Introduction
The adoption of modern contraception methods has significantly increased in sub-Saharan Africa(Reference Bearak, Popinchalk and Alkema1–3). In Ethiopia, the contraceptive prevalence rate (CPR) among currently married women is 41 %(4); however, 35 % of modern contraception device (medical products including sub-dermal implants, intrauterine devices (IUDs) or loops which are designed to prevent pregnancy) users discontinued them before their removal date(5). The desire for pregnancy is the second most common reason for early discontinuation and it accounts for almost 27⋅3 %(Reference Nega, Abera and Tadele6–Reference Belete, Zemene and Hagos9). Any woman who could get pregnant is at a risk of having a baby with neural tube defects (NTDs)(Reference Bibbins-Domingo, Grossman and Curry10). The aetiology of NTDs is complex, multifactorial in origin, but mainly dietary factors play a major role(Reference Berhane, Fikadu and Belachew11–Reference de la Fournière, Dhombres and Maurice23). An optimal intake of the iron–folic acid supplement (IFAS) is very crucial for increasing folate concentrations in red blood cells and could significantly reduce the risk of iron deficiency anaemia and congenital anomalies such as NTDs(Reference Stevens, Finucane and De-Regil24–Reference Cordero, Crider and Rogers27). Iron can modulate folate availability via a cellular one-carbon pathway, and low iron status could alter folate utilisation despite an adequate folate intake and extracellular folate concentrations(Reference Oppenheim, Adelman and Liu28,Reference Valberg29) . A sufficient amount of iron plays an important role in the development of the neural tube and for a successful neural tube closure; however, deficits in iron might cause some cases of NTDs(Reference Mao, McKean and Warrier30–Reference Zohn, De Domenico and Pollock32).
Ethiopia has one of the highest rates of micronutrient deficiencies, including iron deficiency, making it a significant public health concern(Reference Haidar, Melaku and Pobocik33–Reference Herrador, Sordo and Gadisa35). In Ethiopia, 84 % of women of reproductive age (WRA) had low levels of red blood cell folate(Reference Haidar, Melaku and Pobocik33,Reference Bationo, Songré-Ouattara and Hama-Ba36–Reference Haider, Olofin and Wang39) . Because of WRA with low serum folate levels, the incidence of NTDs in Ethiopia has increased alarmingly recording the highest rate and emerged as a major public health concern(Reference Berihu, Welderufael and Berhe40,Reference Berhane and Belachew41) , so there is an urgent need to develop an effective intervention programme to address the above-mentioned problem. Despite the fact that the Ethiopian healthcare system has a fertile ground for the provision of the IFAS to reduce the risk of NTDs, there is no preconception care services to women who discontinue modern contraception methods for planned pregnancy, and thus the golden opportunity for instituting key NTD preventative interventions is lost.
In Ethiopia, providing IFASs to pregnant women is a primary strategy for preventing maternal and newborn morbidity and mortality due to anaemia(Reference Fiedler, D'Agostino and Sununtnasuk42). However, knowledge and adherence to iron–folic acid remain relatively low, and various barriers to the programme's success have been identified(Reference Boti, Bekele and Godana43–Reference Bali, Joshi and Tiwari52). Lessons are learnt from the current healthcare strategy for the provision of the IFAS, and alternative approaches are required to improve adherence to the preconception of the IFAS intake. Evidence from other studies indicates that health education intervention is an important tool to improve knowledge and adherence to micronutrient supplementation(Reference Taye, Abeje and Mekonen49,Reference Girard and Olude53–Reference Forrest60) . For effective intervention, it needs to be locally appropriate, simple and practically implemented through the existing healthcare system. We assumed that the preconception picture-based health education intervention package for women planning to get pregnant is the best approach to reduce the risk of NTDs and other adverse outcomes. Therefore, the aim of the present study was to evaluate the effect of picture-based health education and counselling intervention on knowledge and adherence to the IFAS intake among women planning to get pregnant.
Materials and methods
Study area and period
The present study was conducted in Dire Dawa city administration located 515 km in the eastern part of Ethiopia. It was subdivided into 9 urban and 38 rural kebeles. In 2022, the population of Dire Dawa city administration is 445 000, and has increased by 4⋅46 % from 2021. A number of Ethiopian languages are widely spoken in Dire Dawa city administration by the people from the various nations and nationalities living in Dire Dawa city administration. The study was conducted between May 2021 and October 2021.
Trial design
A double-blind parallel randomised controlled trial was conducted in gynecology and family planning clinic at a healthcare facility to determine the effect of pictured-based nutrition education and counselling on the importance of adherence to the IFAS intake during pregnancy.
Participants
Participants included women in the age group of 18–45 years who requested to interrupt contraception to become pregnant and women with spontaneous abortion who refused to adopt a contraceptive method with an intention to become pregnant.
The inclusion criteria included women currently living in the study area (women who are usual residents and live or intend to live in the area for six or more months) and have given consent to participate in the study. Women who took IFAS or any other microsupplements in the past two months and participants who are mentally/physically challenged to provide consent were excluded from the study. The study was carried out in accordance with the ethical principles of the Helsinki declaration and the requirement of good clinical practice(Reference Association61).
Intervention and its procedure
The details of the study protocol were published elsewhere(Reference Berhane and Belachew62). In accordance with the protocol, midwifery nurses who work in the gynecology ward and family planning clinics invited all eligible women to participate in the study and collected the baseline data. In addition, health extension workers were provided home-to-home picture-based nutrition education and counselling(Reference Bhutta, Das and Rizvi63) for women who were assigned to the interventional arm.
Individual picture-based nutrition education and counselling including picture and text messages were delivered to the intervention group using conventional inter-personal communication intervention for 10–20 min by trained health extension workers on a monthly basis. Education includes warnings about lifestyle, dietary habits, risk factors for anaemia and NTDs, adverse effects of NTDs and IFAS guidelines. The IFAS guide includes information on how to take the IFAS, when to take it, how to absorb it more, side effects of the IFAS and foods rich in iron and folic acid. Educational brochures were also distributed at the end of the education session. The brochure contained key messages with images and text. After completing the education session, an opportunity was given to the participants to discuss the education content and clarify any confusion.
Each participant in the interventional arm received two educational health message reminders (on Mondays and Thursdays) in their local language, via mobile during the daytime to avoid disturbing them, every week to make sure they were taking the IFASs. Anyone at home or in the neighborhood who can read is encouraged to read the texts for women who cannot read.
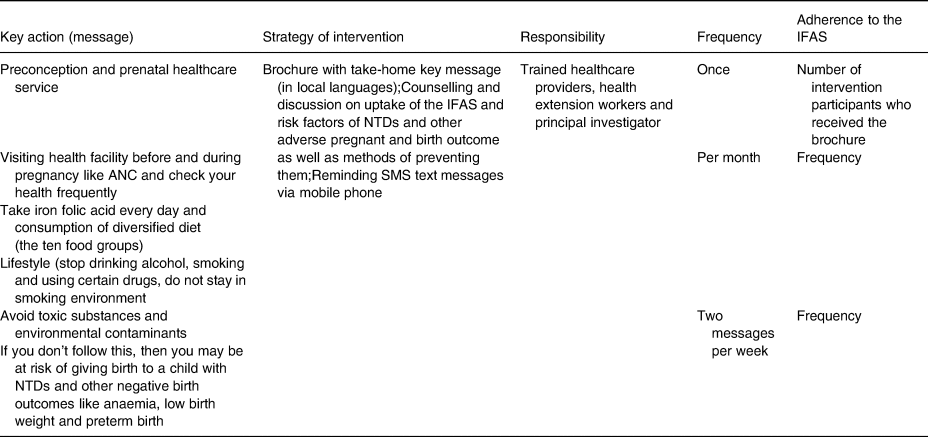
The key messages included ‘eat a diversified food’, ‘take one IFAS tablet per day for at least 90 days’, ‘contact your healthcare provider if you have any complaint related to IFA tablets’, ‘reach and maintain a healthy weight’, ‘visit health facility before and during pregnancy like antenatal care (ANC) and check your health frequently’, ‘avoid toxic substances and environmental contaminants’, ‘avoid living in a stressful or abusive environment; or working with or living around toxic substances’ and ‘Learn your and your partner's family history’ (Table 1). The brochure with take-home messages was also distributed to help participants understand what they have learnt.
Table 1. Intervention protocol for preconception picture-based education and counselling for women, who had an intention to be pregnant, of Dire Dawa city administration, Ethiopia
Every month there was an interaction with their partners and discussion on the issues. These interactions were also important in reducing drop out and assisting participants with any questions that may arise and to increase the involvement of partner in the reproductive health.
The IFAS (thirty iron capsules with 60 mg of ferrous sulphate and 0⋅5 mg of folic acid) was provided to all participants in the intervention and the control groups every month immediately after they removed modern contraception devices(64).
While collecting the IFAS, all participants received a brief information for about 5–10 min regarding the proper usage of the IFAS from the health professional. The information session included the importance of the IFAS, duration of the IFAS to be consumed, the possible side effects of the supplement and ways of handling the side effects. Due to the absence of preconception services for women who plan to get pregnant, the midwifery nurse encouraged the control group to visit the healthcare facility every month to consume the IFAS pills and contacted them if they missed their appointment date. Health professionals did not interfere at any conditions with control arm practices, only the provision and count of the IFAS were done. After the end of the study, similar nutrition information was given to the control group.
Intervention fidelity
The investigators developed criteria to assess the fidelity of the intervention based on the preconception care and dietary guidelines in accordance with WHO recommendations. The criteria included checklists to assess the intervention design, training of counsellors, counselling process and receipt of intervention. Content validity for the education was assured by sending its content to two experts in nutrition and health educational and behavioural science from academic centre. In addition, two expert meetings were held with health professionals for the development of materials. To balance the variations, equal numbers of eligible participants were selected for the intervention and control groups. In addition, to minimise between-educators and counsellors variation, the same health extension workers made three repeated visits for each participant. The intervention process was pretested before the implementation of the trial. Besides, each woman received equal number and frequencies of counselling, and the lengths of contacts within an intervention group were similar to make the process standardised. Picture-based nutrition educator and counsellor's knowledge and skills were assessed by pre- and post-training tests and practical evaluation.
Counting of the remaining IFAS pills were used to measure the adherence of participants to the IFAS intake with the help of the interview about their understanding of the core content of the intervention during home-to-home visits in every month.
Study participants, data collectors (who work at gynecology and family planning service), educator and counsellors were blinded to the study hypotheses and group allocation. Additionally, the data entry clerk was blinded by labelling the groups with a non-identifiable unique number until the analysis was finalised.
Outcomes
The primary outcome of this trial was the adherence to the IFAS intake and knowledge about the IFAS and NTDs.
Sample size
The sample size was calculated using Gpower based on the study considering 80 % power, 0⋅3 effect size and 95 % confidence interval with an intervention to control ratio of 1 and margin of error of 0⋅05. The calculated sample size is 111 and 10 % loss to follow-up was added. The final sample size for a single arm was 122 in the intervention and control arms each. The total sample size was 244.
Randomisation
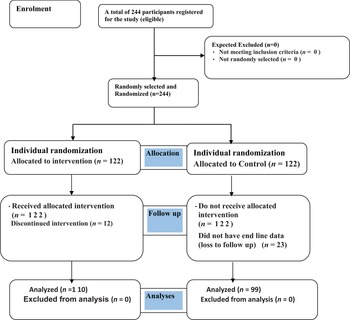
The study subjects were enrolled when they came to the health facility to remove their modern contraception device with an intention to get pregnant or after they had a spontaneous abortion and when they decide that they want to get pregnant immediately. All the necessary information including full address, mobile phone number and a unique ID number of the study participants were recorded. A list of the ID numbers was compiled and sent to the researcher on a weekly basis. Simple randomisation with 1:1 allocation ration was done using ENA for Smart Software. Women randomised to the intervention group only (n 122) received picture-based nutrition education and counselling, where participants in both groups would receive the IFAS and other services being given by the health facility. This study considered the Comprehensive Criteria for Reporting Trials (CONSORT) as a guide for study randomisation (Fig. 1).

Fig. 1. Consort flow diagram showing the effect of picture-based health education and counselling targeting knowledge and adherence to the preconception of iron–folic acid supplement among women who planned to be pregnant: a randomised controlled trial.
Data collection tools and procedures
Data collection was started after receiving official permission to conduct the study and written informed consent from the participants, and before the intervention programme started. Midwifery nurses working in the gynecology and family planning section of health facilities interviewed all eligible participants using face-to-face structured questionnaire. The questionnaire included about the participants’ age, education, occupation, family monthly income, obstetric history and knowledge. Before the formal data collection, the questionnaire was repeatedly pretested and revised based on the analysis of the results. Each interview took around 20–30 min, in a specified room in the gynecology and family planning section.
Twenty-six trained (six midwife nurses and twenty health extension workers) professionals participated in the study. Data collectors and nutrition educator were trained for three days using a training manual that included the following: how to enrol women to the study, how to take the IFAS and the necessary information including the baseline data. In addition, health extension workers received training on how to provide picture-based nutrition education and counselling.
The supervisors and the principal investigator closely monitored the data collection process. Additionally, nutrition counsellors also have monthly meetings with supervisors to discuss any problems they are encountering while providing nutrition counselling. Feedback is provided to the counsellors in these meetings.
Operational definition of terms
Intervention group
Randomly selected women who were given preconception picture-based education and counselling along with 60 mg of elemental iron and 400 μg (0⋅4 mg) of folic acid supplementation for 3 months beginning with the date of contraceptive device removal and pregnancy termination.
Control group
Randomly selected adults taking 60 mg of elemental iron and 400 μg (0⋅4 mg) of folic acid but not given preconception picture-based education and counselling for 3 months beginning with the date of contraceptive device removal and pregnancy termination.
Adherence to the IFAS intake
During the three-month intervention period, the participants were expected to take ninety IFAS pills, on the assumption of one tablet of the IFAS is taken each day starting from the removal of modern contraception device. The participants were divided into two groups based on their adherence to the IFAS intake. If they were able to take at least seventy-two and more IFAS pills or 80 % from the total take period, they were considered an adherent to the IFAS intake, whereas those who were not able to take less than seventy-two IFAS tablets or less than 80 % from the total intake period were considered non-adherents to the IFAS intake(25,Reference Sendeku, Azeze and Fenta45) . Women who did not attend all counselling sessions were deemed non-adherent to the guidelines. Women who dropped out of the study, on the other hand, were labelled as lost to follow-up.
Knowledge
Subjects were graded by asking a series of ten questions about the IFAS and NTDs marking correct answers out of a hundred. ‘Poor knowledge’ was defined as an average knowledge score of 50 % or less.
Intention to treat
Intention to treat (ITT) was calculated by including all participants who were considered randomised in the statistical analysis and were analysed according to the group they were originally assigned.
Duration of the intervention
The time period of picture-based health education and counselling given to the intervention group was 3 months starting from the second half of May 2020 to October 2021.
Modern contraception
Defined as a medical product including sub-dermal implants, IUDs or loops which are designed to prevent pregnancy.
Statistical analysis
Data were presented in the form of descriptive statistics, such as frequency, percentages, mean and standard deviation. The Kolmogorov–Smirnov test was used to check the normality of the distribution. The effects of the intervention between-group differences were assessed using a χ 2 test for categorical variables and an independent t-test for continuous variables with normal distributions. Within-group changes were assessed using a paired t-test after 3 months. The Cohen's d statistic (effect size) was used to measure the significance of the intervention's effect. It was categorised as follows: <0⋅2 has no effect, 0⋅2 to <0⋅5 has a small effect, 0⋅5 to <0⋅8 has a moderate effect and >0⋅8 has a significant effect indicating a strong relationship between the two variables(Reference Cohen65). Adherence to the IFAS intake was conducted with the goal of considering the ITT concept.
Univarite and multivariable linear regression analyses modelling were performed to detect the most independent variables affecting adherence and knowledge to the IFAS by controlling the possible confounding variables. Analyses are based on valid data available for each (set) of variables analysed and no missing data are imputed. Variables with a P-value of <0⋅05 were considered statistically significant in univarite and multivariable analyses. IBM SPSS Statistics 25 was used for these analyses.
Patient and public involvement
In the present study, neither patient nor public was involved in study proposal development, design and analysis of the study.
Results
During the recruitment period (May 2021 and end of October 2021), a total of 244 eligible participants who were enrolled in the study (ITT population). A total of 35 (14⋅3 %) participants (n 12 from intervention and n 23 from control arm) were declined from the study due to different reasons. Overall, the mean (and sd) age of the participants was 28⋅1 ± 5⋅19 years, with 42 % of the participants being between the ages of 26 and 34 years. All participants were married. There were no statistically significant differences between the socio-demographic characteristics and pregnancy-related information of participants in the intervention group and those participated in the control group in terms of age, educational status of women, partner educational status and history of taking IFAS during pregnancy (P > 0⋅05). Additionally before the intervention programme, there were no significant differences between the two groups in terms of history of IFAS or FAS before pregnancy, knowledge on NTDs and preconception of IFAS (P > 0⋅05). However, there were statistically significant differences between two groups in terms of history of ANC visit during pregnancy, history of NTDs affecting pregnancy and history of spontaneous abortion (P < 0⋅05) (Table 2).
Table 2. The socio-demographic characteristics and pregnancy-related information of the study participants (n 244)

FAS, folic acid supplement; IFAS, iron and folic acid supplement.
Pearson correlation (χ 2 test), significant at P < 0⋅05.
After 3 months of intervention, the proportion of adherence to the IFAS was 23 % (n 56). With regard to adherence within the groups, 42⋅6 % (n 52) in the intervention group and 3⋅3 % (n 4) in the control group and the intervention group were significantly higher than in the control group. In the intervention group, the proportion of adherence to the IFAS intake among participants increased by 40⋅1 % and they were statistically different (P < 0⋅0001). At the end of the study, the proportion of adherence to the IFAS increased slightly in the control group and it was increased by 2⋅5 % in the control group (P = 0⋅31). The difference in difference between the two groups of adherence to the IFAS intake was 37⋅6 % and they were statistically significant (P < 0⋅0001) (Table 3). The endline data of adherence between the groups did differ from the baseline data (P = 0⋅31 v. P < 0⋅0001).
Table 3. Differences between baseline and endline adherence to the IFAS and difference in difference between intervention and control groups

BL: baseline; EL: endline.
Significant at P < 0⋅05.
Table 4 presents the changes in knowledge between and within group. Level of knowledge between the groups did differ before and after intervention (P = 0⋅87 v. P < 0⋅0001). The mean knowledge scores were 48 (±26 sd) at their highest and 13 (±8⋅3 sd) at their lowest. A comparison of the scores at the baseline and end of 3 months follow-up showed that the mean change in knowledge was 17⋅6 (±28 sd) points in the intervention group and 18⋅5 (±18⋅8 sd) in the control group. The overall mean change in knowledge mean (and se) between groups was 0⋅9 (±3⋅04 se) and there were significant differences between two groups (P < 0⋅001).
Table 4. A comparison between participants’ mean scores for knowledge of the IFAS

DID: difference in difference.
Significant at P < 0⋅05.
1 Intervention group (n=122) and Control group (n=122).
Univariate and multivariate linear regression analyses were conducted to identify the variables that could independently predict higher adherence rates among the participants of the intervention group following the programme. History of NTDs affecting pregnancy, history of spontaneous abortion and knowledge were independently associated with adherence to the IFAS intake (P < 0⋅05). The most identified factors that affected the adherence to the IFAS intake were history of NTDs affecting pregnancy and knowledge levels (P < 0⋅001) (Table 5).
Table 5. Bivariate and multivariable linear regression analyses for the factors affecting adherence to the IFAS

B, unstandardised coefficients; CI, confidence interval.
R 2 = 0⋅19; F = 14⋅7. All variables with P < 0⋅05 were included in the multivariate analysis.
* Statistically significant at P < 0⋅05.
Discussion
Many research findings regarding the knowledge and adherence to the IFAS intake among pregnant women have been published. To our knowledge, no study has been conducted regarding the knowledge and adherence to the IFAS intake among women who plan to get pregnant. The present study is the first parallel randomised controlled trial to evaluate the effectiveness of nutrition education on the knowledge and adherence to the IFAS intake using an individual's knowledge through picture-based nutrition education and counselling approach. The major goal of this intervention was to encourage women who plan to get pregnant to have a thorough knowledge about and adherence to the IFAS intake to avert the risk of developing NTDs affecting pregnancy and other related negative impacts on women and neonates.
In the present study, the adherence to the IFAS intake was 2⋅2 and 42⋅6 % (before and after the intervention) within the intervention group (P < 0⋅0001) compared with the 0⋅8 and 3⋅3 % (before and after intervention) within the control group (P = 0⋅31) and the average number of supplements taken in the intervention group was significantly higher than in the control group.
This implies that the nutrition education intervention package has a significant positive impact in improving women's health adhered to preconception of the IFAS intake in the intervention group than the control group. Therefore, institutionalised along with link to home delivery nutrition education is one of the promising interventions that could improve the pregnancy and birth outcome and extend to future generation and community as whole(Reference Mok, Poh and Wee66). Even though the study participants were different from our study, the present study was in agreement with the study conducted in Ethiopia(Reference Mengesha, Hidru and Welay67) in Bihar, India(Reference Wendt, Young and Stephenson68), in Kenya(Reference Matiri, Pied and Velez69), from Jordan, Saudi Arabia, India and Indonesia(Reference Nahrisah, Somrongthong and Viriyautsahakul70–Reference Permatasari, Rizqiya and Kusumaningati74).
The nutrition knowledge scores were significantly higher at the endline and 3 months after the sessions compared with the baseline and there was a statistical significant difference between the intervention and control groups. However, the mean score of knowledge in the control group showed some improvement after intervention. The results of previous studies are in line with our own, as we found that the nutrition education has a significant impact in improving knowledge(Reference Sisay and Tesfaye75–Reference Ardanjani, Reisi and Javadzade78). In addition, these studies reported a significant difference in the mean scores between two groups (intervention and control) after intervention only, whereas no significant mean difference was observed at the baseline concurrent with our findings. This may be due to the sensitisation that occurred during the initial exposure to the questionnaire and the recall of the answers from the baseline question(Reference Barthassat79,Reference Prelock, Hutchins and Glascoe80) . The significant improvement in knowledge and adherence among the intervention group may also be related to the methods and repetition of the nutrition education intervention package for 3 months with a strict follow-up(64). Similarly, home visits encourage participants to practice what they know to improve their health(Reference Brämswig, Prinz-Langenohl and Lamers81). The repetition education remained longer in memory according to the information process theory(Reference Shiffrin and Schneider82). However, the proportion of improvement in knowledge and adherence was reported different between studies(Reference Wang, Stewart and Chang83). These differences are related to the duration of the intervention and the method(s) used to deliver the intervention(Reference Gitau, Kimiywe and Waudo76).
The study setting could be the second possible justification. The present study was conducted on women in urban areas. Urban women were more exposed to different media about the importance of the iron folate intake compared with the rural counterparts. Their partners may also be more exposed to various sources of information and more easily understand what the healthcare workers advice.
Despite the fact that the biomarker test of the participants was not performed, and it is unknown whether the level of red blood cell folate is increased or the same as before the intake of the IFAS, various laboratory-based researches provided evidence that the intake of the IFAS over at least 12 weeks before the conception by women of child-bearing age increased the level of red blood cell folate, potentially lowering the risk of NTD-affected pregnancy and(26,Reference Cordero, Crider and Rogers27,Reference Bationo, Songré-Ouattara and Hama-Ba36,Reference Brämswig, Prinz-Langenohl and Lamers81,Reference Hao, Yang and Li84–Reference Samson, Loh and Lee90) . Based on this concrete evidence, we would expect women who adhere to the IFAS to be more protective against NTDs if they become pregnant, because folate sufficiency or optimal blood folate concentrations are directly linked to the risk of NTDs(Reference Stevens, Finucane and De-Regil24,25) .
In general, positive aspects of this intervention include a significant improvement in women's knowledge of nutrition to reduce the risk of NTDs, so the intervention should ideally have a positive impact on both the women themselves and their children. The positive effect will help mothers to form a basis for proper nutrition in subsequent years.
The present study has also a significant practical implication for improving the IFAS adherence, which will avert the risk of developing NTDs and improve maternal and child health in order to achieve the Sustainable Development Goals (SDGs). The findings imply the importance of implementing community-level education through health extension as well as at family planning services and other appropriate departments within the health facility through health extension workers as well as by involving males. Furthermore, this approach has the potential to increase adherence and decrease dropout rates of the ANC programme in the country. Therefore, our intervention designed in a way that can be applicable anywhere in a healthcare system. So, the findings of the present study also highlight the importance and effectiveness of adapting preconception policy and national guidelines. Our intervention programmes have no interference and neither did the authors gave financial incentives for health counsellor of either arms. In conclusion, nutrition and health knowledge may not lead to actual behavioural changes, and other behavioural studies need to be done to reach general conclusions.
Conclusion
In conclusion, the picture-based nutrition education intervention approach along with frequent follow-ups through household visits has a significant impact on knowledge and adherence to the preconception of the IFAS intake among women who plan to get pregnant. It helped to improve women's knowledge on anaemia and NTDs during pregnancy, to raise women's awareness on better dietary practices, and to reduce neonatal and maternal morbidity and mortality.
This intervention is very short, simple and cost-effective. We strongly recommend that this intervention should be widely implemented in the country because of the fertile ground of the health care system. We have the following recommendations for the health policy: the first recommendation is to emphasise that the preconception picture-based nutrition education package programme should be endorsed by policy-makers for women who have removed the modern contraception devices and planned to be pregnant and to focus on the behavioural intake of preconception of the IFAS intake on the existing healthcare system (linking to health facility with health extension programme). Additionally, this intervention package will be developed into a comprehensive national strategy to prevent adverse pregnancy and birth outcome during pregnancy. Also, to resolve the nauseating effect of the IFAS as this was the majority side effect reported by participants in the study; so, the healthcare providers will provide a brief explanation with possible solution. Our third recommendation is for the Ethiopian government to support food fortification consumed by a larger proportion of the population. A large-scale community-based study with a larger sample size is required to determine whether this approach is cost-effective.
Acknowledgements
The authors thank all of the study participants, data collectors and supervisors who participated in the study, as well as the kind and cooperative staff of the health facilities in eastern Ethiopia.
Development of the original idea, study concept, design, analysis, and preparation and writing of the original draft was done by A. B. Analysis, writing, review and editing of the whole document was done by T. B.
There was no fund granted for this work.
We declare here in that we have no conflict of interest. The funders had no role in the design of the study; in the collection, analyses or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
All data generated or analysed during this study are included in this published article.
The Institutional Review Board of Jimma University was granted the ethical clearance with the reference number IHR PGY/738/20. Written informed consent was obtained from a parent and/or legal guardian for study participation after providing detailed information on study objectives, benefits. The procedure used in this study was adhered to the principles of the Helsinki Declaration.
This clinical trial was registered on 6 April 2021 under the ClinicalTrials.gov with identifier number PACTR202104543567379.
The full trial study protocol was published elsewhere and can be accessed on Berhane, A. and Belachew, T., 2022. Effect of preconception pictured-based health education and counseling on adherence to iron–folic acid supplementation to improve maternal pregnancy and birth outcome among women who plan to pregnant: randomized control trial. Clinical Nutrition Open Science. https://doi.org/10.1016/j.nutos.2021.12.002