular disease.
This literature review has examined a diverse range of studies covering numerous demographics, however one notable feature present in several of the papers reviewed identified that ED presentations were primarily from individuals with minor or no previous relevant medical history. As previously noted, this has been attributed to individuals with recognized aliments being able to address the symptoms, self-medicate, and take appropriate preventative measures, potentially minimizing the health impacts of their chronic conditions. Those without this prior knowledge would include the demographic most likely to present to an ED should they become ill secondary to the poor air quality observed in such situations, a phenomenon that can similarly be observed with thunderstorm asthma. Reference Farouque, Walker and Erbas45,Reference Jordan, Faupula and Luther46 Whilst most papers focused on what primary presenting complaints increased or decreased during the wildfires, most papers did not explore patient outcomes relating to EDs. For example, only one paper reported on patient length-of-stay. Reference Dohrenwend, Le, Bush and Thomas26
Beyond providing analysis of the wildfire characteristics, patient presentation characteristics, and patient outcomes, only nine of the identified papers included recommendations and findings to enhance an EDs preparedness for future wildfire events. The recommendations and findings can be grouped broadly into three themes: communication, personnel, and plans (Table 5). Firstly, communication both within the ED and between the ED and hospital services was emphasized as an area that could be enhanced, however it was unclear if these included incident management systems and what role this played in the response. Secondly, was to ensure adequate workforce personnel was outlined. Finally, disaster, mass casualty, or major incident plans relating to the management of wildfire health impacts could be strengthened for future response.
Table 5. Recommendations and Lessons

Abbreviation: ED, emergency department.
Discussion
Previous studies have included a mix of regional, metro, and rural locations, primarily focusing on the short-term effects during and immediately after a specific wildfire event. Reference Grant and Runkle47 Wildfire events and their relationship to ED presentations have primarily been documented in literature from two geographic regions: Australia and North America. Whilst these locations have seen a number of large-scale wildfires in recent times, other areas prone to such events, such as South Africa, Canada, and parts of Europe, have been less well-reported. Wildfires are episodic and can vary in duration, therefore, for those fires of shorter duration, exposure to PM (PM10/PM2.5) may not be enough to detect all but the most sensitive health outcomes. Literature indicates, however, that PM2.5 from wildfires is particularly toxic to the lungs, especially to alveolar macrophages, compared with the more common PM2.5 exposure from urban pollution. This may occur because of a variation in the duration and intensity of exposure, differences in the composition of wildfire and non-wildfire PM, interactions between PM and temperature, and patient behavioral changes. In addition, studies examining fires in peat indicate that they smolder at lower temperatures, produce dense ground-level plumes with high concentrations of volatile organics, which can be more harmful to health than smoke from hardwood forest fires (common wildfires).
Other studies have focused on demonstrating that adult women were at an increased risk for asthma-related ED attendance during wildfire events. This may be attributable to the inherent structural differences between the genders (lung size and growth), differences in deposition of fine particles, and differences in airway hyper-responsiveness. Reference Melgert, Ray, Hylkema, Timens and Postma48 Other work has shown that children appear to be at the highest risk of respiratory-related illness during a wildfire event, with one particular study illustrating a 136% increase in ED visits for asthma while very young children aged zero to one years old experienced a 243% increase. Reference Hutchinson, Vargo and Milet30 This study demonstrated a clear need to implement better early warning systems and community coordination with schools and childcare facilities to minimize such observed health impacts. Other research has indicated that improving communication through public health messaging may assist in reducing the health effects observed.
A lag time was often observed in the reviewed literature regarding presentation to ED following a significant increase in PM10/2.5 levels. This lag varies from one to three days. Reference Walter, Schneider-Futschik, Knibbs and Irving9 As noted, a possible explanation for this lag could be attributed to the patients attempting home treatment and self-medication prior to seeking emergency health care. Factors that could influence such presentations may include the logistics of an individual’s outdoor movement in securing their personal safety and time spent in structural dwellings (minimizing exposure to heat and PM), or the cumulative worsening of the fires from the onset until containment or reduction of PM exposure secondary to dispersion through winds and weather. Emergency departments also need to be prepared for a potential same-day increase in patient presentations relating to the trauma of wildfires, such as burns, as well as for the lag in respiratory and cardiovascular patient presentations relating from wildfire smoke and subsequent increase in airborne fine PM. Such preparedness should include adequate health care supplies such as supplemental oxygen and respiratory-related medications, in addition to the need for surge capacity in in-patient and ED beds for respiratory-related presentations. Reference Ranse, Luther, Hertelendy and Skinner49 Presentations, however, were not differentiated between those who already had underlying chronic conditions that worsened during the fire episode and those who were otherwise healthy prior to the event. In addition, there was no information regarding follow-up of patients who developed a chronic condition during the bushfire event and subsequently returned to ED some months later.
Study Limitations
This literature review identified that documented wildfire studies have only been conducted in a relatively small number of locations globally. Geographical surveys, however, have indicated that wildfires are a common global occurrence Reference Krawchuk, Moritz, Parisien, Van Dorn and Hayhoe50 and thus data on subsequent health impacts in these other areas appear to have not been adequately captured in peer-reviewed literature. Furthermore, a number of studies included in this literature review have also relied on fixed air quality monitors typically located in more densely populated areas, which can be far from the point of origin of the fire, Reference Liu, Wilson and Mickley17 potentially representing a population with baseline characteristics different from the study population. Another limitation of this study is its focus on the published literature in English language. Consequently, relevant information in other languages may be missing. These limitations should be further addressed as a part of future research.
Conclusions
Despite the increasing prevalence of wildfires globally, their documented impacts on EDs are still relatively limited to a small number of countries or regions and have great variability in their findings. Of the data extracted from the included papers, the findings include variation in ED presentation characteristics between locations such as rural versus metropolitan, demographics such as males versus females, and pollution type such as wildfire versus equivalent pollution loading from urban pollution. A greater prevalence of women and children were observed in EDs following a wildfire event and a lag time was sometimes observed between the start of the event and significant increases in ED presentations. The primary presenting complaint secondary to wildfires at EDs across all studies was respiratory, and often this was from individuals with little or no previous history of the disease. Conversely, those more aware of their medical condition (predominantly chronic respiratory conditions) were able to self-medicate and adequately prepare for the event, assuming key messaging was promulgated in a timely manner. Overall, there is limited information regarding wildfire duration versus health impacts on specific demographics, particularly those persons directly involved in combating, suppressing, and preventing such wildfires. The focus of future research should therefore center on examining ED presentations in other regions of the world outside of Australia and America. With a predicted increase in duration and severity of future wildfires, studies should also focus on examining ED preparedness for longer duration and more frequent wildfire events.
Conflicts of interest
The authors declare that they have no competing interests.









