Introduction
Caregivers of cancer patients suffer a profound impact on their well-being and quality of life (Girgis et al., Reference Girgis, Lambert and Johnson2013; Sun et al., Reference Sun, Raz and Kim2019). Their emotional burden worsens when their loved one is hospitalized and requires an intensive care unit (ICU) admission. Moreover, as the cancer population is at high risk of developing life-threatening events that require intensive care treatment (Wallace et al., Reference Wallace, Rathi and Waller2016; Gutierrez et al., Reference Gutierrez, McEvoy and Mead2018; Cuenca et al., Reference Cuenca, Laserna and Reyes2020), developing and enacting better family-centered care strategies for critically ill cancer patients is paramount. Increasing family engagement has been associated with a shorter ICU stay (Lee et al., Reference Lee, Park and Jang2019), decreased cardio-circulatory complications (Fumagalli et al., Reference Fumagalli, Boncinelli and Lo Nostro2006), and reduced patient falls (Dupree et al., Reference Dupree, Fritz-Campiz and Musheno2014) without increasing infection rates or adverse events (Adams et al., Reference Adams, Herrera and Miller2011; Bishop et al., Reference Bishop, Walker and Mark Spivak2013).
Historically, ICUs have maintained strict policies about visitation and family-centered care (Liu et al., Reference Liu, Read and Scruth2013). However, the belief that patients in the ICU benefit from restricted visitation has been contradicted by evidence that social isolation can increase morbidity and mortality (Cacioppo et al., Reference Cacioppo, Hawkley and Norman2011). The COVID-19 pandemic has highlighted the various deleterious psychological effects that prohibiting visitation can generate in patients, families, and healthcare providers (Azoulay et al., Reference Azoulay, Curtis and Kentish-Barnes2021). The Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU suggest that family members of critically ill patients be “offered open or flexible family presence at the bedside” (Davidson et al., Reference Davidson, Aslakson and Long2017). Despite this, hospitals’ visitation policies in their ICUs still vary widely (Liu et al., Reference Liu, Read and Scruth2013). Strict visitation policies cause the families to stay mainly in the ICU waiting room, making them feel less engaged with the care of their loved ones (Davidson et al., Reference Davidson, Aslakson and Long2017). For these reasons, waiting rooms should be a place of comfort with nearby restrooms and places to eat, and should post easily read signage to help family members navigate around (Deitrick et al., Reference Deitrick, Ray and Stern2005; Karlsson et al., Reference Karlsson, Tisell and Engstrom2011).
To enhance the ICU family engagement and overall satisfaction of care by patients and their families, we participated in a national performance improvement study called the Patient-Centered Outcomes Research (PCOR) Collaborative (Kleinpell et al., Reference Kleinpell, Zimmerman and Vermoch2019). We implemented multilevel patient- and family-centered initiatives that were focused on (1) applying an open visitation policy (OVP), (2) using daily two-way communication boards, and (3) enhancing the ICU waiting room experience. Here, we report the perspectives of both the families and the ICU practitioners on these performance improvement initiatives.
Methods
Study design and setting
This “before and after” performance improvement multilevel intervention study was approved by the Qualitative Institutional Review Board and was conducted in the 34-bed medical and 18-bed surgical ICUs at the University of Texas MD Anderson Cancer Center. A multidisciplinary workgroup consisting of physicians, nurses, advanced practice providers, pharmacists, physical therapists, occupational therapists, dieticians, patient educators, patient advocates, chaplains, social workers, ethicists, and volunteer services was formed. The workgroup was involved in planning, addressing concerns, enabling information dissemination, and implementing patient- and family-centered care initiatives. In order to achieve a substantial improvement in family-centered care, the team decided to execute multiple initiatives simultaneously in a multilevel fashion.
To be considered eligible to participate in the study, respondents must have been caregivers of a patient admitted to the ICU or a healthcare provider who primarily worked in the ICU. We conducted pre-intervention (PRE) and the post-intervention (POST) surveys for families of patients admitted to the ICU and for ICU practitioners. The PRE surveys were carried out 1 month before the implementation period. At the same time, the institution renovated the ICUs and waiting rooms following the SCCM ICU design guidelines (Thompson et al., Reference Thompson, Hamilton and Cadenhead2012). After a 6-month implementation period, the POST surveys were conducted. Consequently, there were two separate groups of family members who responded to the surveys (Figure 1). Potential participants were approached by the research team, only those who were willing to participate in the study were offered the links to the survey. The web secure database REDCap was used to anonymously collect and store all the survey data.

Fig. 1. Study schema.
Initiatives
Open visitation policy
A visitor pass system was implemented that allowed each family to have two passes to the ICU. One was a 24-h pass, allowing one family member to stay in the patient's room at any time during the day or night. The second pass allowed a second family member to be in the patient's room between 10:00 AM and 10:00 PM.
Two-way communication boards
We implemented this initiative early to optimize communication between patients, families, and caregivers. Daily goals were established for every patient during multidisciplinary rounds in the morning. Nurses updated the daily goals board with a minimum of two to three goals to be accomplished for the day, and subsequently, with a multidisciplinary approach, the ICU team addressed the goals with patients and families. Audits were performed daily to identify and overcome potential barriers. Patients and families were encouraged to write questions or concerns to the ICU team on the board.
Enhanced waiting room experience
We worked with volunteer services to provide therapeutic coloring books and daily coffee services to the waiting room. A comprehensive calendar was created to inform that family members of events could participate in free of charge. We held events such as ICU family celebrations, card-making sessions, and holiday music therapy sessions directed by a certified music therapist. The calendar also included MD Anderson's Integrative Medicine Program events such as yoga meditation, drumming sessions, Tai Chi, group singing, and cooking lessons.
Surveys
The PCOR collaborative leadership provided the surveys for this study (Kleinpell et al., Reference Kleinpell, Zimmerman and Vermoch2019). The family/caregiver participants’ surveys were based on the Family Satisfaction with Care in the ICU Survey (Wall et al., Reference Wall, Engelberg and Downey2007), which has well-established reliability and validity (Kleinpell et al., Reference Kleinpell, Zimmerman and Vermoch2019). The questions addressed demographic information, staff competence, treatment of family, communication, waiting area environment, and overall family satisfaction. The ICU practitioners responded to the Patient- and Family-Centered Adult Intensive Care: A Self-Assessment Inventory (A Self-Assessment Inventory, 2019). The questions inquired about demographics such as age, sex, ICU practitioner role, years of practice, experience in the ICU, personal and professional experience with family presence, and family-centered care integration. Additionally, both the caregivers’ and practitioners’ POST surveys also included specific questions evaluating the implemented local initiatives (Kleinpell et al., Reference Kleinpell, Zimmerman and Vermoch2019). All surveys were based on a Likert scale.
Statistical analysis
Descriptive analyses were performed for patients’ family and ICU practitioner demographics and responses. For categorical variables, counts and frequencies were reported. Frequencies were calculated based on the non-missing values. For continuous variables, mean and standard deviation were reported. Differences between the PRE and POST intervention surveys were calculated using the Χ2 test. All statistical analyses were performed using the statistical software IBM SPPS Statistics for Windows, version 25 (SPSS Inc., Chicago, IL, USA).
Results
A total of 159 (PRE = 79 and POST = 80) family members completed the surveys. Table 1 describes the demographics and basic information of the participants. The families’/caregivers’ roles included daughter (21%), wife (17%), son (13%), parent (8%), and husband (5%). “Others” involved extended family members (partner, brother, sister, and other) (18%). Almost half of the caregivers (50.9%) had previous experience caring for a family member in the ICU. Approximately 42% of the caregivers lived with the patients. A total of 147 (PRE = 95 and POST = 52) ICU practitioners participated in the surveys. Most of them were nurses (43%), followed by advanced practice providers (12%), clinical pharmacists (12%), physicians (9%), respiratory therapists (9%), and others such as occupational therapists, speech therapists, and dieticians (15%).
Table 1. Demographics and basic information of the participants
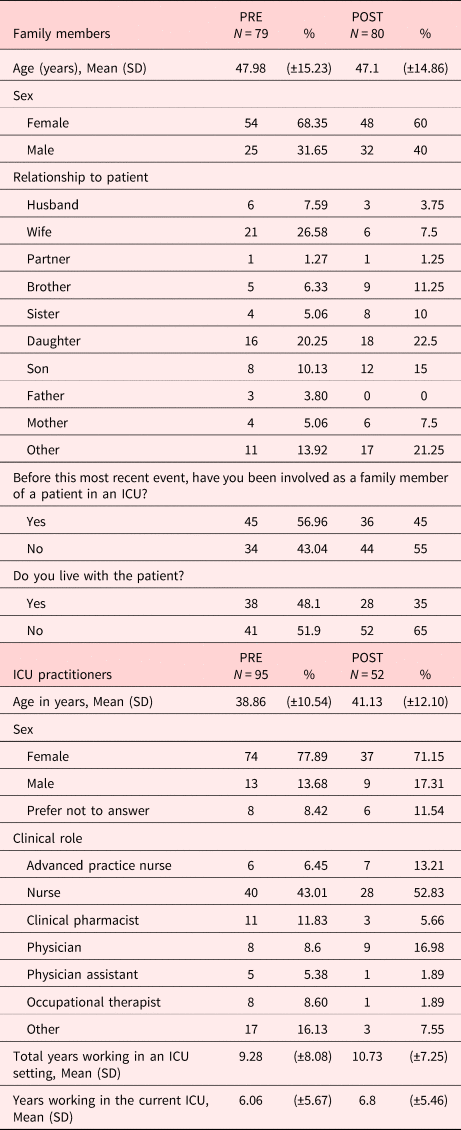
ICU, intensive care unit.
Family members’ perspectives
Overall, in the 159 caregivers (PRE and POST combined), the “excellent” to “very good” response for “ease of getting information” was 72%. The “fair” to “poor” response was 8%. The “excellent” to “very good” responses for “understanding of information” were 74% and the “fair” to “poor” responses were 5%. Regarding their understanding of information, 74% of the participants rated it as “excellent” or “very good” and just 5% considered it “fair” or “poor”. About 73% of caregivers responded “excellent” to “very good” with regard to the “completeness of information,” indicating that most family members were satisfied with how well the information regarding their loved ones was conveyed to them by the care team. A much lower percentage of respondents (8%) reported that “completeness of information” was “fair” to “poor.” Most (71%) of the families were satisfied with the “consistency of information,” indicating that they received similar messages from doctors and nurses, etc. A very small portion of relatives (9%) responded “fair” to “poor.” About 59% of families responded “excellent” to “very good” about the “frequency with which ICU doctors communicated information.” A few families (15%) felt less satisfied, responding “fair” to “poor.” The “excellent” to “good” response for family care and concern by ICU staff was 91%. The responses of the family members by PRE and POST are summarized in Table 2;. Overall, the “excellent” response rate increased from PRE to POST; however, none of the improvements were statistically significant.
Table 2. Family members’ perspectives on information dissemination and decision-making process

N/A responses were excluded from the frequency calculations.
ICU, intensive care unit.
Most of the relatives (80%) felt included in the decision-making process (“very” 55%, “somewhat included” 25%). Fewer relatives felt excluded (9%). There was a statistically significant increase in the rate of “very included” in the decision-making process from the PRE to POST (p < 0.001). A considerable number (78%) felt supported during the process, whereas 8% felt totally or somewhat overwhelmed. A significantly higher rate of participants felt very supported (p = 0.011) after the implementation of the initiatives. About half (45%) of the relatives believed that they had good control of the process, whereas 30% felt less in control, and just 9% felt that the process was somewhat or completely out of their control. The proportion of respondents who felt in control of the process in the POST survey was higher than in the PRE survey (p = 0.005). About 13% of the caregivers believed that they needed more time to make decisions or to discuss or address their concerns.
Caregivers’ perspectives regarding the ICU waiting room areas, OVP, and daily goal boards are presented in Supplementary Table 1. Among the 159 caregivers (PRE and POST combined) who responded to the survey, 71% considered their satisfaction with the ICU waiting area environment to be “excellent” or “very good”. Most respondents described access to the kitchen (69%), nutritious snacks (75%), and laundry facilities (77%) as “very well” to “ok.” Regarding access to place for prayer or reflection, the majority (95%) reported “very well” to “ok” responses. Overall, the “excellent” and “very well” responses rate increased from PRE to POST; however, only access to kitchen facilities (p < 0.001) and nutritious snacks (p = 0.008) were statistically significant. In the POST survey, the families evaluated the OVP and daily board goals. Over half of the respondents knew that the visitation policies had relaxed recently (60.7%), most of them were satisfied with the OVP (89%) and believed that the OVP was helpful for them and their loved ones (87.6%). Likewise, the majority of the participants (77.4%) were aware of the use of the daily goal boards, liked it (81.9%), and agreed that it was helpful for them and their loved ones (81.9%).
ICU practitioners’ perspectives
The ICU practitioners’ perspectives regarding the initiatives are presented in Table 3. Among the 147 respondents (PRE and POST combined), 38% preferred an OVP in the ICU, whereas 42% were in disagreement, and 19% were neutral. Regarding communication with family, 42% of providers believed that the OVP improved it, while 31% disagreed. Almost a quarter of the practitioners (23%) thought that patient care was improved with OVP, whereas 37% disagreed and 40% were neutral. Although 33% responded that OVP was beneficial for the ICU, 41% disagreed and 26% were neutral. In addition, half of them responded that OVP was beneficial for patients, whereas 29% disagreed and 21% were neutral. Most (63%) practitioners agreed that OVP was beneficial for families despite over half of them (51%), believing that it could result in additional work for staff.
Table 3. ICU practitioners’ perspectives about the initiatives
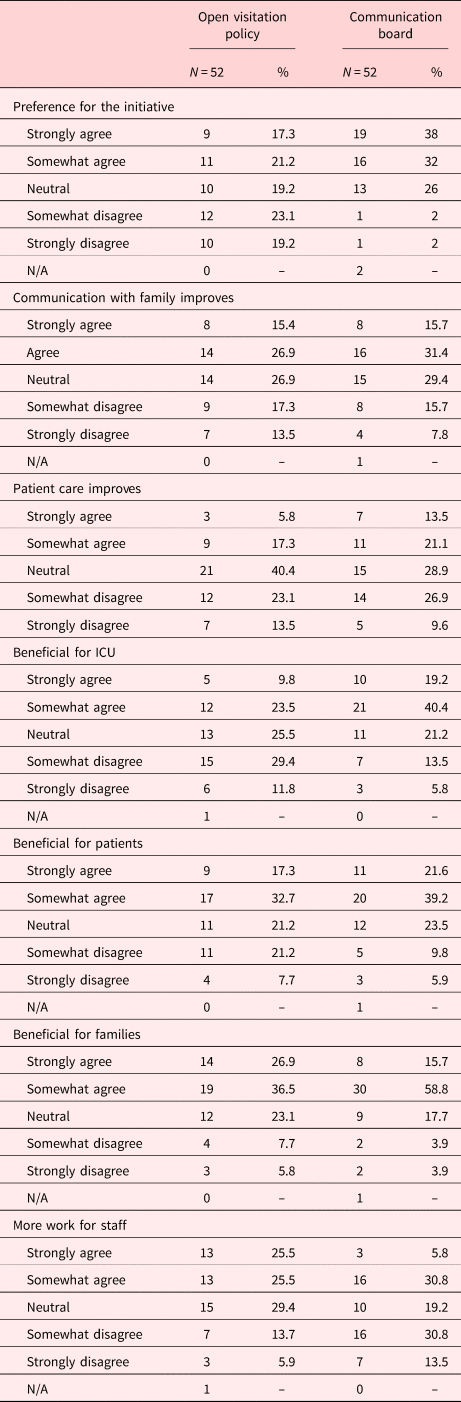
N/A responses were excluded from the frequency calculations.
ICU, intensive care unit.
The use of the two-way communication boards was supported by 70% of the 147 responders, 26% were neutral, and only 4% were in disagreement. While almost half of the ICU practitioners (47%) believed that the board improved communication with patients’ families, only 23% disagreed. More than a third (35%) of the clinicians agreed that patient care improved; however, 65% were either neutral or in disagreement. Even though most of the responders believed it was beneficial for the unit (60%), the patients (61%), and the families (75%); a third agreed that the two-way communication boards created more work for the staff.
Discussion
Our findings suggest that the implementation of OPV, the two-way communication board, and a revamped waiting room experience enhanced communication and engagement between the family members/caregivers and the medical team. For instance, family members felt significantly more included and supported during the clinical decision-making process, which leads to a higher perception of control over medical decisions. Additionally, the three studied initiatives were well received by the family members. On the other hand, among ICU practitioners, the two-way communication board was more accepted than the OVP. More than half of the ICU practitioners believed that the two-way communication boards were beneficial for the unit and the patients. Even though half of the practitioners believed that OVP created additional work for the staff, nearly two-thirds of them also considered this initiative beneficial for the family members. Interestingly, 61.5% of the clinicians (16 out of 26) who believed that OVP created more work also considered it beneficial to the families.
Improving patient- and family-centered outcomes requires a multidisciplinary and coordinated effort. A multilevel approach was selected for this study due to the various facets involved, such as individual caregiver characteristics, medical team interactions, organizational logistics, and institutional policies. Each intervention aimed to improve a different level of influence. For instance, from an organizational level, we enacted an OVP; from a healthcare team level, we implemented the two-way communication boards; and from the families’ environmental level, we renovated the waiting room areas. Despite the potential advantages of conducting multilevel intervention research, interpreting its results is challenging (Clauser et al., Reference Clauser, Taplin and Foster2012; Paskett et al., Reference Paskett, Thompson and Ammerman2016).
This project resulted in several steps toward improved patient- and family-centered intensive care management in cancer patients. Our experience correlates with the growing interest and acceptance of empowering and engaging families and patients by ICU staff (Kleinpell et al., Reference Kleinpell, Heyland and Lipman2018; Naef et al., Reference Naef, Massarotto and Petry2020, Reference Naef, von Felten and Petry2021). Despite the beneficial effects, we encountered barriers with our project. Notably, the ICU staff expressed concerns that the initiatives added additional work strain. There might be some potential explanations for the ICU staff's perception regarding the OVP. First, the use of the ICU visitation passes required the staff to keep track of whether the caregivers were authorized to enter the ICU. Second, sometimes the family members who stayed overnight would accidentally forget to hand over the pass to the following designated caregiver. Dealing with this created unplanned discussions with the family to solve the issue. Third, some caregivers gained entrance to the unit through other entrances not available to the public, which could have made the practitioners feel that their efforts to provide a structured OVP were futile. This phenomenon is not unique to our project. Previous studies have reported the nursing staff concerns that more liberal visitation policies may interfere with their ability to provide excellent patient care (Berti et al., Reference Berti, Ferdinande and Moons2007; Kozub et al., Reference Kozub, Scheler and Necoechea2017). However, ICUs with open visitation reported that families were highly satisfied with the policy (Soury-Lavergne et al., Reference Soury-Lavergne, Hauchard and Dray2012; Chapman et al., Reference Chapman, Collingridge and Mitchell2016). Physicians and nurses in open visitation ICUs tended to view the policy positively as well (Giannini et al., Reference Giannini, Miccinesi and Prandi2013; Chapman et al., Reference Chapman, Collingridge and Mitchell2016).
We also faced difficulties implementing the two-way communication boards. The most commonly reported difficulty by the nursing staff was when other patients occasionally required their attention during rounds, precluding the nurse from writing down that particular patient's goal or taking the extra time to talk to the team and address the family. Despite these issues, family members felt more included in the discussions, which is consistent with the literature. Pronovost et al. (Reference Pronovost, Berenholtz and Dorman2003) carried out a prospective study in which the implementation of daily goal forms resulted in all staff having a better understanding of the goals for individual patients and improved information traffic and communication between families and staff. Additionally, another study reported that implementing ICU daily goal boards decreased the hospital length of stay and reduced errors of omission (Binnekade et al., Reference Binnekade, Brunsveld and Arbous2010).
In light of the obstacles we faced, there is a need to promote the higher acceptance of patient- and family-centered outcomes among the ICU staff. Addressing logistical and operational hurdles expressed by the staff should be a priority. Failing to show willingness to hear their input to improve the initiatives’ workflow could lead to a loss of support from the staff. Another potential action that should be considered is conducting educational sessions about patient-centered outcomes, as this seems to be a viable alternative to reach wider acceptance among the practitioners (Coyne and Dieperink, Reference Coyne and Dieperink2017; Nguyen et al., Reference Nguyen, Bauman and Watling2017).
Other initiatives to improve patients’ and families’ experience in the critical care-related facilities are currently being analyzed before introduction in our unit. For instance, specialized care packages could be provided to the family/caregiver when transitioning to comfort care. This gesture can be used to educate and offer a more empathetic environment for patients, families, and staff during the bereavement process (Oliver et al., Reference Oliver, Hillock and Moore2010). Another strategy is introducing the ICU diary to help support patients and families during their ICU stay. The ICU diary can provide resources for caregiver support and the prevention and management of ICU delirium (Rogan et al., Reference Rogan, Zielke and Drumright2020). Furthermore, the implementation of ICU diaries could also nurture communication and journaling tools that facilitate mental and physical wellness. Future potential interventions must integrate family-centered outcomes with new technologies such as developing a mobile device application that allows easy access to technological education and frequent ICU questions posed by patients and their caregivers. Due to the wide variability between the acceptance and integration of various initiatives, further research on different strategies to successfully increase patient and family engagement is essential.
The present study has several limitations. First, we encountered resistance to cultural change when staff put up barriers to engagement with two-way communication boards. Second, the multilevel implementation of concurrent patient-centered interventions at once made it difficult to isolate the potential beneficial effects of any single measure. Our study could have benefitted from a multilevel regression analysis that could, in part, isolate the effect of each intervention. Third, due to the nature of the study, different families were surveyed before and after the program was enacted. Thus, differences found between the PRE and POST surveys could have arisen from individual inherent factors of the two groups of respondents rather than being a product of the interventions. Fourth, our institution already had high interaction between patient families and ICU practitioners. Thus, this high baseline engagement could have skewed the observed effect. Therefore, our findings should be cautiously interpreted. For instance, the improvement in family communication and engagement and the higher work burden expressed by practitioners in our study might not be similar if the interventions were implemented in different settings such as community nonspecialized cancer centers. Further research should address these concerns.
Conclusions
Our project effectively promoted patient- and family-centered care. The families expressed satisfaction with the communication of information and the decision-making process. Even though more than half of the practitioners agreed that an OVP was beneficial for families, there was a concern that it could create an additional burden to the staff. Practitioners were generally against implementing an OVP and did not believe it would help in patient care. The majority of practitioners supported the use of the two-way communication board which helped transfer information to families and improved their satisfaction. Finally, the added features in the ICU waiting room led to positive changes in family satisfaction. However, due to our limitations, further research is needed to understand whether making this project universal or introducing additional novel practices would significantly benefit patients and families in the ICU.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951521001838.
Acknowledgments
We appreciate the contributions of Mary Ann Oler, education program coordinator of the Department of Critical Care Medicine at The University of Texas MD Anderson Cancer Center, and Tamara K. Locke from the office of Scientific Publications at The University of Texas MD Anderson Cancer Center for their valuable editorial contributions. Part of this work was presented as an abstract in the 49th Annual Critical Care Congress of the Society of Critical Care Medicine, 16-19th February 2020.
Funding
Supported by the NIH/NCI award number P30CA016672. Dr. Nates’ work is supported by the George Sweeney Fellowship, The University of Texas MD Anderson Cancer Center Grant Resources.
Conflict of interest
The authors declare no conflict of interest directly applicable to this research.







