Introduction
A School Feeding Program (SFP) is a targeted social protection program for safeguarding vulnerable children from hunger and has multiple side benefits(Reference Bundy, Burbano and Grosh1–Reference Wang and Fawazi3). At the individual level, an SFP improves school enrolment, attendance and academic performance and may advance the anthropometric status of children(Reference Wang and Fawazi3,Reference Kristjansson, Petticrew and MacDonald4) . At the household level, it alleviates food insecurity and economic stress(Reference Lawson5). At the community level, a home-grown school feeding (HGSF) provides market opportunities to smallholder farmers and stimulates the local economy(6).
Almost all countries in the world implement school feeding at different scales and quality(Reference Jomaa, McDonnell and Probart2). In 2013, globally 368 million children were fed daily at school with an annual investment of 47–75 billion USD(7). Investment per child ranged from 20 to 1500 USD per year(7). SFP has been operated in two modalities: school meals where children are fed in the school compound or take-home rations, where families are given food as incentives for their children's school enrolment. The SFP frequently can be integrated with other school health services including deworming, nutrition education and micronutrient supplementation(7).
In Ethiopia, an SFP was first piloted in 1994 in Tigray region(Reference Poppe, Frölich and Haile8) and the HGSF program was initiated in 2012 in the southern region(9). The coverage of the program has progressively increased and in 2016 more than a million children were reached(9). Currently, the government has expanded HGSF to different parts of the country including urban areas and the program is being considered as a key nutrition-sensitive intervention to combat malnutrition(10).
So far, only a few cross-sectional studies have evaluated the effect of the Ethiopian SFP on the nutritional status of children(Reference Zenebe, Gebremedhin and Henry11,Reference Gutama12) . In Southern Ethiopia, Zenebe et al. reported significantly better body-mass-index for age (BAZ) and height-for-age (HAZ) Z-scores among SFP beneficiaries(Reference Zenebe, Gebremedhin and Henry11). A cross-sectional study in Addis Ababa also found better anthropometric and haemoglobin status among children covered by SFP(Reference Gutama12). A systematic review of SFP evaluations in low- and middle-income countries reported small but significant effect on the weight gain of children(Reference Watkins, Gelli and Hamdani13).
The purpose of the present study was to evaluate the effect of SFP on the anthropometric and haemoglobin status of school children in southern Ethiopia where HGSF is being implemented.
Materials and methods
Study design
A prospective cohort study was used to compare the anthropometric and haemoglobin status of SFP beneficiary and non-beneficiary school children 10–14 years of age. SFP beneficiaries and non-beneficiaries of the program were enrolled from 16 schools and followed for one academic year. Data on exposure, outcome and other pertinent control variables were gathered over two rounds of baseline and end-line surveys. The net effect of the program on the outcomes of interest was estimated using Difference-in-Differences (DID) analysis.
Study setting
The study was conducted in 16 second-cycle primary schools (SCPS) found in four SFP-targeted rural districts (Borecha, Dara, Bona and Loka Abaya) of Sidama region, southern Ethiopia. The region is located approximately 300 km south of the national capital, Addis Ababa, and has about four million inhabitants, of whom 95 % were rural dwellers(14). The zone covers nearly 10 000 km2 area and is characterised by diverse agroecological features. The region is divided into 23 administrative districts.
In Ethiopia, the primary education system is divided into first- (grade 1–4) and second- (grade 5–8) cycles. During the study, 111 SCPS including 27 SFP-targeted schools were operational in the four districts. Schools are typically enrolled in the program in consideration of the severity of the food insecurity situation in their catchment areas, as evaluated by the regional education bureau, donors and other partners. Students registered in SFP-targeted schools receive a daily free cooked school meal prepared from cereals and legumes.
Sample size calculation
The sample size of 480 school children (240 SFP beneficiaries and 240 non-beneficiaries) was determined using G*Power software(Reference Faul, Erdfelder and Lang15) assuming mean BAZ, HAZ and haemoglobin would be compared between the two groups using a one-tailed mean difference t-test at 95 % confidence level and 80 % power. Furthermore, one-to-one allocation ratio, medium effect size (d 0⋅4), design effect of 2 and 20 % allowance for possible dropout were assumed. The sample size calculation formulas in consideration of each objective of the study were presented later (Table 1).
Table 1. Sample size calculation for each objective of the study

Sampling procedure
Students were identified from eight SFP-targeted and eight control schools from the above-mentioned four districts. Students registered in SFP-targeted schools were considered as SFP beneficiaries, whereas, those from non-targeted schools were taken as non-beneficiaries.
From each of the four districts, two beneficiary and two non-beneficiary schools, totally sixteen schools, were included in the study. In every district, two schools with SFP were selected at random from schools enrolled in the program. Then each of the selected schools with the feeding program was one-to-one matched with a control school based on predefined matching criteria: similar agro-ecology features (similar in agricultural production, climatic zone and landscape) and geographical proximity (being within the same district). Ultimately 480 children, 30 eligible students per school, were selected across all the grades using a simple random sampling technique. Purposely to increase the sample size, those who were not willing to take part in the study were replaced by randomly selected eligible children from the same section.
Variables of the study
The exposure variable of interest was SFP enrolment status (beneficiary v. non-beneficiary) and the outcome variables were BAZ, HAZ and haemoglobin concentrations of the children. Control variables were socio-economic status indicators including maternal and paternal literacy, household monthly income, household wealth index, household food insecurity, head of the household (male v. female), type of water source at home (improved v. non-improved), age and sex of the child.
Methods of data collection
Data were collected in two rounds of surveys implemented at the beginning (September 2017) and end (June 2018) of the 2017/2018 academic year. A similar set of variables were collected in the surveys. Haemoglobin status was measured in the field from capillary blood using HemoCue analyzer (HemoCue Hb 301, Ängelholm, Sweden). Haemoglobin measurements were adjusted for altitude according to the recommendation of the World Health Organization (WHO)(16). Height and weight measurements were taken following standard procedures without heavy clothing and shoes using a portable stadiometer and calibrated digital UNICEF scale. Haemoglobin and anthropometric measurements of children were taken in private settings in each school.
Parents of the index children were interviewed at home about socio-demographic, economic, access to social services and household food security situations using a structured and pretested questionnaire prepared in the local Sidamu Afoo language. The parts of the questionnaires on socio-demographic and economic information were adopted from the standard Demographic Health Survey (DHS) questionnaire(17). Household food insecurity was measured in accordance with the Food and Nutrition Technical Assistance (FANTA) indicator guide and classified as food secure and mild, moderate or severe food insecurity(Reference Deitchler, Ballard and Swindale18). In accordance with the criteria of WHO-UNICEF, type of drinking water source was categorised as improved or unimproved(19).
Data analysis
SPSS version 23 software was used to analyse the data. Anthropometric indices were generated using WHO AnthroPlus software based on WHO-2007 population growth reference data. Adolescent children with z-score below −2 for BMI-for-age and height-for-age indices were considered as thin and stunted, respectively. As commonly done in national Demographic and Health Surveys(20), household wealth index – a proxy indicator of household cumulative living standard – was developed using Principal Component Analysis (PCA) based on ownership of durable household assets and materials used for household construction.
DID analysis was used to estimate the net effect of SFP on the three outcomes of interest. DID is an analytic technique for estimating the effect of an intervention based on observational data by taking into consideration the baseline difference between the intervention and control groups and changes overtime in the groups(Reference Wing, Simon and Bello-Gomez21). In the present analysis, DID was estimated using simple and multiple mixed-effects linear regression model with a random intercept defined for each school. Initially, the balance of the control variables between the intervention and control groups was assessed using χ 2 and independent sample t-tests and in the multivariable models, significantly unbalanced variables were adjusted.
Ethical considerations
The study was implemented in accordance with the Declaration of Helsinki for research involving human subjects. The study protocol was approved by Hawassa University Ethics Committee (Reference No; IRB/003/10) and data were collected after taking written informed consent from the parents of the children. Assent was also secured from the children themselves.
Results
Socio-demographic characteristics
Table 2 summarises the characteristics of the 240 SFP beneficiaries and 240 non-beneficiary children and their caregivers. The mean (±sd) age of the caregivers during the baseline survey was 32⋅8 (±9⋅3) and 32⋅1 (±8⋅2) years among SFP beneficiary and non-beneficiary children, and the difference was not significant (P = 0⋅905). The two groups were comparable based on age and sex; however, caregivers of the non-beneficiary children had significantly better educational and economic status and also had better access to improved drinking water sources. The two groups were also significantly different based on religion, marital status, household food insecurity and monthly income (Table 2).
Table 2. Basic characteristics of school feeding program beneficiary and non-beneficiary children and their caregivers, Sidama region, southern Ethiopia, 2017
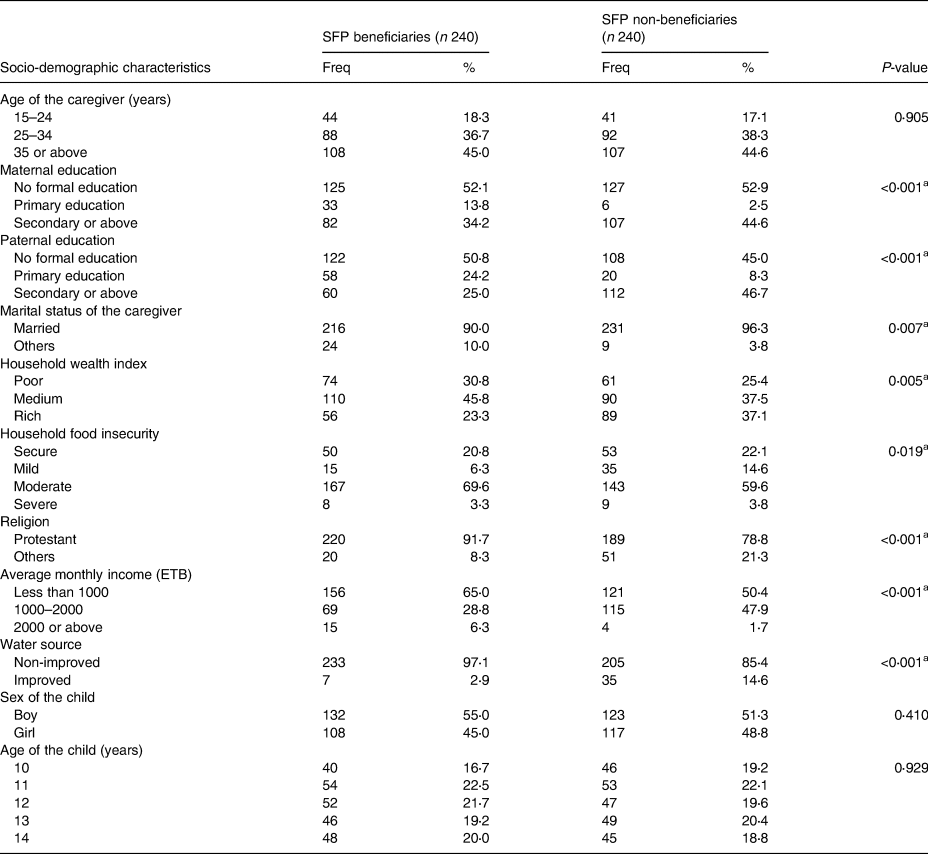
ETB – Ethiopian birr, at the time of the study 1 USD was roughly equivalent to 30 ETB.
a Significant difference at P-value of <0⋅05 (χ 2 test).
Among 480 students enrolled in the study, 17 (3⋅5 %) dropped out of the study; accordingly, they had no measurements for the outcome variables. Dropout rate was significantly lower among SFP beneficiaries (1⋅3 %) as compared to non-beneficiaries (5⋅8 %) (P = 0⋅007).
Effect of SFP on haemoglobin and anthropometric status of school children
Table 3 compares the haemoglobin and anthropometric status of SFP beneficiary and non-beneficiary children during the baseline and end line surveys. At baseline, SFP beneficiaries had significantly lower haemoglobin level (P < 0⋅001) but higher height (P = 0⋅012) and HAZ score (P = 0⋅03). During the end-line survey, the mean haemoglobin in SFP beneficiaries remained significantly lower (P < 0⋅001) but there were no statistically significant differences in terms of the other parameters (Table 3). However, in the sex-stratified analysis, SFP beneficiary males have significantly different BAZ values at end-line survey (P = 0⋅001) (Supplementary Table S1).
Table 3. Anthropometric and haemoglobin status of SFP beneficiary and non-beneficiary children during baseline and end line surveys, Sidama region, southern Ethiopia, 2017

a Statistically significant difference at <0⋅05 level of significance.
b t or x 2 test.
The bi variable and multivariable DiD analyses did not show a significant effect of the SFP, neither on the haemoglobin nor anthropometric status of school children. In the multivariable model adjusted for potential confounders including maternal and paternal literacy, household monthly income, wealth index, household food insecurity, type of drinking water source and religion, SFP did not show a significant net effect on haemoglobin status (β = 0⋅251, 95 % confidence interval (CI): –0⋅238, 0⋅739), BAZ (β = 0⋅121, 95 % CI: –0⋅163, 0⋅405) and HAZ (β = –0⋅291, 95 % CI: –0⋅640, 0⋅588) (Table 4)
Table 4. Effect of a school feeding program on haemoglobin and anthropometric status of school children, Sidama region, Southern Ethiopia, 2017

* Adjusted for maternal and paternal literacy, household monthly income, wealth index, household food insecurity, type of drinking water source and religion of the caregiver.
Discussion
The overarching goal of school feeding programs in low- and middle-income countries is the protection of vulnerable children from hunger and food insecurity. SFP may also have other side benefits including improving the nutritional status of children(Reference Watkins, Gelli and Hamdani13,Reference Ahmed22–Reference Powell, Walker and Chang24) . Nevertheless, in this prospective cohort study, we observed no statistically significant effects of the program on the anthropometric and haemoglobin status of school children.
We found that children who received school meals did not gain weight or height significantly better than their counterparts. This is counter to the conclusion of a systematic review that SFP in low- and middle-income countries has a small but significant effect on the weight gain of children(Reference Watkins, Gelli and Hamdani13). Prospective observational studies or controlled trials undertaken in Bangladesh(Reference Ahmed22), Jamaica(Reference Grantham-McGregor, Change and Walker23,Reference Powell, Walker and Chang24) , Kenya(Reference Mwaniki and Makokha25) and Lao(Reference Buttenheim, Alderman and Friedman26) also confirmed that school meals significantly improve children's anthropometric status. Here it is important to note that the effectiveness of SFP implemented in different settings cannot be directly compared to each other due to remarkable differences in investment and implementation quality(7). During the field work, the researcher observed multiple problems with the implementation of the school feeding programs in the study area. The school feeding programs did not start at the beginning of the academic year. The duration of the intervention period was 7 months (from December to the end of June). All schools had a problem with water supply, and sometimes because of water shortages; the meal of the day was skipped. In addition, in some schools, students shared food because of shortage of dishes and all these factors might affect the quality of the SFP.
Based on survey data, two studies in Ethiopia have reported positive effects of SFP on the anthropometric status of children(Reference Zenebe, Gebremedhin and Henry11,Reference Demilew and Nigussie27) . A comparative cross-sectional study in southern Ethiopia found improved dietary diversity, BAZ and HAZ scores among children who received meals at school than their counterparts(Reference Zenebe, Gebremedhin and Henry11). Likewise, in northern Ethiopia, children not enrolled in the feeding program had two times increased risk of thinness but there was no meaningful difference in the risk of stunting(Reference Gutama12,Reference Demilew and Nigussie27) . However, as both studies used cross-sectional design, they are likely to be affected by systematic errors including confounding and selection bias.
We also observed that SFP had no significant effects on the haemoglobin level of school children. So far, only a few studies have explored the effect of SFP on the haemoglobin level or anaemia status of children. A one-year prospective cohort study in an urban slum in Kenya found that children participating in the SFP had lower levels of anaemia that their controls(Reference Neervoort, Rosenstiel and Bongers28). In a cluster randomised controlled trial in Uganda, SFP reduced the prevalence of anaemia among adolescent girls(Reference Adelman, Gilligan and Konde-Lule29). In Ghana, SFP participants had a significantly higher haemoglobin concentration and the prevalence of anaemia was lowered by 10 percentage points(Reference Abizari, Buxton and Kwara30). In Addis Ababa, the prevalence of anaemia was reduced by 17 percentage points among SFP beneficiaries as compared to 3 percentage points among children in the control group(Reference Gutama12).
The null association observed between SFP enrolment and anthropometric and haemoglobin status of children can be explained by multiple reasons. Firstly, we followed the children for only one academic year, which may not be adequate to assess the long-term effects of the program. Secondly, the quality of school meals provided to children may not be optimal to advance the nutritional status of children In the study districts, SFP beneficiary children were frequently provided with monotonous meals prepared from cereals and legumes and access to nutrient-rich fruits, vegetables and animal source foods through the program was extremely limited and each school child in the study area received a daily hot meal prepared from 150 g of dry cereals and beans in different forms. A local food called ‘Nifro’ is a boiled mixture of maize, beans, vegetable oil and iodised salt. The other meal is called ‘Kinche’, and it is made from cracked wheat with added vegetable oil and iodised salt.
Other studies show that students who participate in school meal programs consume more whole grains, milk, fruits and vegetables during meal times and have better overall diet quality and nutritional status than nonparticipants(Reference Kinderknecht, Harris and Jones-Smith31). In our study area, most primary schools have approximately 2–6 hectares of farmland and it is sufficient to implement school gardening. Also, money in HGSF budgets could be allocated to purchase vegetables and fruits from local farmers. Thus, the deficiencies in some key micronutrients might be addressed through linking HGSF with communities and schools to obtain micronutrient-rich local foods such as nutritious leafy fresh vegetables and fruits that are outstanding sources of vitamins and minerals.
Finally, due to logistic constraints, the initiation of the SFP was delayed for about 3 months and intermittent interruptions were also encountered during the course of the study. A previous study from southern Ethiopia has also witnessed that the SFP in the area is challenged by interruptions due to financial and logistic constraints(Reference Zenebe, Gebremedhin and Henry11).
The full costs of on-site meal programs have been by collecting data from SFP implementers at all levels in four countries in Sub-Saharan Africa. As reported in 2009, costs ranged from US$28 to US$63 per child per year (weighted average US$40 per child per year)(Reference Bundy, Burbano and Grosh1). In Ethiopia, a HG-SFP cost analysis draft report from Partnership for Child-development in 2015 revealed that the total cost per child per year of HGSF in the SNNPR was US$ 28⋅01(32). The present cost, however, might be higher due to inflation.
The following limitations need to be considered while interpreting the findings of the study. Because the study was not a randomised control trial, it was not possible to standardise the intervention including the quality of meal provided to children. Further, we were not able to exclude systematic baseline differences between the two groups. Though key socio-demographic differences between the two groups were statistically adjusted, residual confounding cannot be excluded. As reported in the results section, dropout rates were significantly lower among SFP beneficiaries than in non-beneficiaries and this may underestimate the benefit of the SFP. Finally, due to sample size concerns, we did not measure the effect of SFP separately among undernourished children.
Conclusion
This prospective cohort study did not observe significant contributions of the SFP, as implemented in these four districts in Sidama region. To improve the anthropometric and haemoglobin status of school children SFP should provide healthy balanced meals.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/jns.2022.73
Acknowledgments
The authors acknowledge all the study participants, data collectors and field supervisors for accomplishing the study.
T. A. D. conceptualised the data; verified the methods, investigated the article, performed formal analysis, wrote the original draft; Samson Gebremedhin conceptualised the data, verified the methods, has made substantial contributions to funding acquisition, supervised the article, wrote, reviewed and edited the article, administered the project; B. J. S. conceptualised the data; verified the methods, supervised the article, wrote, reviewed and edited the article.
This study was supported by Hawassa University – NORAD program.
The authors declare that they have no competing interests.






