A long time after the American doctors signaled the existence, in certain regions of South American, of diseases characterized by skin and mucous ulcerations, another great confusion reigned in the chapter of the ulcerative diseases (…) There are no doubts that the American leishmaniasis was frequently encompassed with other diseases, under the names of buba or bouba, bouton of Bahia and Bauru’s ulcer, in Brazil; under the name of uta and espundia in Peru; of pian-bois in French Guiana; of forest yaws in English Guiana, and boschyaws in Dutch Guiana.Footnote 1
In 1917, the French parasitologist Charles Louis Alphonse Laveran published Leishmanioses. Bouton d’Orient, kala-azar, Leishmanioses americaine, [Leishmaniasis. Oriental sore, calazar and American leishmaniasis] as the epilogue of a long professional trajectory dedicated not just to the study, but also to the development of the category of tropical diseases, or exotiques, as the Frenchman preferred. His aim was to gather and systematise a great number of works published about this thematic in the last 14 years (1903–17), that made of his treatise a great compendium about the state of the art of the question of the leishmaniasis.Footnote 2
In the first part of his book, Laveran discoursed about the genesis of the concept of leishmaniasis. Created in 1906, the word was as a creative solution, consensually accepted by several renowned names of tropical medicine, on the matter of trying to answer a curious scientific finding: three diseases (or clinical manifestations), with extremely different symptomatologies and clinical courses and, apparently, without any relationship with each other, seemed to be caused by morphologically indistinguishable protozoa. That fact contradicted the principle of a unique aetiological agent for each disease, a belief much appreciated by pasteurians. Those circumstances were strongly influenced by significant developments in the fields of aetiology and parasitology associated with the germ theory of infectious diseases, based on the theory of the vector-insect, a primordial axis of the new specialty, the Mansonian tropical medicine.Footnote 3
The main initial hypothesis focusing on the clarification of the reasons by which identical protozoa caused absolutely different diseases, suggested the possibility of differentiated biological cycles in the organisms of the intermediary hosts. However, this hypothesis was based on another undiscovered fact: was there an intermediary host? By analogy with other tropical diseases, the hosts could be flies, mosquitoes, bedbugs, fleas or other insects. Another hypothesis attempted to associate the variety of manifestations of the disease to different environments and climates, which could be an element of interference in the action of the pathogen in the human host. Yet, how could the relationship between environments and different clinical manifestations of leishmaniasis be proved? These were some of the questions that were central to the research about this group of diseases in the beginning of the twentieth century, an epoch marked by the increasing establishment of networks of research among scientific institutions recently created in different places of the world, giving concreteness to the programs of microbiology and tropical medicine.
When Laveran approached the problematic related to American leishmaniasis, he recognised the active role of members of South American medical communities in the processes of proposition and validation of the statements about the American disease since 1909, when the first parasitological diagnoses of the mucous form, at that time still perceived as an anomaly, were made in rural areas of the São Paulo state, in the Brazilian Southeast region. That was the first time clinical manifestations connected to parasites of genus Leishmania were found in the Western Hemisphere, increasing considerably the geographical range of the disease, and, also, initiating a new phase of research about this group of diseases. The malady found in the Brazilian Southeast had a preference for invading the mucous parts of the body, especially the nose and the mouth. This newfound illness also showed more extensive and aggressive clinical progresses, compared to the ones observed in the cutaneous leishmaniasis of the Old World, which could last for more than 30 years.
From then on, some members of the South American medical communities defended that the form of leishmaniasis found in São Paulo was not an anomaly. Instead, they claimed it was a particular, and even autochthonous, disease of that region, possibly caused by a particular protozoan, Leishmania braziliensis. Thereby, they opposed their new findings, in all dimensions (clinical description, vectors and epidemiology), to the previously known cutaneous leishmaniasis. The earlier-discovered disease, also known as Oriental Sore, had a clinical course considered benign, with a natural tendency to spontaneous cure in approximately 1 year. A condition accepted, ever since the twentieth century, as an almost inevitable souvenir for European travellers who would venture to endemical regions in Northern Africa, the Mediterranean and certain territories of Asia, such as Mesopotamia, Tunisia and, above all, India.Footnote 4
When tracking back the studies about leishmaniasis in the South American region and mapping the medical network formed around this group of diseases, it is possible to observe a synergistic game between local and global that defies the opposition of central and peripheral contexts. Generally, for other diseases, the microbiologic dynamics revolved around searching for the specific pathogenic agent that would explain the aetiology of a certain clinical case already well known or recently identified. In the case of leishmaniasis, especially the Americans, the dynamics was different: several clinical frames without any kind of relation amongst them, having countless regional denominations (uta, espundia, Bauru’s ulcer, Bahia’s button, pian-bois, etc.), were assigned to morphologically undifferentiated protozoa when parasitological exams revealed them as the causal agents. This gave an important role to the local knowledge in the specific environments where the disease arose in endemic or epidemic character.
In this article, my goal is to analyse how researchers situated in different countries of South America introduced themselves in the processes of construction and globalisation of the paradigm of tropical medicine, through original investigations about the leishmaniasis found in this region. At that time these actors were progressively successful in the conception and validation of their scientific enunciations, in the manner that successive original works were produced in this regional context and published in scientific periodicals of renown, especially in the Bulletin de la Société de Patologie Exotique [Bulletin of the Society of Exotic Pathology]. These ground-breaking reports played a role as a catalyser for the worldwide recognition and diffusion of the proper thematic of this medical field, a situation at the bottom of what Kapil Raj considers a ‘reciprocal, although asymmetrical, process of circulation and negotiation’.Footnote 5
The meanings of tropical medicine in South America and the first diagnoses of leishmaniasis in the region
The microbial theory formulated during the 1860s by Louis Pasteur, Robert Koch and many other investigators from Europe and other parts of the world, opened a new and promising horizon of possibilities for the physicians and researchers (increasingly numerous) who adopted its rules and practices, both in laboratory and in clinical medicine and other connected spheres, such as clinical pathology and pathological anatomy. Thereupon, the morbid manifestations turned out to be considered the result of interactions between microorganisms and human and other vertebrate organisms, opening (to use here the consecrated expression by Paul de Kruif) a true ‘hunt’ for the germs that were suspected to be the aetiological agents of human, animal and vegetal diseases.Footnote 6
The non-European regions, especially those situated in warm and humid climates, became an attractive destiny for young physicians eager to contribute significantly, or even gloriously, to the construction of the new medicine, which was imposing itself. Many of them were not able to perform it in their original countries, because of a lack of professional opportunities or for understanding that the more challenging pathologies to the Western biomedical science were overseas.Footnote 7 The medical-scientific relevance of the tropics increased in synchrony with the advance European imperialism, as well as with the intensification of the contacts between colonised and colonisers and the greater spatial interiorisation of these enterprises. The diseases of these regions, modified in their manifestations and epidemiology by the interventions in their original environments, became great threats to the projects of conquest and occupation of Africa, Asia and the Americas. The imperial metropolises started to send researchers and began to install laboratories in the areas in which they wanted to control or occupy, searching to improve as much as possible not just the profitability, but also the feasibility of the colonialist enterprises.Footnote 8
At the turn of the twentieth century, we can observe a dynamic period of studies and discoveries made by these physicians sent by different European metropolises to the colonial world; such period is frequently associated to the birth of the tropical medicine and of its triumphalist mythology. Institutions connected with the British Crown sent dozens of physicians to the most distant corners of its naval empire. France, after the foundation of the Pasteur Institute in Paris, in 1887, started to establish affiliated societies with it (Saigon, 1891; Tunis, 1893; Argel, 1894; Nah Trang, 1895) and commenced sending military physicians to its colonies. Germany, Belgium, Portugal and Italy also dispatched physician staff to their domains. Robert Koch, director of the Institut für Infektionskrankheiten [Institute for Infectious Diseases], already hallowed by his studies of the tuberculosis bacillus and the elaboration of the postulates of Koch, made successive voyages to Africa and Asia, between 1896 and 1907, with the intention of studying diseases considered obstacles to the German projects in these grounds, for example, malaria, cattle diseases and the sleeping sickness.Footnote 9
At that point, South America was a singular zone for biomedical studies and research. Most of the countries of the region were already free from the colonial yoke, creating spaces and possibilities for the organisation of national medical communities (with varied degrees of autonomy) in charge of initiating studies regarding the scientific issues that involved their local realities. These communities were composed by native and foreign researchers, who considered the non-European world, in particular regions with warm and humid climate, as privileged places for the accomplishment of original work in microbiology and parasitology. On the other hand, South American scientists went frequently to European metropolises for graduate study level or specialised studies, resulting in a multidirectional flux of researchers essential for biomedical research in the region, for the creation of new institutions and, especially, for the construction of knowledge about the American leishmaniasis.Footnote 10
Contrarily to what happened in the European colonial domains, the main concern of the South American tropicalists was not to assure the permanence of the coloniser in the region. Instead, their main task aimed to insure the health of their countrymen, in conjunction with the implementation of projects of modernisation of their countries, such as railroads, hydroelectrical dams, gatherer and agricultural enterprises, etc. Those projects were many times threatened by tropical diseases that ranged, endemically or epidemically, in large regions of the hinterland of the countries of the continent.Footnote 11
Aware of the epistemological news of the emerging field of tropical medicine, the medical regional elites acknowledged, with some perplexity, the resignifications in the comprehension of diseases that would be encompassed as leishmaniasis. Although they did not yet appear as a relevant scientific problem for the region, since 1895 there had been well-known reports about the existence of the cutaneous form in the region. That even led Patrick Manson, aforetime in the first edition of Tropical Diseases – A Manual of Diseases of Warms Climates (1898), to question the geographical relevance of the denomination Oriental sore, considering the disease had been considered ‘common in Bahia, Brazil’.Footnote 12
In Paris, on a personal enterprise of Alphonse Laveran, who invested a great part of the sum received for the Nobel Prize of 1907 won for the assemblage of his work on trypanosomes, was founded the Société de Pathologie Exotique [Society of Exotic Pathology], as a special section of the Pasteur Institute of Paris. According to Laveran, his ambition was to promote a better relationship between the fields of microbiology, protozoology and medical entomology; whose synergies were potentialised by the great extent of the French colonial empire and also by the development and increase of speed of transportation facilities, allowing a quicker dissemination of diseases.Footnote 13
Laveran and the zoologist Felix Mesnil, cofounder of the Societé, besides having strong connections with the branches of the Pasteur Institute founded in French colonial regions, especially those of Algeria and Tunisia, endeavoured gather a real army of collaborators from every part of the world, giving them the position of correspondent partners and opening the possibility for them to publish original work in the Bulletin de la Société de Pathologie Exotique. With ten annual editions, this periodical became fast one of the main sounding boards of tropical medicine, where leishmaniasis appeared frequently as a relevant thematic. Particularly after 1909, when the first reports on South American leishmaniasis showed that they were, according to Laveran himself, extremely differentiated from that known as Oriental sore, both in their epidemiology and in the ‘nature of the ulcerations more tepid, with a longer duration and a healing more difficult, that were produced by it’.Footnote 14
In fact, manifestations of the disease, later classified as mucous leishmaniasis, were already known in the hinterland of the Brazilian state of São Paulo as early as the end of the nineteenth century, when Achilles Breda, a physician of Padua, Italy, published his observations about sixteen Italians who had worked in the region and went back to their country of origin with a disease, which he diagnosed as ‘Brazilian bouba’.Footnote 15 Nevertheless, it was just after 1907, when an outbreak of ulcerations with ‘bizarre clinical aspects’ and ‘undefined etiological nature’ fell upon workers constructing the Northwest Brazil railroad in deep forest area, that the disease drew the attention of the local medical authorities: workers in search of assistance went to the Santa Casa de Misericórdia de São Paulo [Holy House of Mercifulness], in the capital of the state, distant more than 400 kilometres from the city of Bauru, where they had contact with the disease. Initially, there were ‘sparse’ cases, but soon they became so frequent that ‘it was rare the day when a new sick didn’t appear’.Footnote 16
Due to its ‘frequency and treatment difficult’, these ulcerations, popularly called Úlceras do Bauru [Bauru’s ulcerations], were considered by Adolpho Lutz, director of the Bacteriological Institute of São Paulo, the fourth biggest problem of public health in the state, following malaria, goitre and hookworm. Lutz even made an expedition, jointly with Emilio Ribas, director of the Sanitary Service of São Paulo, and Octavio Miranda, head of the Sanitary Commission of Campinas, to the region where the disease raged to study it. In most cases, there were just cutaneous wounds, but in a small percentage of the patients there were also damages to the mucous membranes, in particular of the nasal and pharyngeal cavities.Footnote 17
According to an editorial in the sixth number of the Jornal Médico de São Paulo [Medical Journal of São Paulo], there was already ‘a certain atmosphere of skepticism’ in the medical medium of the state, when the newspaper O Estado de São Paulo [The São Paulo State] published, on 30 March 1909, that the dermatologist Adolpho Carlos Lindenberg, research assistant of the Bacteriological Institute of São Paulo and dermatologist of the Santa Casa de Misericórdia de São Paulo, had found ‘the microbe that he considered as the causer of this affection until now unknown’. It was a protozoan which, ‘by its form and dimension’, was similar to the ‘microbe of the Oriental sore’, a finding which was confirmed, in the next day, by Antônio Carini and Ulysses Paranhos, respectively, director and research assistant of the Pasteur Institute of São Paulo.Footnote 18
This parasitological finding was a great scientific victory for those doctors. They quickly published preliminary communications of their results on the account of not losing the primacy of discovery. After all, the leishmaniases were standing out in tropical medicine, and, for the first time, one of its parasites had been diagnosed in the Western Hemisphere. In the articles, printed in the form of a series both in the Jornal Médico de São Paulo and the Bulletin de la Société de Pathologie Exotique, these researchers had no doubts, despite the larger and more aggressive clinical development of the disease studied in São Paulo, in associating it with the Oriental sore and its causal agent, Leishmania tropica, in the same manner of other North American and European researchers, such as James Wright, Felix Mesnil and Maurice Nicolle. It is worth mentioning, however, that in the French periodical, none of the authors made any reference to the mucous wounds, in contrast with the Brazilian publication. This fact demonstrated the existence of doubts about the possibility of more than one morbid manifestation in the popular denomination of ‘Bauru’s ulcerations’.Footnote 19
In the same year in which the São Paulo researchers linked Bauru’s ulcerations and leishmaniasis, the physician in the position of general inspector of French Guiana, Charles Théodore Grall, and L. Touin, director of the Health Service of Guiana, sent to the zoologist Felix Mesnil, of the Pasteur Institute of Paris and vice president of the Société de Pathologie Exotique a fragment extracted from the ulcerations of a patient of French origin, who lived in the American colony for approximately 10 years. This patient had been contaminated with the disease popularly known as Pian-Bois after a travel to Kouru, the second more populous town of French Guyana. When he was admitted to the hospital of Caiena, the capital of the colony, in February 1909, he related that the disease started to manifest itself by a vesicle in the posterior part of his wrist, which eventually burst, showing a wound lightly suppurative. It soon became an oval ulceration, resistant to all attempted treatments. Mesnil forwarded laceration samples to Louis Nattan-Larrier and Ferdinand Heckenroth, members of the Sóciété de Pathologie Exotique, for parasitological exams. They concluded that Pian-Bois was a form of leishmaniasis, even though some of its characteristics, like its aspect and structure, were different from Oriental sore, and also evaluated that, despite having proven the existence of Leishmania in the French colony, new researches were necessary before it could be possible ‘from one side, to specify completely “the species of this” parasite, and, from the other, to know which is the relevance of its pathogenical role in the diverse cutaneous ulcerations observed in Guyana’.Footnote 20
Starting with those first two parasitological diagnoses in São Paulo and Caiena, the leishmaniasis found in South America became a research theme constantly visited by different actors and scientific institutions, progressively adding new elements to the cartography of the disease in the New World, and also emphasising the observed differential features and providing models for researchers located in other areas of the American continent, who could give original contributions about the clinical, epidemiological and/or parasitological characteristics of leishmaniasis, observed in their different regions of interaction.
In April 1910, Carlos Rao, a student in the fifth year in Faculdade de Medicina do Rio de Janeiro [Medicine School of Rio de Janeiro], diagnosed, when in Manaus, on the Brazilian North, ‘a typical case of ulcerous leishmaniasis’ in the infirmary of the Santa Casa de Misericórdia of that town. He decided to publish his finding to ‘demonstrate that this ulcerous form existed in other regions of Brazil’, besides the state of São Paulo. It was the case of a 22-year-old patient, of Spanish nationality, who said ‘categorically that he hadn’t been in other localities than Manaus and its surroundings and that he had not had worked in the Northwest railroad’.Footnote 21 Observations like that were especially important, because they proved the indigenous characteristic of the disease in the South American continent. Prior to that, the predominant suspicion about its presence in the area was that it was an outcome due to the arrival of a great number of African and Asian immigrants to Brazilian ports. The existence of cutaneous leishmaniasis in the Northern region of Brazil was confirmed in October of that same year, when Alfredo da Matta, a doctor from the state of Bahia who lived in Manaus, published a paper, also in the Jornal Médico de São Paulo, about five cases attended in Manaus. All cases originated in the region surrounding the tributaries of the Purus River and the Trombetas River, in the state of Pará, along with the Acre territory.Footnote 22
In the following years, the diagnoses of leishmaniasis multiplied in different South American countries. Indigenous cases of the cutaneous form were found by the North American parasitologist Samuel Taylor Darling in 1910, in Colombian workers during construction of the Panama Channel.Footnote 23 The Peruvian physician Edmundo Escomel Hervé presented, during the session of the Medical Society of Arequipa on 6 September 1911, preparations made from cutaneous ulcerations, with circined aspects, of a patient that was diagnosed with leishmaniasis, in which he found some leishmanias.Footnote 24 In that same year, Paul Christiaan Flu, professor of bacteriology and hygiene in Leyden University, conceptualised as leishmaniasis, the disease known in Dutch Guyana as boshyaws or boessie yassi. Footnote 25 In 1912, in Yucatan Peninsula, south of Mexico, Harald Seidelin, in a mission sponsored by the Liverpool School of Tropical Medicine to study the yellow fever, associated leishmaniasis with úlcera de los chicleros, which affected workers in the forests collecting chicle, a resin used for making bubble gums. Seidelin recorded a peculiar characteristic of these ulcerations: they were always located in the ears of the patients and many times they destroyed it completely, never propagating to the mucous tissues.Footnote 26 Amongst workers in orange groves in the north of Paraguay, Luis Enrique Migone diagnosed as leishmaniasis many cases of buba, the name the natives gave to the infection.Footnote 27
In the Santa Casa de Misericórdia of Rio de Janeiro, Gaspar Oliveira Vianna, A young physician from state of Pará state, discovered in a patient, from São João do Além Paraíba, in Minas Gerais state, ‘multiple wounds in face, arms and legs, not clinically recognisable as a case of cutaneous leishmaniasis’. When he analysed tissue samples extracted from this patient, Vianna identified a few protozoa that he thought pertaining to the genus Leishmania (Figure 1). They had oval shape, ‘nucleus located a little above the median part’, but they presented a filament, ‘maybe a rudiment of a flagellum, not observed until today’. As a result of this different morphological element, the pathologist from the Oswaldo Cruz Institute considered it could be a new species of the genus, which he baptised as Leishmania brasilienses – the current Leishmania (Vianna) braziliensis. Footnote 28
Figure 1 Sketch of Leishmania brasilienses made by Gaspar Vianna demonstrating the supposed differential sign that would justify the particularisation of the Leishmania found by him. Source: Gaspar Vianna, ‘Sobre uma nova espécie de Leishmania (nota preliminar)’. Brazil Médico, 25 (1911), 411. Available from obrasraras.fiocruz.br/media.details.php?mediaID=169. Accessed on 18 May 2020.
In spite of that, Gaspar Vianna’s hypothesis was received with great caution by national and foreign medical centres. The filament signalled by Vianna was just the already observed rhizoblast described in Leishmania infantum by Frederick George Novy,Footnote 29 head of the Bacteriology Department of Michigan University, in Leishmania donovani by Samuel Rickard Christophers,Footnote 30 from Indian Medical Service, and in L. tropica by Félix Mesnil, Maurice Nicolle and Paul Remlinger,Footnote 31 from Pasteur Institute of Paris. For that reason, the supposed differential signal of Vianna could not be used for the particularisation of the American protozoan.
Despite the fact that the supposed particularisation pointed by Vianna was soon shown as unfounded, the idea of the existence of a differentiated Leishmania in South America was a priority thematic in one extensive agenda of global research that had as its aim to demonstrate that the parasite was the cause of the differences found in the diseases observed in this region. As we will see in the next topic, since 1911, even though they had never gained unanimity at the epoch,Footnote 32 an influential group of researchers started to defend the necessity of the particularisation of the South American disease and his parasite.
Leishmania braziliensis and the debates about the validation of the South American protozoan
Gaspar Vianna was not the first, undoubtedly not the only, researcher to defend the argument that the leishmaniasis cases identified in South America were caused by a species of Leishmania different from L. tropica. Before him, the Italian doctors Affonso Splendore and Antônio Carini, who had been working in São Paulo for years, had already signalised the relevance of the particularisation of the pathogen responsible for the American disease.Footnote 33 Splendore, in fact, was the first one to name the disease as ‘American leishmaniasis’ and to find the parasite in mucosal lesions, a feat that had ‘great nosological importance’ as it ended the remaining doubts about the association of these mucosal manifestations with protozoa of the genus Leishmania, ‘allowing it to complete the clinical picture of leishmaniasis with the description of the most important of its locations’.Footnote 34
The years 1911 and 1912 were of singular importance for the accumulation of knowledge regarding existing leishmaniasis in South America. In the course of those years, some of the main statements that started to guide the debates about the possibility of particularisation of the disease and of the protozoan found in this region were produced. Apparently, Splendore was the first to defend the specificity of the parasite that produced ulcerative lesions in the mucous parts. In an article published in the prestigious German journal The Archiv fur Schiffs- und Tropen-Hygiene [Naval and Tropical Hygiene Archive] in 1911, he reported that when examining patients from the northwest region of São Paulo, leishmanias in mucous lesions was reported. He, then, came upon the possibility of distinguishing it from the Oriental sore, due to subtle differences in the colour of its cytoplasm in cultures.Footnote 35
The director of the Pasteur Institute of São Paulo, Antônio Carini, also considered it opportune to particularise the disease that caused lesions of the nasal and oral mucous membranes. In May 1911, in the Bulletin de la Société de Pathologie Exotique, he stated that despite the great amount of works devoted to leishmaniasis, he had never found references to mucous forms, even though less frequent than dermatological wounds, those were not uncommon in São Paulo. They were more often seen in individuals who had already been affected by the skin disease, although sometimes the disease started at the back of the mouth and, in these cases, it could not be interpreted as the spread of a primitive skin lesion or the result of self-inoculations by the transportation of infectious materials.Footnote 36
Following the observation of several cases and their very characteristic clinical features, the director of the Pasteur Institute in São Paulo no longer hesitated to diagnose them as ‘mucosal leishmaniasis’; he, just like Splendore, began to defend that they were produced by a different protozoan from L. tropica, despite not having found it yet.Footnote 37 For Carini, the location of Leishmania in the mucous cavities should also occur in other neighbouring countries, where the cutaneous form was endemic; if they had not been reported yet, this was due to the frequent diagnostic errors that led to confusion with syphilis, tuberculosis, blastomycosis and yaws (Figure 2). Carini concluded his article by stating that further research was needed on that ‘form of leishmaniasis with location on the mucous membranes of the nose and mouth, with a very characteristic clinical physiognomy, much more serious than the cutaneous form’.Footnote 38

Figure 2 Mucosal and skin lesions characteristic of the disease reported in São Paulo. Source: Antônio Carini, ‘Leishmaniose de la muqueuse rhino-bucco-pharyngée’. Bulletin de la Société Pathologie Exotique, 4, 5 (1911), 289–91. Available from https://www.biusante.parisdescartes.fr/histoire/medica/resultats/index.php?do=page&cote=bspex1911&p=308. Accessed on 04 November 2020.
In Peru, the doctor Edmundo Escomel Hervé, a native of Arequipa, was not regarded in high terms by the medical elite of Lima, but that did not prevent him, or perhaps even encouraged him, to seek foreign dialogue, which would eventually strengthen his professional legitimacy in his own country. In 1904, 2 years after graduating in medicine from the University of San Marco, he attended the microbiology course offered by the Pasteur Institute of Paris. There he established fruitful contacts with renowned French researchers, such as Alphonse Laveran, Louis Nattan-Larrier and Émile Brumpt, before returning to his homeland to dedicate himself to the study of tropical diseases, or ‘national pathologies’, as they were called at the time in his country.Footnote 39
In June 1911, Escomel reported on the pages of the Bulletin de la Société de Pathologie Exotique his observations on espundia, a chronic, little-known disease, spread mainly among indigenous people in or near forests with ‘exuberant vegetation, hot temperature and great humidity’ in central Peru. It was characterised by granular ulcerations with rounded edges that secreted thick pus and that had a clinical development that could last for more than 30 years. In time, the ulcerations healed and left scars, but, later, the disease could resurface in the mucous membranes and spread to ‘the nasal cavities, the vault and the palate veil, the tonsils, the pharynx, the larynx, the cheeks, the tongue, the lips and even the earlobes and the face’, condemning the patient to ‘a miserable life due to his disgusting appearance and fetid breathing’.Footnote 40
There were, for Escomel, two central aspects in the pathogenesis of espundia: the ‘enlargement of the nose’ due to the destruction of the nasal cartilage, allowing it to make the diagnosis ‘at first sight’; and, when the mouth was compromised, the presence of somewhat deep grooves that crossed in all directions the palatal vault. Two of them, always present, crossed forming what he called ‘the palatal cross of espúndia’.Footnote 41 In spite of the detailed description of the pathogenesis process, Edmundo Escomel was unsuccessful in identifying the aetiological nature of that wild disease, but his reports certainly made a strong impression on the president of the Société de Pathologie Exotique, who quickly asked the Peruvian to send to Paris samples of hard palate with the characteristics he described.
In March 1912, Alphonse Laveran, alongside Louis Nattan-Larrier, released the first results of his studies on the disease reported by Escomel in the Bulletin he coordinated, made from a piece of hard palate mucosa of a Peruvian patient who lived with espundia for 50 years. When examining the material sent in January of that same year by the doctor from Arequipa, the French parasitologists found leishmanias ‘with a great analogy with L. tropica but presenting a particularity that seemed interesting to us’: the protozoan from Peru had slightly different behaviour and dimensions and its nucleus appeared to be ‘attached to the [cellular] wall and flattened’, and not rounded or ovular, as the one seen in the parasite responsible for the Oriental sore.Footnote 42
From that moment on, the French doctors entered for once the debate on leishmaniasis found in the South American continent. Dialoguing with the conclusions of Affonso Splendore, Laveran and Nattan-Larrier declared the possibility of dealing with another species of Leishmania. In those terms, that fact ‘would explain the differences that are observed from the clinical point of view’ between the American disease and its eastern counterpart, but to confirm this hypothesis further research would be necessary, since they considered their observations ‘evidently insufficient’ so that they could resolve this issue.Footnote 43
Splendore, upon realising that the Société de Pathologie Exotique was becoming the main discussion forum on leishmaniasis found in South America, published in its Bulletin a new article, in June 1912, in which he reported having observed three more cases of this ‘new nosological entity’, whose ‘localisation could occur not only on the skin, but also on the mucous membranes of the nose and mouth’. Identifying it ‘undoubtedly to the Peruvian infection registered by Escomel under the name espundia’, he claimed priority in his diagnosis and characterised it as being frequent in the region between the states of São Paulo and Mato Grosso.Footnote 44 He also reported that by inoculating monkeys with protozoa taken directly from mucosal lesions, they originated skin lesions with histology ‘identical to that of the Aleppo evil’, but that in its flagellated form it was possible to distinguish them from the pathogen responsible for the Oriental sore, due to its shape and, above all, the greater length of the flagella (Figure 3).Footnote 45
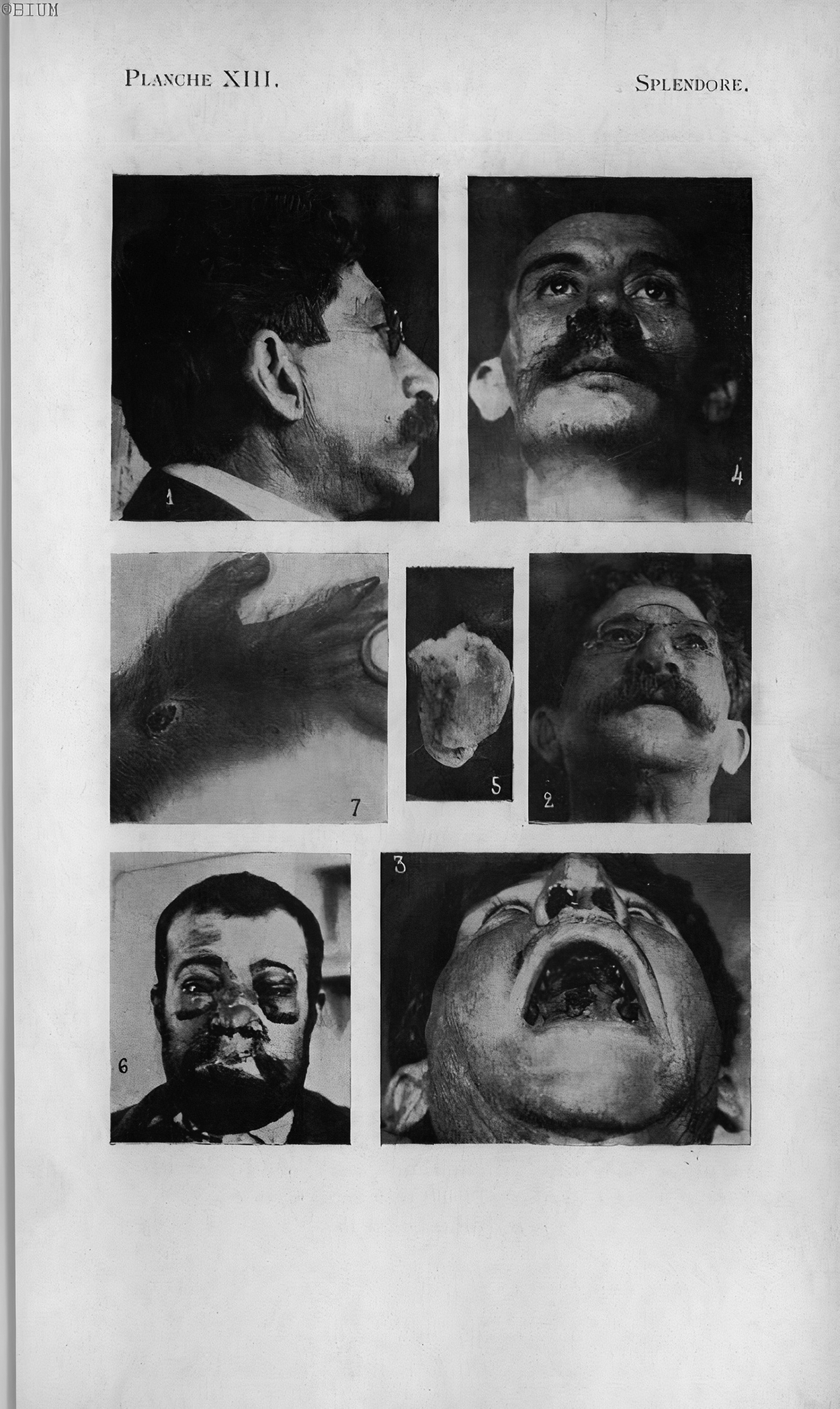
Figure 3 Photographs of the patients examined by Splendore and of the inoculation made in an experimental animal. Source: Affonso Splendore, ‘Leishmaniosi con localizzazione nelle cavità mucose (nuova forma clinica) (avec résumé français)’. Bulletin de la Société Pathologie Exotique, 5, 6 (1912), 413, Planche XIII. Available from https://www.biusante.parisdescartes.fr/histoire/medica/resultats/index.php?do=page&cote=bspex1912&p=453. Accessed on 23 October 2020.
These early studies that sought to characterise the American parasite seemed to be going in the same directions by pointing out certain morphological characteristics different from those observed in L. tropica. Splendore had highlighted different colours in the cytoplasm, fusiform shape and longer flagella of the parasite found in the mucous membranes and Escomel, despite not being able to publicise his finding, identified leishmanias armed with flagella on the human body. These attempts to particularise the variants of Leishmania found in South American, however, were not unanimously accepted in the main forums dedicated to the study of leishmaniasis, notwithstanding the fact that the American disease presented manifestations and clinical trajectories that were extremely different from its eastern counterpart.
In that same month, July 1912, the French parasitologists published their second ‘contribution’ to studies on espundia. Analysing new materials sent by Escomel (for the first time qualified as a corresponding partner in the French society), they confirmed the diagnosis of leishmaniasis made in the first article and brought new elements to defend the particularisation of the American pathogen:
The study of Leishmania americana is too recent for us to conclude about the morphological differences between this Leishmania and L. tropica, but the differences that exist, from a clinical point of view, between this leishmaniasis (yaws or espundia) and the Oriental sore are undeniably evident; so even though we cannot observe any appreciable morphological difference between Leishmania americana and L. tropica, it is necessary to distinguish between these parasites, just as L. donovani and L. tropica are distinguished, even though these two leishmanias present from the morphological point of view great similarity.Footnote 46
For Laveran and Nattan-Larrier, the Leishmania found in South America, even if it was not a new species, appeared to compose at least one variation of L. tropica, and for this reason their proposition was to call it L. tropica var. americana, or, ‘for short’, Leishmania americana. In this second article, the French emphasised the necessity of abandoning regional denominations (uta, espundia, Bauru’s ulcer, Bahia’s button, pian-bois, etc.), as well as the usage of the ‘American Leishmaniasis’ category, in order to end the predominant confusion over diagnoses.Footnote 47
In 1913, the French parasitologist Émile Brumpt, Rafael Blanchard’s main disciple,Footnote 48 accepted the invitation to assume the chair of Natural History at the recently founded São Paulo School of Medicine and Surgery.Footnote 49 Graduated from the Paris School of Medicine, Brumpt was already considered a renowned parasitologist when the invitation was made. Upon his arrival in Brazil, he launched and prefaced the second edition of his medical treatise, Précis de Parasitologie (1913) [Summary of Parasitology], which became a great influence to the region’s tropicalists. In addressing leishmaniasis, Brumpt confirmed agency on L. braziliensis as responsible for American leishmaniasis, becoming the first foreign researcher to validate Gaspar Vianna’s proposition.Footnote 50
The French parasitologist was exceptionally interested in the theme of leishmaniasis, especially the American ones. During the 1-year period of his stay in São Paulo – he would return to France in August 1914, due to the outbreak of the First World War – he carried out extensive epidemiological research on the different varieties of the disease found in the countryside of the state. Between 8 and 30 September 1913, Brumpt organised with Alexandrino Pedroso, director of the anatomopathological laboratory of Santa Casa de Misericórdia of São Paulo, an expedition to non-urban areas of the state, including also some parts of the state of Mato Grosso, to study them. Sixty-five cases were detected during the expedition, 90% of them were benign, remarkably similar to cutaneous leishmaniasis in the Old World (Oriental sore), yet in about 10% of the cases the disease had malignant forms that allowed it to be considered ‘a very individualised condition’. Its epidemiological characteristics led Brumpt and Pedroso to classify it as ‘American forest leishmaniasis’, because, differently from the Oriental sore, endemic in cities with large population agglomerations, the disease observed in São Paulo and Mato Grosso was rife in isolated areas with few human habitations near forests.Footnote 51
In 1914, Gaspar Vianna travelled from Rio de Janeiro to São Paulo to carry out, in Pedroso’s laboratory, research on the behaviour of the protozoan revealed in organisms of naturally infected dogs. He received a cut of a nasal lesion from one of these animals from the São Paulo doctor and found ‘smooth muscle cells with leishmanias’ in a small artery ‘relatively far from the ulcerated part’. It was the first time that the protozoan was seen so distant from the cutaneous lesion. Believing that he had evidence of the parasite’s mobility and its evolution ‘at a distance from the ulcerated point’, Vianna supposed that the lesions caused by L. brasiliensis were much deeper than imagined.Footnote 52
Unlike the note published in Brazil Médico [Medical Brazil] in 1911, when Gaspar Vianna sought to particularise L. brasiliensis from its morphological aspects, he now based its specificity on the location and behaviour in the parasitised organism. This, however, was the last article written by Gaspar Vianna. He died tragically that same year, at the age of twenty-nine, victim of pulmonary tuberculosis contracted during an autopsy. The liquid present in the ribcage of the examined body, under pressure, poured over his unprotected face and mouth. A few days after this incident, the first signs of acute tuberculosis appeared. Two months later, on 14 July 1914, the physician from the state of Pará died.Footnote 53
Gaspar Vianna, one of the youngest researchers at the Instituto Oswaldo Cruz, was the first of them to die, causing great commotion. In addition to his work related to the particularisation of the American leishmaniasis parasite, analysed in this article, he had also proposed at the VII Brazilian Congress of Medicine and Surgery, held in Belo Horizonte in 1912, a treatment for the disease: the subcutaneous injections of emetic tartar quickly became popular around the world, becoming the preferential treatment for all forms of leishmaniasis, including visceral ones. The decrease in the extremely high mortality rates of calazar in the Indian subcontinent, due to the treatment with emetic tartar, contributed to make Gaspar Vianna one of the great idols and martyrs of Brazilian science.Footnote 54
L. braziliensis, nonetheless, was more fortunate than its proponent. The profusion of works about the American disease reverberated in European forums of tropical medicine. In 1914, British physician Patrick Manson, often recognised as the father of modern tropical medicine, launched the fifth edition of Tropical Diseases,Footnote 55 ‘revised from start to finish, and extended’.Footnote 56 In this edition, the author grouped the Oriental sore and the calazar (described in a different chapter in previous editions) in a chapter called ‘Leishmaniasis’ and, for the first time, included the espundia to designate the form of the disease observed in the South American region. In the introduction to that chapter, Manson considered:
Under the term “leishmaniasis” at least three diseases of man are included, viz. kala-azar, Oriental sore, and espundia. These diseases, though clinically quite distinct and having each a definite topical and geographical distribution, are all associated with what optically appears to be the same organism, Leishmania. But though their respective organisms appear to be morphologically identical, it is by no means justifiable to conclude that they are specifically identical. The Leishmania form is common to many protozoa; it is merely a stage – an immature stage – and until the life-history is quite complete, and the natural history of the parasites of these diseases has been worked out, our judgment as to their identity or otherwise should be suspended. If it turns off to be the case that the germ causes of the various clinical forms of leishmaniasis are specifically identical, we shall have to conclude that the special pathogenic properties of these germs have been conferred on them during their extracorporeal life by passage through particular animal intermediaries. Herein lies a wide field for future investigations.Footnote 57
It is worth to note that, instead of using the denomination proposed by Laveran and Nattan-Larrier, ‘American leishmaniasis’, Manson preferred to use the name given by natives of Hispanic countries, espundia. Regardless of including it in the chapter on leishmaniasis, Manson did not name his aetiological agent, though making reference to that of the calazar as L. donovani and that of the Oriental sore as L. tropica. Footnote 58 Using the terms espundia, Brazilian yaws or uta – as it is read in Patrick Manson’s textbook – several authors (Carini, Paranhos, Splendore, Escomel and others) described a severe form of leishmaniasis found in certain South American countries. Describing the clinical course of the espundia, Manson emphasised the moments of this process: initially skin lesions similar in appearance to the Oriental sore appeared, which, when healing, left characteristic marks; months or years later, these marks give origin to intractable ulcers in other locations, as the tongue and/or the oral and nasal cavities, which seriously disfigured the patient and led him to death after long suffering. Even though there were Leishmania corpuscles in the mucous ulcers, they were not found in great number, yet in patients with mucosal lesions, ulcers in the dermis typical of the Oriental sore occurred. Manson believed that they developed at the site of the bite of a forest insect, of a still unknown species. The role played by the intermediate host was fundamental for the definition of the clinical modality of leishmaniasis that would affect the human host.Footnote 59
On the other hand, in Paris, Laveran continued his studies on that group of diseases that aroused so much interest in the field of medicine leading the French to call it ‘exotic’. In May and June, 1915, sessions of the Society he presided over, two dense complementary memories whose title was Leishmaniose américaine de la peau et des muqueuses were presented by him, with a detailed compilation of the works produced so far on the disease and its geographical distribution in South America.Footnote 60
According to Laveran, all attempts to distinguish the American parasite had failed, but he was convinced that it was a variation of the eastern parasite or even a new specie; therefore, he placed great emphasis on the clinical frames of the disease it produced, for it was possible to differentiate Leishmania by its biological characteristics. The French parasitologist stated:
From the morphological point of view, it can be said that there is no permanent feature to differentiate American Leishmania from L. tropica, but this does not prove that the two parasites are identical; Leishmania donovani has the same morphological characteristics as L. tropica, but it was nonetheless agreed that they are two quite different parasites, the first producing the calazar and the second the Oriental sore. Also based on the pathogenic action of the parasite, and on the symptoms and the anatomical lesions it frequently causes, in particular affecting the nasal, buccal and pharyngeal mucous membranes, we have proposed, mr. Nattan-Larrier and I, to establish, not a distinct species, but a Leishmania variety of the Oriental sore, under the name of L. tropica var. americana. Footnote 61
Nevertheless, if both the proposition of the differential sign of Gaspar Vianna and that of Laveran and Nattan-Larrier proved to be erroneous or insufficient to qualify the American protozoan, why should the French’s denomination prevail over that of the Brazilian researcher who preceded it? Despite the death of Gaspar Vianna, new works would come to light in the following years giving new strength to L. braziliensis in detriment of L. tropica var. americana.
In 1915, Alfredo da Matta published an article in three periodicals of different nationalities (Brazilian, Argentine and Venezuelan) in which he analysed both the clinical physiognomy and the classification and synonymy of leishmaniasis found in South America.Footnote 62 He admitted the existence of classic cases of Oriental sore in the region, which he associated with L. furunculosa,Footnote 63 but gave to L. braziliensis a major role, attributing to this protozoan three forms of leishmaniasis: the ulcerous cutaneous, known in rural areas of the Amazon state as ‘sponge’, had the appearance of cauliflower and secreted a purulent liquid capable of producing new cases of the disease; the non-ulcer cutaneous form, with a ‘delicate’ prognosis, which was known as Bauru’s ulcer in São Paulo, ferida braba [hard sore] in Amazonas, yaws in Paraguay and uta in Peru; and, finally, the cutaneous-mucous form, called by Da Matta ‘leishmaniasis of the cavities’, which was located in the mouth, pharynx or vagina of the sick individual. This last type of leishmaniasis had a ‘characteristic, terrible, cancerous invasive slow march’ and was accompanied by a series of complications: the nasal cavities became insufficient to the entrance of the air, the patient remained with his mouth ajar, letting out the saliva and the resulting mucus of the pathogenic process. On a long-term basis, complications concerning olfactory, hearing and even vision could appear.Footnote 64
As a corresponding partner of the Société de Pathologie Exotique, Da Matta sent to be published, in July 1916, the expanded version of his article, with twelve photographs to better document the clinical frames related to that kind of Leishmania. In spite of the three forms presenting characteristics and clinical courses not observed in the Oriental sore, ‘cavity leishmaniasis’ was the form that most concerned authorities and scholars studying the American disease, for it made the patient invalid. At the end of the article, Da Matta reproduced a table systematising the relationships between clinical conditions and their respective causal agents (Figure 4). That led Alphonse Laveran, the president of the Société de Pathologie Exotique, to strongly criticise the attribution of the Oriental sore to L. furunculosa:
It is true that, in 1891, Firth described, under the name of Sporozoa furunculosa, the parasite of the Oriental sore, but the description of this Leishmania seems to us very misinformed. On the contrary, with Wright’s work, all hesitation disappeared, making it impossible to ignore the excellent description and photographs of the parasite presented under the name Helcosoma tropicum. I believe, then, that for this reason the majority of observers give the name of the Oriental sore parasite as L. tropica. Wright.Footnote 65
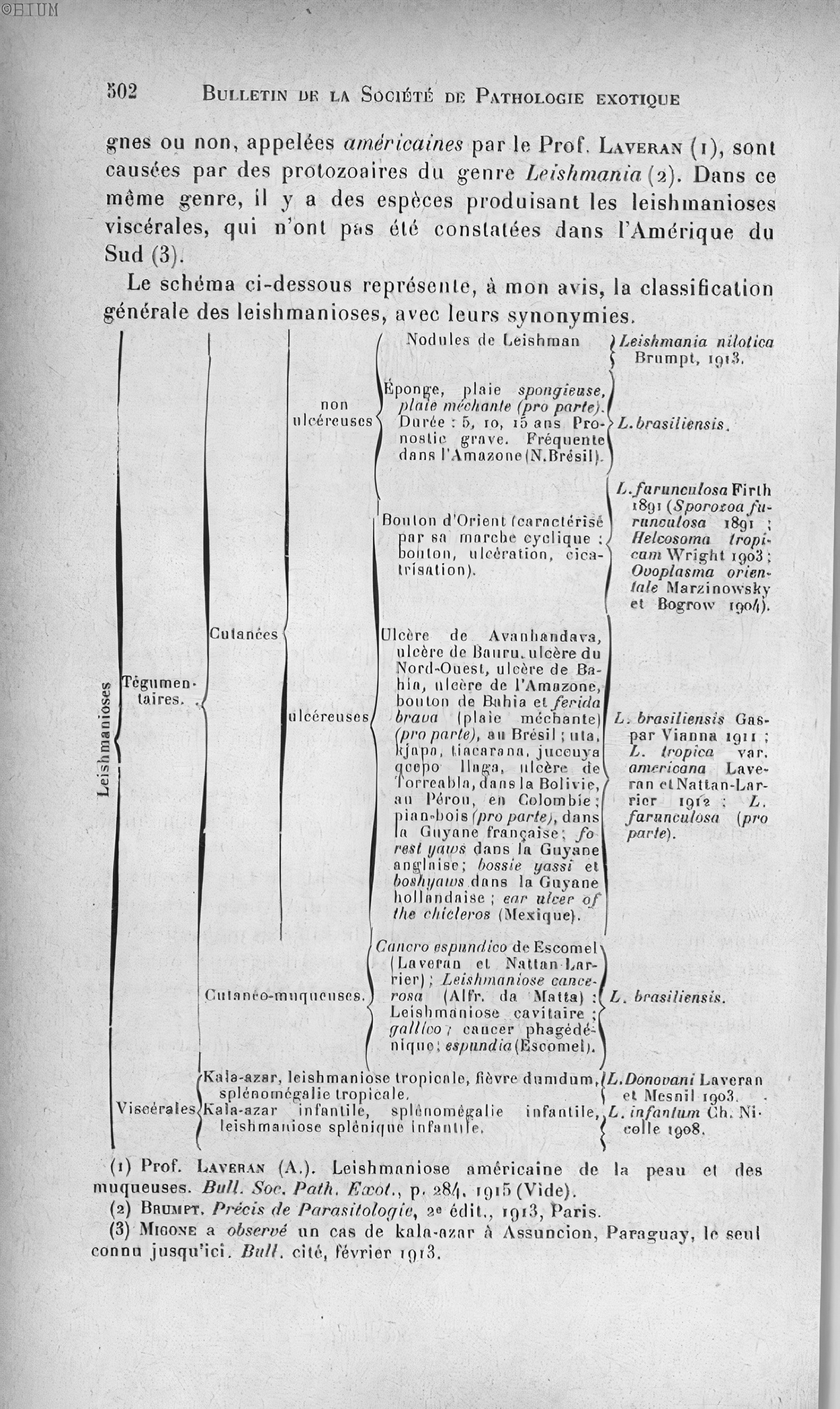
Figure 4 General classification of leishmaniasis, with synonyms. Source: Alfredo Da Matta, ‘Sur les leishmanioses tégumentaires. Classification générale des leishmanioses’. Bulletin de la Société de Pathologie Exotique, 9, 7 (1916), 302–503. Available from https://www.biusante.parisdescartes.fr/histoire/medica/resultats/index.php?do=page&cote=bspex1916&p=541. Accessed on 07 January 2021.
Alphonse Laveran’s comment did not involve just a matter of priority in the description of the Oriental sore agent, but also the support of the name given by the Frenchman to the American parasite: L. tropica var. americana, on the grounds that, as they did not find any differential sign, the only argument that could legitimise their proposition in preference to Gaspar Vianna’s was the same used to delegitimise the name of Firth, in other words, a misinformed description.
In the course of that same year, a new work in defence of L. braziliensis was presented at the first Conference of the South American Society of Hygiene, Microbiology and Pathology, held in Buenos Aires, capital of Argentina, in which for the first time the term ‘American tegumentar leishmaniasis’ was used. In the communication presented by Arthur Neiva and Berlamino Barbará, they fiercely criticised the French authors insistence in not recognising the validity of the nomenclature proposed by Gaspar Vianna. They said: ‘We are surprised by the obstinacy of Laveran in calling it L. tropica var. americana, because this denomination suffers from two errors: one of them quite common here and in Europe; we refer to the denomination of tropical, and another, his misuse of the name ‘American’. Based on Linnaeus’ laws of zoological nomenclature, Neiva and Barbará said that priority should be given to Gaspar Vianna, therefore to L. braziliensis. ‘In general, researchers from South America and Europe indistinctly called L. tropica to the pathogens of American and Eastern leishmaniasis, a name that, for the reasons that precede, cannot prevail and should not be used without incurring in error’.Footnote 66
In this communication, Neiva and Barbará also invoked an exotic argument in defence of the American disease and parasite: pre-Columbian ceramics, known as Incan huacos [ceramic vases], seemed to exhibit human figures with lesions on the nose and mouth that they judged similar to those produced by uta, a popular name given to the cutaneous form of leishmaniasis in Peru. They came to be a very convincing proof of the ancestry and indigenous origin of leishmaniasis in South America. Although this interpretation is not consensual – many believed that the injuries came from mutilations caused by leprosy, syphilis or by corporal punishment – these archaeological findings contributed significantly to the characterisation of cutaneous and cutaneous-mucus leishmaniasis as a disease assigned to the region and, therefore, differentiated from cutaneous leishmaniasis – or Oriental sore – from the Old World.Footnote 67
In 1917, Alphonse Laveran published Leishmanioses. Kala-azar, Bouton d’Orient, Leishmaniasis americaine, the compendium used as an opening to this article. In the chapter referring to American leishmaniasis, the French parasitologist almost repeated paragraph by paragraph the information presented in two communications directed to the society he presided over in 1915, but with few and significant updates. In addition to adopting the classifications and photographs proposed by Da Matta, in the 1916 article, he recognised for the first time the possibility of losing priority in the denomination of the pathogen of American leishmaniasis. In spite of continuing to call it L. tropica var. americana, pondered:
This opinion is not unanimous; some authors consider Leishmania americana to be identical to L. tropica; others demarcate a very distinct species, under the name of L. braziliensis; still others admit that American leishmaniasis can be caused by both L. tropica and L. braziliensis. Footnote 68
As we can perceive by reading that last quotation, in this important compendium Laveran adopted a new stance regarding L. braziliensis. Although previously the French parasitologist emphatically discarded the hypothesis proposed by Gaspar Vianna, the new works, produced based on the South American context, led him to admit the possibility of validating the denomination of Vianna, ratifying the agency and the importance of the research produced by South American tropicalists in the production of knowledge in the tropical medicine field.
Also in 1917, Patrick Manson launched the sixth edition of Tropical Diseases. In the space dedicated to leishmaniasis, Manson replaced the nomenclature ‘Espundia’, used in the fifth edition, with ‘American Leishmaniasis’, made a brief allusion to the possibility of treating skin and cutaneous-mucus diseases with emetic tartar, and also recommended to students in the field of tropical medicine to consult ‘Laveran’s recently published work, “Leishmanioses”, for a full and accurate discussion of this important subject’.Footnote 69
The effort to particularise the species of L. braziliensis was supported by a researcher from the Rockefeller Foundation, the Japanese Hideyo Noguchi. Considered one of the world’s leading specialists in Leptospira and leptospirosis, he was highly regarded at that time for having associated the causative agent of yellow fever with this genus of bacteria, as shown by Benchimol.Footnote 70 Although leishmaniasis was not his most important object of study, he was the first to substantiate, with immunological agglutination technique, the difference between protozoa of the genus Leishmania. In the International Conference on Health Problems in Tropical America, held from 21 July to 1 August 1924 in Kingston, the capital of Jamaica, Noguchi defended the existence of three very distinct species: L. donovani, L. tropica and L. braziliensis. As the two species associated with the visceral form of the disease – L. donovani and L. infantum – showed identical behaviour as antigens when coming into contact with the antibody considered specific and capable of provoking the agglutination reaction, Noguchi considered them identical, but differentiated the pathogen of the Oriental sore from that of the South American cutaneous and mucus leishmaniasis, on behalf of them not having a common ‘agglutinative property’. Strictly speaking, the antibodies caused by these antigens did not produce the characteristic lumps of the pathogen lysis process when cross tests were carried out.Footnote 71
In the 1920s, in addition to all these studies that sought to particularise the disease and the American parasite, it started to come on the scene the works produced by the brothers Edmond and Etienne Sergent, and their assistants at the Pasteur Institute in Algeria,Footnote 72 Henrique Aragão, at the Oswaldo Cruz Institute,Footnote 73 and, soon after that, Saul Adler and Oscar Theodor at the Hebrew University of Jerusalem,Footnote 74 who showed very strong evidence that the tiny blood-sucking flies (still little known by medical entomology) known as phlebotomes could act as, at least, one of the forms of transmission of leishmaniasis, giving more strength to the idea of particularisation of the disease and of the American protozoa, for they demonstrated that the species existing in the South American continent were differentiated from those found in the endemic regions of cutaneous and visceral leishmaniasis in the Old World.
From the 1930s onwards, L. braziliensis started to be recognised as the cause of all pathogenic manifestations of leishmaniasis in South America, while L. tropica var. americana left the scene in the debates in the tropical medicine field. Despite the fact that the researchers did not find any differential sign with the technical resources existing at the time, the American protozoa was validated on the basis of the different pathogenic and epidemiological processes, behaviours in culture media, susceptibility to infect different mammals, and, last but not least, due to the archaeological findings of Inca huacos that pointed to the possible existence of the disease in the pre-Columbian period, indicating that the leishmaniasis found in South America were, in fact, indigenous to the region, theory which would later be confirmed (and expanded with other neotropical Leishmania species),Footnote 75 when, finally, it became possible to differentiate, from the 1960s onwards, these Leishmania species with the introduction of modern molecular biology techniques.
Conclusion
In this article, I sought to demonstrate how researchers from different South American countries took part in the process of globalisation of the tropical medicine paradigm, through research on leishmaniasis found in this region, in order to include them in a global history of tropical medicine that goes beyond European borders and its imperialist practices. Ever since the mid-1990s, David Arnold had already acknowledged that fact. He emphasised the relevance of carrying out analysis which endorsed the transnational perspective for the construction of narratives that allow ‘to see Europe’s medical ventures overseas as more than just a series of independent national narratives’ and also to demonstrate “how medical networks transcended national and imperial divisions, or how medical knowledge was passed on, over time as well as across space, from one European power to another’.Footnote 76
The conclusions of this article go directly against some of Deborah Neill’s ideasFootnote 77 who, despite the excellent work, expressed a certain resistance to include non-European actors and their institutions in the processes of construction and globalisation of tropical medicine. In her book Networks in Tropical Medicine: Internationalism, Colonialism, and the Rise of a Medical Specialty (1890–1930), she sought to analyse the scientific networks formed by a relatively small but well-connected group of European researchers, dedicated to tropical medicine and active in the colonial territories of the African and Asian continent.Footnote 78
According to the author, despite the strong disputes between European nations at the beginning of the twentieth century, the supporters of the new medical specialty, shared commom agendas for research and training and a certain similar ‘European heritage’, leading them to succeed in the building of its scientific authority, in the development of shared and complementary works that often were planned and shared across national borders.Footnote 79 In spite of being strongly influenced by the transnational perspective, Neill’s work is still marked by a Eurocentric vision of the construction, globalisation and institutionalisation of tropical medicine.
For the author, these processes, and even the construction of sociability among its members, were events marked by a ‘strong sense of inter-European cooperation’, and, therefore, occurred almost exclusively within the European continent.Footnote 80 Focusing on the work of researchers from France, Germany, England and Belgium, Neill listed three reasons to justify, in her view, the reasons why the genesis and development of this medical field occurred only within the borders of the largest colonising countries in Europe and not in tropical regions. First, the colonial budget was small and was not enough for the cost with constructions and staff for local institutions. Furthermore, scientists saw proximity with other scientists as more important than proximity to material and patients. And finally, in presenting the third and ‘most important’ reason, she reproduced a quote from the French doctor De George Treilles (1924–2006), in which he argued that Europe was the only place where it was possible to train colonial doctors, because it would not be ‘possible to give solid value to isolated instruction centres in the tropics’.Footnote 81
It is interesting to note that, with the exception of the first aspect, directly related to European imperialist politics and management, the other two can easily be replicated to the rest of the world, that is, in Neill’s arguments it is understood that only within Europe was it possible for the members of this newly created medical field to interact with each other and that, according to the vision of its actors, only medical-scientific institutions located in European territories enjoyed prestige and authority in the field of tropical medicine.
Deborah Neill did not take into account the literature produced about the history of tropical medicine in South America. As several authors in the field of the history of medicine have demonstrated the medical elites from different South American countries had not only been attentive to these initial developments in the European medical field, but they were co-participants and explorers of important frontiers of microbiology and tropical medicine. Basing their methods, procedures and practices in the new assumptions of this field in formation, certain groups of doctors have gained prominence by producing innovative knowledge, conducting prophylactic campaigns, proposing courses and disciplines at research institutes and universities and giving answers to their own and, sometimes, particular public health problems specific to their local realities.Footnote 82
The proposition of this article is to contribute to the building a less Eurocentric view of the processes of construction and institutionalisation of tropical medicine, which includes the diverse characters located in non-European regions, such as Latin and South America, Africa and Asia, in order to abandon, once and for all, George Basalla’s proposals on the diffusion of European Science (with a capital S) to the rest of the world.Footnote 83
Competing interests
The authors have no competing interests to declare.







