Introduction
Despite strict hygiene measures in many countries, Ascaris suum remains a significant problem in commercial pig farming worldwide. The high degree of tenacity of A. suum eggs in the environment hampers anthelminthic treatment efforts (Mejer and Roepstorff, Reference Mejer and Roepstorff2006; Dold and Holland, Reference Dold and Holland2011), leading to a high prevalence and subsequent economic losses due to liver condemnations and lower feed conversion efficacy (e.g. Boes et al., Reference Boes, Kanora, Havn, Christiansen, Vestergaard-Nielsen, Jacobs and Alban2010; Thamsborg et al., Reference Thamsborg, Nejsum, Mejer and Holland2013). After oral infection, third-stage larvae migrate via mesenteric veins to the liver and lungs and enter the small intestine again from approximately day 10 post infection (pi) (Roepstorff et al., Reference Roepstorff, Eriksen, Slotved and Nansen1997; Dold and Holland, Reference Dold and Holland2011). Reaching patency after 6–8 weeks pi, females produce approximately 200 000 eggs per day on average (Sinniah, Reference Sinniah1982). Ascaris suum is closely related to the human parasite Ascaris lumbricoides, which infects approximately 807–1121 million people worldwide (CDC, 2020), resulting in malnutrition and growth retardation especially in children (Hlaing, Reference Hlaing1993; O'Lorcain and Holland, Reference O'Lorcain and Holland2000). Furthermore, A. suum has been identified as an important cause of human ascariosis in endemic areas (Zhou et al., Reference Zhou, Li, Yuan, Deng and Peng2012). Therefore and due to the high degree of relatedness between A. lumbricoides and A. suum, which may hybridize (Zhou et al., Reference Zhou, Li, Yuan, Deng and Peng2012; Easton et al., Reference Easton, Gao, Lawton, Bennuru, Khan, Dahlstrom, Oliveira, Kepha, Porcella, Webster, Anderson, Grigg, Davis, Wang and Nutman2020) and are even regarded as the same species by some authors (Leles et al., Reference Leles, Gardner, Reinhard, Iniguez and Araujo2012), new insights into the parasite–host interaction of A. suum may also be transferable to human ascariosis.
Ascaris suum-related changes in porcine intestinal nutrient absorption have been investigated during the pre-patent phase of the infection, with mixed results. On the one hand, a significant decrease of electrogenic glucose transport was recorded in the porcine jejunum at day 14 after infection with 10 000 (Dawson et al., Reference Dawson, Beshah, Nishi, Solano-Aguilar, Morimoto, Zhao, Madden, Ledbetter, Dubey, Shea-Donohue, Lunney and Urban2005) and day 21 after infection with 25 000 A. suum eggs (Solano-Aguilar et al., Reference Solano-Aguilar, Shea-Donohue, Madden, Quinones, Beshah, Lakshman, Xie, Dawson and Urban2018). On the other hand, Koehler et al. (Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a) were not able to reproduce these observations regarding glucose transport on days 14 and 21 pi, although using a comparable infection dose of 10 000 eggs both as a single- and a trickle-infection, and noting altered transcription patterns of several nutrient transport-related genes. Immunologically mediated parasite expulsion between days 14 and 21 pi (Roepstorff et al., Reference Roepstorff, Eriksen, Slotved and Nansen1997; Masure et al., Reference Masure, Wang, Vlaminck, Claerhoudt, Chiers, Van den Broeck, Saunders, Vercruysse and Geldhof2013) may lead to considerable variation in worm burden between individual animals and may have caused these inconsistent results. However, Koehler et al. (Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a) observed a significant decrease in alanine and peptide transport on day 49 pi, i.e. at the end of the pre-patent phase. Furthermore, the related roundworm Ascaridia galli significantly impaired intestinal glucose and alanine absorption in chicken at 5 weeks pi, i.e. at the end of the pre-patent period and therefore at a time point comparable to day 49 pi for A. suum (Schwarz et al., Reference Schwarz, Gauly, Abel, Das, Humburg, Rohn, Breves and Rautenschlein2011). When excretory–secretory (ES) antigens of adult A. suum were added to porcine jejunal mucosa in an in vitro set-up, an immediate impairment of glucose and alanine transport was evident (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Wendt, Breves and Strube2021b). Therefore, adult parasites may exhibit a stronger modulatory effect on the porcine mucosa as compared to larval or pre-adult parasite stages; however, this has not been investigated yet in vivo.
Regarding the underlying mechanisms of the observed transport impairment, an increase in the transcription of the Th2-associated cytokines interleukin-4 (IL-4) and/or IL-13, as observed e.g. in A. galli-infected chicken (Schwarz et al., Reference Schwarz, Gauly, Abel, Das, Humburg, Rohn, Breves and Rautenschlein2011) as well as in previous studies on A. suum (Dawson et al., Reference Dawson, Beshah, Nishi, Solano-Aguilar, Morimoto, Zhao, Madden, Ledbetter, Dubey, Shea-Donohue, Lunney and Urban2005; Solano-Aguilar et al., Reference Solano-Aguilar, Shea-Donohue, Madden, Quinones, Beshah, Lakshman, Xie, Dawson and Urban2018), may trigger a reduction of the intestinal sodium-coupled glucose absorption by activating the signal transducer and activator of transcription 6 (STAT6) signalling pathway (Madden et al., Reference Madden, Whitman, Sullivan, Gause, Urban, Katona, Finkelman and Shea-Donohue2002; Zhao et al., Reference Zhao, McDermott, Urban, Gause, Madden, Yeung, Morris, Finkelman and Shea-Donohue2003). Consequently, infection with the nematode Heligmosomoides polygyrus leads to reduced intestinal glucose absorption in wild type, but not in STAT6-deficient mice (Madden et al., Reference Madden, Yeung, Zhao, Gause, Finkelman, Katona, Urban and Shea-Donohue2004). Furthermore, in a study on Nippostrongylus brasiliensis-infected mice, the sodium glucose cotransporter 1 (SGLT1) showed a reduced activity and the expression of glucose transporter 2 (GLUT2) was downregulated, whereas glucose transporter 1 (GLUT1) showed a compensatory increase, presumably induced by hypoxia-inducible factor 1-alpha (Hif1α) (Notari et al., Reference Notari, Riera, Sun, Bohl, McLean, Madden, van Rooijen, Vanuytsel, Urban, Zhao and Shea-Donohue2014).
Transport activity and localization of SGLT1 (in intracellular compartments vs the plasma membrane) can be altered directly by protein kinase A (PKA) due to phosphorylation (Subramanian et al., Reference Subramanian, Glitz, Kipp, Kinne and Castaneda2009). However, in pigs, it is not yet clear whether SGLT1 phosphorylation via PKA results in an increased or a decreased transporter activity (Klinger and Breves, Reference Klinger and Breves2018; Klinger et al., Reference Klinger, Lange, Brandt, Hustedt, Schroder, Breves and Herrmann2018). Additionally, leucotriene treatment of rat intestinal epithelial cells (IECs) resulted in a reduced absorption of amino acids due to phosphorylation of the neutral amino acid transporter A (ASCT1) by PKA (Arthur and Sundaram, Reference Arthur and Sundaram2014). Phosphorylation via PKA may also impair the activity of Na+/H+-exchanger 3 (NHE3), subsequently changing the intracellular pH, which affects the function of peptide transporter 1 (PepT1) (Thwaites et al., Reference Thwaites, Ford, Glanville and Simmons1999; Kennedy et al., Reference Kennedy, Leibach, Ganapathy and Thwaites2002).
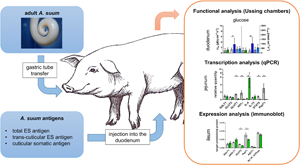
To provide more insight into the modulation of intestinal nutrient transport processes by A. suum, this study aimed at characterizing changes in the functional, transcriptional and expression levels after exposure of parasite-naïve pigs to different adult A. suum antigen fractions. To complete the picture, 1 group of parasite-naïve pigs was exposed to adult A. suum worms by gastric tube transfer to include natural conditions of antigen release as well as ES and cuticular somatic antigen (CSO) interactions.
Materials and methods
Preliminary work and animals used in this study
To test whether the controlled application of adult roundworms via gavage into the stomach of pigs results in establishment of infection, 10 pigs and 130 viable A. suum specimens were used. Each pig received 10–16 adult A. suum, which were flushed into the stomach through a plastic tube (1.5 cm diameter) with tap water during anaesthesia. For the following 10 days, daily coproscopical examinations [flotation using saturated sodium chloride (NaCl) solution and modified McMaster technique] were conducted and the entire fecal mass was collected and screened for expelled roundworms. By day 2 pi, all animals showed A. suum egg excretion, which lasted until day 10 pi in 9 pigs and until day 9 pi in 1 pig (Supplementary Table 1). During the first 3 days pi, i.e. the period relevant for the main experiment, 12 expelled worms (0–3 per animal) were noted. On day 11 pi, anthelmintic treatment was conducted, resulting in worm expulsion in 9 pigs. Only the animal which had been coproscopically negative on day 10 pi did not excrete any worms post-treatment. These findings confirmed previous transfer attempts by Jungersen et al. (Reference Jungersen, Eriksen, Nielsen, Roepstorff and Nansen1996), and showed that infection of pigs with adult A. suum, bypassing the natural larval migration, is possible.
Weaned German landrace (hybrid) fattening pigs (17 male, 19 female), approximately 10 weeks of age and weighing 30 kg, were obtained from the Ruthe Research and Education Farm of the University of Veterinary Medicine Hannover, which is free of A. suum, and kept at the Clinic for Swine, Small Ruminants and Forensic Medicine, University of Veterinary Medicine Hannover. For parasitological monitoring, fecal samples were taken after arrival and on the day of necropsy (days 11–48 after arrival) and analysed with the combined sedimentation–flotation method using saturated zinc sulphate solution as flotation medium. The animals were kept in groups of 8–15 individuals on straw bedding and received standard pig diet (Deuka Ferkelstarter Primo, Düsseldorf, Germany) at recommended rates and water ad libitum. Prior to experimental inoculations, animals were allowed to acclimatize for a minimum of 7 days.
Inoculation of pigs with adult A. suum worms by gastric tube transfer
For oral transfer of adult worms collected from an abattoir at the same day, 12 pigs were anaesthetized [azaperone 2 mg kg−1 BW (Stresnil®, Elanco Animal Health, Bad Homburg, Germany); ketamine 20 mg kg−1 BW, Ursotamin®, Serumwerk Berneburg Tiergesundheit GmbH, Bernburg, Germany] and 6 of them were inoculated with 30 living adult A. suum (male:female ratio, 1:2). Worms were flushed individually through a gastric tube (outer diameter 1.5 cm) with a total amount of 1.5 L tap water. The 6 control animals were given 1.5 L of tap water only. Excess water was drained through the tube in regular intervals.
After adult worm transfer, the 6 inoculated pigs were separated by grids to collect all individual feces until necropsy 3 days later. Collected feces were rinsed through a sieve and the sieve residues were examined for the presence of A. suum specimens.
Adult A. suum ES and CSO antigen production
Adult A. suum antigen fractions (total ES, trans-cuticular ES and CSO antigens) were produced by in vitro cultivation of 420 adult worms collected at a commercial pig abattoir as described previously (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a). Briefly, total ES and trans-cuticular ES were each obtained by incubating 210 worms (male:female ratio of 1:2 to reflect natural distribution) in Roswell Park Memorial Institute (RPMI) medium for 3 days at 37°C and 5% carbon dioxide. To obtain trans-cuticular ES, the worms' mouth and anal openings were sealed with tissue glue prior to incubation. ES-containing medium was collected every 24 h and replaced by fresh medium. The different antigen fractions were centrifuged, sterile-filtered and pooled before concentration by lyophilization.
CSO was produced by homogenizing the cuticles of 210 adult A. suum (male:female ratio, 1:2) after shock-frosting in liquid nitrogen. The resulting homogenate was dissolved in 700 mL double-distilled water.
Inoculation of pigs with adult A. suum antigens
To prevent gastric degradation after oral application, A. suum antigens were directly applied into the gut. Laparotomy of 24 pigs was performed under anaesthesia via injection as described above, with 6 pigs each receiving either total ES, trans-cuticular ES or CSO antigens via injection into the proximal duodenum using a 21 G cannula, while further 6 pigs served as placebo-treated controls. The applied volume per pig corresponded to the amount of ES antigens produced by 30 worms over 3 days or the CSO antigen of 30 worms, respectively, resulting in the application of 131.5 mg total ES antigen (136 mL, protein concentration: 967.1 μg mL−1), 279.8 mg trans-cuticular ES antigen (216 mL, protein concentration: 1295.3 μg mL−1) and 329.66 mg of the CSO antigen (100 mL, protein concentration: 3296.6 μg mL−1). The control group received 150 mL 0.9% NaCl solution.
Collection of pig intestinal mucosa samples
Pigs were euthanized 3 days after inoculation by bolt shot and subsequent exsanguination. After immediate removal of the intestines, intestinal tissue samples of approximately 5 × 3 cm2 each were taken for quantitative real-time polymerase chain reaction (qPCR) and immunoblots approximately 1 m (duodenum) and 6 m (jejunum) distal of the pylorus as well as 1 m (ileum) proximal of the ileocaecal valve. The total jejunal length was on average 12 m, thus, the position of sampling at 6 m reflects the main location of adult roundworms in the middle of the jejunum (Nejsum et al., Reference Nejsum, Roepstorff, Anderson, Jorgensen, Fredholm and Thamsborg2009). Subsequently, the mucosa was stripped with a glass slide, snap-frozen in liquid nitrogen and stored at −80°C until further use.
For Ussing chamber experiments, intestinal segments measuring 50 cm in length were taken directly distal of the aforementioned sampling sites, rinsed with ice-cold 0.9% NaCl and stored in Ussing buffer as previously described (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a, Reference Koehler, Springer, Issel, Klinger, Wendt, Breves and Strube2021b).
Functional analyses of nutrient transport by Ussing chamber experiments
After opening and removal of the serosa, intestinal tissues were mounted in Ussing chambers with an exposed mucosal surface area of 1.00 cm2 to measure electrogenic nutrient transport (Clarke, Reference Clarke2009). Eight Ussing chambers were used per intestinal segment and animal, of which 4 chambers were used for glucose transport measurements and 2 chambers each for alanine and glycyl-l-glutamine (glygln) transport measurements.
The composition of Ussing buffers and the basic procedure have been previously described by Koehler et al. (Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a, Reference Koehler, Springer, Issel, Klinger, Wendt, Breves and Strube2021b). Briefly, after setting the potential differences to 0 mV, 20 min of equilibration were allowed before the tested substrates (either 5 mm glucose, 10 mm alanine or 10 mm glygln) were added to the mucosal side of the respective chambers and the short-circuit current (I sc) as well as tissue conductance (G t) were measured. In order to obtain glucose flux rates, 5 μCi 3H-d-glucose were added to the glucose-containing chambers 10 min after the addition of 5 mm glucose to either the mucosal or the serosal side. From the radioactive side, 50 μL samples were taken after 20 min of equilibration and 60 min after 5 μCi 3H-d-glucose addition, additionally to 4 500-μL samples which were obtained in 15 min intervals from the unlabelled side starting 20 min after the addition of labelled glucose. Radioactivity was measured in decays per min. At the end of each experiment, 10 μ m forskolin was added to serosal side to test for tissue viability. Finally, ΔI sc and ΔG t were calculated by subtracting the basal value before substrate addition from the maximal value after addition, and the net glucose flux rate (J net) was determined by subtracting the serosal-to-mucosal flux rate (J sm) from the mucosal-to-serosal flux (J ms).
Transcriptional qPCR analysis of nutrient transport-associated genes
RNA extraction, cDNA synthesis and qPCR experiments were conducted as described by Koehler et al. (Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a). In brief, mRNA extraction from 30 to 40 μg of frozen duodenal, jejunal and ileal mucosa was achieved with the GenElute Direct mRNA Miniprep Kit (Sigma-Aldrich, Taufkirchen, Germany) and the RNA to cDNA EcoDry™ Premix (OligodT) stripes (Takara Bio Europe, Frankfurt am Main, Germany) were used for cDNA synthesis. For qPCR experiments, cDNA was diluted 1:10 in RNAse-free water and stored at −80°C until further use.
Differential transcription of nutrient transport-associated target genes (SGLT1, GLUT1, GLUT2, Hif1α, IL-4, IL-13, STAT6, PepT1) in relation to 2 reference genes (TATA box binding protein and peptidyl prolyl isomerase A as recommended by Park et al., Reference Park, Kwon, Hwang, Park, Kim and Kim2015) was quantified by duplex qPCR, based on primer-TaqMan MGB probe combinations designed by Koehler et al. (Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a). To quantify transcription levels and amplification efficiencies, plasmid standard dilution series (100–106 copies per μL) for each gene were included in each duplex qPCR run.
Each plate included the co-detection of 2 genes of interest and the 2 reference genes, the respective serial plasmid standard dilutions and a no-template control. Each sample was analysed in duplicate, and each run was replicated (n = 4 technical replicates per sample). Results were analysed with qBase+ software (version 3.2, Biogazelle, Ghent, Belgium). Averaged baseline-corrected sample fluorescence (dRn) was normalized against reference genes, inter-run calibrated and corrected for run-specific amplification efficiencies to obtain the relative quantities of each target gene. Therefore, the average of all samples was set to 1 and used as calibrator.
Expression analysis by semi-quantitative immunoblotting
Immunoblot analyses were conducted on jejunal and ileal mucosa to investigate differential expression of the transporters SGLT1, phosphorylated (p)SGLT1, GLUT2, ASCT1 and PepT1. In addition, expression of Na+/K+-ATPase was assessed, as activity of ASCT1 and NHE3, which may affect the function of PepT1, is dependent on available sodium.
The apical membrane (for SGLT1, pSGLT1, ASCT1 and PepT1) and the basolateral membrane (for GLUT2 and Na+/K+-ATPase) of IECs were prepared from 1.5 g of intestinal mucosa by sub-cellular fractioning as previously described (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a). Briefly, tissue was homogenized and separation of apical from crude membrane proteins (containing the basolateral proteins) was achieved through precipitation by dropwise addition of calcium chloride (final concentration of 100 mm). To enrich the crude membrane proteins, 2 mL of the homogenate were centrifuged (25 830 g, 4°C, 60 min). For enrichment of apical membrane proteins, 7.5 mL of the homogenate was centrifuged at 2000 g at 4°C for 30 min, followed by a second centrifugation step of 4 mL of the resulting supernatant (25 830 g, 4°C, 60 min). The pellet was dissolved in resuspension buffer (10 mmol L−1 TRIS base, 150 mmol L−1 NaCl, pH 7.4) with the addition of Protease Inhibitor Cocktail (P8340) and Phosphatase Inhibitor Cocktail (P5726) (Sigma-Aldrich, Taufkirchen, Germany).
For immunoblotting according to Koehler et al. (Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a), samples were loaded on sodium-dodecyl-sulphate-polyacrylamide gels and transferred to nitrocellulose membranes (Amersham, Freiburg, Germany). Membranes were incubated with the primary antibody at 4°C overnight, washed 3 times with TBS-Tween and then incubated with the respective horseradish-peroxidase conjugated secondary antibody for 90 min at room temperature. To measure the pSGLT1/SGLT1 ratio, the protocol was modified as follows: after incubation with the primary pSGLT1 antibody, the membrane was stripped, washed twice with TBS-Tween and blocked again. Afterwards, the membrane was exposed to the primary SGLT1-specific antibody before incubation with the respective secondary antibody. SuperSignal® West Dura Extended Duration Substrate was used for detection of SGLT1, ASCT1, PepT1 and Na+/K+-ATPase while SuperSignal® West Femto Maximum Sensitivity Substrate (both from Thermo Fisher Scientific, Waltham, USA) was used for pSGLT1 and GLUT2 according to the manufacturer's instructions. Images were taken with ChemiDoc™ MP imaging system and band intensities were analysed with Image Lab 5.2.1 software (both from Bio-Rad Laboratories, Feldkirchen, Germany).
To normalize target band intensity to the total protein content of the samples, membranes were stained with Indian ink [fountain pen ink 4001, Pelikan, Hannover, Germany, with 2% (v/v) glacial acetic acid] and the ratio between total and target protein contents was calculated.
Statistical analyses
The results of short-circuit current (ΔI sc), glucose net flux rates (J net), transcription and expression analyses are presented as arithmetic means ± s.d. Comparisons between exposure and control groups were performed by Mann–Whitney U tests using GraphPad Prism (v 8.0.1, San Diego, California, USA). Differences were regarded as statistically significant if P ⩽ 0.05.
Results
Parasitological analyses
All fecal samples taken from the study animals after arrival were coproscopically negative for helminth eggs or other parasite stages. On the day of necropsy, the control animals as well as the animals inoculated with the different A. suum antigens remained coproscopically negative, while the 6 pigs experimentally infected by adult worm transfer were positive for A. suum eggs. During examination of deposited feces, expulsion of 2 worms 1 day prior to necropsy was noted in 2 pigs each, while 1 pig expelled 3 worms. By necropsy, milk spots were not observed in any of the experimental animals.
Nutrient transport modulation analyses
A comprehensive overview of the results of the functional, transcriptional and expression analyses in the duodenum, jejunum and ileum after exposure of pigs to adult A. suum worms or total ES, trans-cuticular ES and CSO antigens is given in Fig. 1.

Fig. 1. Heat maps showing the decreased (blue) or increased (red) mean fold-change of transcriptional, expression and functional data of pigs exposed to adult Ascaris suum worms or different antigen fractions, respectively, compared to the respective control group in the duodenum (a), jejunum (b) and ileum (c). Significant differences as determined by Mann–Whitney U test are indicated with asterisks (P ⩽ 0.05). ES, excretory–secretory antigen; CSO, cuticular somatic antigen.
Functional modulations in short-circuit currents (ΔI sc) and glucose net flux rates (J net)
The results of trans-epithelial transport processes in the different intestinal sections are displayed in Fig. 2 and Supplementary Table 2, showing that after exposure of pigs to adult A. suum worms or trans-cuticular ES antigens, no significant effects on nutrient transport were recorded on any functional level. By contrast, in pigs inoculated with total ES antigens, a significantly increased ΔI sc of glucose (P = 0.026) as well as an increased net flux rate of 3H-d-glucose (J net; P = 0.026) were detected in the duodenum. Furthermore, the transport (ΔI sc) of alanine and glygln was significantly increased in the duodenum (P = 0.026 and P = 0.009) as well as in the jejunum (P = 0.015 and P = 0.015).

Fig. 2. Results of Ussing chamber measurements on duodenal, jejunal and ileal mucosa 3 days after exposure to adult A. suum worms or total ES, trans-cuticular ES and CSO antigens. Graphs display the short-circuit current (ΔI sc) in response to mucosal addition of 5 mm glucose (left y-axis) and the calculated 3H-glucose net flux rate after the addition of 5 μCi 3H-d-glucose (J net, right y-axis) (a–c) as well as short-circuit currents (ΔI sc) in response to mucosal addition of 10 mm alanine (d–f) or 10 mm glygln (g–i). Results are shown as arithmetic means ± s.d. Significant differences as determined by Mann–Whitney U test are indicated with asterisks (P ⩽ 0.05). ES, excretory–secretory antigen; CSO, cuticular somatic antigen.
Pigs exposed to CSO antigens showed a significant decrease of the 3H-d-glucose net flux rate in the ileum (P = 0.041), but – similar to the total ES antigen-treated pigs – an increased alanine transport in the duodenum (P = 0.015) and jejunum (P = 0.002), while glygln transport was increased in the jejunum only (P = 0.002).
Functional modulations in tissue conductance (G t)
Just before the addition of the substrates glucose, alanine or glygln, G t was compared between the exposed and control groups. Pigs exposed to adult A. suum worms showed a higher G t in the ileum chambers used for alanine and glygln transport measurements (U = 0, P = 0.002 each). Further, G t significantly increased in the jejunum of pigs exposed to total ES antigens in glucose (U = 4, P = 0.026) and alanine (U = 2, P = 0.009) chambers. In pigs exposed to trans-cuticular ES antigens, G t decreased in the duodenum, used in chambers for glucose (U = 5, P = 0.041) and glygln (U = 1, P = 0.004) measurements, and in the jejunum in glygln chambers (U = 1, P = 0.004). No significant changes in G t were noted in the ileum of any exposed group.
Transcriptional modulations of nutrient transport-associated genes
Transcriptional data of analysed genes associated with intestinal nutrient transport are presented in Fig. 3 and Supplementary Table 3. In pigs exposed to adult roundworms, the transcription rate of GLUT1 and STAT6 significantly increased in the duodenum (P = 0.026 each), but decreased in the jejunum (P = 0.002 and P = 0.004). Further, Hif1α and PepT1 transcriptions decreased (P = 0.002 each), while IL-4 transcription was 16 times higher compared to the control group (P = 0.002). In the ileum, however, IL-4 transcription underwent a significant decrease (P = 0.017) and IL-13 was increased (P = 0.026, Fig. 3c).

Fig. 3. Transcription data of nutrient transport-associated genes in the duodenal, jejunal and ileal mucosa 3 days after exposure to adult A. suum worms (a–c) or total ES, trans-cuticular ES and CSO antigens (d–f). Results are shown as arithmetic means ± s.d. Significant differences as determined by Mann–Whitney U test are indicated with asterisks (P ⩽ 0.05). ES, excretory–secretory antigen; CSO, cuticular somatic antigen.
Regarding exposure to adult A. suum antigens, striking differences were noted between the different antigens and intestinal sections, respectively. After total ES antigen inoculation only the duodenal GLUT2 transcription was altered (P = 0.041, Fig. 3d). This increase remained in the jejunum, where additionally the 2 other glucose transporters as well as Hif1α and PepT1 were upregulated (GLUT1 and GLUT2: P = 0.004; SGLT1 and Hif1α: P = 0.002; PepT1: P = 0.026). However, none of these genes was significantly regulated in the ileum, where IL-13, IL-4 and STAT6 were significantly affected by either up- (IL-13, P = 0.002) or downregulation (IL-4: P = 0.041; STAT6: P = 0.015).
Following exposure to trans-cuticular ES antigens, most genes were significantly regulated in the duodenum, with GLUT1 (P = 0.004), Hif1α, STAT6 and PepT1 (P = 0.002 each) showing increased transcription compared to the control group, while IL-4 transcription was decreased (P = 0.002). In the jejunum, Hif1α and PepT1 showed a decreased transcription (P = 0.015 and 0.041), while the other mentioned genes returned to unaltered levels. Additionally, jejunal transcription of IL-13 was significantly affected in terms of an upregulation (P = 0.015). The described significant jejunal regulations of Hif1α, PepT1 and IL-13 persisted in the ileum (P = 0.002 each) in addition to decreased levels of GLUT1 and STAT6 (P = 0.002 each).
Exposure to CSO antigens led to the most significant effects in the duodenum, with increased transcription rates of each glucose transporter (SGLT1 and GLUT2, P = 0.009; GLUT1, P = 0.026) as well as Hif1α (P = 0.002) and STAT6 (P = 0.004), while PepT1 transcription decreased (P = 0.002). Of these, only GLUT2 transcription remained increased in the jejunum (P = 0.041), where IL-13 also underwent transcriptional upregulation (P = 0.009). The latter upregulation was still observable in the ileum (P = 0.002), whereas the other significant transcriptional alterations in the ileum were downregulation of IL-4 (P = 0.004), STAT6 (P = 0.009), Hif1α (P = 0.026) and PepT1 (P = 0.008).
Expressional modulations of nutrient transport-associated proteins
Nutrient transport-associated protein expression profiles examined in the jejunum and ileum are displayed in Fig. 4 and Supplementary Table 4. Pigs exposed to adult A. suum worms revealed no significant changes in protein expression in the jejunum, while a significant reduction of GLUT2 and PepT1 expression (P = 0.026 each) was noted in the ileum.

Fig. 4. Expression data of nutrient transport-associated proteins in the jejunal and ileal mucosa 3 days after exposure to adult A. suum worms (a, b) or total ES (c, d), trans-cuticular ES (e, f) and CSO antigens (g, h). Results are shown as arithmetic means ± s.d. Significant differences as determined by Mann–Whitney U test are indicated with asterisks (P ⩽ 0.05). ES, excretory–secretory antigen; CSO, cuticular somatic antigen.
Following total ES antigen inoculation, pSGLT1 expression was decreased in the jejunum, but increased in the ileum (P = 0.009 each). Exposure to trans-cuticular ES antigens resulted in increased GLUT2 expression in the jejunum (P = 0.026), and decreased Na+/K+-ATPase expression in the ileum (P = 0.009). CSO antigens revealed no significant effects on protein expression, either in the jejunum or ileum. Representative immunoblots of the significantly regulated proteins are shown in Fig. 5.

Fig. 5. Immunoblots of nutrient transport-associated proteins in the jejunal and ileal mucosa of the 6 pigs per group 3 days after exposure to adult A. suum worms (a) or total ES (b) and trans-cuticular ES antigens (c). Only proteins showing significant differences compared to the respective control pigs (Mann–Whitney U test, P ⩽ 0.05) are shown. M, molecular weight marker; ES, excretory–secretory antigen.
Discussion
This study aimed at characterizing the effects of adult A. suum worms and their different antigen fractions having direct contact with the gut mucosa on small intestinal nutrient absorption. In addition to its economic importance in pig production, A. suum infection in pigs can be regarded as a valuable model for human ascariosis due to the close phylogenetic relationship or even conspecificity of A. suum with A. lumbricoides (Leles et al., Reference Leles, Gardner, Reinhard, Iniguez and Araujo2012; Easton et al., Reference Easton, Gao, Lawton, Bennuru, Khan, Dahlstrom, Oliveira, Kepha, Porcella, Webster, Anderson, Grigg, Davis, Wang and Nutman2020).
Based on previous in vitro experiments, there is strong evidence that adult worms or rather their secreted or exposed ES and CSO antigens, respectively, affect intestinal nutrient transport (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a). This study aimed to test this assumption in vivo by inoculating pigs with either adult A. suum via worm transfer, precluding previous effects on the mucosa due to A. suum larval development, or isolated ES and CSO antigens. As the previous in vitro study revealed a profound effect of total ES antigens on nutrient transport (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a), trans-cuticular ES antigen was included in this study to narrow down the antigen fractions responsible for the observed effect. Thirty adult worms per pig were chosen for inoculation as well as antigen production to mimic a realistic natural worm burden of infected pigs (Mejer and Roepstorff, Reference Mejer and Roepstorff2006). A prior study on pigs experimentally infected with A. suum eggs did not produce any clear results regarding effects on intestinal nutrient transport, however, this may have been due to the fact that the study period encompassed mainly the pre-patent phase of the infection (days 21 and 35 pi), with only the latest investigated time point (day 49 pi) corresponding to the onset of patency and thus to the presence of mature or nearly mature worms (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a). Here, adult worms were expected to cause a major impairment of transport processes, as they expose the mucosa to both ES and CSO antigens.
Surprisingly, however, no functional alteration of glucose, alanine nor dipeptide (glygln) transepithelial transport was measured upon exposure to adult A. suum worm in any intestinal segment. Nevertheless, significant transcriptional regulations of nutrient-associated genes were observed in the small intestine, which were most prominent in the jejunum. As transport processes were rapidly affected after exposure to adult A. suum antigens in vitro (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Strube and Breves2021a), the lack of a measurable functional effect was unexpected. One explanation is that the exposure period of 3 days was not sufficient. Moreover, the antigen concentration was probably much lower than in the in vitro experiment (Koehler et al., Reference Koehler, Springer, Issel, Klinger, Wendt, Breves and Strube2021b), which could explain the absence of a measurable effect on the functional level. Possibly, variation in the number of successfully established worms may have also played a role. A follow-up study with a larger number of infected pigs will be necessary to investigate the quantitative effect of worm burden on alterations in nutrient transport physiology. Nevertheless, pigs also carry different worm burdens under field conditions, so a similar picture can be expected in natural situations. Despite the absence of statistically significant functional alterations, a significant downregulation of GLUT1, STAT6, Hif1α and PepT1 transcription in the jejunum as well as GLUT2 and PepT1 expression in the ileum indicates a negative impact of infection on transport physiology. Additionally, the increased tissue conductance observed with regards to ileal mucosa used for alanine and glygln transport measurements may have masked a downregulation on the functional level in this intestinal compartment.
In contrast, GLUT1 and STAT6 transcription were increased in the duodenum. As the main location of adult roundworms is a 3 m long section in the middle of the jejunum, retrograde transport of A. suum antigens to the duodenum seems unlikely (Nejsum et al., Reference Nejsum, Roepstorff, Anderson, Jorgensen, Fredholm and Thamsborg2009). Rather, the increase of GLUT1 and STAT6 transcription in the duodenum may have been a compensatory reaction to the observed downregulation in the jejunum and ileum.
In contrast to the exposure to adult worms, an overall upregulation of gene transcription and an increased nutrient transport were observed in proximal parts of the small intestine after exposure to total ES and CSO antigens. In the jejunum, inoculation of these antigen fractions resulted in an increased alanine and glygln transport, whereas glucose transport was not significantly altered. However, an upregulation of all 3 glucose transporters, as well as Hif1α and PepT1, was observed after exposure to total ES antigens, whereas pSGLT1 expression was decreased. In pigs, it is not yet clear whether SGLT1 phosphorylation via PKA results in an increased or a decreased transporter activity (Klinger and Breves, Reference Klinger and Breves2018; Klinger et al., Reference Klinger, Lange, Brandt, Hustedt, Schroder, Breves and Herrmann2018). After exposure to CSO antigens, only GLUT2 transcription was significantly increased in the jejunum. Interestingly, the upregulation of transport processes was even more pronounced in the duodenum. Regarding total ES antigens, a significant increase of short-circuit currents of all nutrients (glucose, alanine and glygln) was noted in addition to increased glucose net flux rates. The enhanced transport of glucose could be due to an increase of GLUT2 expression, as the transcription rate was significantly increased. However, while exposure to CSO upregulated the transcription of all 3 glucose transporters as well as Hif1α, no increased functional glucose transport in terms of an increased short-circuit current or net flux rate was observed. Whether this is due to a delayed translation of gene transcription to expression, e.g. in case of post-translational modifications, or to other reasons remains to be elucidated in future studies.
Trans-cuticular antigens yielded primarily upregulation in the duodenum and a mixed pattern in the jejunum, but induced no functional alterations. This might indicate that the ES fraction released via the mouth and/or anal opening, which is contained in the total but not trans-cuticular ES, is essentially driving the functional transport changes. It remains to be investigated whether a constant, additive or even synergistic effect is exerted on the functional level in interaction with CSO, which likewise induced increased alanine and dipeptide transport.
However, when interpreting the functional measurements, alterations of tissue conductance (G t) should be taken into account. An increase of G t was noted in the jejunum of the ES antigen-treated group prior to alanine addition, which may have contributed to the increase of ΔI sc in these Ussing chambers. However, G t was not altered in the duodenum, indicating that active alanine transport was indeed increased. Despite the functional increase in jejunal alanine transport, expression of ASCT1 and Na+/K+-ATPase was not significantly affected. So far, it is known that ASCT1 activity is inhibited by phosphorylation via protein kinase C α (PKCα) or PKA, e.g. mediated by leucotriene D4 (LTD4) during chronic inflammation (Arthur and Sundaram, Reference Arthur and Sundaram2014). LTD4 increases the intracellular calcium concentration, thus activating the PKC signal transduction pathway (Thodeti and Sjolander, Reference Thodeti and Sjolander2002). Therefore, A. suum antigens might have affected the calcium channels of the IECs, which should be addressed in further studies. Likewise, dipeptide (glygln) transport was increased despite unaltered PepT1 expression. Therefore, the absorption of dipeptides may have been modulated via (de-)phosphorylation of the NHE3 by PKA (Zhao et al., Reference Zhao, Wiederkehr, Fan, Collazo, Crowder and Moe1999; Donowitz and Li, Reference Donowitz and Li2007; Kocinsky et al., Reference Kocinsky, Dynia, Wang and Aronson2007). Di- and tripeptides are transported against an electrochemical proton gradient, which is in part maintained by NHE3 (Kennedy et al., Reference Kennedy, Leibach, Ganapathy and Thwaites2002; Watanabe et al., Reference Watanabe, Kato, Ito, Kubo, Sai and Tsuji2005).
Overall, the observed increase in transport processes and gene transcription in the duodenum and jejunum was unexpected, but may have been preceded by a transient downregulation. As the antigens were applied as a single dose, the time span of 3 days until sampling may have been too long to capture such a transient effect, especially considering the small intestinal transit time of only 2–4 h (Henze et al., Reference Henze, Koehl, Bennett-Lenane, Holm, Grimm, Schneider, Weitschies, Koziolek and Griffin2021). The observed upregulation may have been a mechanism of the host to counter-regulate the preceding glucose loss or inability to absorb glucose, especially as a rather high antigen concentration was applied.
The observed upregulation dissipated further along the intestinal axis and switched to a mainly down regulatory pattern on the transcriptional level after exposure to all 3 antigen fractions in the ileum, similar to the changes induced by adult A. suum worms. In addition, a significantly decreased ileal glucose net flux rate (J net) was measured after CSO antigen treatment. J net constitutes a more accurate measurement of glucose transport than ΔI sc, as ΔI sc is affected by the transport of other charged molecules (Harari et al., Reference Harari, Russell and Castro1987; Shea-Donohue et al., Reference Shea-Donohue, Sullivan, Finkelman, Madden, Morris, Goldhill, Pineiro-Carrero and Urban2001). Overall, this confirms previous studies demonstrating reduced glucose absorption due to A. suum or their antigens (Dawson et al., Reference Dawson, Beshah, Nishi, Solano-Aguilar, Morimoto, Zhao, Madden, Ledbetter, Dubey, Shea-Donohue, Lunney and Urban2005; Solano-Aguilar et al., Reference Solano-Aguilar, Shea-Donohue, Madden, Quinones, Beshah, Lakshman, Xie, Dawson and Urban2018; Koehler et al., Reference Koehler, Springer, Issel, Klinger, Wendt, Breves and Strube2021b). On reaching the ileum, the A. suum antigens may have already been partially degraded, resulting in a lower concentration as compared to the duodenum and jejunum, and thus causing less of a counter-regulation and more similar alterations compared to natural infections.
In the duodenum as well as in the ileum, trans-cuticular ES and CSO antigens caused similar patterns on the transcriptional level, e.g. an increase of GLUT1, Hif1α, STAT6 and PepT1 in the duodenum, but a decrease of Hif1α and PepT1 in the ileum. This can easily be explained by the fact that both antigen fractions probably contained similar (trans-)cuticular proteins.
Results with regard to the Th2 cytokines IL-4 and IL-13 did not fully correspond to the expected pattern. IL-13 transcription was consistently increased in all experimental groups in the ileum, but only in trans-cuticular and CSO-treated groups in the jejunum, while no significant changes were observed in the duodenum. In contrast, IL-4 transcription was increased in the jejunum, but decreased in the ileum of pigs exposed to adult A. suum. The decrease in the ileum was also observed after total ES and CSO treatment. It has been suggested that regulation of IL-13 primarily takes place on the receptor level, whereas regulation of IL-4 signalling occurs at the transcriptional level (Daines and Hershey, Reference Daines and Hershey2002). Regulation of IL-4 expression is complex and involves several transcription factors, re-stimulation by antigens and other cytokines or inflammatory molecules produced by various cell types, e.g. mast cells, and is therefore hardly predictable in vivo (Guo et al., Reference Guo, Hu-Li and Paul2004; Paul and Zhu, Reference Paul and Zhu2010; Hepworth et al., Reference Hepworth, Danilowicz-Luebert, Rausch, Metz, Klotz, Maurer and Hartmann2012).
Conclusions
In summary, adult A. suum and their different antigen fractions affected intestinal transport physiology in this study, demonstrating that larval development is not required to trigger physiological effects. However, the observed effects were not always in the expected direction and should be confirmed in future studies. For the planning of future experiments, correct exposure period seems crucial. While exposure to adult worms led to a downregulation of relevant molecules for glucose transport on the transcription and expression levels, modulation of functional transport processes was not observed within the period of 3 days. Possibly, a longer exposure time would have been needed for functional alterations to become apparent. In contrast, 3 days after a single exposure to A. suum antigens may have been too late to capture a transient downregulation, and the observed upregulation may have been the result of a counter-regulatory strategy of the host in the face of the high, single-dose antigen concentration. A continuous exposure to lower antigen concentrations might be more representative of natural infections. In addition, measuring relevant metabolites in host serum will allow further insights into the metabolic consequences of altered intestinal physiology. As A. suum in pigs serves as a model for human ascariosis, these insights are also relevant for human health and contribute to the understanding of malnutrition in helminth-infected children.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0031182022001512.
Data availability
Data supporting results are provided within the article and in the Supplementary materials.
Acknowledgements
The authors thank Ulla Küttler, Daniela Jordan, Marion Burmester, Karin Hustedt, Kerstin Kiri, Nadine Schnepel, Dirk Voigtlaender and Michael Rohde for excellent technical assistance.
Author's contributions
G. B. and C. S. conceived and planned the experiments and acquired the funding. M. W. performed sedation, surgeries and inoculation of the experimental animals. S. KO. and N. I. carried out the Ussing chamber experiments and analysed the data. S. KL. contributed to Ussing chamber data analysis. S. KO. carried out the qPCR and analysed the data. N. I. carried out the western blots and analysed the data. S. KO., A. S. and N. I. performed the statistical analyses. S. KO., A. S., S. KL., G. B. and C. S. interpreted the data. S. KO. and A. S. drafted the manuscript. S. KL., M. W., G. B. and C. S. revised and edited the manuscript. All authors read and approved the final manuscript.
Financial support
This research was funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation), grant numbers BR 780/23-1 and STR 1171/14-1.
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical standards
Animal experiments were performed in accordance with the German Animal Welfare act in addition to national and international guidelines for animal welfare. Experiments were permitted by the ethics commission of the Animal Care and Use Committee of the German Lower Saxony State Office for Consumer Protection and Food Safety (Niedersächsisches Landesamt für Verbraucherschutz und Lebensmittelsicherheit) under reference number 33.19.42502-04-16/2272.