Introduction
Excessive body weight is one of the most challenging public health issues of our time( 1 ). Our relationship with food is important; a recent UK report on securing a positive ‘Food Future’ indicated that consumers feel a loss of connection with food that should be preserved( 2 ). Problematic food and eating behaviours, for example binge and emotional eating, have been characterised in obesity. In mindfulness, an individual observes their immediate experience using an open and non-judgemental stance( Reference Bishop, Lau and Shapiro 3 ). One of the modern-day pioneers of mindfulness is Jon Kabat Zinn who developed the Mindfulness-Based Stress Reduction (MBSR) programme which is used in mainstream medicine internationally, particularly in the management of depression( Reference Kabat-Zinn 4 ). Recent reviews have examined the evidence for mindfulness in the management of pain( Reference Chiesa and Serretti 5 , Reference Zeidan, Grant and Brown 6 ), depression( Reference Klainin-Yobas, Cho and Creedy 7 , Reference Piet and Hougaard 8 ) and psychological well-being( Reference Chiesa and Serretti 9 , Reference Hofmann, Grossman and Hinton 10 ).
In relation to eating behaviours, research began into the use of mindfulness in binge eating with early interventions in the late 1990s when Kristeller & Hallet( Reference Kristeller and Hallett 11 ) undertook a pilot study among obese women with binge eating disorder using Mindfulness-Based Eating Awareness Training (MB-EAT). This intervention was later developed for obese populations with or without binge eating disorder( Reference Kristeller, Baer and Quilian-Wolever 12 ). In recent years there has been increased interest in using mindfulness and mindful eating in obese/overweight and normal-weight populations.
Mindful eating consists of making conscious food choices, developing an awareness of physical v. psychological hunger and satiety cues( Reference Dalen, Smith and Shelley 13 ), and eating healthfully in response to those cues( Reference Miller, Kristeller and Headings 14 ). It is conceptualised as being aware of the present moment when one is eating( Reference Hendrickson and Rasmussen 15 ), paying close attention to the effect of the food on the senses, and noting the physical and emotional sensations in response to eating( Reference Kristeller, Wolever and Sheets 16 ). There is no universal definition of mindful eating but these principles are consistent in the literature.
Intuitive eating is a discreet, but complementary term, often used interchangeably with mindful eating. Intuitive eating was originally defined by two US Registered Dietitians in 1995( Reference Mathieu 17 ) who described ten aspects of intuitive eating including a rejection of ‘diets’, a discouragement of labelling foods as ‘bad’, an encouragement to honour hunger, and allow satisfaction with food intake. Both mindful eating and intuitive eating concentrate on internally focused eating( Reference Anderson, Schaumberg and Anderson 18 ); intuitive eating, however, does not involve meditation( Reference Mathieu 17 ).
A number of recent systematic reviews have been published looking at the effectiveness of mindful eating( Reference Godfrey, Gallo and Afari 19 ), and mindfulness interventions( Reference Katterman, Kleinman and Hood 20 ) in binge eating, and mindfulness-based interventions for eating disorders and obesity and obesity-related behaviours( Reference Godsey 21 – Reference O’Reilly, Cook and Spruijt-Metz 23 ). The three reviews that looked at binge eating showed a positive effect of mindfulness in reducing this maladaptive eating behaviour; the effect sizes were moderate( Reference Katterman, Kleinman and Hood 20 ). Furthermore, there was evidence of its efficacy in emotional( Reference Katterman, Kleinman and Hood 20 , Reference O’Reilly, Cook and Spruijt-Metz 23 ) and external( Reference O’Reilly, Cook and Spruijt-Metz 23 ) eating. The role of mindfulness in weight management was less apparent( Reference Katterman, Kleinman and Hood 20 , Reference Godsey 21 ). The high level of heterogeneity between studies( Reference Katterman, Kleinman and Hood 20 ) and methodological weakness of many studies( Reference Olson and Emery 22 ) were highlighted.
Mindfulness is a key component of interventions based on dialectical behaviour therapy and Acceptance and Commitment Therapy (ACT), which are both third-wave therapies to promote awareness, acceptance and distress tolerance( Reference Godfrey, Gallo and Afari 19 ).
The aim of this paper is to present the results of a structured literature review looking at the outcomes of mindfulness, including mindful eating and intuitive eating, in changing eating behaviours (including binge eating, emotional eating and eating in response to cues) in healthy populations of any age and weight status. As this is an emerging area of science, the review includes both observational and intervention studies to provide an indication of the direction of future research. The review provides details of the tools used to measure outcomes and the interventions themselves including their theoretical basis. The review also includes a brief summary of potential associated mechanisms that may explain the observed results.
Methodology
The structured review was carried out combining the following search terms and within the three parameters: population, intervention and outcomes. Search terms were combined with ‘or’ within parameters, and combined with ‘and’ across parameters. Only peer-reviewed interventions and observational studies were included.
Population
Search terms were: healthy population or adult or child or obese or overweight or binge eating or problematic eating or disordered eating or diabetes or diabetic.
Intervention
Search terms were: mindful eating or mindfulness or mindfulness based intervention or meditation or mindfulness based cognitive behaviour therapy or mindfulness based stress reduction or acceptance based practices or mindful body scan or intuitive eating.
These search terms were also searched in combination with cognitive behaviour/behavior therapy or acceptance and commitment therapy or weight intervention or weight program.
Outcomes
Search terms were: weight or weight related eating behaviour/behavior or overeating or eating behaviour/behavior or eating pattern or dietary behaviour/behavior or dietary pattern or snacking behaviour/behavior or diet quality or energy intake or energy balance or meal frequency or external eating or self-regulation or intuitive eating or mindless eating or mindful eating or distracted eating or appetite awareness or hunger recognition or emotional eating or self-efficacy for eating behaviour/behavior or self-efficacy for healthy eating or self-confidence or wellness or well-being or quality of life.
Databases
The search was conducted using a University search engine which searched multiple databases: AMED (Alternative MEDicine), ASSIA (Applied Social Sciences Index), BioMed central, BMJ open, British Nursing Index, CINAHL (Nursing and Allied Health), Clinical Evidence, Cochrane Library, Conference Proceedings Citations Index, Ebsco, Medline, NICE, PsycARTICLES, PsycINFO, PubMed, Sage Journals Online and Science Direct.
Inclusion criteria
Included were papers consistent with the search strategy outlined above in the databases listed, and English articles published until August 2015.
Exclusion criterion
Excluded were non-English-language papers.
Coding and scoring of results
For both the intervention and observational studies, results were ‘coded’ and summarised as follows. A ‘positive’ code indicated the outcome demonstrated a beneficial effect of mindfulness (for example, decreased binge eating, weight loss, and reduced energy intake). A ‘neutral’ code indicated that there was no significant effect from the intervention. A mixed code indicated that there were some positive and neutral results. ‘Negative’ codes indicated that the measured outcome was in an opposite direction to the hypothesis.
Outcomes that were measured in three or more studies were ascribed a percentage score calculated by giving all positive codes one point, negative results were given minus one point, and neutral or mixed codes were given no score. The points were added per outcome, divided by the total number of outcomes and expressed as a percentage.
We acknowledge that this is not a conventional way of summarising the results of the studies and does not account for effect size. However, it provides an overview of findings in the wide range of papers included in the review, and gives an indication of whether or not there is consistency in the literature.
Search strategy results
The results of the structured literature review are shown in Fig. 1 and resulted in sixty-eight papers.
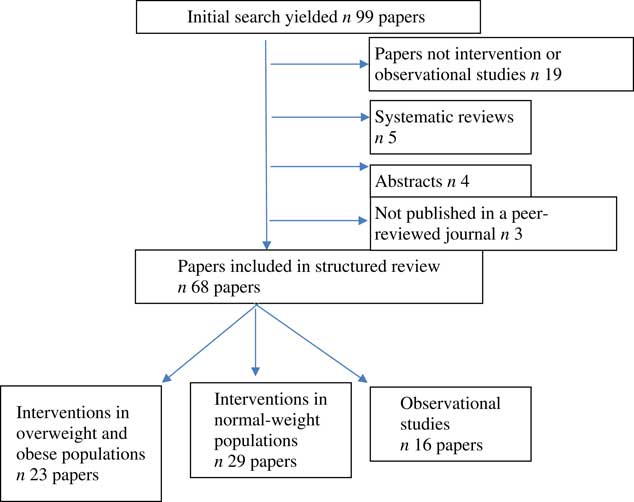
Fig. 1 Literature search results.
Results – intervention studies
The search yielded twenty-three studies (twenty-four papers) in overweight/obese subjects( Reference Kristeller and Hallett 11 , Reference Dalen, Smith and Shelley 13 , Reference Miller, Kristeller and Headings 14 , Reference Kristeller, Wolever and Sheets 16 , Reference Alberts, Mulkens and Smeets 24 – Reference Timmerman and Brown 43 ) and twenty-nine papers describing interventions in normal-weight subjects( Reference Hendrickson and Rasmussen 15 , Reference Anderson, Schaumberg and Anderson 18 , Reference Mantzios and Wilson 34 , Reference Cavanagh, Vartanian and Herman 44 – Reference Woolhouse, Knowles and Crafti 61 ).
Characteristics of the intervention studies
The majority of interventions have taken place in the last 5 years. Most of the interventions in obese/overweight populations were undertaken in female populations, while studies of normal-weight populations included more men. Many of the interventions had small sample sizes of fifty or fewer subjects: fourteen of the overweight/obese studies( Reference Kristeller and Hallett 11 , Reference Dalen, Smith and Shelley 13 , Reference Alberts, Mulkens and Smeets 24 , Reference Alberts, Thewissen and Raes 25 , Reference Baer, Fischer and Huss 27 – Reference Boutelle, Zucker and Peterson 29 , Reference Daubenmier, Kristeller and Hecht 31 – Reference Leahey, Crowther and Irwin 33 , Reference Niemeier, Leahey and Palm Reed 37 , Reference Stites, Singletary and Menasha 41 , Reference Timmerman and Brown 43 ), and ten of the studies in normal-weight populations( Reference Courbasson, Nishikawa and Shapira 45 , Reference Healy, Joram and Matvienko 47 – Reference Hill, Masuda and Melcher 49 , Reference Jacobs, Cardaciotto and Block-Lerner 51 , Reference Kearney, Milton and Malte 54 , Reference May, Andrade and Batey 58 – Reference Woolhouse, Knowles and Crafti 61 ). Three of the studies in the overweight/obese populations were carried out among children( Reference Boutelle, Zucker and Peterson 28 , Reference Boutelle, Zucker and Peterson 29 , Reference Soleimaninanadegani and Shahmohammadi 40 ); one of these studies had a sample size of more than 300 but the results of this study were not clearly described( Reference Soleimaninanadegani and Shahmohammadi 40 ). The majority of the studies( Reference Hendrickson and Rasmussen 15 ) among normal-weight populations were performed with students( Reference Hendrickson and Rasmussen 15 , Reference Anderson, Schaumberg and Anderson 18 , Reference Mantzios and Wilson 34 , Reference Hamilton, Fawson and May 46 – Reference Higgs and Donohoe 48 , Reference Hong, Lishner and Han 50 – Reference Jordan, Wanga and Donatoni 53 ).
Theoretical basis of the interventions in overweight and obese subjects
Mindfulness-based cognitive therapy/mindfulness action-based cognitive therapy, and mindful eating were the most commonly used approaches and were both used in four studies. Table 1 outlines the details of the theoretical basis of these studies.
Table 1 Theoretical basis of interventions in overweight and obese subjects (n 23)

MBCT, mindfulness-based cognitive therapy; MBSR, Mindfulness-Based Stress Reduction; MB-EAT, Mindfulness-Based Eating Awareness Training.
Theoretical basis of the interventions in normal-weight populations
Mindfulness was the most frequently cited basis in the studies among normal-weight subjects and was reported in eight papers which contained thirteen studies( Reference Mantzios and Wilson 34 , Reference Hamilton, Fawson and May 46 , Reference Jacobs, Cardaciotto and Block-Lerner 51 , Reference Jordan, Wanga and Donatoni 53 , Reference Lacaille, Ly and Zacchia 56 – Reference Papies, Barsalou and Custers 59 ). Three papers used mindful eating( Reference Hendrickson and Rasmussen 15 , Reference Higgs and Donohoe 48 , Reference Hong, Lishner and Han 50 ) and two intuitive eating( Reference Anderson, Schaumberg and Anderson 18 , Reference Healy, Joram and Matvienko 47 ). One paper which contained three studies used emotional awareness( Reference Kidwell, Hasford and Hardesty 55 ). Cognitive defusion( Reference Jenkins and Tapper 52 ) and ACT were each used in one paper( Reference Hill, Masuda and Melcher 49 ).
Intervention length, intensity and scope
The majority of interventions (n 18) in the overweight/obese populations consisted of sustained weight-management programmes of medium to high intensity carried out for a medium length of time, i.e. 6 weeks to 4 months. Two studies lasted longer than 4 months and two were for a shorter duration with one study not detailing its intervention length. In many of these studies mindfulness was the sole focus of the intervention which often included mindful eating as a key element of the programme. An example of a mindfulness intervention is the one developed by Alberts et al. in 2012, a programme with five core components( Reference Alberts, Thewissen and Raes 25 ):
-
(1) Mindful eating;
-
(2) Awareness of physical sensations;
-
(3) Awareness of thoughts and feelings related to eating;
-
(4) Acceptance and non-judgement of sensations, thoughts, feelings, and body;
-
(5) Awareness and step-by-step change of daily patterns and eating habits.
In contrast, many of the interventions in normal-weight populations were single-day laboratory-based studies such as completion of food tasks, rating of pleasure in food or observed food intake after a test meal. Studies often looked only at a specific practice of mindfulness such as the body scan, or mindful eating of a raisin and were therefore lower-intensity interventions than those in obese/overweight individuals.
Summary of the tools/methods used to measure outcomes in intervention studies
The following two tools were the most frequently used to measure individuals’ mindfulness state and awareness:
-
(1) The Five Facet Mindfulness Questionnaire contained thirty-nine items( Reference Baer, Fischer and Huss 27 ) It: (a) measures trait (rather than state) mindfulness across five subscales (observing, describing, acting with awareness, non-judging of inner experience and non-reactivity to inner experience); and (b) reports internal consistency of 0·87 (as measured by Cronbach’s α).
-
(2) The Mindfulness Awareness Attention Scale contained fifteen items( Reference Brown and Ryan 62 ). It: (a) measures trait or dispositional levels of mindfulness; (b) measures each item on a six-point Likert scale and measures levels of day-to-day awareness, attention and observation; (c) reports reliability of 0·82 (as measured by Cronbach’s α).
The Mindful Eating Questionnaire contained twenty-eight items( Reference Framson, Kristal and Schenk 63 ) and was the only tool used to measure mindful eating. It: (a) assesses five domains of mindful eating (disinhibition, awareness, external cues, emotional response and distraction) on a four-point Likert scale; and (b) reports reliability of 0·7–0·9 (as measured by Cronbach’s α).
Intuitive eating, when measured, was evaluated using the Intuitive Eating Scale( Reference Tylka and Kroon Van Diest 64 ) which contains twenty-one items. It: (a) assesses each item on a five-point Likert scale; (b) measures readiness to eat in response to internal cues to determine choice and quantity of food; eating to satisfy physical rather than emotional reasons; awareness and trust of internal cues; and (c) reports internal consistency of >0·70 (as measured by Cronbach’s α) and test–retest reliability of 0·90 (as measured by Cronbach’s α).
Tools used to measure eating-related behaviours
Eating behaviours were most frequently assessed using the Dutch Eating Behaviour Questionnaire( Reference Van Strien, Frijters and Bergers 65 ), the Eating Attitudes Test( Reference Garner, Olmsted and Bohr 66 ) and the Eating Disorders Examination Questionnaire( Reference Black and Wilson 67 ).
The studies reviewed used thirty-two measures of eating behaviour assessing a broad range of eating behaviours, attitudes, cognitions about food and related issues. Some of these were previously validated tools, others adapted, and others developed specifically for a study.
Tools used to measure issues related to food consumption and hunger
The majority of self-report measures involved 24 h recalls which were translated into energy intakes by the investigator. The studies applying objective measures involved the investigator weighing the amount of food consumed, usually within a controlled laboratory environment. The assessment of hunger was always via self-report rating scale, either on an analogue or Likert scale. There were eleven measures of the quantity of food consumed via self-report and objectively weighed.
Summary of results from intervention studies
The results of the intervention studies are presented with results in overweight/obese populations being detailed before those in normal-weight populations. Most intervention effect was seen in binge eating, emotional eating and external eating and more emphasis is given to these interventions, alongside the weight-management interventions in overweight/obese populations. Overall, the studies in overweight/obese populations were relatively longer and more intense compared with those carried out in normal-weight populations. Many of the observational studies were short, day-long laboratory experiments, and these are briefly summarised after the intervention studies.
A summary of the results from the intervention studies is presented in Table 2. In five of the papers in normal-weight populations, multiple related studies were reported in a single paper and the results have been collated in Table 2( Reference Mantzios and Wilson 34 , Reference Jordan, Wanga and Donatoni 53 , Reference Kidwell, Hasford and Hardesty 55 , Reference May, Andrade and Batey 58 , Reference Papies, Barsalou and Custers 59 ).
Table 2 Summary of coded results from intervention studies using mindfulness, mindful eating and intuitive eating techniques

* Note that effect size is not accounted for in the coding of positive, negative and neutral and the code only provides an indicator of the direction of results; it is not trying to assess overall evidence. The ‘score’ in the final column is merely a convenient summary tool in situations where there have been three or more studies.
† Calculation of score. Only health outcomes with three or more studies are ‘scored’: a positive study scores +1 point; a negative study scores –1 point; a neutral study scores 0 points; a study with mixed results scores 0 points. The points are summed, divided by the number of studies and expressed as a percentage. An example for effect of mindful eating on weight in overweight/obese: 8 × 1=8/16=0·5, giving a score=50 %.
‡ Cholesterol and blood pressure.
Ten outcomes were given a percentage score as described previously. In studies that measured weight, binge eating, emotional eating, food intake (in overweight and obese populations) and food choice (in normal-weight populations) the score was 50 % or above, indicating that most of the results were positive or neutral/mixed. Only two studies had negative results related to weight gain( Reference Kearney, Milton and Malte 54 ) and an increase of energy intake( Reference Anderson, Schaumberg and Anderson 18 ).
Results of physiological health outcomes
Outcomes of weight management interventions
Weight loss was seen in eight( Reference Dalen, Smith and Shelley 13 , Reference Kristeller, Wolever and Sheets 16 , Reference Boutelle, Zucker and Peterson 28 , Reference Corsica, Hood and Katterman 30 , Reference Daubenmier, Kristeller and Hecht 31 , Reference Niemeier, Leahey and Palm Reed 37 , Reference Soleimaninanadegani and Shahmohammadi 40 , Reference Timmerman and Brown 43 ) of the sixteen studies in overweight/obese population studies. However, the effect sizes varied widely with only three studies reporting significant weight loss( Reference Dalen, Smith and Shelley 13 , Reference Kristeller, Wolever and Sheets 16 , Reference Niemeier, Leahey and Palm Reed 37 ); the latter of these reported a mean weight loss of 12 (se 4) kg over 6 months. In two studies the weight loss was minimal( Reference Boutelle, Zucker and Peterson 28 , Reference Corsica, Hood and Katterman 30 ), and in two studies weight was stabilised or weight gain was less in the intervention group( Reference Daubenmier, Kristeller and Hecht 31 , Reference Timmerman and Brown 43 ). In one study results were not reported( Reference Soleimaninanadegani and Shahmohammadi 40 ).
The duration of the eight studies in overweight/obese populations that resulted in weight loss varied from 6 to 24 weeks and sample sizes varied from ten( Reference Dalen, Smith and Shelley 13 ) to 300( Reference Soleimaninanadegani and Shahmohammadi 40 ).
Weight-loss interventions
Of the eight studies that reported weight loss in overweight/obese populations, five of them were comprehensive mindfulness programmes( Reference Dalen, Smith and Shelley 13 , Reference Kristeller, Wolever and Sheets 16 , Reference Corsica, Hood and Katterman 30 , Reference Daubenmier, Kristeller and Hecht 31 , Reference Soleimaninanadegani and Shahmohammadi 40 ) where mindful eating was a component of the programme, although details of the intervention were not reported in one of these studies( Reference Soleimaninanadegani and Shahmohammadi 40 ). The rest of these programmes taught the core elements of mindfulness such as being present in the moment and self-acceptance of the current state. The study with the greatest weight loss held group sessions for 24 weeks based on an acceptance-based behavioural intervention for weight loss; this was a pilot study, which taught key components of this approach including values, acceptance and cognitive defusion using mindfulness( Reference Niemeier, Leahey and Palm Reed 37 ).
Mindful eating in a restaurant setting was the sole focus of one of the eight studies( Reference Timmerman and Brown 43 ); the other two studies focused on the regulation of cues( Reference Boutelle, Zucker and Peterson 28 ) and used an ACT approach where mindfulness was a core component( Reference Niemeier, Leahey and Palm Reed 37 ).
There was some variation between interventions but the following were key elements of the mindful eating components:
-
(1) Mindful eating was taught by a specific exercise such as the ‘mindful raisin’ exercise;
-
(2) Mindfully attending to the eating experience by noticing smell, texture and taste of the food;
-
(3) Reducing the speed of eating;
-
(4) Guided meditations that focused on awareness of hunger and satiety;
-
(5) Mediations to identify eating triggers including emotional triggers;
-
(6) Mediations to manage cravings.
An example of how these elements were delivered in a mindfulness intervention is given in Table 3 from a nine-session MB-EAT programme for binge eating( Reference Kristeller, Wolever and Sheets 16 ).
Table 3 Example of how elements were delivered in a mindfulness intervention from a nine-session Mindfulness-Based Eating Awareness Training (MB-EAT) programme for binge eating( Reference Kristeller, Wolever and Sheets 16 )

The studies that did not report weight loss or where there was no intervention effect on weight were more variable in terms of duration and intensity than the studies above. A couple of the studies had a mindfulness component as part of an education programme, with an ACT( Reference Tapper, Shaw and Ilsley 42 ) and MB-EAT( Reference Miller, Kristeller and Headings 36 ) basis and were similar to the studies where weight loss was observed. Other studies had a narrower focus, for example internal cues( Reference Bacon, Stern and Van Loan 26 ), mindful eating( Reference Boutelle, Zucker and Peterson 29 ) and mindful breathing( Reference Stites, Singletary and Menasha 41 ), and tended to have shorter duration of 4–8 weeks.
Weight loss in normal-weight populations
In two of the three normal population studies that measured weight( Reference Mantzios and Wilson 34 , Reference Kidwell, Hasford and Hardesty 55 ), weight loss was observed although effect sizes were small; these were short-term experimental studies. In one study undertaken among veterans with chronic conditions, weight increased( Reference Kearney, Milton and Malte 54 ).
Other objective physiological measures
Three studies measured other objective physiological measures – with both improvement and mixed results reported for cardiovascular risk factors in overweight/obese populations( Reference Dalen, Smith and Shelley 13 , Reference Bacon, Stern and Van Loan 26 ), and improvement in glycaemic control in diabetics( Reference Miller, Kristeller and Headings 14 , Reference Miller, Kristeller and Headings 36 ). This suggests that mindfulness interventions can create changes in physiological markers, most likely because of mindfulness-induced changes to eating habits rather than mindfulness per se having a direct effect on the physiological marker. This is an area of limited research.
Eating behaviours and food-related outcomes
A range of eating behaviours that may be associated with weight status was measured across the intervention studies including binge eating, emotional eating, external eating and cravings. Food intake and choices were also measured in some studies. A number of the studies showed that mindfulness enabled participants to become more aware of their internal states of hunger and satiety alongside the recognition of specific cues. Other studies showed that mindfulness generated more overall internal awareness, for example thoughts and feelings (which could include satiety and hunger). More generic mindfulness techniques emerged strongly in the studies. These included the body scan exercise and mindful breathing exercises. Acceptance-based exercises were used in a number of studies connected to recognition of emotions and thoughts.
Eating-related behaviours
Binge eating
Binge eating symptoms were measured in nine studies in overweight/obese populations. All the studies reported positive changes in binge eating symptoms over the course of the study, as evidenced by self-report measures. In four of the studies binge eating was a specific target of the intervention( Reference Kristeller and Hallett 11 , Reference Kristeller, Wolever and Sheets 16 , Reference Leahey, Crowther and Irwin 33 , Reference Smith, Shelley and Leahigh 39 ). The first of these studies was the initial exploratory work with mindfulness and any eating-related behaviour( Reference Kristeller and Hallett 11 ).
Binge eating symptoms were assessed in four studies in normal-weight populations( Reference Courbasson, Nishikawa and Shapira 45 , Reference Hill, Masuda and Melcher 49 , Reference Smith, Shelley and Dalen 60 , Reference Woolhouse, Knowles and Crafti 61 ); three were undertaken in binge-eating-disorder populations. Positive results were seen in all studies.
Collectively, these results suggest strong evidence for the efficacy of mindfulness in reducing the frequency and intensity of binge eating symptoms. This is particularly notable given the high degree of heterogeneity between the studies in terms of design and intervention.
Binge eating interventions
Specific mindful eating strategies were included in the majority of studies that measured binge eating. In many cases, this was complemented with generic mindfulness meditations such as breathing techniques and body scans often as part of a mindfulness-based curriculum, for example, MB-EAT( Reference Kristeller, Wolever and Sheets 16 ), MBSR( Reference Smith, Shelley and Leahigh 39 , Reference Smith, Shelley and Dalen 60 ) or mindfulness-based cognitive therapy( Reference Baer, Fischer and Huss 27 , Reference Leahey, Crowther and Irwin 33 ). Mindfulness was also sometimes combined with ACT( Reference Tapper, Shaw and Ilsley 42 , Reference Hill, Masuda and Melcher 49 ) or action-based cognitive therapy( Reference Courbasson, Nishikawa and Shapira 45 ). Awareness of internal hunger cues was not as prevalent in these studies. These findings suggest that in the management of binge eating, the ability to eat mindfully is a key technique.
Emotional eating
Ten studies measured emotional eating in overweight/obese populations. Reductions in emotional eating were reported in seven of these studies( Reference Kristeller and Hallett 11 , Reference Alberts, Thewissen and Raes 25 , Reference Corsica, Hood and Katterman 30 , Reference Daubenmier, Kristeller and Hecht 31 , Reference Leahey, Crowther and Irwin 33 , Reference Mason, Lustig and Brown 35 , Reference Smith, Shelley and Leahigh 39 ) and three studies showed no change( Reference Boutelle, Zucker and Peterson 29 , Reference Tapper, Shaw and Ilsley 42 , Reference Timmerman and Brown 43 ). One of the studies where there was no effect was undertaken among children( Reference Boutelle, Zucker and Peterson 29 ), another was focused on restaurant eating only( Reference Timmerman and Brown 43 ), and the third was an ACT-based intervention where mindfulness was not the sole focus( Reference Tapper, Shaw and Ilsley 42 ). These positive results provide support for the use of mindfulness-based interventions in reducing emotional eating in overweight or obese populations.
Only one study measured emotional eating in a normal-weight population( Reference Kearney, Milton and Malte 54 ) where no impact of the MBSR intervention was seen; this population of veterans with chronic conditions may not be generalisable.
External eating
External eating was measured in five of the studies within an overweight/obese population. Four of these studies showed a positive change in external eating and were undertaken in populations suffering from stress eating, problematic eating, disordered eating attitudes, and children learning specifically about cues( Reference Alberts, Thewissen and Raes 25 , Reference Boutelle, Zucker and Peterson 28 , Reference Daubenmier, Kristeller and Hecht 31 , Reference Pearson, Follette and Hayes 38 ). One study, in this population reported a neutral result( Reference Tapper, Shaw and Ilsley 42 ). This was an ACT intervention study over 6 months among women. External eating was measured in one study in a normal-weight population suffering from binge eating and the intervention reduced binge eating episodes.
Taken together, these findings suggest that mindfulness can be helpful in reducing external eating and reduce the responsiveness of individuals to external cues such as food packaging and time of day. The evidence in normal-weight populations appears to be limited.
External eating and emotional eating interventions
All studies that looked at external and emotional eating used specific mindful eating techniques in their interventions. Mindfulness techniques such as body scans, breathing exercises and awareness of bodily sensation were utilised in the studies to a varying extent. In the studies done in overweight and obese populations the mindful practice was part of a wider curriculum( Reference Kristeller and Hallett 11 , Reference Alberts, Thewissen and Raes 25 , Reference Corsica, Hood and Katterman 30 , Reference Daubenmier, Kristeller and Hecht 31 ), or sometimes supported by a one-day workshop( Reference Pearson, Follette and Hayes 38 ). This suggests that in order to effect change in external and emotional eating, it is important to use techniques that increase awareness of internal states, combined with acceptance techniques. Combining these with mindful eating seems to be important.
Cravings
Cravings were measured in one study in an overweight/obese population( Reference Alberts, Mulkens and Smeets 24 ), which showed a positive response to a mindfulness-based intervention, and in three studies in normal-weight populations, all of which showed mixed/neutral results( Reference Hamilton, Fawson and May 46 , Reference Lacaille, Ly and Zacchia 56 , Reference May, Andrade and Batey 58 ). These studies were all laboratory-based studies and two of them were day-long studies only. Given the limited number of studies and their short duration, the role of mindfulness in reducing cravings remains to be fully elucidated.
Hunger awareness
Hunger awareness was measured in two overweight/obese populations and positive results were reported in both studies( Reference Kristeller and Hallett 11 , Reference Boutelle, Zucker and Peterson 28 ). In one of these studies a 12-week curriculum was developed which focused on ‘Regulation of Cues’; children in this group had significant reductions in eating in response to external cues and negative states, and attending to food responsiveness( Reference Boutelle, Zucker and Peterson 28 ). A study in normal-weight students which made one focus group concentrate on the sensory experience of foods showed a lower pre-snack hunger rating than either of the control groups( Reference Higgs and Donohoe 48 ). These results suggest that mindfulness is effective in increasing hunger awareness, although this was only measured in three studies, so the finding should be considered preliminary.
Body dissatisfaction
Two studies measured body dissatisfaction in relation to mindfulness interventions in overweight/obese populations( Reference Pearson, Follette and Hayes 38 , Reference Smith, Shelley and Leahigh 39 ). Both of these studies demonstrated positive results, but this is a limited evidence base from which to suggest that mindfulness can support improvements in body dissatisfaction.
Food intake and choice
Food intake was measured in four studies in overweight/obese populations and three of these reported a reduced energy intake, as measured by self-report via 24 h recalls or FFQ( Reference Boutelle, Zucker and Peterson 28 , Reference Miller, Kristeller and Headings 36 , Reference Timmerman and Brown 43 ). The first two of these studies were comprehensive education programmes while the third focused on intake at lunchtime only. One study did not find a reduction in energy intake as a result of their intervention among children and their parents( Reference Boutelle, Zucker and Peterson 29 ).
Food intake was measured in nine studies in normal-weight populations, with four studies reporting a reduction of food intake( Reference Higgs and Donohoe 48 , Reference Jenkins and Tapper 52 , Reference Jordan, Wanga and Donatoni 53 , Reference Kidwell, Hasford and Hardesty 55 ), four reporting neutral results( Reference Cavanagh, Vartanian and Herman 44 , Reference Jacobs, Cardaciotto and Block-Lerner 51 , Reference Kearney, Milton and Malte 54 , Reference Marchiori and Papies 57 ) and one reporting negative results( Reference Anderson, Schaumberg and Anderson 18 ). One of these studies reported that higher levels of intuitive eating was associated with increased food intake in a permissive environment which was an unexpected finding( Reference Anderson, Schaumberg and Anderson 18 ). No change in food intake was seen in a study among veterans with chronic health problems( Reference Kearney, Milton and Malte 54 ). In contrast to the studies in overweight/obese populations, in all but one study( Reference Kearney, Milton and Malte 54 ), food intake was measured in short-duration, low-intensity experiments in laboratory settings using test meals or snacks rather than in a free-living situation.
These results suggest that more evidence is needed before it is possible to say if mindfulness and/or mindful eating can reduce the quantity of food consumed.
Food choice was measured in one study in overweight/obese populations which looked at lunches purchased and showed positive trend in choosing healthier meals( Reference Stites, Singletary and Menasha 41 ). Food was measured in five studies in normal-weight populations. Three of these studies reported positive food choices( Reference Hendrickson and Rasmussen 15 , Reference Jordan, Wanga and Donatoni 53 , Reference Kidwell, Hasford and Hardesty 55 ) as a result of mindfulness intervention and two studies reported mixed/neutral results( Reference Hong, Lishner and Han 50 , Reference Papies, Barsalou and Custers 59 ). As per food intake, these were low-intensity, laboratory studies asking participants to make a snack choice, with the healthier choice being determined as positive.
Results – observational studies
Theoretical basis
Eight papers focused on intuitive eating( Reference Anderson, Schaumberg and Anderson 18 , Reference Denny, Loth and Eisenberg 68 – Reference Smith and Hawks 75 ), five papers focused on mindfulness( Reference Levin, Dalrymple and Himes 76 – Reference Roberts and Danoff-Burg 80 ), two papers focused on mindful eating( Reference Khan and Zadeh 81 , Reference Moor, Scott and McIntosh 82 ) and one paper had a combined mindfulness and mindful eating approach( Reference Beshara, Hutchinson and Wilson 83 ).
Summary of results from observational studies
Sixteen observational studies were identified in the literature search and a summary of the associations observed are shown in the Table 4; it should be noted that some studies investigated more than one association. Many of the observational studies looked at associations between an aspect of eating or mindfulness and related it to an outcome in an existing cohort, for example level of mindfulness, or intuitive eating and BMI. Associations were made using the tools and scales already outlined in the intervention studies.
Table 4 Summary of coded results from observational studies showing the association between mindfulness, mindful eating and intuitive eating and parameters related to health measures and eating behaviours

* Note that effect size is not accounted for in the coding of positive. The code only provides an indicator of direction of results and is not trying to assess overall evidence.
Two of the cohorts were substantial, with 1000( Reference Moy, Petrie and Dockendorff 72 ) and 2000( Reference Gast, Madanat and Nielson 69 ) subjects, respectively. The cohort populations were diverse, with six undertaken among university students( Reference Gast, Madanat and Nielson 69 – Reference Herbert, Blechert and Hautzinger 71 , Reference Outland, Madanat and Rust 73 , Reference Roberts and Danoff-Burg 80 , Reference Moor, Scott and McIntosh 82 ) and two taken among other young adult populations( Reference Denny, Loth and Eisenberg 68 , Reference Herbert, Blechert and Hautzinger 71 ). The remaining cohorts were spread across a wide age spectrum from middle school( Reference Moy, Petrie and Dockendorff 72 ) to older obese adults( Reference Paolini, Burdette and Laurienti 78 ). Four of the cohorts were from overweight/obese populations of which two were waiting for bariatric surgery( Reference Levin, Dalrymple and Himes 76 , Reference Ouwens, Schiffer and Visser 77 ).
Intuitive eating was associated with a lower BMI in four studies( Reference Denny, Loth and Eisenberg 68 , Reference Hawks, Madanat and Hawks 70 , Reference Sairanen, Tolvanen and Karhunen 74 , Reference Smith and Hawks 75 ). Other observations included a decreased emotional eating with higher levels of mindfulness( Reference Levin, Dalrymple and Himes 76 , Reference Ouwens, Schiffer and Visser 77 , Reference Pidgeon, Lacota and Champion 79 ) and a higher level of everyday mindfulness was related negatively to self-report serve size of energy-dense food( Reference Beshara, Hutchinson and Wilson 83 ). In one of the large cohorts in young adults, there was no difference in intuitive eating by age or sex( Reference Denny, Loth and Eisenberg 68 ) while another study which compared males and females in a young adult population found higher levels of anti-dieting and self-care subscales of the intuitive eating scale( Reference Gast, Madanat and Nielson 69 ). One study found males trusting their bodies more than females on when to eat( Reference Denny, Loth and Eisenberg 68 ) but this was reversed in a second study( Reference Moy, Petrie and Dockendorff 72 ). Another study looking at associations with intuitive eating showed that those who consistently overrode fullness feelings were more likely to use moderate to extreme effort to maintain their weight( Reference Outland, Madanat and Rust 73 ).
Interoceptive sensitivity is a measure of awareness of the subject’s bodily state; this was positively related to higher levels of intuitive eating( Reference Herbert, Blechert and Hautzinger 71 ). An online survey in Pakistan showed a significantly positive relationship between overall mindful eating and mental well-being( Reference Khan and Zadeh 81 ). In one of the group of bariatric patients, greater mindfulness, particularly awareness, was related to fewer binges and emotional eating( Reference Levin, Dalrymple and Himes 76 ). Another observation in bariatric patients showed that mindfulness was positively associated with restrained eating behaviour( Reference Ouwens, Schiffer and Visser 77 ).
These studies indicate that both mindfulness and intuitive eating showed promise in positively influencing complex relationships with food and eating behaviours.
Potential associated mechanisms
The literature search showed a growing evidence base for mindfulness, mindful eating and intuitive eating, but the papers retrieved generally did not discuss underlying mechanisms. Therefore, a further search of the scientific literature was undertaken to provide potential explanations for the observed effects. We identified three separate hypothesised mechanisms that were suggested by functional MRI (fMRI) results; fMRI measures brain activity by detecting associated changes in blood flow.
Increased awareness of, and increased responsiveness to, internal physical cues
Interoception can be measured by an individual’s ability to report their heart rate. Interoception is connected with the mindful awareness of an individual’s internal state, especially in relation to physical factors such as hunger and satiety. Increased awareness enables individuals to eat in response to these physical cues of hunger and satiety.
Mindful eating has been shown to slow down consumption of a meal and allows both registration of feelings of fullness and greater control over eating( Reference Gerweck and Celentano 84 , Reference Lofgren 85 ). Additionally, a slower pace of eating reduces overall energy consumption as individuals feel full on a smaller quantity of food( Reference Monroe 86 ).
One study using fMRI showed a decrease in mid-line cortical structures associated with interoception during a mindfulness body scan. This suggests an increased awareness of internal state( Reference Ives-Deliperi, Solms and Meintjes 87 ). In another study, fMRI results showed reduced activation in the insula( Reference Farb, Anderson and Mayberg 88 ) which is the part of the cerebral cortex implicated in self-awareness and perception and hence is linked with interoceptive awareness.
Increased awareness of, and reduced responsiveness to, internal emotional cues
Mindfulness trains individuals to notice distressing thoughts, emotions and sensations. By increasing awareness of these cues, individuals are then able to tolerate their distress and not allow these non-physical cues make them eat more( Reference Ouwens, Schiffer and Visser 77 ).
By learning to bring the experience fully into awareness many types of distress that would have provoked an automatic reaction can be tolerated. Thus, distress tolerance is increased and automaticity reduced. In relation to emotional eating, mindfulness reduces misperception of emotions as hunger and therefore stops increased eating in response to non-physical cues( Reference Ouwens, Schiffer and Visser 77 ).
As defusion-reduced reactivity enhances tolerance to non-physical emotional cues, the cultivation of mindfulness becomes self-reinforcing( Reference Caldwell, Baime and Wolever 89 ). Further, mindfulness increases the capability to relax when faced with negative events and emotion. This has been found to be especially true in reducing impulsivity, which is associated with mindless overeating( Reference Ouwens, Schiffer and Visser 77 ).
fMRI studies have shown altered activity levels in the amygdala related to general emotional arousal/salience following mindfulness training. Decreased activation has been found in the amygdala, the parahippocampal area and the insula during perception of negative stimuli in subjects but these activity levels have been regulated following mindfulness training( Reference Lutz, Herwig and Opialla 90 ). Others have used fMRI to show that mindfulness makes an impact on the neural systems underlying emotional regulation. It appears to regulate amygdala functioning via functional connectivity from the medial prefrontal cortex( Reference Murakami, Katsunuma and Oba 91 ).
fMRI studies conducted on individuals practising mindfulness have found a significant reduction in activity in the anterior cingulated cortex region which plays a role in the processing of emotion. ‘Findings collectively show that mindfulness meditation has an overall “quietening” effect on brain regions associated with subjective and cognitive appraisal of emotions’( Reference Ives-Deliperi, Solms and Meintjes 87 ). Significant self-reported differences in awareness of emotion are unlikely to be simply due to a blunting of the emotional experience but ‘represent more fundamental change in regulatory response’( Reference Farb, Anderson and Mayberg 88 ).
Anatomical studies lend further support to changes in the areas of the brain associated with emotional regulation. Studies conducted pre- and post-MRI on participants following an 8-week mindfulness programme found an increase in grey matter concentration in the left hippocampus and posterior cingulated cortex, temporo-parietal junction, and cerebellum – areas associated with learning and memory processes, emotional regulation and self-referential processing( Reference Hölzel, Carmody and Vangel 92 ).
Increased awareness of, and reduced responsiveness to, external cues
Overeating may reflect a non-mindful reliance on environmental or external cues (for example, packaging size), so that the cues destroy the subject’s ability to self-monitor the food they eat( Reference Beshara, Hutchinson and Wilson 83 ). The use of mindfulness is designed to interrupt these automatic, non-conscious external influences( Reference Forman and Butryn 93 ). Increasing awareness of an individual’s reactions to attractive food items, and a recognition of these reactions as passing mental states rather than real experiences, reduced the likelihood of individuals initiating purchasing and eating behaviours( Reference Papies, Barsalou and Custers 59 ). Mindfulness practice( Reference Beshara, Hutchinson and Wilson 83 ) and mindful eating specifically reduced the impact of the external norms around consumption and enabled individuals to reduce their food intake( Reference Mantzios and Wilson 34 , Reference Wansink 94 ).
fMRI has been used to compare results of subjects who received an 8-week mindfulness-based stress reduction course with those of a control group( Reference Kilpatrick, Suyenobu and Smith 95 ). When asked to pay attention to the external sounds in the scanner environment, the mindfulness group showed increased functional connectivity in auditory and visual networks and the areas associated with attentional and self-referential processes.
These observations from fMRI studies are of interest but are insufficient on their own to explain the mechanism by which mindfulness exerts its effects. More research is needed to fully elucidate further mechanisms and these must explain other influencing behavioural factors.
Discussion
From the papers reviewed there appears to be reasonable evidence that mindfulness, including mindful eating techniques, can help to change eating behaviours. The evidence for the effectiveness of mindfulness and mindful eating in binge eating disorders appears to be the strongest with consistently positive results in both overweight/obese populations and those of normal-weight status. There was also a positive effect on emotional eating as a result of mindfulness interventions and in a lesser number of studies a positive result was seen for reducing eating in response to external cues. This is consistent with the findings of O’Reilly et al. in 2014( Reference O’Reilly, Cook and Spruijt-Metz 23 ), who examined the role of mindfulness with obesity-related behaviours and a review looking at the effectiveness of mindfulness in binge eating( Reference Godfrey, Gallo and Afari 19 , Reference O’Reilly, Cook and Spruijt-Metz 23 ).
Food cravings, eating attitudes and body dissatisfaction were explored in only a limited number of studies. Although binge eating and emotional eating are important obesity-related behaviours, the results for the use of mindfulness in achieving weight loss in overweight/obese individuals were mixed and generally effect sizes were small. This is not surprising given the complex and multifaceted nature of obesity, which requires a multi-pronged treatment approach. The diversity of the interventions makes it difficult to identify the effective elements. With regard to the interventions that did not report weight loss there were no striking differences from the ones that were successful, except that a couple of the studies were of lower intensity and shorter duration. This diverse range of treatments included mindfulness as part of a third-wave therapy such as ACT, mindfulness curricula based on established programmes in other conditions adapted for eating, for example MBSR and mindfulness-based cognitive therapy, through to less intense interventions which employed mindfulness techniques as stand-alone interventions. However, the majority of successful interventions included mindful eating as part of a comprehensive mindfulness programme. These mindfulness programmes contained core elements of mindfulness including meditation, awareness and being present. A recent review on the effectiveness of mindfulness in achieving weight loss found that the majority of studies did result in weight loss but the extent to which mindfulness could be attributed to the effect was not apparent( Reference Olson and Emery 22 ). This study also noted the wide variation in interventions and methodological weaknesses.
It is important to recognise that many of the studies in binge eating and weight loss did not have a non-intervention control group and did not measure changes in mindfulness. Furthermore, few of the studies had a follow-up so it is not possible to determine long-term success. Despite these methodological weaknesses, the use of mindfulness and mindful eating in weight management and obesity-related behaviours shows promise and the field warrants further investigation.
In contrast to the intervention studies in overweight/obese studies, nearly half of the studies in normal-weight populations were laboratory-based, day-long studies, many of which were carried out among students. A small number of the studies were medium-length interventions (i.e. 6–16 weeks’ duration), which highlights the great variation in intensity of factors in the interventions in normal-weight subjects. The interventions were diverse and included teaching intuitive eating, providing mindfulness information, a mindfulness group intervention for 4 months, body scan-guided imagery, mindful eating exercises and mindful awareness. Furthermore, the outcomes varied widely, so comparison between studies was not possible. The outcomes included food choices, food intake, and the following eating behaviours: cravings, binge eating, internal cues, and the relationship with food. Overall, the results indicated a positive role for mindfulness and/or mindful eating on influencing eating behaviours. This avenue of research also merits further research as this has the potential to be relevant to public health nutrition messaging regarding food choices.
The observational studies also provide direction for future research but, by their nature, are evidence of association only. It is interesting to note that, in these observational studies, the focus was on intuitive eating whereas only two interventions( Reference Bacon, Stern and Van Loan 26 , Reference Healy, Joram and Matvienko 47 ) were based on intuitive eating. This indicates that intuitive eating is an emerging topic and further research is needed to examine its potential in positively having an impact on eating behaviours. The findings of the observational studies were unanimously positive, demonstrating a beneficial association of mindfulness/mindful eating or intuitive eating.
Overall, many studies were limited by small subject numbers and were also predominately carried out among female populations, the majority of whom were from Caucasian backgrounds. Given the importance of weight reduction in the management of type 2 diabetes and in CVD, it was surprising not to find more studies in these patient groups. This is likely to be an area of study in the future.
While research into the mechanisms of action of mindfulness is ongoing, particularly in relation to mindful eating, concomitant psychological and physiological findings have yielded three key hypotheses about the associated processes involved in the brain. Results from fMRI studies show that mindfulness is associated with reduced amygdala activity and may reduce emotional arousal. Mindfulness possibly works by increasing inner physical cues to eat (hunger and satiety), and decreasing the emotional and external cues to eat.
Only two studies reported negative results regarding the mindfulness or mindful eating intervention (small increases in weight and food intake), and one of these was in a population that is not generalisable.
Strengths and limitations of the present structured review
This structured review provides a literature review about the potential of mindfulness, mindful eating, and intuitive eating to make an impact on eating behaviours. It takes a broad approach, which provides perspective on the state of current research and direction of future research. It is common in research for observational studies to precede interventions where observed associations can be tested in experimental conditions. The description of the interventions and the tools used for outcome measures adds a new element to the systematic reviews undertaken to date in this area.
The review was never intended to be a systematic review and, as such, cannot make categorical statements on the quality of the evidence base. Furthermore, a rigorous critical appraisal of the literature is beyond the scope of this review. ‘Attention’ was not included in the search terms for the interventions undertaken and it has since become apparent that this would have been a relevant search term. Attentive eating is a similar concept to mindful eating and has been shown to reduce food intake( Reference Higgs 96 , Reference Robinson, Kersbergen and Higgs 97 ).
Conclusions
Mindfulness and mindful eating interventions appear to be most successful in the reduction of binge eating regardless of weight status. Mindfulness and mindful eating interventions also reduced emotional eating and eating in response to external cues which are important behaviours related to obesity.
In overweight individuals, the impact of mindfulness and mindful eating on reducing body weight was mixed; it might be that mindfulness and mindful eating have a role to play in the prevention of weight gain. Mindfulness/mindful eating resulted in a positive shift in food habits and in the quantities of food consumed in some studies. There is evidence both for the efficacy of one-off mindfulness interventions and also for the benefit of repeated practice on improving outcomes. On the basis of this review, encouraging a mindful approach to eating appears to be a positive message to be included in general weight-management advice to the public.
Acknowledgements
The present review was funded by an unconditional grant from Mondelez International. The authors are all independent freelance consultants and followed guidelines for scientific integrity from the inception of the review to final drafting of the manuscript. Mondelez International did not have any role in undertaking the review or interpreting the results.
The authors have no declarations of interest to declare.








