Introduction
Every year, millions of people across the world are being affected by floods, landslides, cyclones, hurricanes, tornados, tsunamis, volcanic eruptions, earthquakes, wildfires, or human-made disasters. In the past ten years, 83% of all disasters triggered by natural hazards were caused by extreme weather and climate-related events. 1 The on-going global pandemic of coronavirus disease 2019 (COVID-19) has caused a health and economic crisis emphasizing to the world how important disaster preparedness and disaster resilience are. Reference Shoss, Horan, DiStaso, LeNoble and Naranjo2
In addition to the COVID-19 pandemic, multiple climate-related disasters are also happening at the same time. 1 For example, more than 100 other disasters occurred around the world affecting over 50 million people during the first six months after COVID-19 was declared a pandemic by the World Health Organization (WHO; Geneva, Switzerland) in March 2020. Reference Arvin3
Asia has suffered the highest number of disaster events. In total, there were 3,068 disasters occurring in Asia from 2000 through 2019. China reported the highest number of disaster events (577 events), followed by India (321 events), the Philippines (304 events), and Indonesia (278 events). 4
Recent disaster events emphasize the need for disaster risk reduction in the health sector as well as health services in developed countries. For example, in 2011 during the Japan earthquake and tsunami, 80% of the hospitals in Fukushima, Miyagi, and Iwate prefectures of Japan were destroyed or severely damaged, and many local public health personnel were also affected by the disaster, resulting in the entire paralysis or severe compromise of the health services. Reference Mulyasari, Inoue and Prashar5,Reference Nohara6
Disasters can cripple health facilities, leading to partial or total collapse of health services, especially in developing countries. 7 For example, after the Algerian earthquake in 2003, 50% of the health facilities in the impacted area were damaged and were no longer operational. 7 A further example occurred when an earthquake struck in South Asia in October 2005 and caused the complete destruction of almost 50% of health facilities in the affected areas in Afghanistan, India, and Northern Pakistan, ranging from sophisticated hospitals to rural clinics, overwhelming the existing Emergency Medical Services. 7 Currently, most South Asian countries, including Sri Lanka and India, are in a state of crisis resulting from COVID-19, with overcrowded hospitals, low oxygen supplies, and overwhelmed capacity. 8,Reference Jayawardena9
Sri Lanka, a developing nation and small island in the Indian Ocean, is frequently battered by natural disasters. The most devastating disaster it had ever experienced was the tsunami of 2004, which killed over 30,000 people and internally displaced almost one-half a million people. The health systems of the country were severely affected, completely damaging 44 health institutions and partially damaging 48 health institutions. In addition, 35 health care workers (HCWs) lost their lives and a large number of health workers were affected by injuries or psychological trauma due to the loss of their family members or properties. 10 Monsoon floods and landslides also affect several health facilities across the country annually. Sometimes, they have even led to the full or partial evacuation of affected hospitals, as experienced, for example, during the floods of 2016 and 2017, due to infrastructure damage or the functional collapse of services. These instances have resulted in huge economic impacts on the government for recovery-related needs. 11,12
Sri Lanka has also experienced several man-made disasters resulting in mass-casualty incidents. A 26-year war came to an end in 2009 after more than 64,000 deaths, hundreds of thousands of injuries, and the displacement of more than 800,000 persons. Reference Siriwardhana and Conflict13 The Easter-Sunday bombing attack on April 21, 2019 was a recent human-made disaster which killed 250 people and resulted in more than 500 casualties. 14 These mass-casualty incidents caused an acute surge of patients to nearby hospitals, interrupting normal hospital operations and overwhelmed hospital capacity due to ill-preparedness, poor coordination, and limited resources. Reference Persoff, Ornoff and Little15
Notwithstanding the vulnerability of Sri Lanka to disasters, there is no standard hospital disaster preparedness evaluation tool used in Sri Lanka at the moment. Such a tool could be used to inform potential improvements to hospital-level disaster preparedness. Therefore, with the goal of establishing a tool appropriate for Sri Lanka, this study aimed to determine the existence and distribution of hospital preparedness tools across the world, and also to identify the important components of those study instruments.
Aim
The aim of this research was to determine the main components included in hospital disaster preparedness evaluation instruments.
Methodology
A systematic review was performed across three journal databases: Ovid Medline (US National Library of Medicine, National Institutes of Health; Bethesda, Maryland USA); Embase (Elsevier; Amsterdam, Netherlands); and CINAHL (EBSCO Information Services; Ipswich, Massachusetts USA) using the appropriate specifications for each database. The PRISMA Systematic Review Guidelines were used for the review, and the PRISMA 2020 checklist is shown in Appendix 1 (available online only). The search of the databases was conducted on November 23, 2020. The details of the search strategy are shown in Appendix 2 (available online only). Additional documents (grey literature) were sourced by a related search of Google (Google Inc.; Mountain View, California USA), relevant websites, and also from the reference lists of selected articles. Keywords used were: hospitals, health facilities, health services, and health personnel. These were combined with: disaster planning, disaster preparedness, and the terms: checklist, surveys, questionnaire, or toolkit.
Selection of Articles
Initially, two independent reviewers (NM and GO) screened titles and abstracts of the retrieved articles for eligibility. From the abstracts selected by both reviewers, full texts were retrieved and considered for eligibility. If discrepancies occurred between reviewers, the reasons were identified and a final decision was made by the main author (NM).
Inclusion Criteria
Articles published across the world from 2011 through 2020, written in English language, which were conducted on the disaster preparedness of hospitals, health facilities, or health personnel using toolkits, checklists, or questionnaire surveys were selected for this study. The “safe hospitals” concept became popular after 2010 when the WHO introduced a guidebook on safe hospitals in emergencies and disasters. Therefore, the search was started from 2011, as relevant hospital disaster preparedness assessments were most likely to be published after this time.
Exclusion Criteria
The published studies in a language other than English, not available in full text, and not related to health sector disaster preparedness were excluded.
Data Synthesis and Analysis
Data extraction and analysis were based on the Joanna Briggs Institute (JBI; Adelaide, Australia) manual for evidence synthesis. 16 In order to identify the basic information, the selected studies were analyzed in the following categories: reference; year of publication; country of origin (where the study was published or conducted); type of hazard; sample size; and the study design.
The global distribution of studies was analyzed according to the WHO’s six geographical regions, namely South-East Asia, the Western-Pacific, the Eastern Mediterranean, the Americas, Europe, and Africa regions. 17,18 The distribution of studies was also analyzed according to the four categories of the United Nations Human Development Index (UNHDI). 19 The UNHDI comprises three dimensions: health, education, and standard of living. The health dimension is measured by life expectancy at birth, the education dimension by mean years of schooling for adult persons aged 25 years and above and expected years of schooling for children at school entering age, and the standard of living dimension is assessed by gross national income per capita. Based on the cut-off points of the HDI, the UN has identified four categories of human development (HD); Low HD, Medium HD, High HD, and Very High HD. 19
The global literature classifies a hospital’s disaster preparedness and response in terms of the “4S’s” – space, stuff, staff, and systems. Reference Munasinghe, O’Reilly and Cameron20–Reference Lavonne24 The space domain includes: the physical space needed for patient care and workspace (infrastructure and their access routes). The stuff domain includes logistics, equipment, and supplies. The staff domain includes human resources. And the system domain includes all the plans, procedures, and protocols needed for preparedness management. Reference Munasinghe, O’Reilly and Cameron20–Reference Lavonne24 Similarly, preparedness themes of each selected study were identified according to this 4S conceptual framework.
Results
The search resulted in a total of 1,568 articles, including 1,563 from databases and five from grey literature. After removing the duplicates, there were 1,070 articles. Based on the inclusion criteria, only 53 articles were selected for data extraction and synthesis. Figure 1 illustrates the PRISMA flow diagram.

Figure 1. PRISMA 2009 Flow Diagram.
Table 1 summarizes the basic information of the selected articles. All these studies have assessed the preparedness of either the facilities or the HCWs. Altogether, these studies assessed the preparedness of approximately 5,100 HCWs across the world, including different categories of acute care providers such as physicians, doctors, nurses, paramedics, and health care assistants. These studies have also assessed approximately 1,930 different levels of hospitals (government, rural, military, tertiary, and district), health care facilities, and emergency departments (Table 1).
Table 1. Basic Information of the Selected Articles

Abbreviations: HCW, Health Care Worker; EMS, Emergency Medical Services; VAMC, Veterans Affairs Medical Center; CBRN, Chemical, Biological, Radio, Nuclear Disasters.
Table 2 illustrates the number of publications by hazard type. One-half of the studies (27) covered all hazards, and the rest of the studies focused on a specific type of hazard. Among them, there were biological hazards like Ebola, influenza, and COVID-19; natural disasters like earthquake, flood, or extreme weather events; and man-made disasters like chemical-only, chemical, biological, radiological, and nuclear (CBRN), or mass-casualty incidents.
Table 2. Number of Publications by Hazard Type
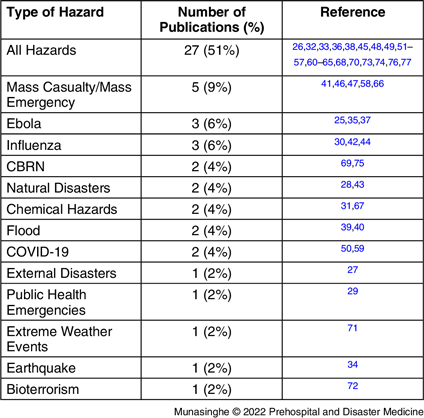
Abbreviation: CBRN, Chemical, Biological, Radiological, and Nuclear.
These studies have used different methodologies; however, the majority (41) were cross-sectional studies. Reference Vong, Samuel and Gould25–Reference Hosseini, Bahadori, Raadabadi and Ravangard65 The next most common were longitudinal studies, Reference Aladhrai, Djalali, Della Corte, Alsabri, El-Bakri and Ingrassia66–Reference Der-Martirosian, Radcliff and Gable68 followed by Delphi, Reference Olivieri, Ingrassia and Della Corte69,Reference Zhong, Clark, Hou, Zang and FitzGerald70 mixed method, Reference Paterson, Berry, Ebi and Varangu71,Reference Wang, Jiang, Shao, Zheng and Sun72 and systematic reviews. Reference Rezaei, Maracy, Yarmohammadian and Sheikhbardsiri73,Reference Nekoie-Moghadam, Kurland, Moosazadeh, Ingrassia, Della Corte and Djalali74 In addition, there was one retrospective, one observational, Reference Kotora75 one scoping review, Reference Zhong, Clark, Hou, Zang and Fitzgerald76 and one interventional Reference Worrall77 study (Table 1).
Figure 2 demonstrates the number of publications by year. There were six publications on hospital disaster preparedness in 2011. The analysis of publication incidence by year revealed an overall rise in publication rate from 2012-2016. A decline in the publication rate was observed thereafter until 2020.
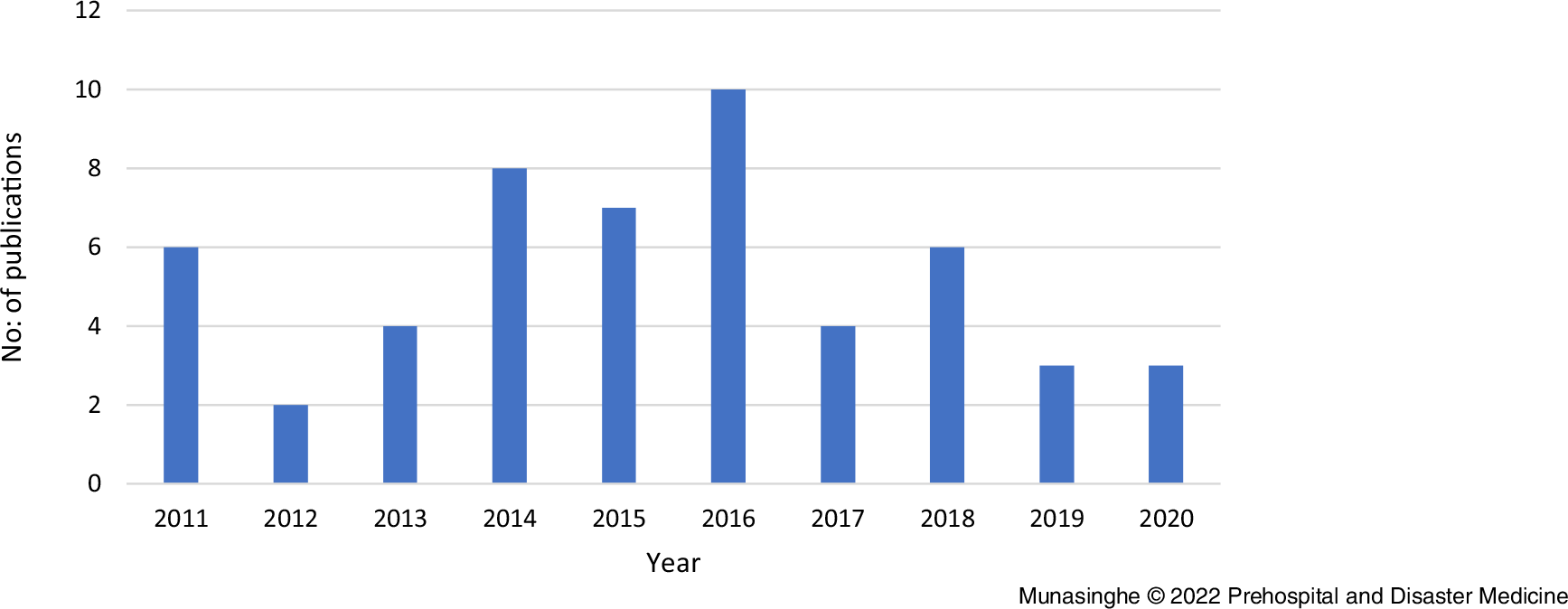
Figure 2. Number of Articles by Year of Publication.
Altogether, these studies were conducted in 24 different countries around the world. Iran has published the highest number of studies (twelve), followed by China (six), USA (five), and Saudi Arabia (three). All the other countries have published one or two studies (Table 3).
Table 3. Number of Publications by Country (Including the WHO Region and Reference)

Abbreviations: WHO, World Health Organization; AH, All hazards; BT, Bioterrorism; PHE, Public Health Emergencies; MC, Mass Casualty; Ex. Weat, Extreme Weather events; Influ, Influenza; Chem, Chemical events; CBRN, Chemical, Biological, Radiological, and Nuclear.
Figure 3 demonstrates the number of publications by WHO region and Table 3 illustrates the number of publications by country (including the WHO region, reference, and disaster type). The Eastern Mediterranean region has recorded the greatest number of publications (18), with Iran being responsible for two-thirds of the publications in the region. The Western-Pacific region had the second largest number of publications (12), with China recording the highest number of publications in that region. The European and Americas regions had a similar number of publications (eight and seven, respectively), and the UK and USA were the most represented countries in those regions. The South-East Asian region had six publications, where all three included countries (Sri Lanka, India, and Thailand) had two publications each. The African region recorded the lowest number of publication (two). The Americas and European regions had a focus on CBRN emergencies, whereas other regions had focused on natural disasters (Table 3).
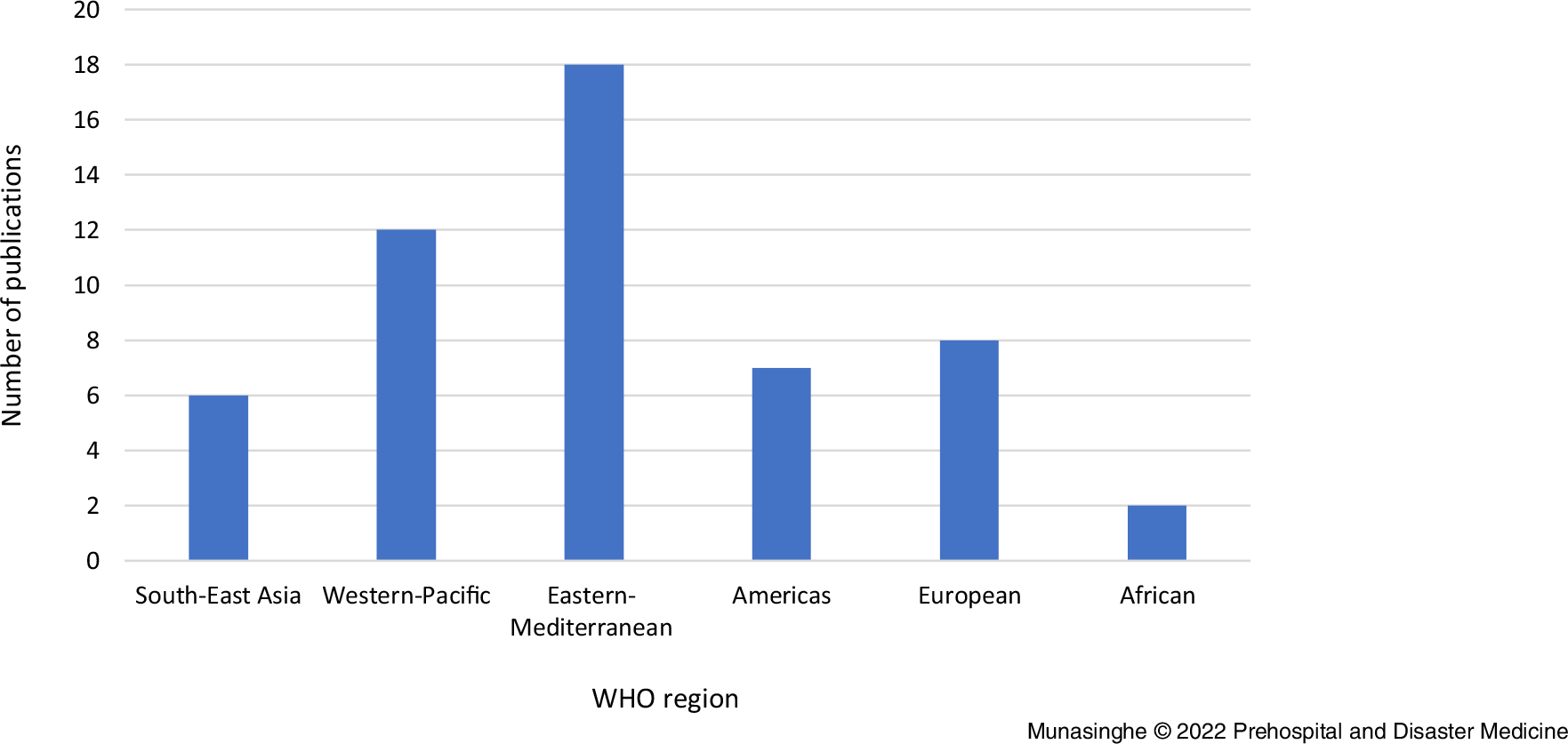
Figure 3. Number of Publications by WHO Region.
Abbreviation: WHO, World Health Organization.
Figure 4 illustrates the number of publications by UNHDI. The countries with Very High HD and High HD have published the majority of studies, 23 and 24 publications, respectively. Conversely, the countries with Medium HD and Low HD have published a low number of studies, with four and three publications, respectively. Table 4 illustrates the number of publications by UNHDI, including the country and hazard type. Significantly, there were five publications concerned with man-made disasters like chemical or CBRN incidents among the developed countries, while only one study focused on such disasters (bio-terrorism: BT) among the developing countries. It was clear that developing countries have more focus on natural disasters.

Figure 4. Number of Publications by UNHDI.
Abbreviations: UNHDI, United Nations Human Development Index; HD, Human Development.
Table 4. Number of Publications by UNHDI Including the Country and Hazard Type
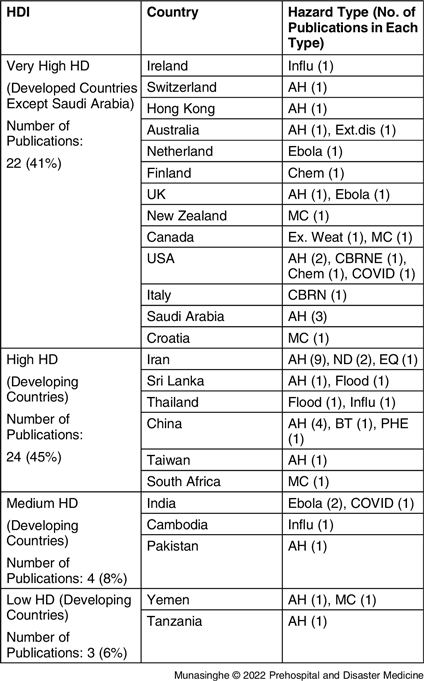
Abbreviations: UNHDI, United Nations Human Development Index; HD, Human Development; AH, All hazards; BT, Bioterrorism; PHE, Public Health Emergencies; MC, Mass Casualty; Ex. Weat, Extreme Weather events; Influ, Influenza; Chem, Chemical events; CBRN, Chemical, Biological, Radiological, and Nuclear.
Table 5 summarizes the different themes/components identified in those study instruments according to the 4S domains.
Table 5. Analysis of Different Themes/Components of Study Instruments According to 4S Domains

Abbreviations: ICC, Incident Command Centre; ICU, Intensive Care Unit; ICS, Incident Command System; SOP, Standard Operating Procedure; MOU, Memorandum of Understanding; PPE, Personal Protective Equipment; CES, Continuity of Essential Services; PDR, Post-Disaster Recovery.
For the space domain: infrastructure and isolation/decontamination facilities were considered more frequently, with 20 and 16 publications, respectively, while morgue facilities and accessibility/access routes were considered less frequently, in only seven and five studies, respectively.
For the stuff domain: logistics, personal protective equipment (PPE), and medicines/medical equipment/medical gases/other supplies (food, water, fuel reserves) were considered among the majority of studies, 32, 27, and 27, respectively, while back-up power, stockpiling, and transport themes were included in a smaller number of studies, 12, 12, and 11, respectively.
For the staff domain: training/education/capacity building and drills/simulation exercises were included in the majority of studies, 40 and 34 studies, respectively, while vaccination, rewards/incentives, and volunteer themes were given the least priority, with seven, six, and six studies, respectively.
For the systems domain: information/communication, Incident Command System (ICS), disaster plans, and safety/security themes were considered in most of the studies, while waste management and the handling of dead bodies were given the least priority, considered only in eight and three studies, respectively.
Overall, isolation/decontamination facilities, Incident Command Centre (ICC), intensive care unit/ICU, and laboratories were considered frequently under the space domain, while access routes and morgue space were given less priority. For the stuff domain, PPE, medicines, and medical equipment were frequently considered in the broad category of logistics, while back-up power, stockpiling, and transport-related themes were considered less frequently. Capacity-building-related themes were frequently considered under the staff domain, while psychological well-being-related themes were given less priority. Further, communication, ICS, and disaster plans were considered frequently under the system domain, while the waste management and handling of dead bodies were given less priority in the majority of the study tools.
Discussion
This is the first study to review publications assessing hospital-level disaster preparedness across the world using the 4S framework. Over the decade, the annual rate of publications varied considerably, with an overall increase up to 2016, and surprisingly, a reduction thereafter. Also, the developing countries with “Medium” and “Low” HDI featured less in terms of publications on hospital disaster preparedness. However, the developing countries with “High” HD contributed to a similar number of publications to developed countries.
Surprisingly, this study found that the number of publications was reduced during the second-half of the decade despite the increase in disaster events globally. In contrast, a past study conducted on public health emergency preparedness from 1997-2008 reported that there was a 33% growth of publications per year. Reference Savoia, Massin-Short, Rodday, Aaron, Higdon and Stoto78 Interestingly, Iran, as a highly vulnerable country to both natural and human-made disasters, 1 has published the majority of studies on hospital disaster preparedness. Therefore, the Eastern Mediterranean region has recorded the highest number of publications during the decade.
One of the important findings of the study was the significant interest in chemical hazards, CBRN, and bio-terrorism hazards in the Americas and European regions. All of these publications originated from developed countries such as USA, Italy, and Finland. Similarly, a study conducted by Mohsen, et al found that the majority of research on biological events were from USA, China, and Canada. Reference Mohsen, Mehrdad, Abbas, Gholam, Pirhossein and Hamid79 This trend may be due to assumed international best practice for disaster preparedness being adopted by the European Union and other developed nations. Reference Sabol, Šesták, Polívka and Mroz80 However, no country is immune from CBRN threats, and therefore, those countries with more advanced disaster preparedness monitoring would have the capacity to partner with developing countries in implementing adequate preparedness measures for CBRN emergencies. The main focus of the South-East Asian region was on natural disasters, such as floods, and infectious disease outbreaks; none of the countries in the region published a study on man-made disasters during the decade. The Easter-Sunday terrorist attack that occurred in 2019 in Sri Lanka highlighted the importance of preparedness for CBRN events. Reference Wickramarathne81
The global literature reports that the countries with a Low HDI have a lower research investment and are, therefore, less dominant in the research and development area. Reference Livingston, Waring and Pacheco82 Conversely, the countries with a High HDI dominate with research publications. This study has further emphasized that the countries with a Low HDI have less publications despite their high vulnerability to disasters.
A comprehensive plan should address every possible disaster scenario with contingency plans. Adequate preparedness of all 4S domains is, therefore, equally important. However, surprisingly, this study found that access routes, transport, morgue facilities, handling of dead bodies, back-up power, stockpiling, vaccination, rewards/incentives for staff, volunteer, and waste management themes were given less priority in most of the studies.
Regarding the access routes, the WHO emphasized that in order to ensure the safety of lives, hospitals and health facilities must remain safe, accessible, and functioning at maximum capacity during emergencies or disasters. 83 Therefore, the WHO has identified that a safe site and accessibility are important aspects of a hospital disaster preparedness. They also recommended hospitals be located near good roads with an adequate means of transportation. To ensure readiness in transport preparedness, the WHO recommends having adequate transport equipment, equipped ambulances, and other vehicles. Therefore, transport facilities are one of the crucial aspects under the stuff preparedness, which is essential for transporting casualties from field to hospital, moving patients to other referral hospitals, and evacuating patients in an emergency or disaster situation. 83 However, this review identified that transport was neglected in the majority of the published studies.
This study identified that back-up power has also been neglected under the stuff preparedness in the majority of the studies. Electric power is a critical lifeline of a hospital. A survey conducted in Japan found that 65% of disaster-base hospitals considered electricity to be the paramount lifeline for the functioning of their hospital. Reference Klinger, Landeg and Murray84 All the medical devices, diagnostic equipment, communication devices, lighting, heating and cooling systems, elevators, and IT-based patient information systems become useless when there is a power failure. Therefore, back-up generators or a reliable alternative power source should be an essential part of the stuff preparedness.
The study identified that most of the selected studies have ignored stockpiling under the stuff preparedness. The WHO also emphasizes that hospitals have a stockpile of at least one week of adequate emergency medicines and supplies when preparing for disasters. 83 The COVID-19 pandemic has proven that stockpiling is a cornerstone of a holistic approach to disaster preparedness. 85 One of the biggest reasons for countries to fail in their initial response to the pandemic was the lack of necessary PPE and emergency equipment to deal with the pandemic. Therefore, in addition to having a national stockpile, it is important to have an individual hospital stockpile of critical medicines, vaccines, emergency equipment, and supplies. 85 Periodic reviews and dynamic use of stockpiles are also necessary to ensure the effective use of stored equipment and other items before their expiry.
The study also found that morgue facilities and dead body handling were neglected themes under the space and the system preparedness, respectively. However, the COVID-19 pandemic has highlighted the importance of ensuring adequate morgue capacities in hospitals. For example, in India, during the peak of the pandemic, hospital morgues and crematoriums were overwhelmed and the bodies were piled up due to inadequate morgue facilities. Reference Dasgupta and Mohan86 Therefore, in order to ensure proper identification and handing of dead bodies, adequate morgue capacity, temporary morgue spaces, cold storage facilities, and adequately trained staff are crucial. Reference Munasinghe and Matsui57
The study also identified that vaccination, rewards/incentive, and volunteer themes were neglected by the majority of studies under staff preparedness. The COVID-19 pandemic highlighted how important vaccination, volunteers, and rewarding were in improving psychological well-being of the staff. Martinese, et al examined the measures motivating hospital workers to report for duty during a crisis situation. They identified preventative measures for self and family, followed by alternative accommodation and financial incentives as high priority incentives. Reference Martinese, Keijzers, Grant and Lind87 Another study also reported that access to PPE and vaccines, childcare arrangements, volunteers’ networks, adequate training, and protection from disaster-related legal sanctions are some of the major incentives to motivate staff during disasters. Reference Powell88 Therefore, these aspects should be considered in emergency planning as it plays a key role in motivating staff to work in disaster situations.
The study found that waste management was given the least priority under system preparedness. Waste management is an essential part of disaster preparedness, especially given that clinical waste should be handled carefully as it contains hazardous materials such as infectious, toxic, and radioactive substances. 89 The WHO recently reported that tons of extra medical waste from the COVID-19 response put enormous strains on health care waste management systems around the world. Therefore, the WHO emphasizes the dire need of improving the waste management practices in order to minimize the human and environmental impacts. Improper waste management could result in secondary disasters. Therefore, contingency plans are necessary for managing hospital waste as well as the waste generated in CBRN events.
As highlighted in the above discussion, all of these less prioritized areas have a significant impact in different disaster scenarios. Therefore, in a comprehensive disaster plan based on an all-hazard approach, it is also important to address these neglected aspects the same way as frequently prioritized areas.
Limitations
This study selected only the published articles on hospital-based disaster preparedness studies. However, there may be some publications related to hospital disaster preparedness in community or public health preparedness studies that were not published on the databases searched. In addition, this study selected only articles written in the English language from 2011-2020.
Conclusion
Few published studies used a toolkit, checklist, or questionnaire to assess hospital disaster preparedness across the world during the decade of 2011-2020. The countries with Low HD have a smaller number of publications and the developing countries generally have less focus on CBRN preparedness. The majority of the past studies have neglected some crucial aspects of hospital disaster preparedness. Important preparedness themes were identified under each domain of the 4S framework, and these aspects should be properly addressed in order to ensure adequate preparedness of hospitals. The results of this systematic review can be used for planning a comprehensive disaster preparedness tool.
Conflicts of interest/funding
No financial disclosures were reported by the authors of this paper. The authors declare no conflicts of interest.
Author Contributions
NM and GO: conceptualization, designing, screening and selection of studies, and analysis of the selected studies. NM: writing and preparation of the draft. GO and PC: supervising, reviewing, editing, and approving the final version of the manuscript for submission.
Acknowledgements
The authors would like to thank Ms. Lorena Romero, Senior Librarian, Alfred Health (Melbourne, Australia) for her assistance with planning the search strategies; and Mr. Adam Clark, Manager, Library Services at Alfred Health for his guidance on EndNote references.
Supplementary Materials
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X22001212












