Introduction
Unhealthy diets and poor nutrition are leading risk factors for the rising rates of non-communicable diseases globally(Reference Afshin, Sur and Fay1). Dietary guidelines are developed as a reference standard to inform policy actions and regulation to attenuate these dietary risk factors(2). At the time of writing, ninety countries have developed food-based dietary guidelines, eighty-two of which recommend limiting or reducing the consumption of free or added sugar(Reference Hawkes, Jewell and Allen3,Reference Herforth, Arimond and Álvarez-Sánchez4) . Added sugars, generally defined as all monosaccharides and disaccharides added to foods by the manufacturer, cook or consumer(5), have increased in the food supply over the last 30 years, and are often a component of ultra-processed foods(Reference Popkin and Hawkes6,Reference Rikkers, Lawrence and Hafekost7) . The WHO recommends ‘free sugar’ consumption (consisting of both added sugar and sugars that are naturally present in honey, syrups and fruit juices) of no more than 10 % of total energy intake(Reference World Health8). Similarly, the Scientific Advisory Committee on Nutrition (SACN) in the UK and the USA dietary guidelines recommend limiting the intake of free sugar to 5 % and added sugar to 10 % of energy intake, respectively(9). Despite these recommendations, added sugar consumption contributes on average 11–17 % and 7–11 % of energy intake in European children and adults(Reference Azaïs-Braesco, Sluik and Maillot10), and 7·5–19·5 % across the American population(Reference Steele, Baraldi and da Costa Louzada11). Frequent overconsumption of added sugar has been linked with obesity, non-communicable diseases including type 2 diabetes, and dental caries, particularly from sugar-sweetened beverages (SSB)(Reference Sanigorski, Bell and Swinburn12–Reference Te Morenga, Mallard and Mann15).
A variety of policy actions have been implemented globally to reduce added sugar intakes(Reference Lang and Rayner16). Examples include: education based on the recommendations of food-based dietary guidelines(Reference Dixon, Borland and Segan17); food reformulation(Reference Leroy, Requillart and Soler18); taxation of added sugar(Reference Colchero, Rivera-Dommarco and Popkin19); restricting sugar-enriched food and drink availability(Reference Hawkes20); marketing restrictions(Reference Brinsden and Lobstein21); public awareness campaigns(Reference Crane, Egan and Browne22); and front-of-pack nutrient labelling(Reference Popkin and Hawkes6,Reference Thow and Hawkes23,Reference Peters, Dunford and Jones24) . Contesting paradigms exist regarding which types of policy actions should be implemented to reduce the consumption of added sugar. Broadly, these competing paradigms can be described as either ‘holistic’ or ‘reductionist’ in their approach to public health(Reference Federoff and Gostin25). Policy actions that align with the holistic paradigm target broader economic and food system changes, including improving dietary patterns, food security, the preservation of biodiversity and sustainability(Reference Fardet and Rock26). Conversely, a reductionist worldview promotes policy actions that target individual food products and their nutrient and ingredient composition(Reference Fardet and Rock26). The reductionist worldview has also been described as ‘nutritionism’ – an ideology in which the nutrients that comprise foods determine their value in the diet, as opposed to the whole food or dietary pattern(Reference Scrinis27).
A case study of saturated fat provides an example of the unintended consequences of reductionist policy. After research linked saturated fat to heart disease, consumers were encouraged to decrease its consumption(Reference Schleifer28). Consequently, trans-fats (partially hydrogenated plant oils) were often used to replace saturated fats in processed foods(Reference Schleifer28). Though trans-fats were initially regarded as a healthier, cheaper and often plant-based (i.e. ‘natural’) alternative, evidence now demonstrates that they contribute to heart disease to a greater extent than some saturated fats(Reference Remig, Franklin and Margolis29), and potentially increase the risk of type 2 diabetes and abdominal adiposity(Reference Micha and Mozaffarian30,Reference Kavanagh, Jones and Sawyer31) . In turn, trans-fats have now been reduced or removed from many food supply chains globally, though in many cases have been replaced with interesterified fats(Reference Mensink, Sanders and Baer32,Reference Mills, Hall and Berry33) . The health effects of interesterified fats, particularly in terms of cardiovascular health, are debated(Reference Mensink, Sanders and Baer32,Reference Mills, Hall and Berry33) . Parallels may be drawn between the reductionist approach to decrease saturated fat consumption by trans-fats substitution and current nutrient-specific policy actions to decrease added sugar consumption.
Substituting non-nutritive sweeteners (NNS) for added sugar in ultra-processed food is one action that may reduce added sugar in the food supply. NNS are non-energy food additives that impart sweetness when added to a product(34). They are used as substitutes for nutritive sweeteners (including sugar, honey and high-fructose maize syrup, among others) to reduce the energy and sugar content of processed foods while maintaining their palatability(Reference Chattopadhyay, Raychaudhuri and Chakraborty35). The phrase ‘NNS’ has been chosen for this review based on terminology used by organisations including the Codex Alimentarius Commission (Codex), the United States Department of Agriculture and the FAO, as well as being commonly used throughout the literature. NNS are also commonly referred to as artificial sweeteners (although this term ignores ‘natural’ sweeteners including stevia and monk fruit extract), non-caloric sweeteners, low-calorie sweeteners, intense sweeteners and high-intensity sweeteners. There are currently thirteen NNS approved for use globally (though specific types of sweeteners permitted for use differ between countries). The amounts of NNS that can be used in a product, and the products to which they can be added, is determined by each country’s food standards regulating body. Online Supplementary Table S1 details all NNS currently in the global food supply, including their sweetener class, acceptable daily intake (ADI), relative sweetness to sucrose, energy per g, uses and properties. In this instance, NNS does not include polyols, as these additives have a small energy content(Reference Grembecka36).
Given the novelty of many NNS, questions have been posed about their risk to public health(Reference Sylvetsky, Hiedacavage and Shah37). Systematic reviews have found that the benefits and harms of NNS are inconsistently reported(Reference Toews, Lohner and de Gaudry38,Reference Azad, Abou-Setta and Chauhan39) . Experimental animal studies and observational studies in human subjects have reported associations between NNS consumption and weight gain(Reference Toews, Lohner and de Gaudry38,Reference Fowler, Williams and Resendez40–Reference Stellman and Garfinkel42) , changes to the gut microbiome (by saccharin, sucralose and stevia)(Reference Ruiz-Ojeda, Plaza-Díaz and Sáez-Lara43) and an increased risk of type 2 diabetes(Reference O’Connor, Imamura and Lentjes44,Reference Bhupathiraju, Pan and Malik45) . Relationships from observational studies can only be classified as correlational and may suffer from bias, as participants with existing morbidities may be more likely to consume NNS than those without. Comparatively, clinical trials and experimental studies in human subjects have generally shown that NNS consumption is associated with a reduction in BMI(Reference Peters, Wyatt and Foster46–Reference Imamura, O’Connor and Ye48) and fasting blood glucose(Reference Raben, Vasilaras and Møller49,Reference Nichol, Holle and An50) . Additionally, some experimental studies have found no effects of NNS consumption on BMI(Reference Madjd, Taylor and Delavari51,Reference Kuzma, Cromer and Hagman52) . As public health impacts typically rely on dietary patterns, more studies are needed that detail the impacts of diets high in NNS on dental health, type 2 diabetes and other health outcomes. The overall consensus throughout the literature is that NNS are not carcinogenic(Reference Mishra, Ahmed and Froghi53,Reference Gallus, Scotti and Negri54) . In addition to these toxicological concerns, particular NNS (including acesulfame-K) are ‘micro-pollutants’; they are not effectively removed from wastewater after treatment, and hence may contaminate water supplies(Reference Mawhinney, Young and Vanderford55,Reference Scheurer, Storck and Brauch56) .
In public health, the nature and scope of risk are broader than the toxicological outcomes outlined above. Concerns have also been raised over the potential substitution effects of low-energy, NNS-containing discretionary foods for nutritious whole foods, and the long-term impact this may have on population health(Reference Sylvetsky, Hiedacavage and Shah37). Nutrient-level policies to reduce added sugar consumption may encourage the reformulation of existing high-sugar products with NNS. This can create a ‘health halo effect’, allowing industry to make discretionary products appear ‘healthy’(Reference Brownell and Koplan57). This perception of healthiness may be used to promote the consumption of low-sugar, low-energy discretionary foods while displacing more nutritious foods from the diet.
Despite the increasing attention on added sugar intake, and subsequent policy actions to reduce it, there is a lack of understanding of the politics influencing the promotion of such actions, the impact of these policy actions on the added sugar and NNS composition of foods and beverages, and the subsequent impact on NNS consumption and overall dietary balance. Thus, the aim of the present review is to evaluate how policy actions to reduce added sugar consumption may influence NNS-related food supply trends, the consumption of NNS and dietary patterns more broadly. This review will be divided into three sections: (i) an overview of current NNS food supply and consumption patterns; (ii) added sugar-reduction policies and their impact on NNS; and (iii) the impact of NNS on food choice, energy intake and diet quality.
Methods
A narrative review method was adopted, given the complexity of the topic, and the diverse aims, study designs and methods of the included literature(Reference Green, Johnson and Adams58,Reference Popay, Roberts and Sowden59) . To improve the rigour of the review, a systematic search of the literature was performed. This involved restricting the focus to well-defined areas of interest, and the application of strict inclusion and exclusion criteria(Reference Ferrari60). The search followed four steps: (i) a scoping review; (ii) systematic search for relevant literature; (iii) appraisal of studies selected for review; and (iv) data extraction, analysis and synthesis of the results.
Scoping review and systematic search for relevant literature
After consultation with a research liaison librarian, databases used included EBSCOhost (advanced search database – Academic Search Complete; Business Source Complete; CINAHL Complete; Global Health, GreenFILE; Health Policy Reference Center, MEDLINE Complete, PsycINFO, SocINDEX), Web of Science and Scopus. These databases were chosen for their comprehensiveness and conventional use in the public health nutrition discipline. Given the broad nature of the review, three searches with different search strings were used to capture all relevant literature. Search terms were identified from an initial scoping review. The search was conducted in March and April of 2019 and updated in January of 2020. Search strings are shown in Table 1. A citation snowballing technique was also used, which involved hand searching key papers’ reference lists.
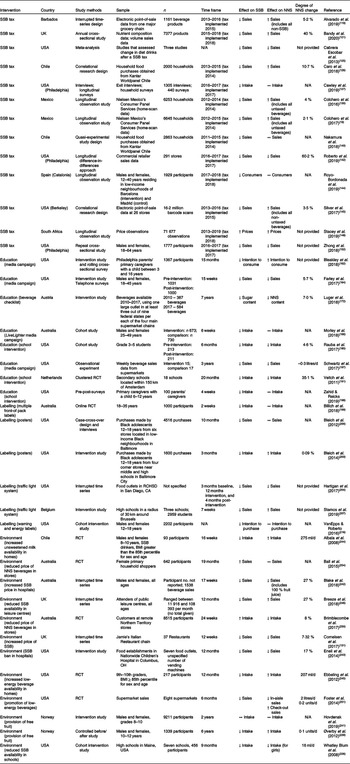
Table 1. Search strings used for the present review
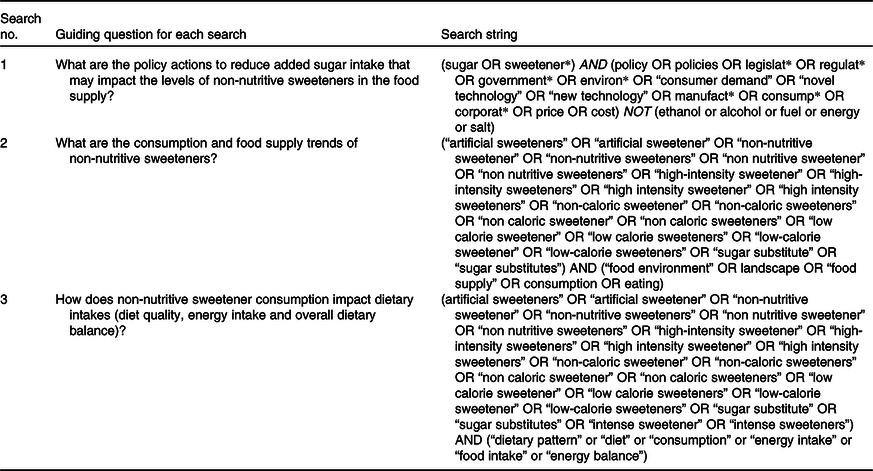
The inclusion and exclusion criteria are shown in Table 2. The year 1878 was chosen as the starting date for literature as this marked the discovery of the first NNS (saccharin).
Table 2. Inclusion and exclusion criteria for the present review
* The year 1878 was chosen as this was when the first non-nutritive sweetener (saccharin) was discovered.
Appraisal of selected studies for review
Duplicates were removed. Remaining records were then screened against the inclusion and exclusion criteria listed in Table 2. This involved the following steps: (i) screening of studies by title; (ii) screening of remaining studies by abstract; (iii) screening of remaining studies by full text. A second reviewer independently screened 10 % of articles by title and abstract, and all full-text articles, to minimise bias. Disagreements were resolved through discussion; where no agreement was reached, a third party acted as an arbiter. As this research aimed to assess the effects of existing, implemented policy initiatives, modelling studies were intentionally excluded. This decision was made to clearly address the research question and aims, for which policy actions needed to have been implemented such that their influence on the food supply and consumption could be determined. For search 1, only studies that explored how a policy action directly affected NNS consumption or levels in the food supply were critically analysed. Despite the potential for the same policy actions discussed in other studies to have an impact on NNS, it was not possible to infer this outcome if the authors had not specifically analysed the change in NNS consumption, sales or levels in the food supply. Fig. 1 shows a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart of the search.

Fig. 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the search.
Data extraction, analysis, and synthesis
Included studies were uploaded to the qualitative analysis software NVivo (QSR International, version 12) for data extraction and analysis. First, all studies were coded using a coding schema derived from the scoping review. Constant comparative analysis was used to compare, integrate, modify and/or generate new codes through ongoing rounds of data analysis(Reference Glaser61,Reference Fram62) . The coded data were used to identify major themes that were then synthesised into the results. Results were discussed comprehensively with the research team as the analysis progressed to limit researcher subjectivity.
Results
Overview of studies
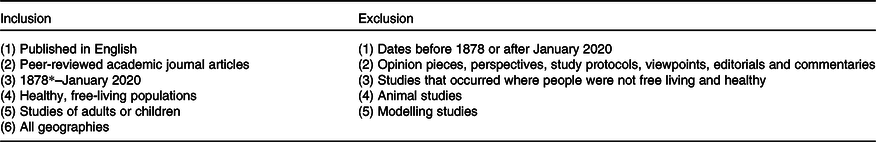
A total of 246 peer-reviewed journal articles were included in the review. As shown in Fig. 2, the frequency of studies assessing NNS increased over time. This suggests an increased research interest in this topic area, consistent with a growing number of policy actions targeting added sugar internationally and the rise in variety and regulation of NNS.
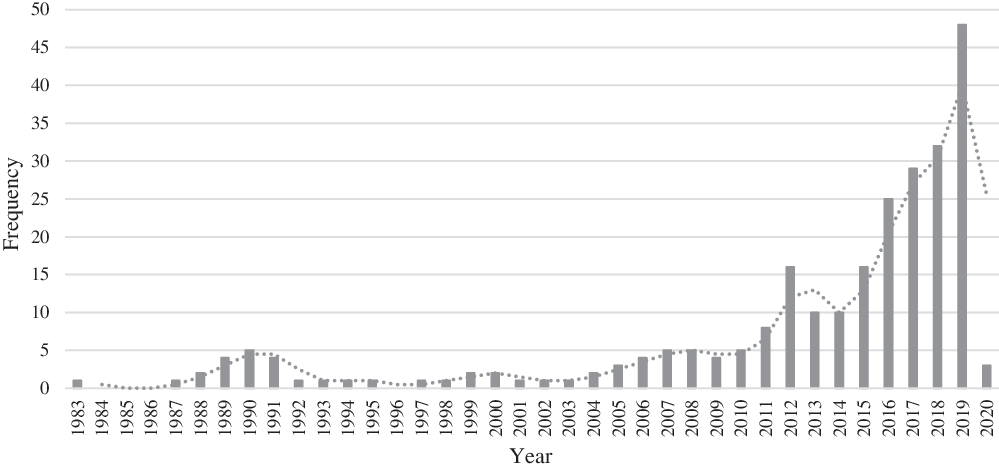
Fig. 2. Frequency of studies included in the review by year.
Current non-nutritive sweetener food supply and consumption patterns
Fifty-four studies included in the review explored NNS consumption trends and levels in the food supply. A description of these studies is included as online Supplementary Table S2.
Food supply patterns
Studies found NNS in a wide variety of products across the global food supply, often in food that consumers may not expect, were not labelled as ‘diet’ or ‘lite’ and were not traditionally sweet. These products included yoghurt(Reference Durán Agúero, Noel and Arrivillaga63–Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77), dairy desserts (including mousse and ice-cream)(Reference Arcella, Le Donne and Piccinelli64,Reference Chung, Suh and Yoo66–Reference Garavaglia, Garcia and Zapata69,Reference Janvier, Goscinny and Donne71,Reference Le Donne, Mistura and Goscinny72,Reference Sylvetsky, Jin and Clark74,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77–Reference Vin, Connolly and McCaffrey79) , milk(Reference Ha, Ha and Choi80,Reference Probst, Dengate and Jacobs81) , carbonated beverages(Reference Durán Agúero, Noel and Arrivillaga63–Reference Buffini, Goscinny and Van Loco65,Reference Dellavalle, Malek and Hunt67–Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72–Reference Huizinga and Hubert92) , energy drinks(Reference Ng, Slining and Popkin73,Reference Dunford, Taillie and Miles78) , bakery products(Reference Figueiredo, Scapin and Fernandes68,Reference Pielak, Czarniecka-Skubina and Trafiaek76,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77,Reference Probst, Dengate and Jacobs81,Reference Tennant and Vlachou93) , other drinks (fruit drinks, ice tea, vegetable juice, nectar, cordial and flavoured mineral water)(Reference Durán Agúero, Noel and Arrivillaga63–Reference Buffini, Goscinny and Van Loco65,Reference Figueiredo, Scapin and Fernandes68–Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72,Reference Ng, Slining and Popkin73,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77,Reference Hedrick, Passaro and Davy84,Reference Lino, Costa and Pena86,Reference Mesirow and Welsh88,Reference Boulton, Hashem and Jenner94) , pre-made coffee/tea(Reference Ha, Ha and Choi80,Reference Ha, Ha and Choi83–Reference Lee, Do and Lee85,Reference Mesirow and Welsh88) , table-top sweeteners(Reference Arcella, Le Donne and Piccinelli64,Reference Buffini, Goscinny and Van Loco65,Reference Dellavalle, Malek and Hunt67,Reference Garavaglia, Garcia and Zapata69,Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72,Reference Pielak, Czarniecka-Skubina and Trafiaek76,Reference Hedrick, Passaro and Davy84) , confectionery (including chewing gum)(Reference Arcella, Le Donne and Piccinelli64–Reference Dellavalle, Malek and Hunt67,Reference Garavaglia, Garcia and Zapata69–Reference Le Donne, Mistura and Goscinny72,Reference Pielak, Czarniecka-Skubina and Trafiaek76,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77,Reference Vin, Connolly and McCaffrey79–Reference Probst, Dengate and Jacobs81,Reference Ha, Ha and Choi83,Reference Lee, Do and Lee85) , pickled food(Reference Ha, Ha and Choi83,Reference Lee, Do and Lee85) , processed fruits and vegetables(Reference Tennant and Vlachou93), jam(Reference Arcella, Le Donne and Piccinelli64,Reference Grech, Kam and Gemming70–Reference Le Donne, Mistura and Goscinny72,Reference Zygler, Wasik and Kot-Wasik75) , salad dressing(Reference Dellavalle, Malek and Hunt67,Reference Ng, Slining and Popkin73,Reference Lee, Do and Lee85) , cream substitutes(Reference Dellavalle, Malek and Hunt67), alcoholic drinks(Reference Chung, Suh and Yoo66,Reference Ha, Ha and Choi80,Reference Ha, Ha and Choi83,Reference Lee, Do and Lee85,Reference Kim, Lee and Lim95) , condiments(Reference Chung, Suh and Yoo66,Reference Janvier, Goscinny and Donne71,Reference Le Donne, Mistura and Goscinny72,Reference Pielak, Czarniecka-Skubina and Trafiaek76,Reference Vin, Connolly and McCaffrey79,Reference Lee, Do and Lee85,Reference Martyn, Nugent and McNulty87) , syrup(Reference Le Donne, Mistura and Goscinny72,Reference Ha, Ha and Choi80) , cereal(Reference Probst, Dengate and Jacobs81,Reference Tennant and Vlachou93) , miscellaneous snack foods(Reference Lee, Do and Lee85), protein bars(Reference Ng, Slining and Popkin73), baby food(Reference Ng, Slining and Popkin73), flavoured ice(Reference Lee, Do and Lee85,Reference Meenakshi, Khanna and Mukul96) , fish products(Reference Zygler, Wasik and Kot-Wasik75,Reference Lee, Do and Lee85) and pan masala(Reference Meenakshi, Khanna and Mukul96). While most of these sweetened products were found in several countries, pan masala was specific to India, whilst the alcoholic drinks Soju, Takju and Yakju were specific to South Korea. It is important to note that all products found to contain NNS were ultra-processed foods.
The products contributing the most to NNS consumption were carbonated beverages(Reference Durán Agúero, Noel and Arrivillaga63,Reference Buffini, Goscinny and Van Loco65,Reference Dellavalle, Malek and Hunt67,Reference Garavaglia, Garcia and Zapata69,Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72–Reference Zygler, Wasik and Kot-Wasik75,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77,Reference Dunford, Taillie and Miles78,Reference Ha, Ha and Choi80,Reference Durán Agúero, Oñateb and Riverac82–Reference Hedrick, Passaro and Davy84,Reference Lino, Costa and Pena86,Reference Martyn, Nugent and McNulty87,Reference Piernas, Ng and Popkin89–Reference Sjöberg and Penttilä91) , dairy products (especially yoghurts)(Reference Durán Agúero, Noel and Arrivillaga63,Reference Buffini, Goscinny and Van Loco65–Reference Figueiredo, Scapin and Fernandes68,Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72–Reference Sylvetsky, Jin and Clark74,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77,Reference Dunford, Taillie and Miles78) , confectionery (including chewing gum)(Reference Arcella, Le Donne and Piccinelli64–Reference Chung, Suh and Yoo66,Reference Le Donne, Mistura and Goscinny72,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77,Reference Probst, Dengate and Jacobs81,Reference Leclercq, Berardi and Sorbillo97) , table-top sweeteners(Reference Arcella, Le Donne and Piccinelli64,Reference Dellavalle, Malek and Hunt67,Reference Garavaglia, Garcia and Zapata69,Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72,Reference Hedrick, Passaro and Davy84) and juices(Reference Durán Agúero, Noel and Arrivillaga63,Reference Garavaglia, Garcia and Zapata69,Reference de Lourdes Samaniego-Vaesken, Partearroyo and Cano77,Reference Hedrick, Passaro and Davy84) . Some studies found that NNS did not always entirely replace sugar in sweetened products; rather, they were used in addition to nutritive sweeteners(Reference Ng, Slining and Popkin73,Reference Piernas, Ng and Popkin89,Reference Sylvetsky, Welsh and Brown98) .
Non-nutritive sweetener consumption
Few studies (n 10) explored the trends of NNS consumption over time. Those that did demonstrated an increase(Reference Ng, Slining and Popkin73,Reference Sylvetsky, Jin and Clark74,Reference Durán Agúero, Oñateb and Riverac82,Reference Mesirow and Welsh88,Reference Piernas, Ng and Popkin89,Reference Sylvetsky, Welsh and Brown98–Reference Fakhouri, Kit and Ogden103) (Table 3). Consumer purchasing data are included together with data on consumption, as the trends in NNS purchasing were often used as a proxy by studies to estimate consumption trends. The major contributors to the increase in NNS consumption were beverages(Reference Mesirow and Welsh88,Reference Piernas, Ng and Popkin89,Reference Sylvetsky, Welsh and Brown98–Reference Drewnowski and Rehm101,Reference Fakhouri, Kit and Ogden103) , though changes in beverage consumption were also often the only variable studied.
Table 3. Trends of non-nutritive sweetener (NNS) consumption by country
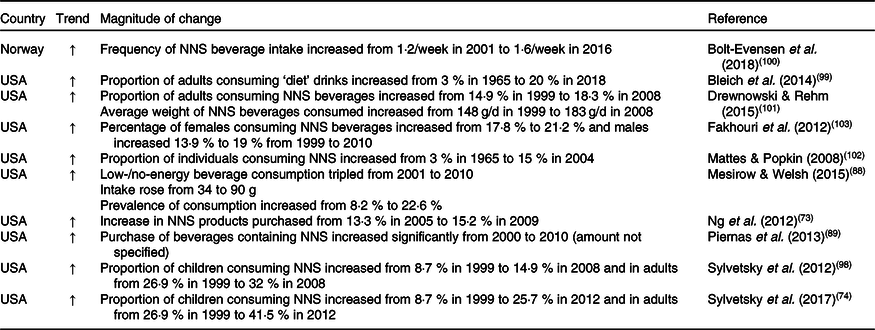
↑, Increase.
Though longitudinal studies suggested that the proportion of the population consuming NNS is increasing, almost all cross-sectional studies demonstrated that amounts consumed did not exceed the ADI (the amount of the sweetener that can be consumed on a daily basis over a lifetime without appreciable risk to health)(Reference Durán Agúero, Noel and Arrivillaga63–Reference Chung, Suh and Yoo66,Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72,Reference Vin, Connolly and McCaffrey79,Reference Durán Agúero, Oñateb and Riverac82,Reference Ha, Ha and Choi83,Reference Lee, Do and Lee85–Reference Martyn, Nugent and McNulty87,Reference Tennant and Vlachou93,Reference Kim, Lee and Lim95,Reference Leclercq, Berardi and Sorbillo97,Reference Bär and Biermann104–Reference Huvaere, Vandevijvere and Hasni106) . Generally, this was determined through either food records(Reference Arcella, Le Donne and Piccinelli64,Reference Buffini, Goscinny and Van Loco65,Reference Durán Agúero, Oñateb and Riverac82,Reference Bär and Biermann104) or a combination of diet recalls (to determine consumption) and food label surveys/HPLC (to determine the amount of NNS in food and beverage items)(Reference Chung, Suh and Yoo66,Reference Le Donne, Mistura and Goscinny72,Reference Ha, Ha and Choi80,Reference Lee, Do and Lee85,Reference Lino, Costa and Pena86,Reference Kim, Lee and Lim95,Reference Diogo, Silva and Pena105,Reference Huvaere, Vandevijvere and Hasni106) . There were exceptions to this finding, although these were generally found in particular sub-groups of consumers(Reference Durán Agúero, Noel and Arrivillaga63,Reference Bär and Biermann104,Reference Mancini, Paul and Gauvreau107) . Consumption of NNS was closer to the ADI for toddlers and children, probably due to their lower body mass but not proportionately decreased consumption of sweeteners(Reference Garavaglia, Garcia and Zapata69,Reference Vin, Connolly and McCaffrey79,Reference Ha, Ha and Choi83,Reference Tayel, Khamis and Darwish90,Reference Tennant and Vlachou93,Reference Bär and Biermann104,Reference Mancini, Paul and Gauvreau107) . Illustratively, Garavaglia et al. (Reference Garavaglia, Garcia and Zapata69) found that 1·1 % of pre-schoolers and 0·9 % of school children in Argentina exceeded the ADI of cyclamate. Additionally, Meenakshi et al. (Reference Meenakshi, Khanna and Mukul96) found that an Indian sub-population could be exceeding the ADI for saccharin due to high consumption of pan masala and crushed ice. Of the sweeteners studied, cyclamate was almost always the sweetener closest to or exceeding the ADI(Reference Durán Agúero, Noel and Arrivillaga63,Reference Arcella, Le Donne and Piccinelli64,Reference Garavaglia, Garcia and Zapata69,Reference Leclercq, Berardi and Sorbillo97,Reference Bär and Biermann104,Reference Leth, Fabricius and Fagt108) . Contributing factors may include the relative affordability of cyclamate when compared with other sweeteners, the higher amounts by weight included in food (as cyclamate is only 30 × sweeter than sugar, compared with advantame, which is 20 000 × sweeter) and its prevalence as a commonly used sweetener in many countries’ food supplies(Reference Moskowitz109).
The characteristics of NNS consumers were consistent across most studies. Frequently, in comparison with non-consumers, NNS consumers had a higher BMI(Reference Grech, Kam and Gemming70,Reference Sylvetsky, Jin and Clark74,Reference Hedrick, Passaro and Davy84,Reference Tayel, Khamis and Darwish90,Reference Sylvetsky, Welsh and Brown98,Reference Bleich, Wolfson and Vine99,Reference Chia, Shardell and Tanaka110–Reference Bellisle, Altenburg de Assis and Fieux114) (though one study found this association only in women, not men(Reference Durán Agúero, Noel and Arrivillaga63)), higher education level/socio-economic status(Reference Durán Agúero, Noel and Arrivillaga63,Reference Grech, Kam and Gemming70,Reference Sylvetsky, Jin and Clark74,Reference Pielak, Czarniecka-Skubina and Trafiaek76,Reference Hedrick, Passaro and Davy84,Reference Piernas, Ng and Popkin89,Reference Bleich, Wolfson and Vine99,Reference Bolt-Evensen, Vik and Stea100,Reference Malek, Hunt and Dellavalle111–Reference An113,Reference Drewnowski and Rehm115) , were more likely to be women(Reference Arcella, Le Donne and Piccinelli64,Reference Grech, Kam and Gemming70,Reference Sylvetsky, Jin and Clark74,Reference Hedrick, Passaro and Davy84,Reference Piernas, Ng and Popkin89,Reference Tayel, Khamis and Darwish90,Reference Sylvetsky, Welsh and Brown98–Reference Bolt-Evensen, Vik and Stea100,Reference Malek, Hunt and Dellavalle111,Reference Monteiro, Hassan and Rodrigues112,Reference Drewnowski and Rehm115) , had increased consumption with age(Reference Grech, Kam and Gemming70,Reference Sylvetsky, Jin and Clark74,Reference Hedrick, Passaro and Davy84,Reference Bolt-Evensen, Vik and Stea100,Reference Malek, Hunt and Dellavalle111,Reference Monteiro, Hassan and Rodrigues112,Reference Drewnowski and Rehm115) (though two studies found the opposite(Reference Bleich, Wolfson and Vine99,Reference Chia, Shardell and Tanaka110) ), were more likely to be non-Hispanic whites(Reference Grech, Kam and Gemming70,Reference Sylvetsky, Jin and Clark74,Reference Hedrick, Passaro and Davy84,Reference Piernas, Ng and Popkin89,Reference Bleich, Wolfson and Vine99,Reference Malek, Hunt and Dellavalle111,Reference Drewnowski and Rehm115) , more likely to be on a diet(Reference Grech, Kam and Gemming70,Reference Hedrick, Passaro and Davy84,Reference Tayel, Khamis and Darwish90,Reference Bolt-Evensen, Vik and Stea100) or have type 2 diabetes(Reference Grech, Kam and Gemming70,Reference Sylvetsky, Jin and Clark74,Reference Chia, Shardell and Tanaka110) and were more likely to live in an English-speaking country(Reference Grech, Kam and Gemming70,Reference Drewnowski and Rehm115,Reference Jin, Sylvetsky and Kandula116) .
Added sugar-reduction policies and their impact on non-nutritive sweeteners in the food supply
A total of 134 studies included in the review assessed policy actions to reduce added sugar consumption. Five main policy categories emerged: taxation (n 38), education (n 41), food environment interventions (n 49), labelling (n 22) and reformulation (n 6). Here, n is larger than the total number of studies as some described more than one policy action.
A summary of studies that have assessed the impact of these policy actions on added sugar consumption, and how this has affected either NNS consumption or levels in the food supply, is shown in Table 4. Studies that assessed policy actions promoting the consumption of whole foods or improved dietary patterns, including subsidies on fruits and vegetables or the promotion of dietary guidelines, were infrequent. Instead, the majority of the policy actions studied were reductionist, focusing only on nutrients (added sugar) rather than the foods or dietary patterns.
Table 4. Summary of studies assessing the impact of policy actions targeting added sugar consumption on non-nutritive sweetener (NNS) consumption or levels in the food supply
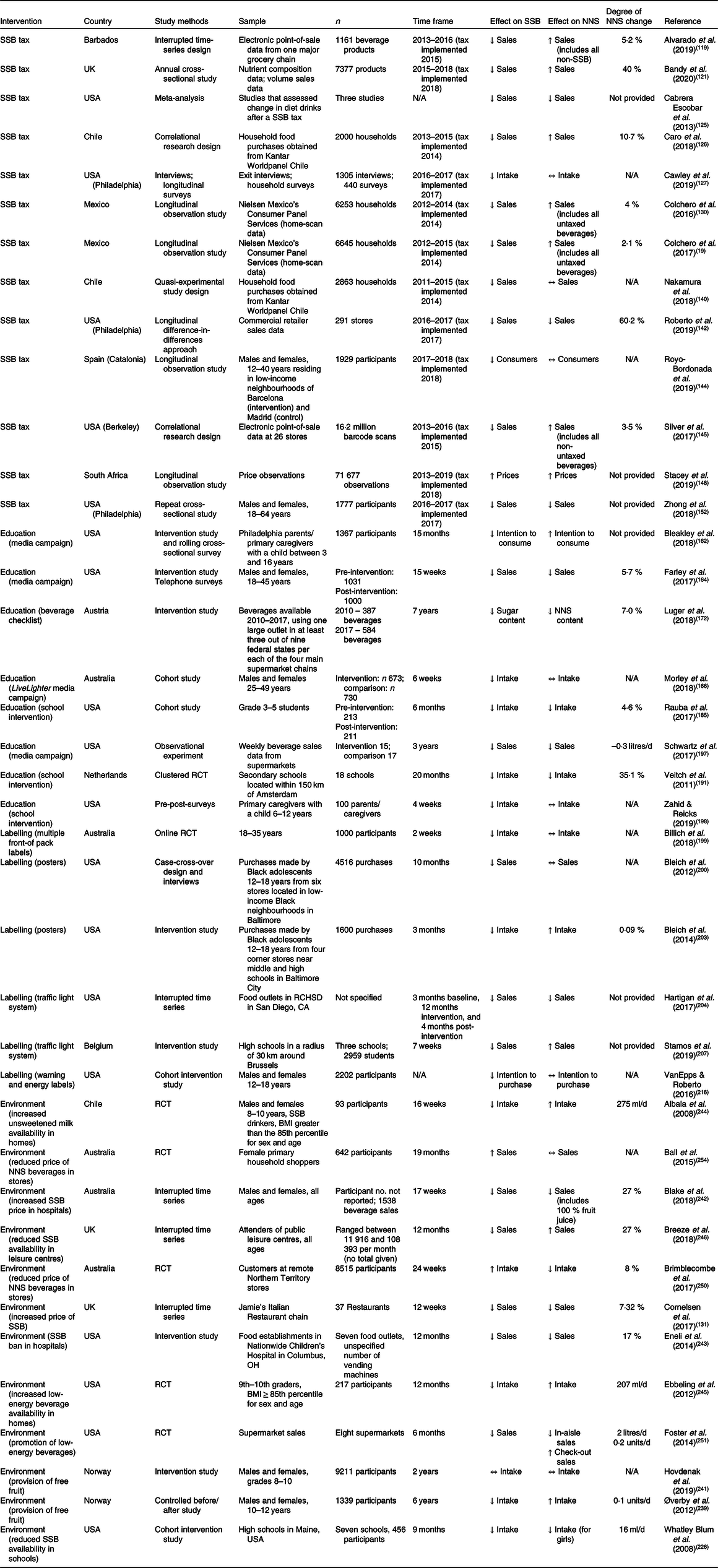
SSB, sugar-sweetened beverages; ↓, decrease; ↑, increase; N/A, not applicable; ↔, no change; RCT, randomised controlled trial; RCHSD, Rady Children’s Hospital-San Diego.
Taxation
Of the studies included in the review, thirty-eight focused on taxation(Reference Popkin and Hawkes6,Reference Colchero, Rivera-Dommarco and Popkin19,Reference Acton, Jones and Kirkpatrick117–Reference Zhong, Auchincloss and Lee152) . This includes those that both did and did not directly assess the impact of sugar taxes on NNS consumption and levels in the food supply. In this instance, studies referred to an excise tax – an indirect tax imposed on the manufacture of certain types of goods and products(Reference Brownell, Farley and Willett153). Taxes on added sugar are used to increase the price of a product relative to its low-sugar counterparts, following the economic principle of ‘price elasticity’ (the percentage change in demand caused by a percentage change in price)(Reference Chaloupka, Powell and Warner154). In this model, less expensive alternatives are thought to be more desirable to consumers, thus reducing the demand for high-sugar products(Reference Chaloupka, Powell and Warner154,Reference Colchero, Salgado and Unar-Munguía155) . At the time of writing, forty-one countries have enacted a SSB tax (excluding the USA, where taxes are state-specific)(156). Generally, SSB taxes (as the name suggests) only apply to SSB, though select countries (including France, Philippines, India and the state of Philadelphia in the USA) also tax beverages containing NNS. Chile is currently the only country to subsidise ‘diet’ beverages, further enhancing the price elasticity between SSB and beverages containing NNS(Reference Guerrero-López, Unar-Munguía and Colchero157).
Few of the studies assessing taxes explored how this intervention may affect NNS consumption or levels in the food supply (n 13; Table 4). Despite not directly reporting so, it is likely that the SSB taxes discussed in other studies also had an effect on these outcomes, as encouraging industry to reformulate is one of the key aims of nutrient-specific taxes(156,Reference Baker, Jones and Thow158) . SSB sales decreased in all studies that explored this outcome in response to a tax (Table 4)(Reference Colchero, Rivera-Dommarco and Popkin19,Reference Alvarado, Unwin and Sharp119,Reference Bandy, Scarborough and Harrington121,Reference Cabrera Escobar, Veerman and Tollman125–Reference Cawley, Frisvold and Hill127,Reference Colchero, Popkin and Rivera130,Reference Nakamura, Mirelman and Cuadrado140,Reference Roberto, Lawman and Levasseur142,Reference Royo-Bordonada, Fernandez-Escobar and Simon144,Reference Silver, Ng and Ryan-Ibarra145,Reference Zhong, Auchincloss and Lee152) . While some studies (n 6) suggested that a tax on SSB increased the purchase of NNS beverages(Reference Colchero, Rivera-Dommarco and Popkin19,Reference Alvarado, Unwin and Sharp119,Reference Bandy, Scarborough and Harrington121,Reference Caro, Corvalán and Reyes126,Reference Colchero, Popkin and Rivera130,Reference Silver, Ng and Ryan-Ibarra145) , others (n 3) found the opposite(Reference Cabrera Escobar, Veerman and Tollman125,Reference Roberto, Lawman and Levasseur142,Reference Zhong, Auchincloss and Lee152) , and yet others (n 3) found no change in consumption or purchasing behaviour(Reference Cawley, Frisvold and Hill127,Reference Nakamura, Mirelman and Cuadrado140,Reference Royo-Bordonada, Fernandez-Escobar and Simon144) . In four studies, NNS beverages were grouped with all non-SSBS(Reference Colchero, Rivera-Dommarco and Popkin19,Reference Alvarado, Unwin and Sharp119,Reference Colchero, Popkin and Rivera130,Reference Royo-Bordonada, Fernandez-Escobar and Simon144) . This may confound the results, as the change in non-SSB sales could be attributable to water, milk or juice. In South Africa, Stacey et al. (Reference Stacey, Mudara and Ng148) found that prices for artificially sweetened and low-sugar drinks increased, despite not being affected by the SSB tax, which may have impacted the effect of the tax on beverage purchases overall. Zhong et al. (Reference Zhong, Auchincloss and Lee152), Cawley et al. (Reference Cawley, Frisvold and Hill127) and Roberto et al. (Reference Roberto, Lawman and Levasseur142) found decreases in NNS beverage consumption post-tax; however, the tax in Philadelphia (which the studies analysed) also targeted NNS beverages. This reduced the likelihood of consumers substituting SSB with NNS beverages, as there would be no relative change in price elasticity.
The main data source for these studies was scanned labels of products, either by participants in the home or at the point of sale. Though the sample size generated by these methods is extensive, there is an absence of information on food consumed outside the home or grocery store purchases. This is problematic, as a large proportion of ‘soft’ drinks (both NNS and SSB) are likely to be purchased and consumed outside the home(Reference Ogden, Kit and Carroll159,Reference Bezerra, de Moura Souza and Pereira160) . Additionally, in data sources including Nielsen Homescan Panel Data, participants must scan all groceries at home. The process of recording all purchases can be time consuming, which could result in under-reporting(Reference Einav, Leibtag and Nevo161).
Education interventions
Education-based interventions included media campaigns(Reference Popkin and Hawkes6,Reference Kirkpatrick, Raffoul and Maynard137,Reference Bleakley, Jordan and Mallya162–Reference Morley, Niven and Dixon170) , community education(Reference Doymaz and Neuspiel171–Reference Yuhas, Porter and Brock178) and education in schools and childcare centres(Reference Avery, Bostock and McCullough179–Reference Santaló, Gibbons and Naylor196) on the harms of excess added sugar consumption. Of the studies exploring this policy action (n 39), only eight (Table 4) addressed the impact that education interventions to reduce added sugar intake may have on NNS consumption and levels in the food supply. While most studies (n 5) found that NNS beverage consumption and sales decreased in response to education addressing added sugar consumption(Reference Farley, Halper and Carlin164,Reference Luger, Winzer and Schätzer172,Reference Rauba, Tahir and Milford185,Reference Veitch, Singh and van Stralen191,Reference Schwartz, Schneider and Choi197) , one study found the opposite(Reference Bleakley, Jordan and Mallya162), and yet two others found no association(Reference Morley, Niven and Dixon166,Reference Zahid and Reicks198) .
When analysing responses to the ‘Beverage checklist’ (a guide for beverage selection based on the nutritional value of a drink) in 2012, Luger et al. (Reference Luger, Winzer and Schätzer172) found that while the percentage of beverages containing NNS increased initially, by 2017 there was a net decrease of 7 %. During this period, added sugar content in beverages decreased significantly, suggesting a lack of substitution of sugar with NNS. In school settings, both Veitch et al. (Reference Veitch, Singh and van Stralen191) and Rauba et al. (Reference Rauba, Tahir and Milford185) found that an SSB education campaign directed at children greatly reduced both SSB and NNS beverage consumption. In studies from Farley et al. (Reference Farley, Halper and Carlin164) and Schwartz et al. (Reference Schwartz, Schneider and Choi197) NNS beverage sales decreased in both groups that received anti-SSB messaging and their controls.
Contrastingly, when using text messages and newsletters to promote positive beverage purchases, Zahid & Reicks(Reference Zahid and Reicks198) found that while SSB intake decreased, NNS beverage consumption was not affected. Similarly, Morley et al. (Reference Morley, Niven and Dixon166) found that despite a decrease in SSB intake, there was no change in reported NNS beverage consumption after exposure to the LiveLighter campaign (a programme to encourage healthier dietary choices and lifestyles). Finally, in a study from Bleakley et al. (Reference Bleakley, Jordan and Mallya162), parents exposed to anti-SSB messaging expressed an increased intention to substitute SSB with NNS beverages for both their children and themselves. Overall, studies that assessed education campaigns to reduce added sugar intake did not examine the potential substitution effect of NNS for sugar. Among those that did, most studies found a decrease in NNS consumption and sales. This may be explained in part by the fact that many of the media campaigns to reduce SSB intake promoted replacing SSB with water.
Labelling
Labelling interventions included energy and nutrient-specific labelling(Reference Billich, Blake and Backholer199–Reference Bleich, Barry and Gary-Webb203), traffic light labelling (a system wherein foods are graded from green (best choice) to red (limit consumption))(Reference Popkin and Hawkes6,Reference Bergallo, Castagnari and Fernández123,Reference Hartigan, Patton-Ku and Fidler204–Reference Stamos, Lange and Dewitte207) , other nutrient-based front-of-pack labelling(Reference Popkin and Hawkes6,Reference Studdert, Flanders and Mello149,Reference Billich, Blake and Backholer199,Reference Cawley, Sweeney and Sobal208–Reference Siegel, Anneken and Duffy210) and warning labels(Reference Popkin and Hawkes6,Reference Bergallo, Castagnari and Fernández123,Reference Bollard, Maubach and Walker124,Reference Ares, Machin and Vidal211–Reference VanEpps and Roberto216) . Labelling interventions aim to provide consumers with easy-to-understand information regarding micro-/macronutrients and energy within a product, potentially negative effects of a product or its ingredients, and are used to compare one product with another(Reference Kanter, Vanderlee and Vandevijvere217). A secondary aim of labelling interventions is to encourage reformulation by the food industry to produce ‘healthier’ food(Reference Kanter, Vanderlee and Vandevijvere217). Of note, labelling of this variety is commonly only applied to processed and ultra-processed foods. Of the studies exploring this policy action (n 22), six addressed the impact that labelling may have had on NNS consumption and levels in the food supply (Table 4). While one study found that NNS beverage consumption and sales decreased in response to labelling interventions(Reference Hartigan, Patton-Ku and Fidler204), two found the opposite(Reference Bleich, Barry and Gary-Webb203,Reference Stamos, Lange and Dewitte207) , and three others found no association(Reference Billich, Blake and Backholer199,Reference Bleich, Herring and Flagg200,Reference VanEpps and Roberto216) .
When traffic light labelling was used by Hartigan et al. (Reference Hartigan, Patton-Ku and Fidler204) in a hospital setting, in which NNS beverages and SSB were classified as yellow and red, respectively, sales of both beverages decreased over time. Comparatively, using a similarly designed traffic light system in Belgian high schools, Stamos et al. (Reference Stamos, Lange and Dewitte207) found that while SSB sales decreased, NNS beverage sales increased. Though in their 2012 study(Reference Bleich, Herring and Flagg200), Bleich et al. found no significant change in consumption, in 2014, Bleich et al. (Reference Bleich, Barry and Gary-Webb203) demonstrated that when energy information was presented on beverages, SSB consumption decreased, while NNS beverage consumption increased. When assessing the impact of front-of-pack labels on beverage selection, Billich et al. (Reference Billich, Blake and Backholer199) found no statistically significant effect of ‘negative’ sugar labelling on the likelihood of a consumer choosing a NNS beverage. Similarly, a study assessing beverage selection when using SSB warning labels by VanEpps & Roberto(Reference VanEpps and Roberto216) found no increase in non-labelled beverage consumption, including NNS beverages.
Over half of the studies that assessed labelling did not examine the potential substitution effect of NNS for sugar. Of those that did, the majority showed neither a positive nor negative association between labelling interventions to reduce added sugar consumption and NNS consumption. Similarly to education campaigns, the small sample of studies cannot be used to conclusively support nor deny potential substitution effects of NNS for sugar in both the food supply and consumption.
Environmental interventions
Food environment interventions predominantly involved reducing the availability of SSB in schools(Reference Popkin and Hawkes6,Reference Bergallo, Castagnari and Fernández123,Reference Hsiao and Wang135,Reference Kirkpatrick, Raffoul and Maynard137,Reference Studdert, Flanders and Mello149,Reference Taber, Chriqui and Powell167,Reference Avery, Bostock and McCullough179,Reference Rahman, Jomaa and Kahale184,Reference Tipton187,Reference Vézina-Im, Beaulieu and Bélanger-Gravel189,Reference Levy, Friend and Wang190,Reference Bauhoff218–Reference Hovdenak, Bere and Stea241) , though interventions were also implemented in hospitals(Reference Blake, Peeters and Lancsar242,Reference Eneli, Oza-Frank and Grover243) , homes(Reference Albala, Ebbeling and Cifuentes244,Reference Ebbeling, Feldman and Chomitz245) , community centres(Reference Breeze, Womack and Pryce246), workplaces(Reference French, Harnack and Hannan247,Reference Yan, Pappas and Yuan248) and stores(Reference Cornelsen, Mytton and Adams131,Reference Hobin, Bollinger and Sacco209,Reference Gustafson, Ng and Jilcott Pitts249–Reference Ball, McNaughton and Le254) . Of the studies exploring this policy action (n 49), only twelve (Table 4) addressed the impact that environmental interventions aiming to reduce added sugar intake had on NNS consumption and levels in the food supply. In some regions (including New York City), beverages containing NNS are not permitted for sale in schools, which may limit the number of studies able to assess changes in NNS consumption/sales in response to sugar policy. Similarly, some studies included NNS beverages as a type of SSB. Consequently, assessing responses of NNS products to a policy to reduce added sugar consumption was not feasible(Reference Huang and Kiesel232). While some studies (n 4) found that NNS beverage consumption and sales increased in response to policy targeting added sugar(Reference Øverby, Klepp and Bere239,Reference Albala, Ebbeling and Cifuentes244–Reference Breeze, Womack and Pryce246) , the majority (n 6) found the opposite(Reference Cornelsen, Mytton and Adams131,Reference Whatley Blum, Davee and Beaudoin226,Reference Blake, Peeters and Lancsar242,Reference Eneli, Oza-Frank and Grover243,Reference Brimblecombe, Ferguson and Chatfield250,Reference Foster, Karpyn and Wojtanowski251) , and two saw no association(Reference Hovdenak, Bere and Stea241,Reference Ball, McNaughton and Le254) .
When free fruit was provided to children’s homes, Øverby et al. (Reference Øverby, Klepp and Bere239) found that SSB and NNS beverage consumption decreased and increased, respectively, despite neither beverage being directly targeted by the intervention. Comparatively, Hovdenak et al. (Reference Hovdenak, Bere and Stea241) found that supplying fruit to children in schools had no effect on either SSB or NNS beverage intake. Albala et al. (Reference Albala, Ebbeling and Cifuentes244) and Ebbeling et al. (Reference Ebbeling, Feldman and Chomitz245) found that when access to low-energy beverages in the home was improved, SSB intake decreased, while NNS beverage consumption increased. In a study of beverage availability and consumption in schools, Whatley Blum et al. (Reference Whatley Blum, Davee and Beaudoin226) observed that reduced availability of SSB was often paired with a reduction in NNS beverage availability. This resulted in decreased consumption of both beverages in the intervention cohort(Reference Whatley Blum, Davee and Beaudoin226). In a hospital setting, Eneli et al. (Reference Eneli, Oza-Frank and Grover243) found that a ban on SSB decreased NNS beverage sales significantly, despite these products being available after the intervention.
Influencing the prices of SSB and NNS beverages produced differing outcomes depending on the study. Blake et al. (Reference Blake, Peeters and Lancsar242) and Cornelsen et al. (Reference Cornelsen, Mytton and Adams131) found that increasing the price of SSB in a supermarket and restaurant, respectively, resulted in decreased sales of both SSB and NNS beverage sales, despite the price increase not extending to the NNS beverages. Comparatively, Breeze et al. (Reference Breeze, Womack and Pryce246) found that when the price for SSB was increased in community leisure centres, though SSB sales decreased by 27 %, sales of NNS beverages increased by the same magnitude. When implementing in-store promotions of NNS and water, Foster et al. (Reference Foster, Karpyn and Wojtanowski251) found a decrease in NNS beverage purchases from supermarket aisles, but an increase in those purchased at the checkout. Interestingly, Brimblecombe et al. (Reference Brimblecombe, Ferguson and Chatfield250) found that when subsidising bottled water and NNS beverages, sales of SSB increased, yet sales of subsidised NNS beverages decreased. In a study subsidising the price of fruits, vegetables, water and low-energy beverages, Ball et al. (Reference Ball, McNaughton and Le254) found no bearing of the intervention on NNS beverage sales.
Though most studies found that food environment interventions to reduce added sugar intake increased the sale and consumption of NNS beverages, the paucity and discordance of study results limit the dependability of this finding. Additionally, as the bulk of studies assessed interventions in the context of schools, results of these studies may not be generalisable to other settings or populations, particularly adults.
Reformulation
Reformulation can be used to reduce added sugar by modifying the ingredients in processed food(Reference Van Raaij, Hendriksen and Verhagen255). Often, this involves replacing added sugar with other sweeteners (including NNS) to maintain the level of sweetness and palatability. Reformulation activities aim to improve the energy and nutrient intakes of the population without consumers making major changes to their dietary patterns(Reference Van Raaij, Hendriksen and Verhagen255). At writing, no country has legislated a mandatory reformulation target for sugar, though voluntary reformulation policies and charters have been seen in countries including France, Switzerland and the UK(256,257) . Instead, reformulation targets are often a response to (or in pre-emption of) government policy to reduce added sugar in the food supply(Reference Durán Agúero, Noel and Arrivillaga63,Reference Figueiredo, Scapin and Fernandes68–Reference Grech, Kam and Gemming70,Reference Sylvetsky, Jin and Clark74,Reference Dunford, Taillie and Miles78,Reference Ha, Ha and Choi80,Reference Ha, Ha and Choi83,Reference Bolt-Evensen, Vik and Stea100) . Six studies discussed reformulation of added-sugar products and the effect on the food supply, including NNS use(Reference Popkin and Hawkes6,Reference Ortún, López-Valcárcel and Pinilla141,Reference Vandevijvere and Vanderlee150,Reference Hashem, He and MacGregor258–Reference Borges, Louzada and de Sá260) . Popkin & Hawkes(Reference Popkin and Hawkes6) discussed NNS as a potential replacement for sugar in processed food, and commented on the ambiguity of how to include these additives within future policy. Vandevijvere & Vanderlee(Reference Vandevijvere and Vanderlee150) suggested that labelling policies effectively stimulated reformulation by the food industry, and that despite a paucity of evidence, similar incentives are produced by taxes. Ortún et al. (Reference Ortún, López-Valcárcel and Pinilla141) speculated that policy actions to reduce added sugar, including taxes, encourage innovation by the food industry, including reformulation. Welsh et al. (Reference Welsh, Lundeen and Stein259) and Borges et al. (Reference Borges, Louzada and de Sá260) reported an increased effort of beverage industries to market ‘alternative beverages’ (including NNS beverages) as healthier alternatives for consumers. Though Hashem et al. (Reference Hashem, He and MacGregor258) conducted a meta-analysis which found that reformulation may decrease added sugar intake, how this may affect levels of NNS in the food supply was not examined.
The impact of non-nutritive sweeteners on diet quality, food choice and energy intake
Sixty-four articles focused on the effect of NNS consumption on dietary intakes. Compared with the other sections of this review, industry involvement was prevalent. Of the studies included in this section, approximately 50 % list either industry funding or a conflict of interest relating to the food industry. Of the studies explicitly funded by industry, four stated that their funders had no role in the design, analysis or presentation of the study, twenty-three stated only that the study was ‘supported’ by industry, and three stated direct involvement of industry in the study.
Dietary patterns, food, and nutrient consumption
A summary of articles (n 25) related to diet quality is shown as online Supplementary Table S3. Of these studies, fifteen were diet recalls, three were randomised controlled trials (RCT), three were food records, three were observational studies and one was a parallel study. The included articles assessed all three dietary exposure levels: dietary patterns, food groups, and nutrients.
-
(1) Dietary patterns
The effect of NNS consumption on overall dietary patterns was mixed. Some studies found that consumption of NNS was associated with a healthier dietary pattern, characterised as a higher Healthy Eating Index (HEI)-2005 score(Reference Drewnowski and Rehm115), an increased likelihood to have a ‘restrained’(Reference Elfhag, Tynelius and Rasmussen261) or ‘prudent’(Reference Drewnowski and Rehm115,Reference Piernas, Mendez and Ng262,Reference Duffey, Steffen and Van Horn263) eating pattern, or a higher Nutritional Quality Index (NQI) score (though this was only found in overweight and obese consumers)(Reference Rusmevichientong, Mitra and McEligot264). Moreover, Binkley & Golub(Reference Binkley and Golub265) found that consumers who purchased NNS beverages made healthier food choices generally. Other studies found that NNS consumption was associated with a poorer dietary pattern than non-consumption, including emotional eating (eating in response to negative emotions such as anxiety or loneliness)(Reference Elfhag, Tynelius and Rasmussen261), a lower HEI-2010 score (though only among high-socio-economic status consumers)(Reference An113) and a decreased likelihood of adhering to a prudent purchasing pattern(Reference Piernas, Mendez and Ng262). Piernas et al. (Reference Piernas, Mendez and Ng262) found that NNS consumers were more likely to follow a fast-food/ready-to-eat meal pattern.
-
(2) Food groups
Comparably, there was no clear consensus in the literature on the impact of NNS consumption and intake of specific food and nutrient groups. While some studies found that, when compared with non-consumers of NNS, consumers ate more fruit(Reference Drewnowski and Rehm115,Reference Piernas, Mendez and Ng262,Reference Gibson, Horgan and Francis266,Reference Sigman-Grant and Hsieh267) , vegetables(Reference Drewnowski and Rehm115,Reference Piernas, Mendez and Ng262,Reference Gibson, Horgan and Francis266,Reference Sigman-Grant and Hsieh267) , nuts(Reference Piernas, Mendez and Ng262) and legumes(Reference Drewnowski and Rehm115), the opposite was found in other studies(Reference Gibson, Horgan and Francis266,Reference Piernas, Tate and Wang268) . Moreover, Duffey & Popkin(Reference Duffey and Popkin269) found that consumers from the ‘vegetable cluster’ (a dietary pattern characterised by vegetable consumption) were less likely to drink diet drinks. Drewnowski & Rehm(Reference Drewnowski and Rehm115) found that NNS consumers had a higher intake of whole grains than non-consumers. An intervention by Piernas et al. (Reference Piernas, Tate and Wang268) found that when compared with a cohort encouraged to drink water, those encouraged to drink NNS beverages did not decrease carbohydrate-rich grains. Yet another study by Piernas et al. (Reference Piernas, Mendez and Ng262) found that consumers of NNS had a higher percentage of energy intake from ready-to-eat cereals.
While Binkley & Golub(Reference Binkley and Golub265) found that dairy product consumption in all product categories declined with increased NNS beverage consumption, others found that NNS consumers had a higher intake of low-fat dairy products(Reference Drewnowski and Rehm115,Reference Binkley and Golub265,Reference Brunkwall, Almgren and Hellstrand270) and dairy products overall(Reference Grech, Kam and Gemming70) than non-consumers. Fowler et al. (Reference Fowler, Williams and Resendez40) found that specifically milk consumption was lower among NNS consumers, though Ca intake was similar. Comparatively, Gibson et al. (Reference Gibson, Horgan and Francis266) found no difference in milk consumption based on beverage consumption patterns. They also observed that consumers of NNS ate more fish than SSB consumers(Reference Gibson, Horgan and Francis266), though less than those who consumed no sweetened beverages at all(Reference Gibson, Horgan and Francis266). Compared with non-consumers of NNS, consumers were found to have a higher oil intake(Reference Drewnowski and Rehm115). Additionally, An(Reference An113) found that, overall, those consuming NNS had a higher energy intake from discretionary foods.
NNS beverage consumers were found to eat more snacks(Reference Bleich, Wolfson and Vine99,Reference Piernas, Mendez and Ng262,Reference Binkley and Golub265) and desserts than other beverage consumer clusters(Reference Piernas, Mendez and Ng262), with Binkley & Golub(Reference Binkley and Golub265) suggesting that snacks offset the lower energy of diet beverages. Their study found that NNS consumers were more willing and likely to buy reduced-fat, -sugar and -energy versions of foods than other consumer groups, including milk, ice cream, frozen dinners and salad dressing(Reference Binkley and Golub265,Reference Brunkwall, Almgren and Hellstrand270) . A study by Bleich et al. (Reference Bleich, Wolfson and Vine99) in obese adults found that this was particularly true for salty snacks. However, Piernas et al. (Reference Piernas, Tate and Wang268) found that NNS consumers actually decreased dessert intake. Sigman-Grant et al. (Reference Sigman-Grant and Hsieh267) reported that those that consumed NNS yoghurt, jelly and desserts consumed more of these products than those who consumed the full-sugar versions.
-
(3) Nutrients
NNS consumers were found to consume less carbohydrate generally(Reference Grech, Kam and Gemming70,Reference Bellisle, Altenburg de Assis and Fieux114,Reference Fantino, Fantino and Matray271–Reference Ratliff, Riedt and Fulgoni275) and less added sugar(Reference Grech, Kam and Gemming70,Reference Bellisle, Altenburg de Assis and Fieux114,Reference Drewnowski and Rehm115,Reference Gibson, Horgan and Francis266,Reference Sigman-Grant and Hsieh267,Reference Fantino, Fantino and Matray271–Reference Markey, Le Jeune and Lovegrove273,Reference Ratliff, Riedt and Fulgoni275) than non-consumers, though Gibson et al. (Reference Gibson, Horgan and Francis266) suggested that this decrease in sugar is owing to the decreased contribution from beverages rather than from the diet overall. Comparatively, Sylvetsky et al. (Reference Sylvetsky, Figueroa and Zimmerman276) found that children who consumed NNS beverages had higher intakes of added sugar, total sugar and carbohydrates (when compared with those who drank water). In habitual consumers of NNS, consumption of protein was lower from vegetable sources(Reference Bellisle, Altenburg de Assis and Fieux114) yet higher from animal products(Reference Bellisle, Altenburg de Assis and Fieux114,Reference Drewnowski and Rehm115) . Other studies found an increase in protein consumption overall compared with non-consumers(Reference Fowler, Williams and Resendez40,Reference Raben, Vasilaras and Møller49,Reference Grech, Kam and Gemming70,Reference Bellisle, Altenburg de Assis and Fieux114,Reference Gibson, Horgan and Francis266,Reference Markey, Le Jeune and Lovegrove273,Reference Piernas, Ng and Mendez277) . Compared with non-consumers of NNS, consumers were found to have a higher intake of saturated fats(Reference Fowler, Williams and Resendez40,Reference Drewnowski and Rehm115,Reference Leahy, Ratliff and Riedt272,Reference Piernas, Ng and Mendez277) and a higher total fat consumption as a percentage of energy intake(Reference Fowler, Williams and Resendez40,Reference Markey, Le Jeune and Lovegrove273) . However, some studies found that NNS consumers consumed less energy from discretionary fats(Reference Drewnowski and Rehm115,Reference Sigman-Grant and Hsieh267,Reference Brunkwall, Almgren and Hellstrand270) and alcohols(Reference Raben, Vasilaras and Møller49). Generally, studies found that consumers of NNS had higher intakes of Na(Reference Grech, Kam and Gemming70,Reference Drewnowski and Rehm115,Reference Winther, Aasbrenn and Farup278) . Additionally, Bellisle et al. (Reference Bellisle, Altenburg de Assis and Fieux114) found that NNS consumers ingested higher amounts of cholesterol than non-consumers. Most studies found no difference in micronutrients between NNS consumers and non-consumers(Reference Bellisle, Altenburg de Assis and Fieux114,Reference Gibson, Horgan and Francis266,Reference Sigman-Grant and Hsieh267,Reference Fantino, Fantino and Matray271) , though Winther et al. (Reference Winther, Aasbrenn and Farup278) found that intake of NNS was associated with a reduced intake of some vitamins.
Energy intake: (1) long-term studies
Long-term studies (those that assessed intake across more than 1 d) that investigated NNS consumption and energy intake (n 23) are shown as online Supplementary Table S4. Generally, NNS beverage consumption was associated with lower overall energy intake, ranging from a reduction of 76 kcal to 781 kcal (318 kJ to 3268 kJ) in average daily energy intake(Reference Fowler, Williams and Resendez40,Reference Raben, Vasilaras and Møller49,Reference An113,Reference Bellisle, Altenburg de Assis and Fieux114,Reference Duffey, Steffen and Van Horn263,Reference Binkley and Golub265–Reference Sigman-Grant and Hsieh267,Reference Brunkwall, Almgren and Hellstrand270,Reference Sørensen, Vasilaras and Astrup274,Reference Higgins and Mattes279–Reference Reid, Hammersley and Hill281) . In some studies, SSB were included as dietary supplements, and their energy was included in daily totals, which may exaggerate these differences(Reference Sørensen, Vasilaras and Astrup274). Bleich et al. (Reference Bleich, Wolfson and Vine99) found that energy intake from solid food was higher in NNS consumers than those that drank SSB, though only in overweight and obese adults. Healthy-weight populations consuming NNS had a lower energy intake than non-consumers(Reference Bleich, Wolfson and Vine99). Gibson et al. (Reference Gibson, Horgan and Francis266) found that NNS consumers had a lower intake of energy from food, a difference of approximately 40–50 % when compared with SSB consumers. However, Winther et al. (Reference Winther, Aasbrenn and Farup278) and Piernas et al. (Reference Piernas, Mendez and Ng262,Reference Piernas, Ng and Mendez277) found the opposite, with higher energy intake associated with NNS consumption. Similarly, a study by An(Reference An113) found that NNS beverages were associated with the second largest increase in energy intake from discretionary foods (second to coffee) among beverage categories. This association was strongest among obese adults(Reference An113). Yet other studies found no clear association between NNS and long-term energy intake(Reference Grech, Kam and Gemming70,Reference Gibson, Horgan and Francis266,Reference Markey, Le Jeune and Lovegrove273,Reference Sylvetsky, Jin and Mathieu282,Reference Tate, Turner-McGrievy and Lyons283) .
Compensatory effects of NNS were found in multiple studies(Reference Grech, Kam and Gemming70,Reference An113,Reference Markey, Le Jeune and Lovegrove273) . This compensatory effect was most evident in high-income and -educated groups, which (as highlighted in the previous section) are higher consumers of NNS beverages than their low-socio-economic-status counterparts(Reference An113). Leahy et al. (Reference Leahy, Ratliff and Riedt272) found that consumers of NNS beverages had a comparative energy intake to water consumers, while Stookey et al. (Reference Stookey, Constant and Gardner284) found that water consumption greatly reduced dietary energy intake over time.
The majority of these studies employed a dietary recall method. Whilst the most pragmatic method for this type of research, recalls are associated with desirability bias (in which participants may be dishonest in their responses to impress researchers), unreliability errors and measurement errors, which may affect results(Reference Gibson, Charrondiere and Bell285). Despite these limitations, dietary recalls are often used in nutrition research as they can be culturally sensitive, do not require high levels of literacy, and provide quantitative data(Reference Gibson, Charrondiere and Bell285,Reference Gibson286) . Additionally, evidence suggests that participants tend to overestimate how healthy their diet is, subsequently underestimating energy, Na, sugar and fat(Reference Gibson286).
Energy intake: (2) short-term studies
Thirty-four primary studies assessed the effect of a pre-load of NNS on subsequent food intake in a post-intervention meal (online Supplementary Table S5). Six studies found an increase in food intake(Reference Birch, McPhee and Sullivan287–Reference Tey, Salleh and Henry292), twenty-four saw no significant difference(Reference Fantino, Fantino and Matray271,Reference Anderson, Saravis and Schacher293–Reference Chern and Tan315) and four studies found a decrease in food intake(Reference Rogers, Pleming and Blundell316–Reference Van Wymelbeke, Beridot-Therond and de La Gueronniere319). Most participants were either ‘healthy’ or of a ‘normal weight’ (generally referring to a BMI of 18–25 kg/m2) despite overweight and obese individuals being the primary consumers of NNS (as described previously). It is interesting to note that of the six studies that found an increase in food intake after a NNS preload, three were funded by the sugar industry(Reference Gadah, Brunstrom and Rogers288,Reference Lavin, French and Read290,Reference Rogers and Blundell291) , and a fourth was funded by a now fragmented multi-national corporation(Reference Birch, McPhee and Sullivan287). Comparatively, three of the four studies that found a decrease in food intake were published by the same author, who has received direct and indirect funding from organisations including Coca-Cola, Sugar Nutrition and The International Sweeteners Association(Reference Rogers, Pleming and Blundell316–Reference Rogers, Burley and Alikhanizadeh318). Additionally, these studies administered the NNS in tablet form, mitigating the potentially important effects of sweet taste or satiety of the preload. Overall, of the thirty-four studies that assessed NNS preloads and subsequent food intake, nineteen (or over 50 %) were either directly funded by, received products from, or had authors who had connections with industry(Reference Fantino, Fantino and Matray271,Reference Birch, McPhee and Sullivan287,Reference Gadah, Brunstrom and Rogers288,Reference Lavin, French and Read290,Reference Rogers and Blundell291,Reference Anderson, Saravis and Schacher293,Reference Beridot-Therond, Arts and Fantino295–Reference Black, Tanaka and Leiter297,Reference Drewnowski, Massien and Louis-Sylvestre301,Reference Mattes304–Reference Rogers, Carlyle and Hill306,Reference Rolls, Kim and Fedoroff308–Reference Ryan-Harshman, Leiter and Anderson310,Reference Rogers, Pleming and Blundell316–Reference Rogers, Burley and Alikhanizadeh318) .
Fluids were used as the pre-load almost exclusively throughout the studies. NNS beverages may be easier to manipulate in experimental studies, as NNS only need to impart sweetness in a beverage, as opposed to texture and other sensory variables that may be affected by the removal of sugar in other products. For most short-term studies assessing energy intake, consumption behaviour was measured under experimental conditions rather than in free-living populations. This may limit the applicability of the findings in real-world dietary patterns and behaviours(Reference Penders, Wolters and Feskens320). Often, food intake was only measured over the course of a single meal, preventing the evaluation of compensatory effects in the long term. In addition, participants were often blinded to the use of NNS in their samples. In a real-world context, awareness of added sugar and energy content of a food or drink may contribute to compensation.
Discussion
The aim of the present review was to provide an overview of current NNS food supply and consumption patterns and to evaluate added sugar-reduction policies and their impact on NNS and the impact of NNS on food choice, energy intake and diet quality.
Assessment of the different types of sweeteners in the global food supply, and quantified amounts of sweeteners in products, was limited. It is difficult to measure direct quantities of NNS in the food supply, as many countries do not require the volume of NNS in a product to be declared on the label, only that they are an ingredient(Reference Baker-Smith, de Ferranti and Cochran321). Despite comprehensive cross-sectional analysis of which products contain NNS, the trends of NNS use in the food supply are under-researched. There is a general consensus that the number of products containing NNS are increasing(Reference Garavaglia, Garcia and Zapata69,Reference Grech, Kam and Gemming70,Reference Le Donne, Mistura and Goscinny72,Reference Lee, Do and Lee85,Reference Bolt-Evensen, Vik and Stea100) , which may contribute to an overall increased level in the food supply. However, no studies have measured the volume change of NNS in the food supply over time. This is a significant gap in the literature.
Most studies used cross-sectional study designs, thus demonstrating NNS consumption in a snapshot of time only. Due to the numerous different populations and study parameters, comparing these studies to derive consumption trends is not possible. Outside the USA, exploration of the consumption trends of NNS is limited. In many countries, national diet surveys are sporadic, and do not have up-to-date information on current rates of consumption. This is especially important for NNS, as there is the potential for a rapid increase in consumption given the accumulative legislative actions (particularly SSB taxes) to reduce added sugar in the food supply. Further research is needed to assess contemporary trends and patterns of NNS consumption globally.
High education/socio-economic status may be associated with NNS consumption as these consumers are typically more health-focused, and may desire low-energy alternatives(Reference Wardle and Steptoe322). Additionally, women may be more likely to consume NNS than men, as a larger proportion of ‘diet’ or ‘lite’ products are marketed to this group(Reference Durán Agúero, Noel and Arrivillaga63). Women are also typically more likely to be on a ‘diet’ than men, thus may be more likely to choose lower-energy products(Reference Kiefer, Rathmanner and Kunze323). One contradiction throughout the studies is that those who are overweight/obese are more likely to consume NNS than those with a healthy BMI. This could be for many reasons. First, these populations may be more likely to be the target of diet campaigns (NNS are prevalent in diet foods)(Reference Yang324). Second, the results may be affected by reverse causality; those who are overweight aim to reduce their energy intake by consuming diet/low-energy food, rather than this food contributing to obesity(Reference Winther, Aasbrenn and Farup278,Reference Gardner325,Reference Visek, Blake and Otterbein326) . Third, individuals may use the consumption of NNS as a rationale to make unhealthy food choices or to consume larger portion sizes as these products have less energy than their full-sugar counterparts(Reference Bleich, Wolfson and Vine99,Reference Visek, Blake and Otterbein326,Reference Riobó Serván, Sierra Poyatos and Soldo Rodríguez327) .
While a broad range of policy actions targeting added sugar consumption was discussed, the underlying political factors that shape these policies, particularly in terms of the lack of holistic policy actions implemented globally, were not explored. Though some policy actions focused on ‘discretionary’ food, most policy actions targeted sugar as a nutrient, as opposed to suggesting a reduction in ultra-processed foods generally or promoting whole food consumption. Though broader national food policies may comprise policy actions that target different parts of the food supply, the results of this study demonstrate that the majority are nutrient-focused. As public health policy has an impact on the food supply and consequently consumption patterns, understanding why particular types of policy actions are promoted and implemented over others is imperative.
In general, the potential impact of these policy actions on NNS was not widely considered. The studies that did assess this outcome had mixed results. Though taxation seemingly increased NNS in the food supply in most studies, the opposite was true in others. Comparatively, education campaigns to reduce added sugar consumption were associated with a decrease in NNS purchases and intakes; yet others find the opposite, or no effect. Inconsistent associations were found for education labelling and food environment interventions. However, given the paucity of studies that explored these impacts, the conclusions that can be drawn are limited. While most studies were experimental in nature, the types of methods used, sample sizes and time periods analysed varied greatly. Furthermore, the impact of each policy action on NNS consumption can only be described as an association, not causative, as other factors may have made an impact on consumption rates. It is important to note that based on the available evidence it is not possible to suggest that one single policy action is the sole trigger for a change in added sugar or NNS consumption. Rather, an interaction between policy actions is likely to be the cause. Further research is needed to demonstrate how policy actions may have an impact on levels of NNS in the food supply, and to what magnitude.
Compared with the other sections of this review, industry involvement was prevalent in studies assessing the impact of NNS consumption on dietary intakes. Of the studies included in this section, approximately 50 % list either industry funding or a conflict of interest relating to the food industry. This involvement is a cause for concern, as previous studies suggest that when research is sponsored by the sweetener industry, both results and conclusions are more likely to be favourable towards NNS(Reference Mandrioli, Kearns and Bero328). Comparatively, when studies were funded or supported by the sugar industry, the reverse was found(Reference Mandrioli, Kearns and Bero328). The bias found in industry-sponsored studies is a well-documented issue in nutrition research, and may potentially undermine the results of the present review(Reference Mandrioli, Kearns and Bero328–Reference Hennessy, Cullerton and Baker331). Greater research funding from governments and other funding agencies is needed to avoid a reliance on industry-funded analyses in the case of NNS.
The reviewed cross-sectional studies of the impact of NNS intake on diet quality were only able to show a correlative effect, not causative outcomes. How products containing NNS may create substitution effects in the diet, i.e. displacing one food for another, was not explored. This may be due to the limitations of the data sources used; large epidemiological studies, while useful for exploring the associations and potential impacts of NNS on overall dietary balance, do not explore consumer behaviour in terms of food choice and direct substitution. Sample data were often limited, encompassing only a few days of intake, which may not be representative of usual consumption patterns. In addition, most studies used a self-administered diet questionnaire to obtain data. Participant bias, recall bias and social-desirability bias may make an impact on the validity of these results(Reference Gibson, Charrondiere and Bell285,Reference Archer, Hand and Blair332) . An additional limitation of food composition databases is their inability to accurately capture all NNS in the food supply; thus consumers may be assigned to clusters incorrectly. The metric used to determine the healthiness of a diet varied between studies, including HEI scores (including multiple iterations), Nutritional Quality Index (NQI) scores and the defining of food pattern clusters (for example, vegetable cluster, breakfast cluster). Additionally, the clustering of participants varied throughout the literature – while some participants were clustered as binary ‘users’ or ‘non-users’, others were further classified by dietary pattern (‘prudent’ or ‘Western’). Given these limitations, developing and evaluating biomarkers for NNS intake would be a useful tool to monitor NNS consumption in the future.
In studies that assessed dietary patterns, there was no differentiation between types of NNS. Most studies assessed dietary patterns in relation to the consumption of NNS beverages, as opposed to all products containing NNS. This could be for many reasons. Beverages are the primary source of NNS in most diets(Reference Sylvetsky, Jin and Clark74). Additionally, they are a well-known source of NNS to consumers, who may be more likely to recall them during FFQ or dietary interviews as opposed to other NNS-containing items, including sauces and dairy products. This is a considerable limitation of the literature, as NNS are becoming prevalent in food sources including yoghurts and desserts and are found across a wide variety of products in the food supply.
Overall, while food regulators and epidemiologists often focus predominantly on the immediate safety and toxicological aspects of NNS as opposed to the impact on dietary patterns, the progression of these additives in the food supply may be a powerful marker of the reductionist approach to public health that currently prevails in policy making. Consumer behaviour and food choice are greatly influenced by the food environment and food supply, which have been shaped by the current reductionist approach to public health. From the findings of the present review, questions can be raised regarding the fundamental effectiveness of current policy approaches at tackling the underlying causes of chronic disease. While they may reduce added sugar intake, whether these policies reduce the consumption of ultra-processed food, improve diet quality and improve population health is unclear. Fundamentally, reductionist policy actions can be seen as a marker for the ‘business-as-usual approach’ to public health and safety, and therefore do not target the underlying issues with our current global foods system.
Limitations and future directions
The present review was limited by the exclusion of studies published in languages other than English, particularly as countries in South and Latin America have been leaders in policy actions aiming to reduce added sugar reduction. Additionally, there is the potential for demonstrations of the relationship between policy to reduce added sugar consumption and increases in NNS in the food supply from non-academic sources including industry documents or government reports that have not been included in the present review.
The present review highlighted many areas for future research. While a range of policy actions has been implemented to reduce added sugar intake, the potential impact of the policies on levels of NNS in the food supply is unclear and warrants further exploration. This includes a lack of research on the different effects of reductionist or holistic policies, as well as those that target either nutrients, food, dietary pattern of food systems, and on combinations of different policy actions on NNS in the food supply. The vast majority of studies included in this review explored high-income countries, despite the potential for changes in the consumption of ultra-processed food in middle-low income countries (particularly in response to the nutrition transition)(Reference Baker and Friel333,Reference Baker and Friel334) . Overall, there is some evidence to indicate that consumption of NNS is increasing in some contexts, though a global analysis of consumption trends is proposed. NNS are widely available in the food supply, especially in beverages, dairy products and confectionery. However, trends in the reformulation of different product categories, and differences between geographical locations and economy-income levels require further study. Research examining how the increased availability of low-sugar discretionary products affects global diets is limited, particularly potential substitution effects of low-sugar beverages for water and/or milk from the diet.
Conclusion
A range of policy actions has been implemented to reduce added sugar intake globally. The potential impact of these policy actions on NNS-related food supply changes and consumption has not been satisfactorily determined. Most of these policy actions were downstream in nature, potentially encouraging reformulation of individual food products as opposed to improving food systems or dietary patterns. The underlying political factors that shape these policies, and the implementation of reductionist policy actions, have not been explored. NNS were found in an extensive range of products across the food supply, and consumption of NNS has increased over the last two decades in some countries. The literature exploring how NNS consumption has an impact on overall dietary balance was mixed and potentially influenced by industry-funded research. The potential substitution effect of reformulated, ultra-processed food containing NNS for nutritious whole foods was unclear. It is therefore important for future research to determine why nutrient-focused policy actions are championed over others, what their impact is on the food supply and subsequently, how consumption and dietary intakes are affected.
Acknowledgements
The present review was funded by an Australian Government Research Training Program.
The authors’ responsibilities were as follows: M. A. L. conceived the original topic for investigation and its aims. All authors were responsible for the conceptualisation of the paper; C. R. was responsible for the literature search, data analysis and drafted the manuscript; K. S. was also responsible for literature screening, M. A. L., C. G., K. S. and P. B. provided a critical review of the paper. All authors contributed to and agreed on the final version of the manuscript.
There are no conflicts of interest.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S0954422420000268